Overview
This article addresses the emotional challenges faced by healthcare providers when it comes to communication. It highlights the often-overwhelming administrative burdens that can hinder patient care. By focusing on effective strategies for utilizing clinical terminology in progress notes, we can enhance both communication and care quality in healthcare settings.
Adopting standardized terminology is a powerful solution. It minimizes misunderstandings among healthcare providers, fostering a more collaborative environment. Moreover, research shows that when uniform language is employed, patient outcomes significantly improve. Reduced miscommunication errors and better care coordination are just a few of the benefits that come from this approach.
Imagine a healthcare setting where everyone speaks the same language—where providers can focus on what truly matters: the patients. By embracing standardized terminology, we can create a more supportive and effective care environment.
Let’s take action together. By prioritizing clear communication, we can ensure that our patients receive the best possible care. How can we implement these strategies in our daily practice? Together, we can make a difference in the lives of those we serve.
Introduction
In the intricate world of healthcare, the use of clinical terminology is not just a technical necessity; it is a vital element for fostering effective communication and delivering high-quality patient care. By embracing precise and standardized language in progress notes, healthcare professionals can significantly enhance clarity and coordination among care teams. This, in turn, leads to improved patient outcomes, which is the ultimate goal we all strive for.
Yet, amidst these aspirations, a pressing question lingers: what barriers stand in the way of implementing these best practices? Understanding these challenges is crucial. Many healthcare providers face overwhelming administrative burdens that can detract from the compassionate care they wish to provide.
How can we work together to overcome these obstacles? By fostering a more efficient and compassionate healthcare environment, we can ensure that the focus remains on the patient. Let us reflect on how we can support each other in this journey, creating a system where everyone thrives.
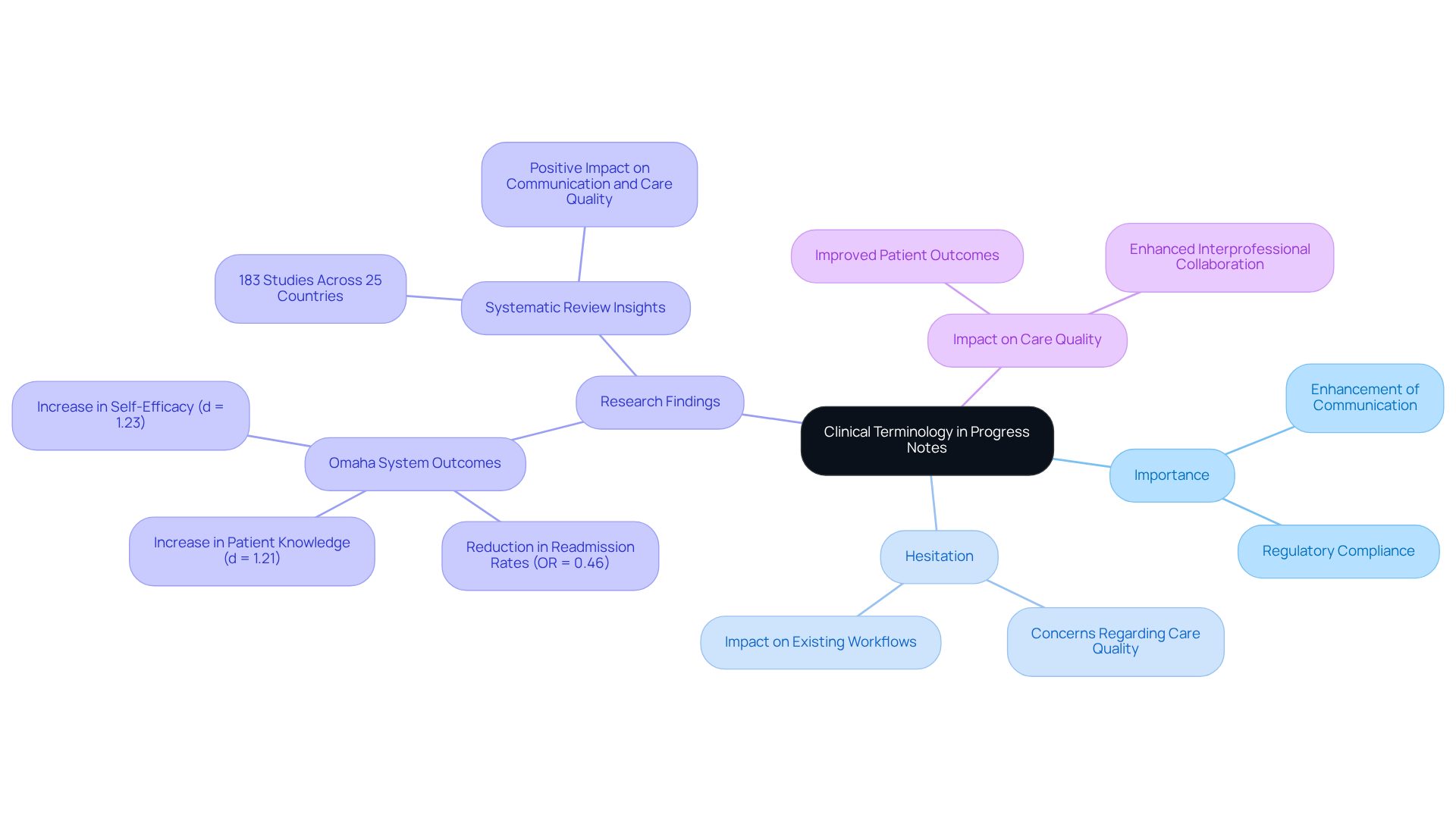
Understand the Role of Clinical Terminology in Progress Notes
