Overview
In the demanding world of healthcare, clear, concise, and complete medical record documentation is not just a task—it's a crucial element that enhances patient care. Have you ever felt overwhelmed by the complexities of documentation? You're not alone. Effective documentation practices not only improve accuracy and communication among healthcare teams but also ensure compliance with regulatory standards, alleviating some of the burdens you face.
When documentation is streamlined, it significantly reduces errors and administrative burdens. This allows you to focus more on what truly matters: connecting with your patients. Imagine the positive impact on health outcomes when you can dedicate more time to meaningful interactions instead of paperwork.
By embracing these effective practices, you can foster a more supportive environment for both yourself and your patients. Let’s work together to improve our documentation methods—because every detail counts in providing compassionate care. Your commitment to excellence in documentation can lead to a healthier future for your patients and a more fulfilling experience for you as a provider.
Introduction
Clear, concise, and complete medical record documentation is not just a regulatory requirement; it is a cornerstone of effective patient care. As healthcare providers face the emotional challenges of navigating complex administrative tasks, the integration of AI technology and structured documentation practices emerges as a vital solution. This approach promises to enhance both efficiency and accuracy, alleviating some of the burdens that can weigh heavily on providers.
However, with the stakes so high—ranging from patient safety to financial reimbursement—how can providers ensure that their documentation practices not only meet standards but also genuinely improve patient outcomes? This article explores seven impactful strategies that leverage technology and teamwork to transform medical record documentation. By embracing these practices, providers can ultimately lead to better care for patients.
Here are some key strategies to consider:
- Integrate AI tools to streamline documentation processes.
- Foster teamwork among healthcare staff to share the workload.
- Implement structured templates for consistent record-keeping.
- Prioritize training to enhance staff proficiency with documentation tools.
- Encourage regular feedback to refine practices continuously.
- Utilize patient engagement tools to capture accurate information.
- Monitor outcomes to ensure documentation improvements translate into better care.
By focusing on these strategies, healthcare providers can navigate their documentation challenges with confidence, ensuring that patient care remains at the forefront of their efforts.
CosmaNeura: Streamline Medical Record Documentation with AI Technology
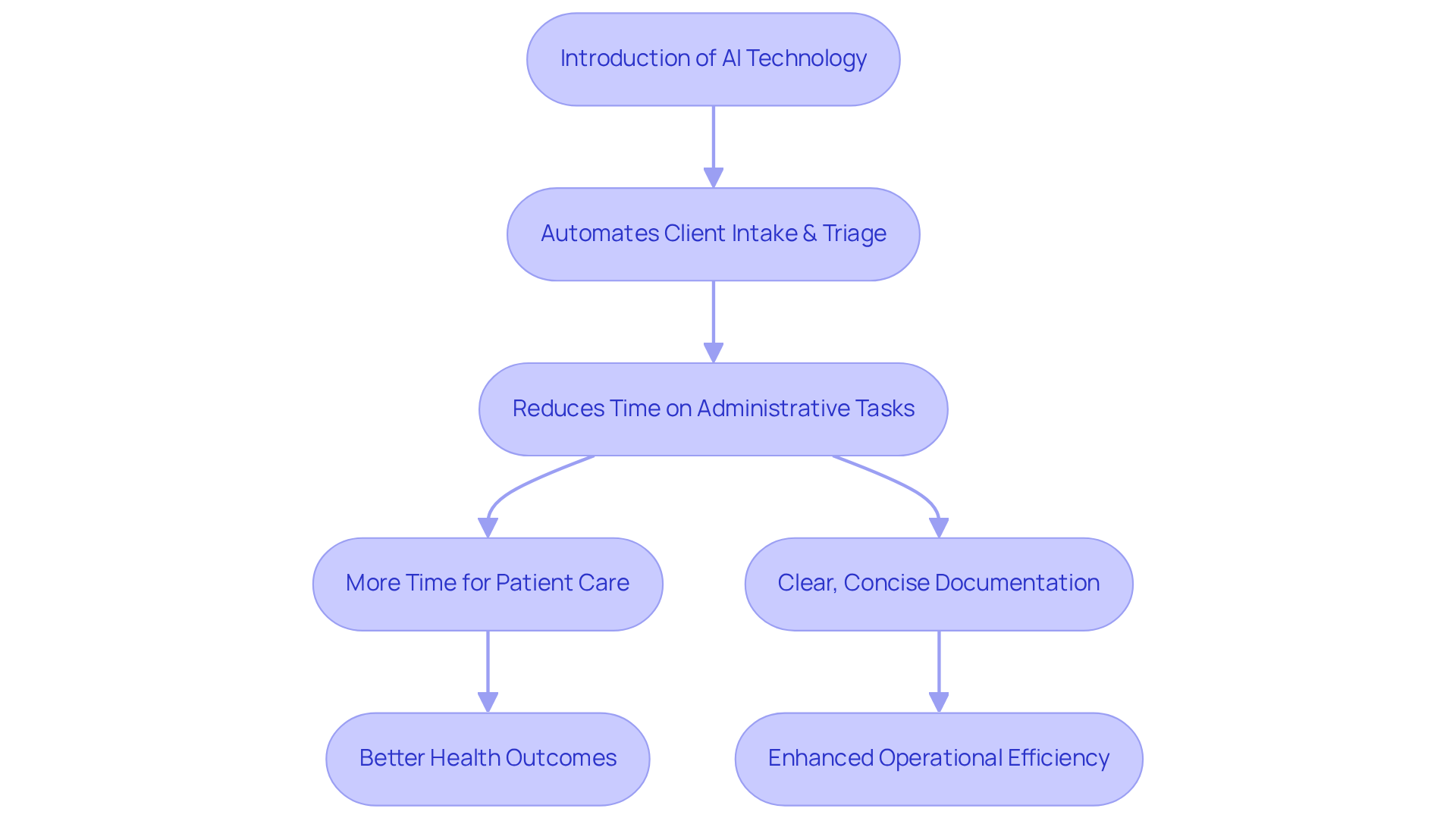
CosmaNeura's AI platform is here to transform the way is handled, addressing the emotional challenges healthcare providers face daily. By automating essential processes like client intake and triage, this platform significantly reduces the time medical professionals spend on administrative tasks. This shift allows them to devote more time to what truly matters: supporting their patients.
As a result, clear, concise, and complete medical record documentation results in better accuracy, ensuring that providers can deliver prompt and efficient assistance. The integration of AI technology into record-keeping signifies a meaningful step forward in medical management, particularly for faith-oriented providers who prioritize compassionate care.
Imagine the possibilities: forecasts indicate that healthcare providers could reduce record-keeping time by up to 50% by 2027. This presents a remarkable opportunity for enhanced efficiency, as clear, concise, and complete medical record documentation results in better health outcomes. Moreover, 80% of health system executives recognize AI as a transformative force in traditional practices, highlighting its essential role in streamlining administrative workflows and alleviating clinician burnout.
By embracing AI, service providers can not only enhance their operational efficiency but also uphold their commitment to delivering high-quality, ethically aligned support. Let's take this step together towards .
Enhance Communication Among Healthcare Teams Through Accurate Documentation
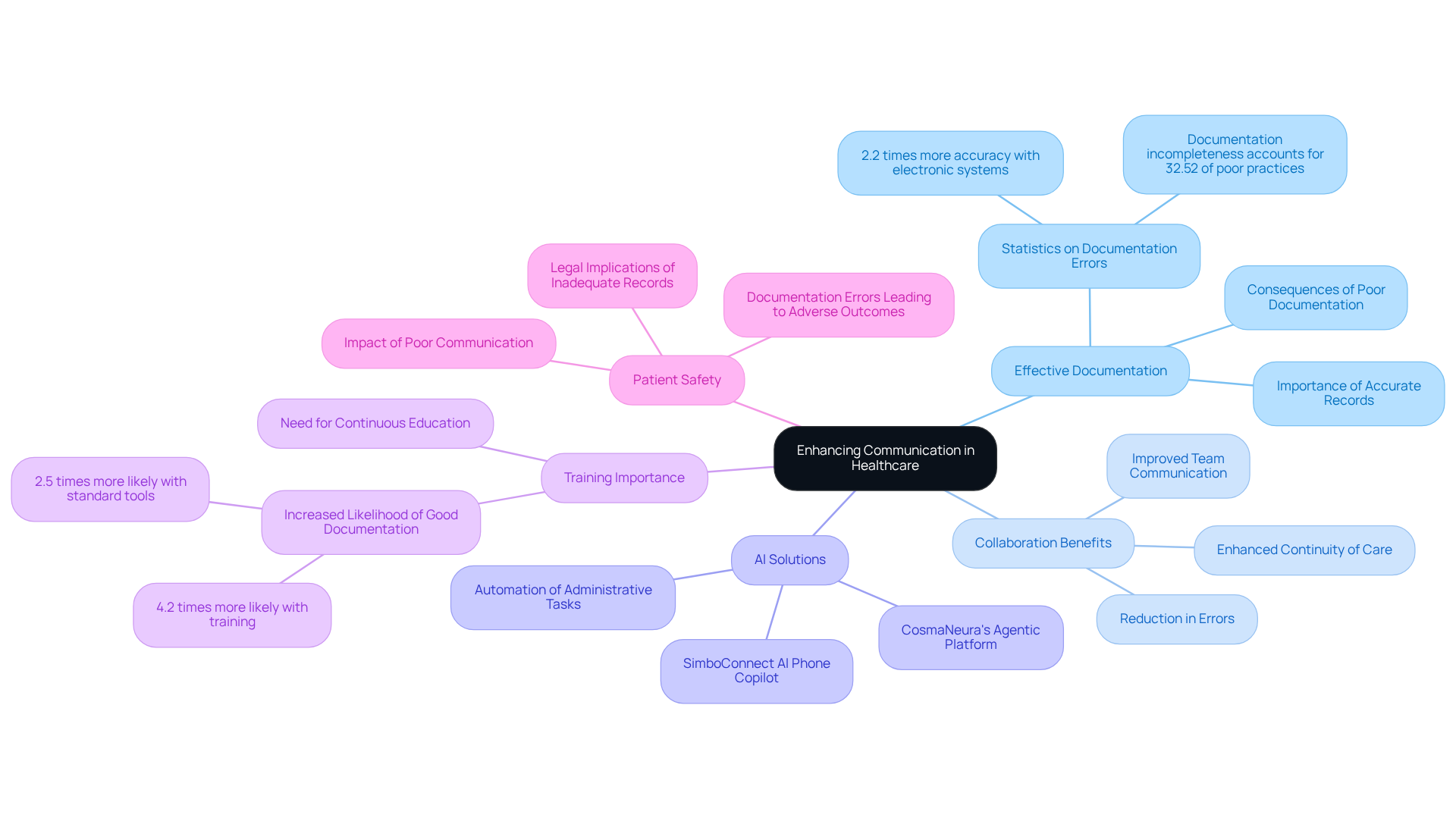
Effective communication among healthcare teams is achieved when clear, concise, and complete medical record documentation results in better collaboration. This is particularly important when faced with challenges such as restricted access to services and increasing administrative burdens. Have you ever felt overwhelmed by the amount of information you need to manage? When all team members have access to clear, concise, and complete medical record documentation, it results in better collaboration significantly. This minimizes the risk of mistakes and enhances continuity of care, especially in multidisciplinary teams where different specialists contribute to an individual's treatment plan.
By ensuring that clear, concise, and complete medical record documentation results in better collaborative efforts, medical providers can strengthen their approach, ultimately leading to improved patient outcomes. Innovative AI solutions, like CosmaNeura's Agentic Platform, can transform this process by simplifying record-keeping practices and alleviating administrative burdens. Research shows that medical practitioners using electronic record-keeping systems are 2.2 times more likely to maintain accurate records compared to those relying on manual forms.
Moreover, record-keeping errors contribute to significant patient injuries and fatalities each year in the USA, underscoring the serious consequences of inadequate record management practices. To enhance the quality of records, is crucial. This not only improves their skills and understanding but also increases the likelihood of effective documentation by 2.5 times when standard tools are available.
This enhanced precision ensures that clear, concise, and complete medical record documentation results in better operations and empowers medical teams to make informed decisions. In turn, this leads to improved overall safety and quality of service. Let's work together to address these challenges and ensure that every patient receives the care they deserve.