Clinical terminology is more than just a language; it is the vital foundation of medical services, providing a standardized framework for recording interactions, diagnoses, and treatment plans. By using precise terms, we significantly enhance communication among medical providers, which minimizes the risk of misunderstandings and errors. For example, opting for the term 'hypertension' instead of 'high blood pressure' fosters clarity and ensures that everyone on the care team comprehends the individual's condition consistently. This shared understanding is essential for delivering and nurturing effective interprofessional collaboration.
Yet, despite the clear advantages of a uniform clinical language, many healthcare professionals hesitate to embrace creative solutions. This reluctance often stems from concerns about potential impacts on care quality and existing workflows. Such hesitation can hinder the implementation of efficient communication methods that are crucial for improving patient outcomes.
Research indicates that standardized nursing vocabularies (SNTs) can lead to better outcomes for patients. A systematic review of 183 studies across 25 countries revealed that implementing SNTs, such as NANDA-I and the Omaha System, positively affected communication and care quality. In one remarkable instance, the Omaha System's nurse-led transitional care program resulted in a significant reduction in readmission rates (odds ratio = 0.46) and notable increases in patient knowledge and self-efficacy (d = 1.21 and d = 1.23, respectively).
Furthermore, precise clinical language not only enhances care for patients but also helps meet regulatory requirements, thereby elevating the overall quality of medical records. By adopting clinical terminology for progress notes, medical providers can ensure consistency in their documentation. This facilitates better data exchange and comparison of outcomes across various settings. Such dedication to standardization, supported by innovative AI solutions like CosmaNeura's Agentic Platform, ultimately enhances the clinical terminology for progress notes, leading to more effective management of patients and improved healthcare delivery. This approach addresses administrative burdens and enriches the overall experience for both providers and patients.
As we navigate these challenges together, let us consider how embracing standardized clinical language could transform our practice and enhance the care we provide. Are we ready to take this step towards a more effective and compassionate healthcare system?