Reduce Risk Management Exposure with Comprehensive Medical Records
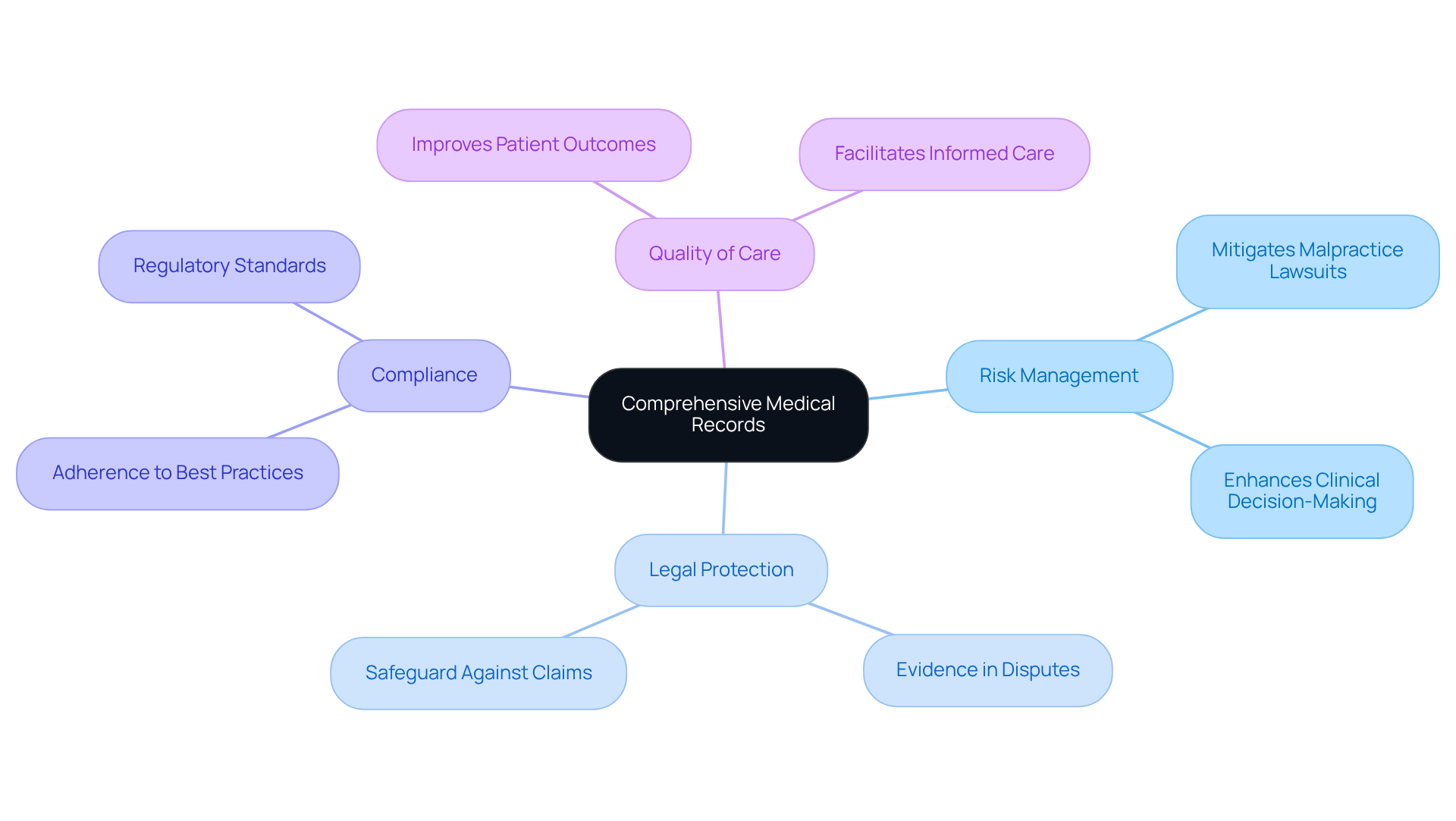
Clear, concise, and complete medical record documentation results in better effective risk management in healthcare. Have you ever considered how meticulous documentation can alleviate your concerns about compliance with best practices and regulatory standards? This thoroughness not only protects against potential legal claims but also demonstrates that clear, concise, and complete medical record documentation results in better quality of service you provide. In the event of a dispute, well-maintained records become crucial evidence of the care delivered, helping to mitigate the risk of malpractice lawsuits. Did you know that record-keeping failures are involved in 20% of medical malpractice cases? This statistic underscores the importance of accurate and thorough records.
For instance, implementing a Cumulative Patient Profile (CPP) ensures that all relevant health information is easily accessible. This aids in informed clinical decision-making and enhances the overall delivery of medical services. By prioritizing thorough record-keeping, you can ensure that clear, concise, and complete medical record documentation results in better legal protection while promoting a higher standard of client service. It is also essential for medical records to include patient identification, contact details, and a comprehensive overview of the patient's medical history. Maintaining precise and efficient records is crucial because clear, concise, and complete medical record documentation results in better outcomes.
As Michael Paskavitz, Vice President of Candello, stated, "This report highlights the necessity for accuracy in health care records as a crucial safeguard against malpractice claims." By adhering to these record-keeping standards, you not only enhance your legal protections but also align your practices with ethical considerations, particularly those rooted in Catholic teachings. Together, let’s embrace these practices to ensure the .
Meet CMS Hospital Quality Indicators and PQRS Measures with Proper Documentation
Clear, concise, and complete medical record documentation results in better compliance with the Centers for Medicare & Medicaid Services (CMS) Hospital Quality Indicators and Physician Quality Reporting System (PQRS) measures. These standards are not just regulatory requirements; they are crucial in ensuring that medical providers can offer high-quality services. Are you feeling overwhelmed by the administrative burdens of record-keeping? By maintaining careful records, providers can demonstrate compliance while also preparing for better reimbursement rates and improved quality ratings. This dual benefit strengthens the financial health of healthcare organizations and underscores their commitment to delivering exceptional patient care.
Consider this: efficient record-keeping methods can represent as much as 95% of securing suitable reimbursement, as highlighted in the case study 'Ensuring Appropriate Reimbursement via Records.' Dr. David Schillinger emphasizes, "Medical reimbursement mirrors what you record, not merely what you perform," showcasing the direct link between record quality and financial outcomes. This understanding can alleviate some of the stress associated with documentation, knowing that precise records also act as a safeguard against malpractice claims, providing vital evidence of the treatment delivered, as illustrated in the case study 'Risk Management through Accurate Documentation.'
As medical services continue to advance, the significance of clear, concise, and complete medical record documentation results in better compliance and enhances patient care cannot be overstated. Let’s work together to embrace effective record-keeping practices that not only fulfill regulatory requirements but also enhance the quality of care you provide. Your dedication to maintaining these standards reflects a profound .
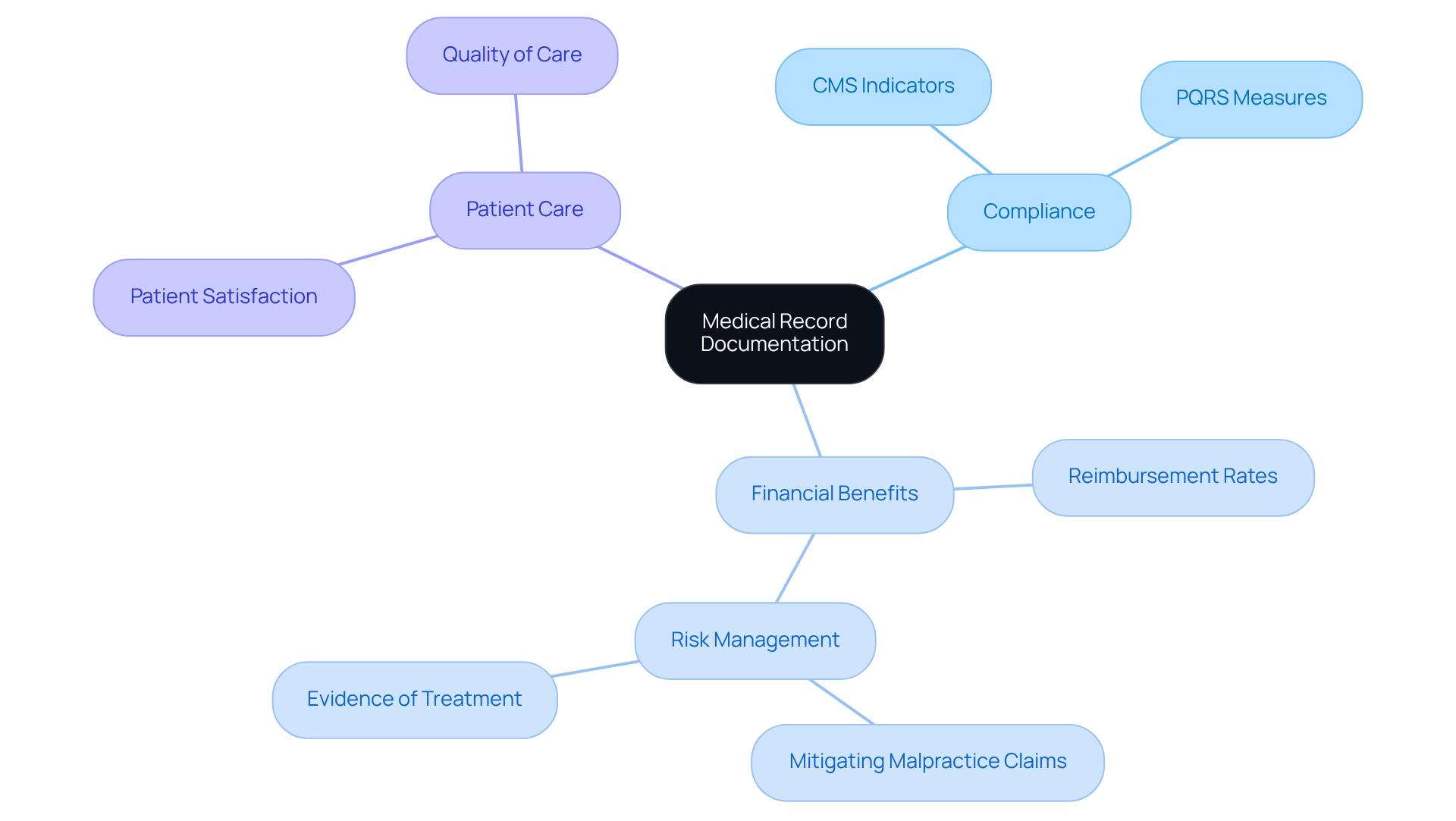
Ensure Appropriate Reimbursement Through Detailed Medical Records
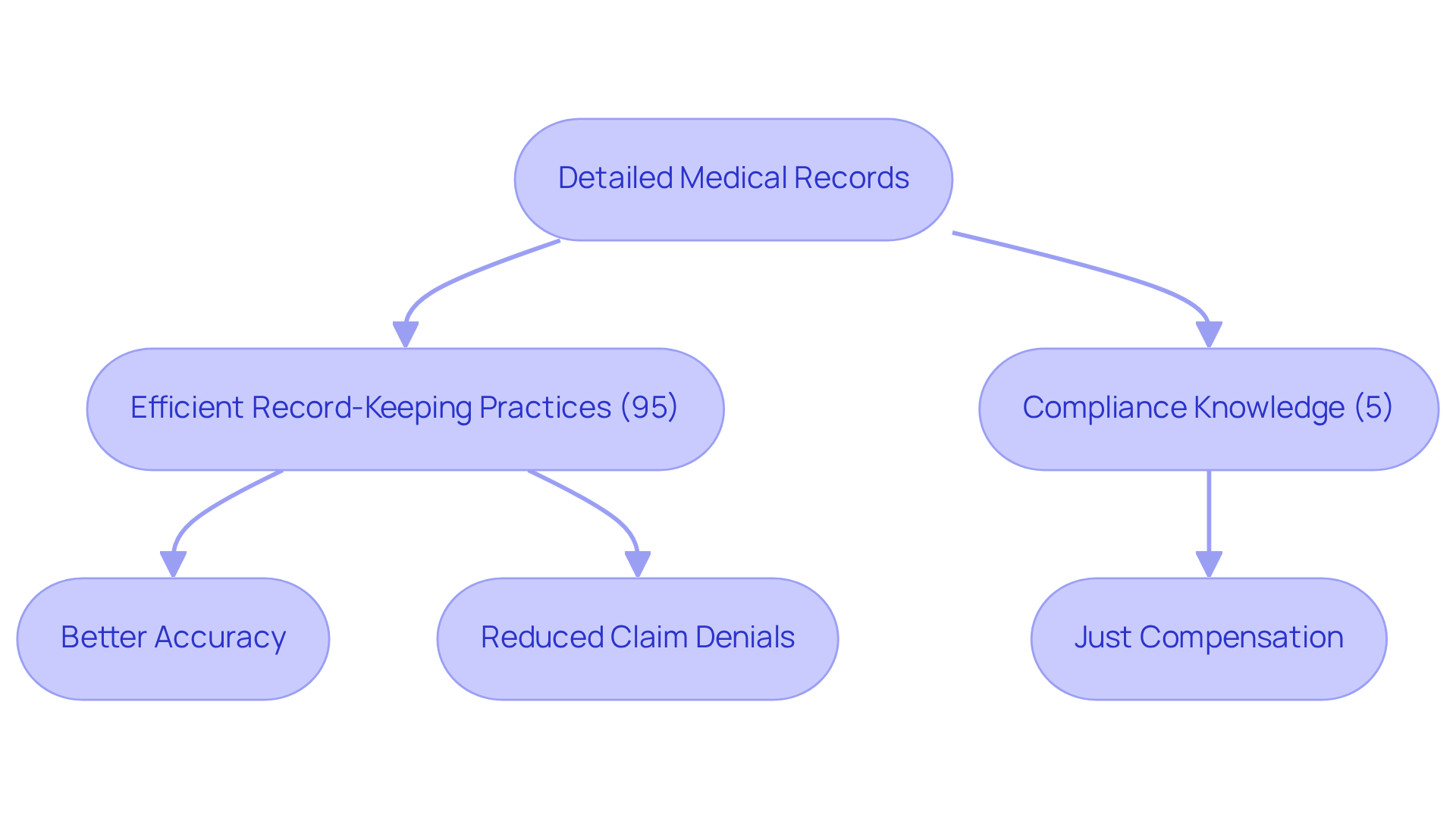
Detailed medical records are essential for ensuring that healthcare providers receive the reimbursement they deserve from insurance companies. Have you ever felt overwhelmed by the administrative tasks that take time away from patient care? Clear, concise, and complete medical record documentation results in better support for coding and billing procedures and helps secure fair payment for the services you provide. The financial health of your practice can be significantly impacted, as clear, concise, and complete medical record documentation results in better accuracy, preventing inaccuracies or omissions that lead to claim denials or reduced payments.