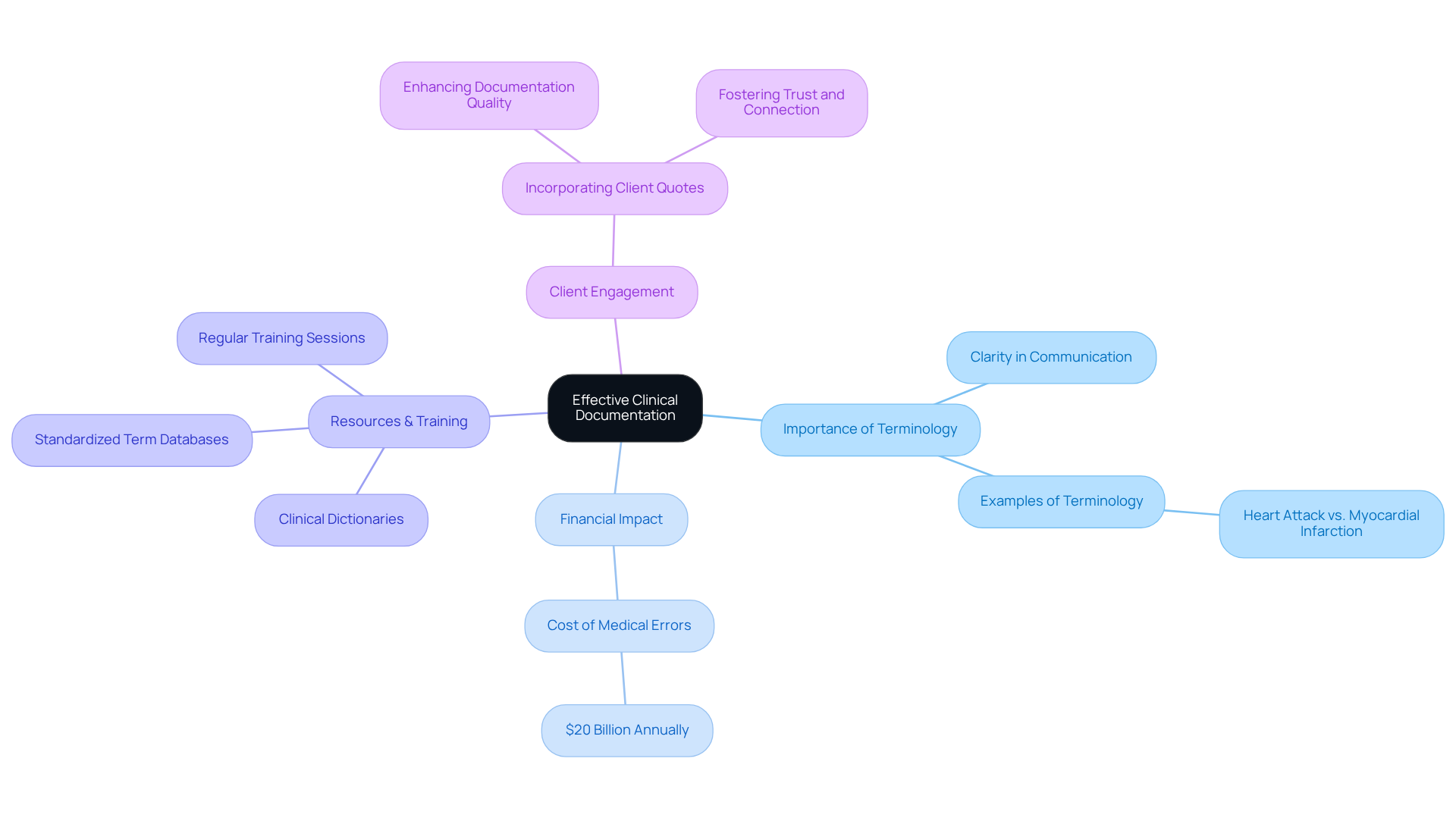
Select Appropriate Clinical Terms for Effective Documentation
Choosing suitable clinical terminology for progress notes can be challenging, especially when considering the emotional landscape of both providers and patients. It's essential to understand not only the individual's condition but also the nuances of their treatment. Providers should prioritize the use of clinical terminology for progress notes that is both clinically precise and accessible. For instance, using 'heart attack' instead of the medical term 'myocardial infarction' in patient-facing documentation can significantly enhance comprehension.
Medical errors can impose a staggering financial burden of around $20 billion annually on the healthcare system. This statistic underscores the importance of . Resources like clinical dictionaries and standardized term databases are invaluable tools for identifying the most relevant words.
Moreover, regular training sessions on clinical terminology for progress notes can empower providers, ensuring that documentation remains clear and effective. Current trends indicate a growing emphasis on user-friendly language within the clinical terminology for progress notes. This shift reflects a commitment to enhancing understanding and engagement in patient care.