Consider this: efficient record-keeping practices can account for up to 95% of guaranteeing appropriate reimbursement, while the remaining 5% relates to compliance knowledge. By leveraging AI technology, you can ensure that clear, concise, and complete medical record documentation results in better accuracy and completeness for your billing processes. This not only mitigates the risk of but also ensures that you are justly compensated for your hard work.
The benefits of this approach are twofold: it enhances your financial results and promotes a more efficient medical delivery system. Imagine the peace of mind that comes from knowing your administrative tasks are streamlined, allowing you to focus on what truly matters—your patients. Let's work together to create a more supportive environment for healthcare providers, where you can thrive both financially and emotionally.
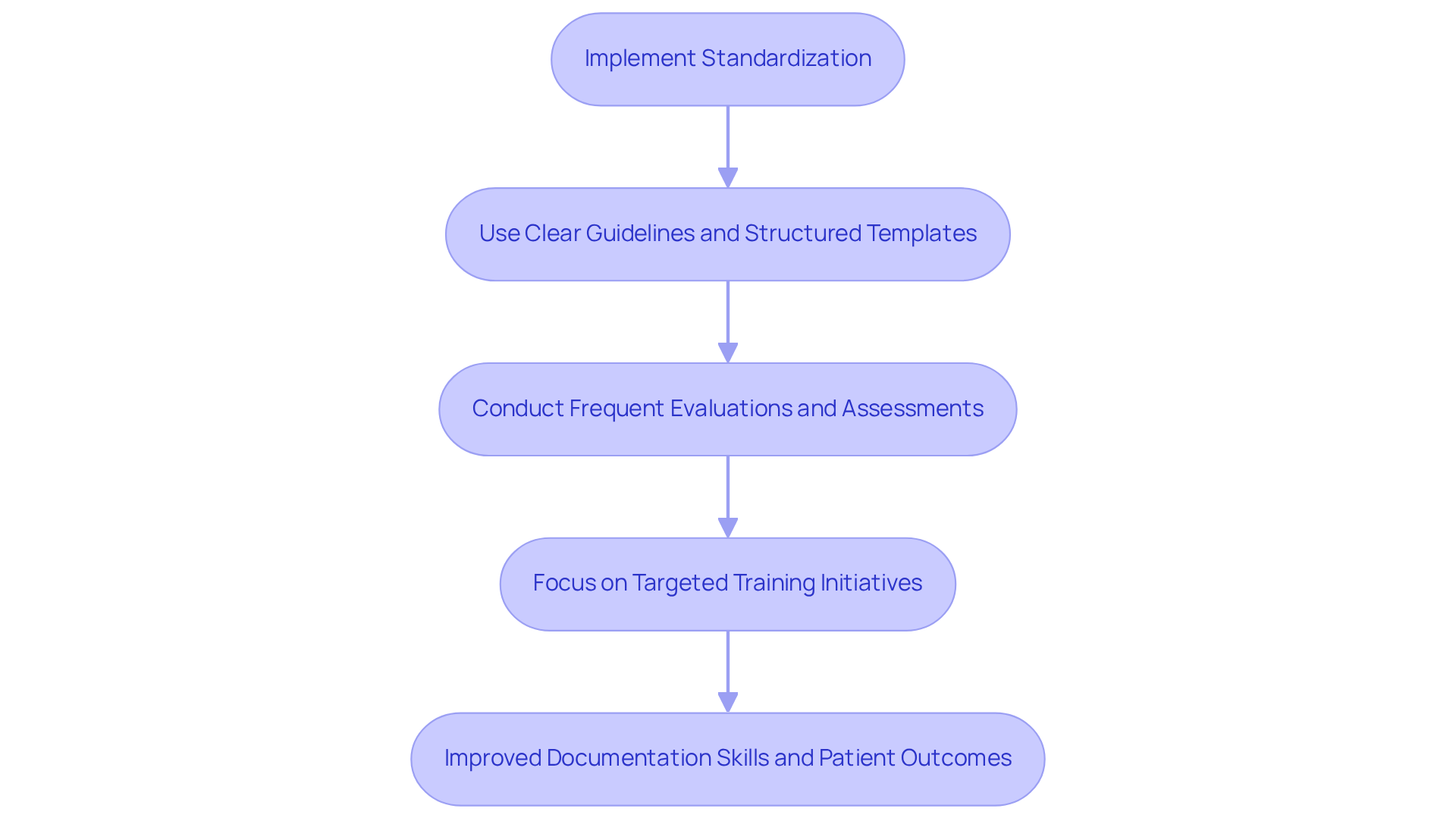
Implement Standardization and Regular Review to Improve Documentation Skills
Standardizing record-keeping practices is not just a procedural necessity; it’s a vital step towards ensuring that clear, concise, and complete medical record documentation results in better quality of medical records. Have you ever felt overwhelmed by the sheer volume of administrative tasks? By implementing clear guidelines and structured templates, healthcare providers can achieve consistency and accuracy in patient records, alleviating some of that burden. Frequent evaluations and assessments are crucial in identifying areas for enhancement. This enables focused training initiatives that can significantly improve record-keeping abilities among providers.
Research has shown that having clear, concise, and complete medical record documentation results in better note quality. For instance, scores rose from 64.35 to 77.2 after applying standardized practices. This commitment to not only empowers individual providers but also elevates the overall quality of care given to individuals. Imagine the difference it makes when every healthcare provider feels confident in their record-keeping.
Moreover, routine evaluations foster an environment of responsibility and ongoing enhancement. This ensures that records remain accurate and relevant. As highlighted in numerous studies, clear, concise, and complete medical record documentation results in better patient outcomes. It’s essential for medical organizations to prioritize these approaches. By embracing these practices, we can create a more supportive and effective healthcare environment for everyone involved.
Key Solutions:
- Implement clear guidelines and structured templates.
- Conduct frequent evaluations and assessments.
- Focus on targeted training initiatives.
Let’s work together to ensure that our record-keeping practices not only meet the standards but also reflect our commitment to compassionate care.
Leverage Peer Support for Enhanced Documentation Practices
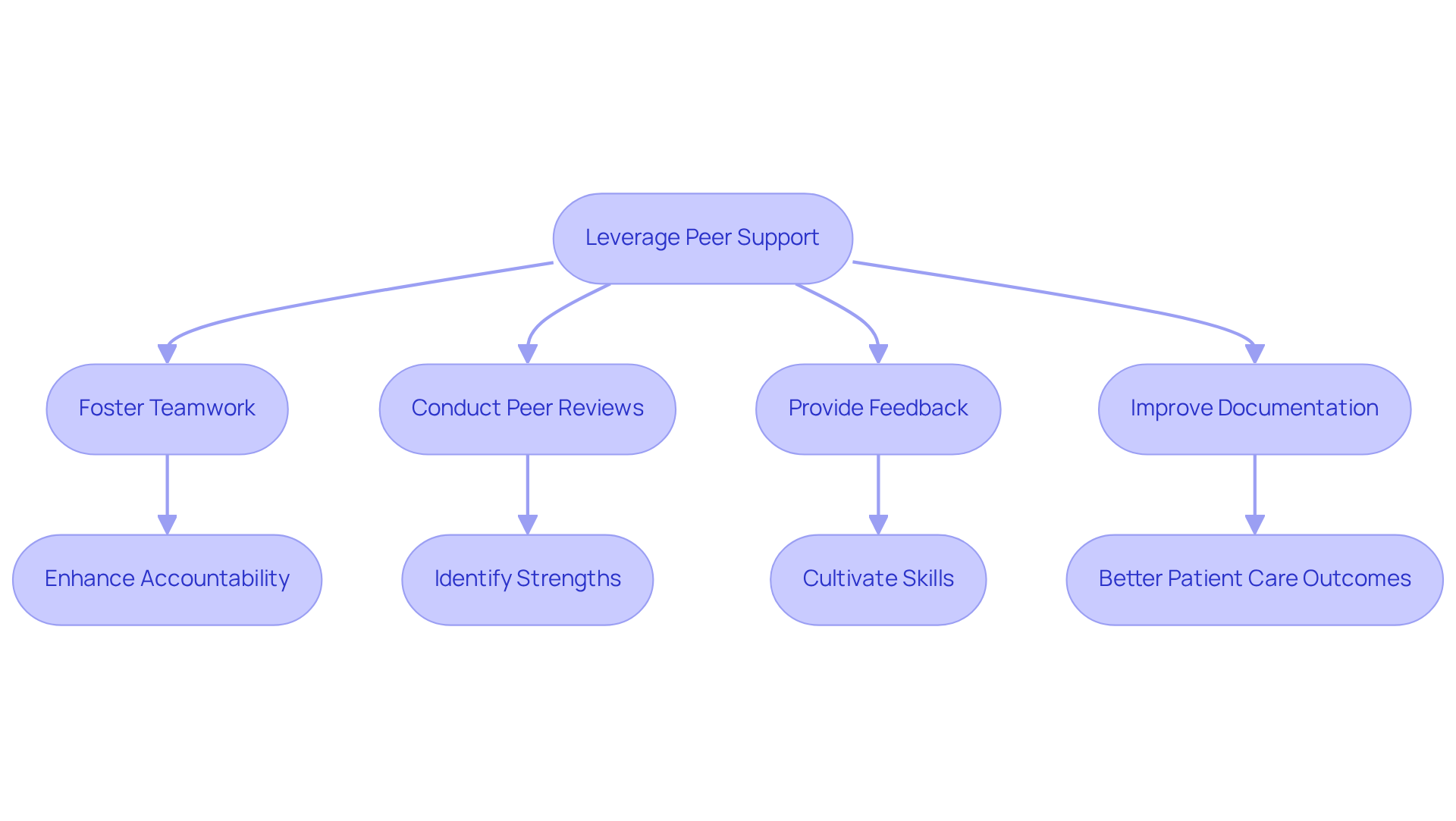
Healthcare providers often face emotional challenges, particularly when it comes to record-keeping. The administrative burdens can weigh heavily, impacting the quality of patient care. However, employing peer support can significantly enhance these methods. By fostering an environment of teamwork and collective learning, medical teams can ensure that clear, concise, and complete medical record documentation results in better record-keeping abilities and effective sharing of best practices.
Imagine the difference regular peer reviews and feedback sessions can make. They not only help identify strengths and areas for improvement but also cultivate a sense of accountability and teamwork. This collaborative approach enhances individual skills and contributes to a more cohesive and effective medical team. Ultimately, clear, concise, and complete medical record documentation results in .
Data suggests that clear, concise, and complete medical record documentation results in better accuracy for medical teams participating in collaborative learning. Research shows that such methods can decrease mistakes by as much as 30%. For instance, a peer support program in Texas demonstrated that clear, concise, and complete medical record documentation results in better collaborative efforts across clinical locations, which led to a 25% improvement in record quality. This highlights the tangible benefits of teamwork in medical environments.
By embracing peer support, you can take a step towards alleviating some of the pressures you face. Consider how this practice could transform your team's dynamics and enhance the care you provide. Together, we can create a supportive network that not only uplifts each other but also ultimately benefits our patients.
Link Structured Documentation to Improved Patient Care Outcomes
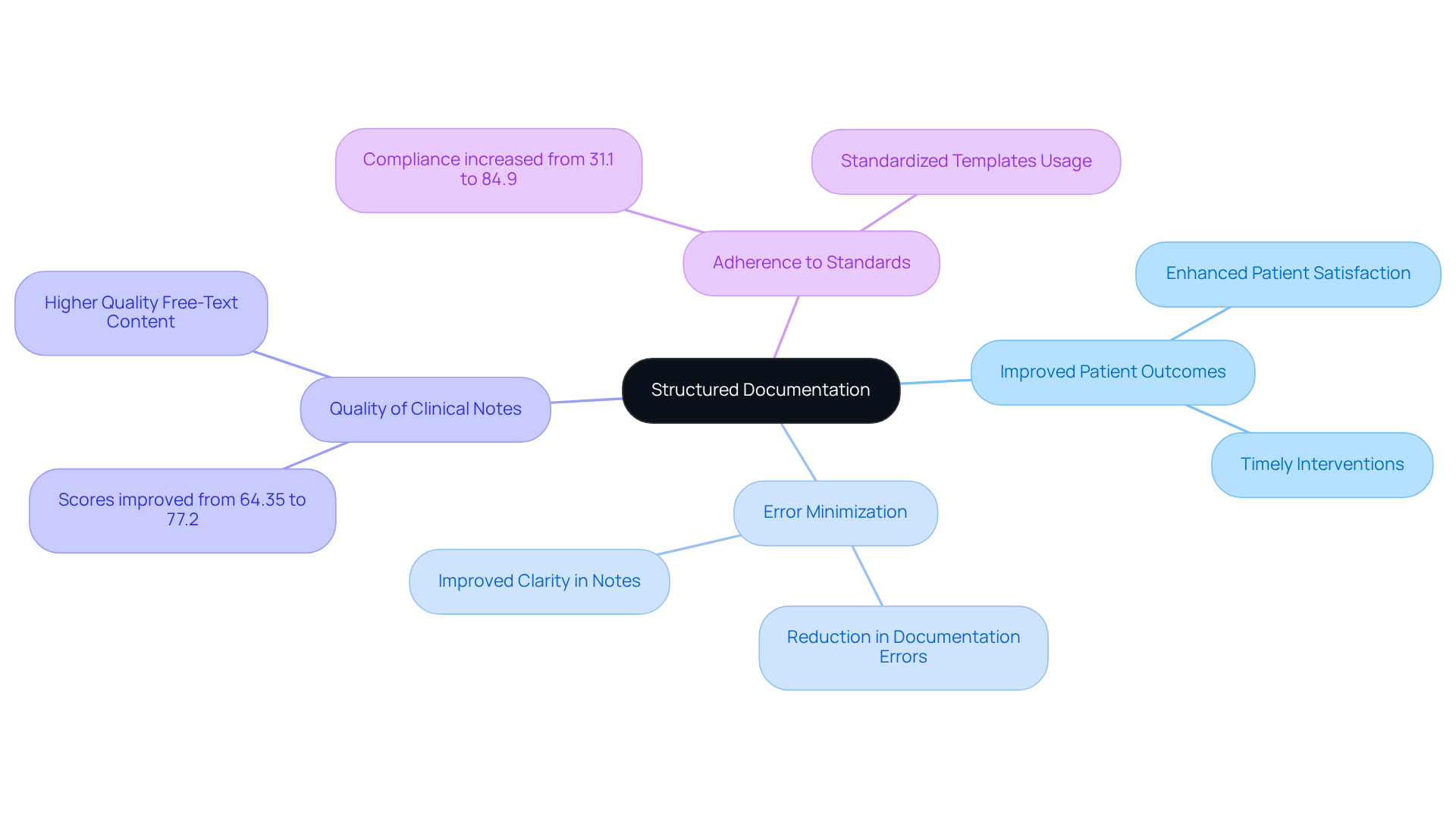
Clear, concise, and complete medical record documentation results in better health outcomes by ensuring that all relevant information is gathered systematically and readily accessible. Have you ever felt overwhelmed by the sheer volume of patient data? When healthcare providers implement , they ensure that clear, concise, and complete medical record documentation results in better retrieval of essential patient information, which supports informed decision-making and timely interventions. This approach emphasizes that clear, concise, and complete medical record documentation results in better minimization of errors, ultimately elevating the quality of care provided.