Consider this: including client quotes in therapy notes has been shown to improve documentation quality and client engagement. Such practices highlight the significance of client viewpoints, reminding us that their voices matter in the healing process. By embracing these approaches, we can foster a more compassionate and effective healthcare environment.
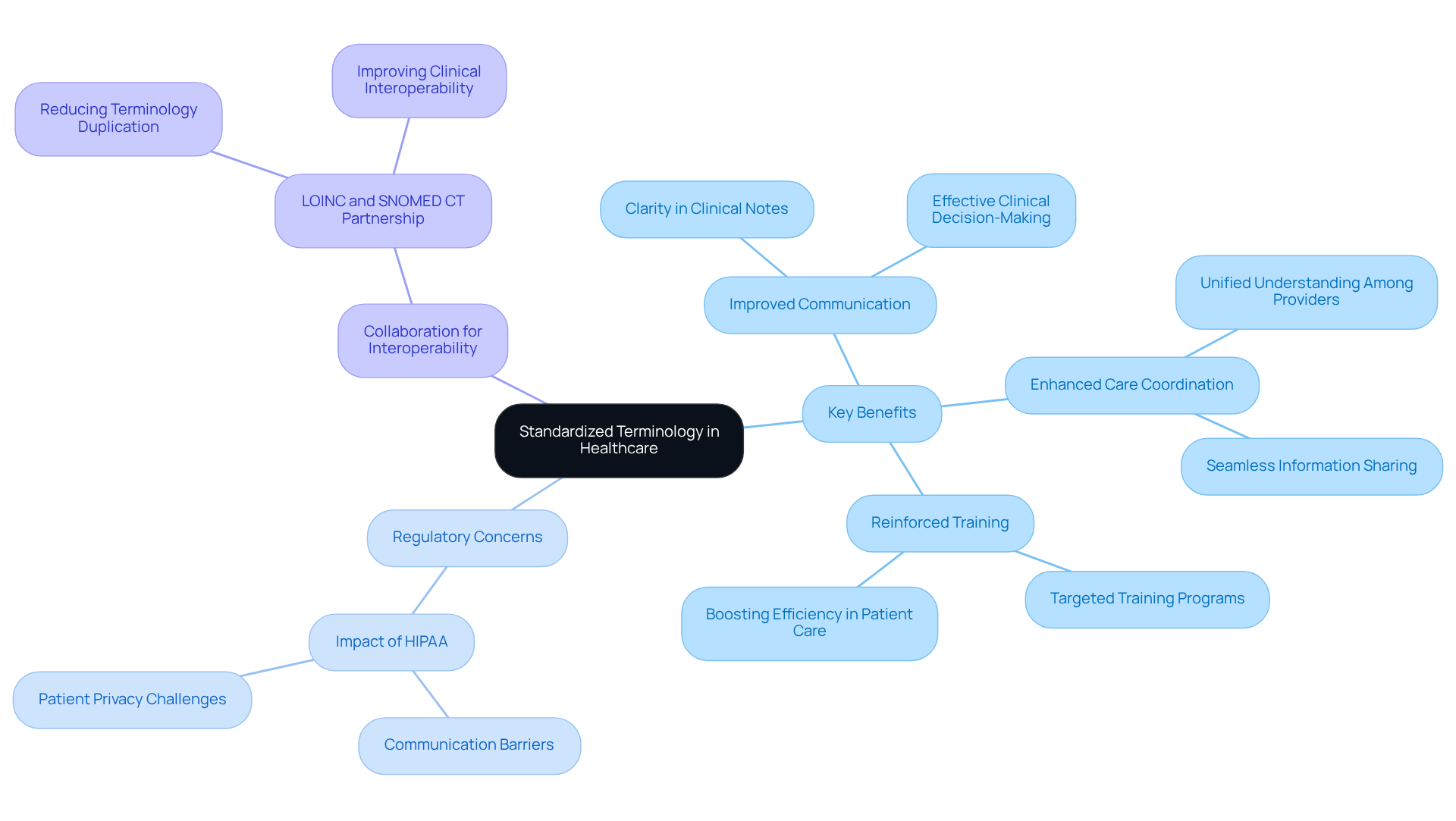
Utilize Standardized Terminology to Enhance Interprofessional Communication
Enhancing Interprofessional Communication with Standardized Terminology
In the complex landscape of healthcare, the adoption of standardized terminology, such as SNOMED CT and LOINC, is vital for fostering effective interprofessional communication. These systems create a common language that all providers can utilize, significantly minimizing the risk of miscommunication and ultimately enhancing patient care.
Key Benefits of Standardized Terminology:
- Improved Communication: Have you ever faced confusion when interpreting a colleague's notes? When a nurse documents a patient's symptoms using clinical terminology for progress notes, physicians can swiftly interpret the information without ambiguity. This clarity leads to more effective clinical decision-making, which is crucial for patient outcomes.
- Enhanced Care Coordination: Imagine a healthcare team where every member understands the same information seamlessly. The use of clinical terminology for progress notes streamlines communication, promoting better care coordination and ensuring that everyone is on the same page.
- Reinforced Training: By implementing targeted training programs on standardized language, we can reinforce its application across the medical team. This not only enhances collaboration but also boosts overall efficiency in patient care.
Addressing Regulatory Concerns: The fragmentation of healthcare systems is further complicated by regulatory concerns, such as HIPAA. While these regulations are essential for protecting patient privacy, they can create significant between patients and their providers. How can we bridge this gap?
Collaboration for Interoperability: In late 2022, a collaboration between LOINC and SNOMED CT was initiated to reduce terminology duplication and improve clinical interoperability. By aligning their standards, these organizations enable a unified approach to health data exchange. This collaboration is essential for delivering high-quality care and utilizing clinical terminology for progress notes to address the challenges posed by fragmented medical systems.
Real-World Example: Consider a recent case where a healthcare team utilized standardized terminology to document a patient's treatment plan. This approach resulted in a remarkable 30% reduction in miscommunication errors, significantly improving patient outcomes. Such examples highlight the effectiveness of using uniform terminology in real-world scenarios, reinforcing the importance of this practice in our daily work.
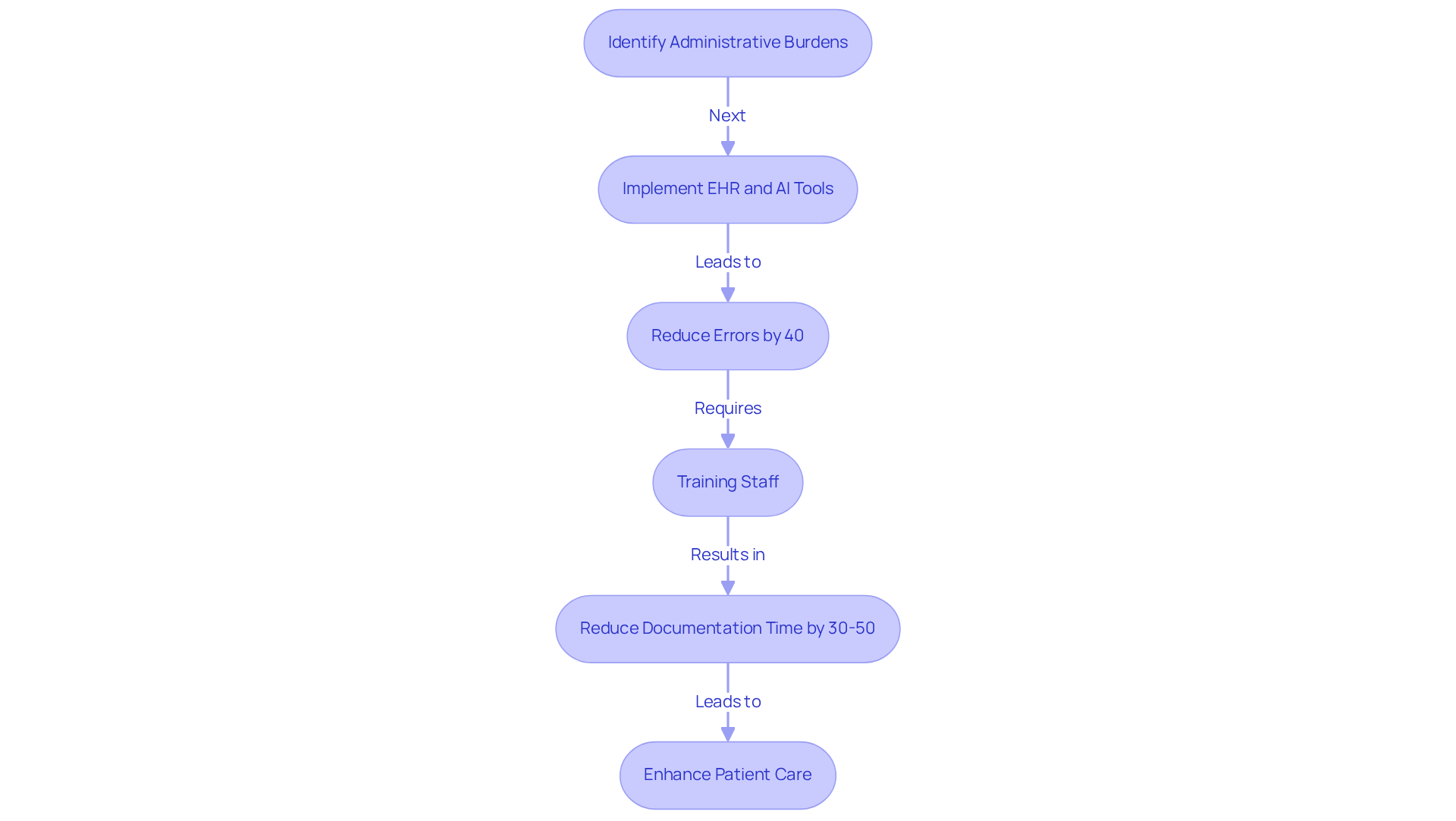
Leverage Technology for Efficient Clinical Documentation
In today's healthcare environment, providers often face overwhelming administrative burdens that can detract from the quality of patient care. Leveraging technology, particularly electronic health records (EHRs) and speech recognition software, can significantly ease these challenges. EHRs simplify documentation by prompting providers with clinical terminology for progress notes that are based on medical history. This not only helps ensure compliance with regulations but also reduces the likelihood of errors, which is a common concern for many in the field.