For instance, studies have shown that organized records lead to a remarkable improvement in the quality of clinical notes, with scores rising from 64.35 to 77.2 post-implementation. Furthermore, adopting structured templates has been linked to a boost in adherence to record-keeping standards, increasing from 31.1% to 84.9%. By embracing these methods, medical providers can enhance patient outcomes and satisfaction, fostering a more efficient healthcare environment.
Imagine the difference it could make in your practice. By prioritizing organized records, you ensure that clear, concise, and complete medical record documentation results in better workflow and that your patients receive the best possible care. Let's work together to create a supportive and effective medical setting for everyone.
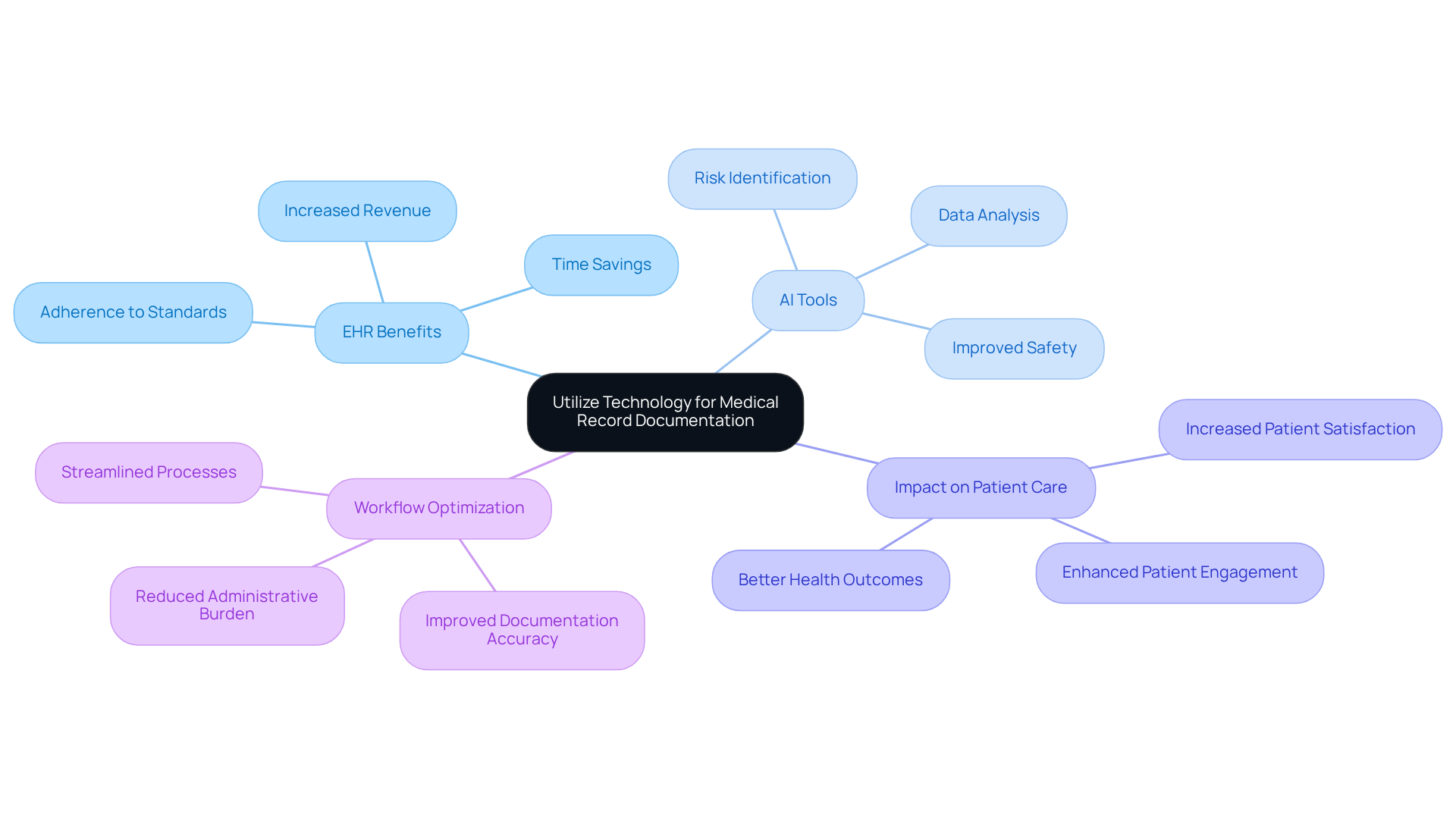
Utilize Technology to Facilitate Efficient Medical Record Documentation
In the demanding world of healthcare, providers often grapple with overwhelming administrative burdens. The incorporation of technology, particularly electronic health records (EHRs) and AI-driven record-keeping tools, can significantly alleviate these pressures. These sophisticated systems not only streamline regular tasks but also reduce the time service providers spend on record-keeping, allowing them to focus more on what truly matters—patient care.
Imagine a scenario where healthcare professionals can dedicate more time to assisting individuals rather than getting bogged down by paperwork. EHRs have been shown to enhance the utilization of specific ICD codes, leading to increased revenue and improved adherence to record-keeping standards. By optimizing workflows, technology empowers healthcare providers to deliver better quality service to individuals, ultimately fostering a more supportive environment for patients.
Moreover, studies reveal that clear, concise, and complete medical record documentation results in better outcomes and higher patient satisfaction. AI tools can analyze data trends, helping providers make informed choices and identify health risks. This not only improves safety but also elevates the quality of services offered.
As we embrace these advancements, let’s reflect on how we can further support each other in navigating these changes. How can we ensure that technology serves as a tool for compassion in our practice? Together, we can create a that prioritizes both efficiency and empathy.
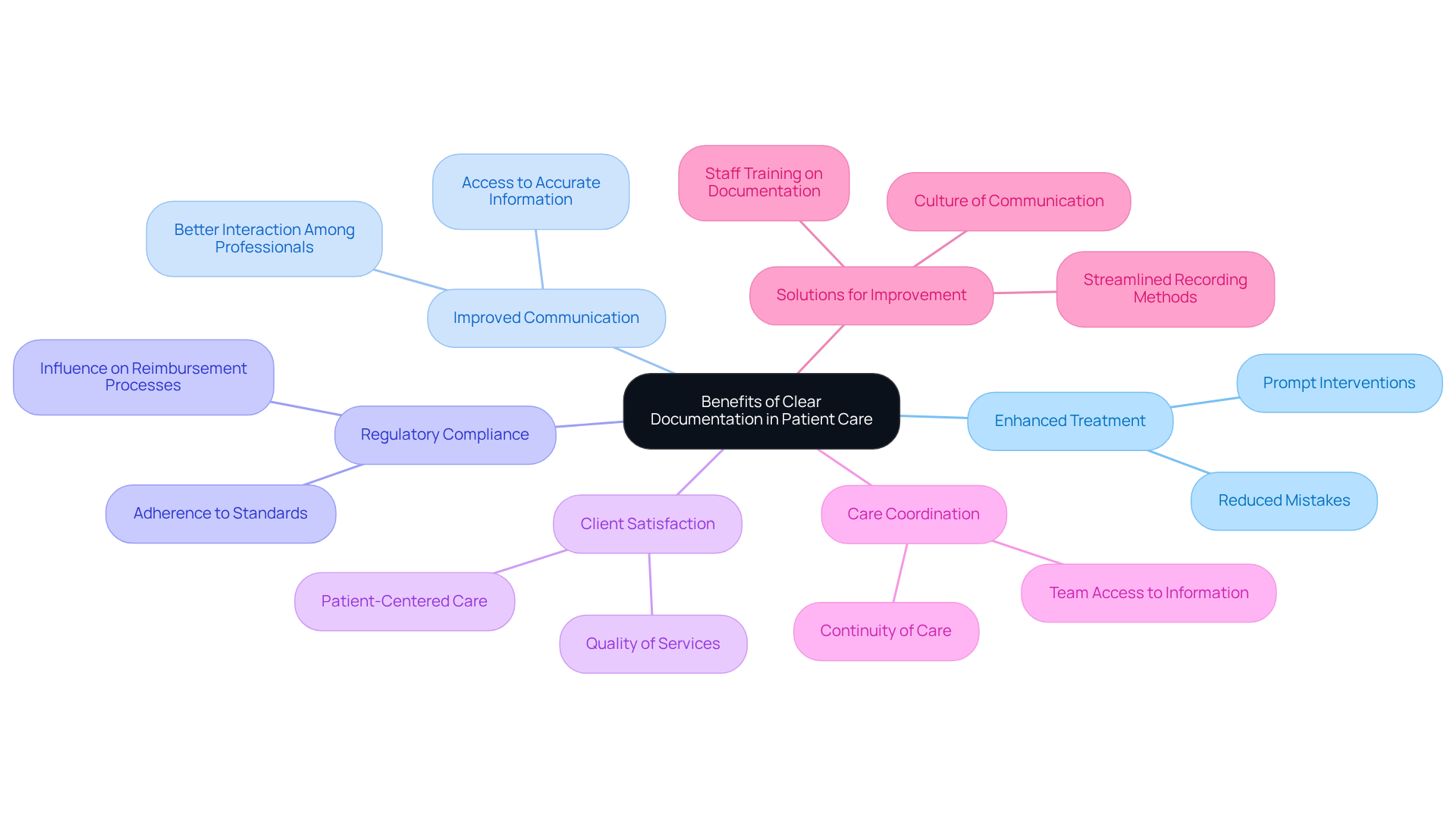
Recognize the Overall Benefits of Clear Documentation for Patient Care
The importance of clear, concise, and complete medical record documentation results in better enhancement of individual treatment. Superior records ensure that clear, concise, and complete medical record documentation results in better interaction among medical professionals and reduces the likelihood of mistakes, thereby ensuring individuals receive prompt and suitable interventions. Have you ever considered how much time medical professionals dedicate to record-keeping compared to direct interaction with those they treat? This highlights the necessity for effective recording methods that do not diminish engagement with clients.
Additionally, comprehensive records are crucial for adhering to regulatory standards, which can directly influence reimbursement processes. By emphasizing that clear, concise, and complete medical record documentation results in better quality of services, medical professionals can elevate the quality of services provided, boost client satisfaction, and improve outcomes. Effective documentation practices demonstrate that clear, concise, and complete medical record documentation results in better care coordination, ensuring that all team members have access to accurate and up-to-date patient information.
Ultimately, this fosters a . Let’s work together to focus on enhancing our documentation practices, so we can provide the best possible care for our clients. Here are some key solutions:
- Implement streamlined recording methods.
- Prioritize training for staff on effective documentation.
- Foster a culture of communication among team members.
By addressing these areas, we can create a more compassionate and effective healthcare experience for everyone involved.
Conclusion
Clear, concise, and complete medical record documentation is not just a requirement; it is essential for enhancing patient care and improving overall healthcare outcomes. Have you ever considered how effective documentation practices can transform your daily routines? By prioritizing these practices, healthcare providers can ensure that vital information is accurately recorded and readily accessible, leading to better decision-making and timely interventions. This emphasis on documentation not only streamlines administrative workflows but also fosters a culture of accountability and collaboration among healthcare teams.
Throughout this discussion, we have seen how adopting AI technology, implementing standardized procedures, and leveraging peer support can significantly improve documentation quality. Imagine reducing administrative burdens while ensuring compliance with regulatory standards—these strategies collectively enhance the efficiency of healthcare delivery. Moreover, the positive correlation between meticulous record-keeping and reduced legal risks underscores the necessity for comprehensive documentation practices in safeguarding both patient safety and provider accountability.
As the healthcare landscape continues to evolve, embracing these documentation improvements is crucial for fostering a more compassionate and effective care environment. By actively working towards better documentation practices, healthcare providers can enhance their operational efficiency while prioritizing patient well-being. Remember, the commitment to clear, concise, and complete medical records is a vital step in ensuring that every patient receives the high-quality care they deserve. Let’s take this journey together, improving our practices for the benefit of all.