Consider this: studies show that medical institutions utilizing EHR data analytics have reported a 40% decrease in diagnostic errors compared to traditional paper-based systems. Imagine the peace of mind that comes from knowing that technology is actively supporting your clinical decisions. Moreover, AI-driven tools allow for real-time transcription during consultations, capturing essential information effortlessly. This means you can focus more on what truly matters—providing compassionate care to your patients.
on these technologies is crucial. Effective training can lead to a remarkable 30-50% reduction in documentation time, maximizing the benefits of these systems and ensuring their smooth integration into clinical workflows. As healthcare continues to evolve, embracing these technologies is essential for improving documentation practices, particularly through the use of clinical terminology for progress notes, and enhancing overall patient care. Together, we can navigate these changes and create a more supportive environment for both providers and patients.
Conclusion
Embracing standardized clinical terminology in progress notes is not just beneficial; it is essential for enhancing communication, improving patient outcomes, and fostering a collaborative healthcare environment. Have you ever considered how precise and consistent language can significantly reduce misunderstandings and errors? By ensuring that every member of the care team is aligned in their understanding of patient conditions and treatment plans, we can truly transform the patient experience.
Key strategies to consider include:
- Selecting appropriate clinical terms that resonate with both providers and patients
- Utilizing standardized terminology to enhance interprofessional communication
- Leveraging technology to streamline documentation processes
These approaches not only improve the quality of care but also address regulatory requirements and administrative burdens. Ultimately, they lead to more effective patient management, allowing us to focus on what truly matters: our patients.
The commitment to using clinical terminology in progress notes represents a transformative step towards a more efficient and compassionate healthcare system. As the landscape of healthcare continues to evolve, it is vital for us as providers to embrace these strategies, invest in training, and leverage technology to enhance our documentation practices. By doing so, we can ensure that every patient receives the high-quality care they deserve while paving the way for improved collaboration and communication among providers. Together, let’s create a healthcare environment that is not only effective but also nurturing and supportive.




