Overview
This article highlights an important step towards enhancing patient care: integrating behavioral health services within primary care settings. Have you ever considered the emotional challenges healthcare providers face when trying to address both mental and physical health needs? By implementing strategies such as co-location of services, warm hand-offs, and universal screening, we can significantly improve patient outcomes. These methods not only address mental health needs alongside physical health care but also foster a more holistic approach to patient well-being.
Imagine the impact of a system where mental health support is seamlessly woven into primary care. This integration allows us to respond to the whole person, ensuring that no aspect of health is overlooked. It’s about creating an environment where patients feel understood and supported in all their health journeys. By recognizing and addressing these intertwined needs, we can cultivate a more compassionate healthcare experience.
As we move forward, let’s embrace these strategies and work together to enhance patient care. How can we further engage with these solutions to make a meaningful difference in our practices? Together, we can create a healthcare system that truly supports the mental and physical health of every patient.
Introduction
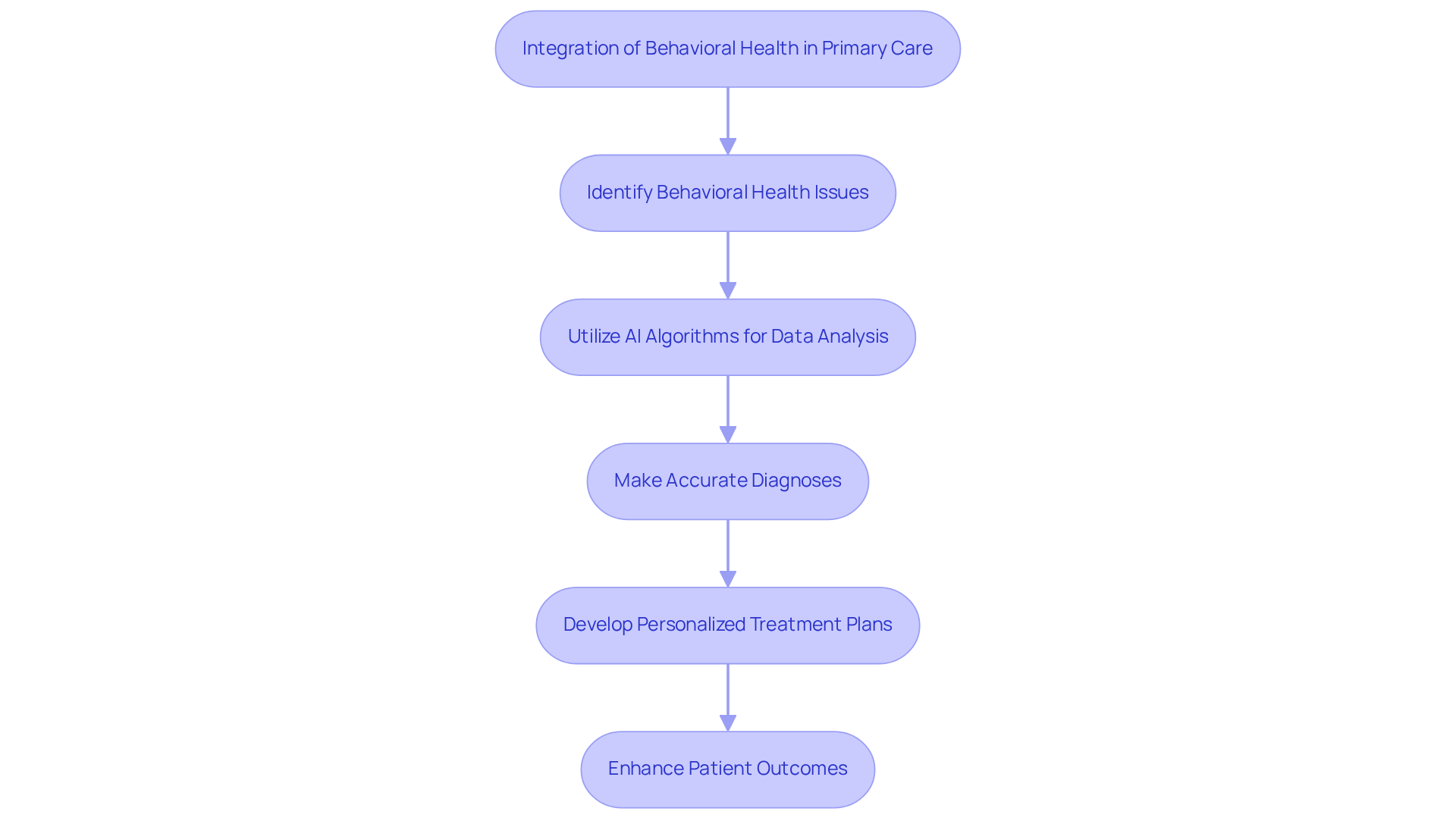
Integrating behavioral health into primary care is not merely a trend; it’s an essential step towards enhancing patient outcomes in our increasingly complex healthcare landscape. By addressing mental well-being alongside physical health, primary care providers can unlock a holistic approach that fosters improved diagnoses and personalized treatment plans.
However, as the demand for effective care continues to rise, how can healthcare systems ensure they are not only meeting these needs but also nurturing a supportive environment for patients? This article delves into best practices for integrating behavioral health services, revealing strategies that empower both providers and patients on their journey towards comprehensive wellness.
In recognizing the emotional challenges faced by healthcare providers, we can better understand how administrative burdens impact patient care. Together, let’s explore solutions that not only enhance the quality of care but also create a compassionate atmosphere for those we serve.
Define Behavioral Health in Primary Care
Individuals may encounter behavioral health issues that encompass a range of mental well-being and substance use disorders, such as anxiety, depression, and addiction. In primary care, this means integrating these aspects into routine healthcare practices to encounter behavioral health. Why is this integration so important? It allows providers to effectively encounter behavioral health needs while addressing physical wellness needs simultaneously, leading to better outcomes for individuals.
AI algorithms, particularly machine learning, can analyze vast amounts of medical data, including histories, symptoms, and test results. This capability supports physicians in making accurate diagnoses and developing personalized treatment plans. Did you know that approximately 80% of individuals with mental disorders visit a primary physician at least once a year? This statistic underscores the primary care setting as a crucial environment where we can encounter behavioral health for of these conditions.
By clearly defining mental wellness and leveraging advanced algorithms, providers can more effectively encounter behavioral health signs and symptoms in their patients. This enables prompt and appropriate assistance. For example, research indicates that AI-driven tools can reduce diagnosis time by up to 30%, significantly improving patient outcomes.
In light of these advancements, how can we further support our healthcare providers? By embracing these technologies, we can foster a more compassionate approach to care that prioritizes the emotional and mental well-being of those we serve.
Integrate Behavioral Health Services Effectively
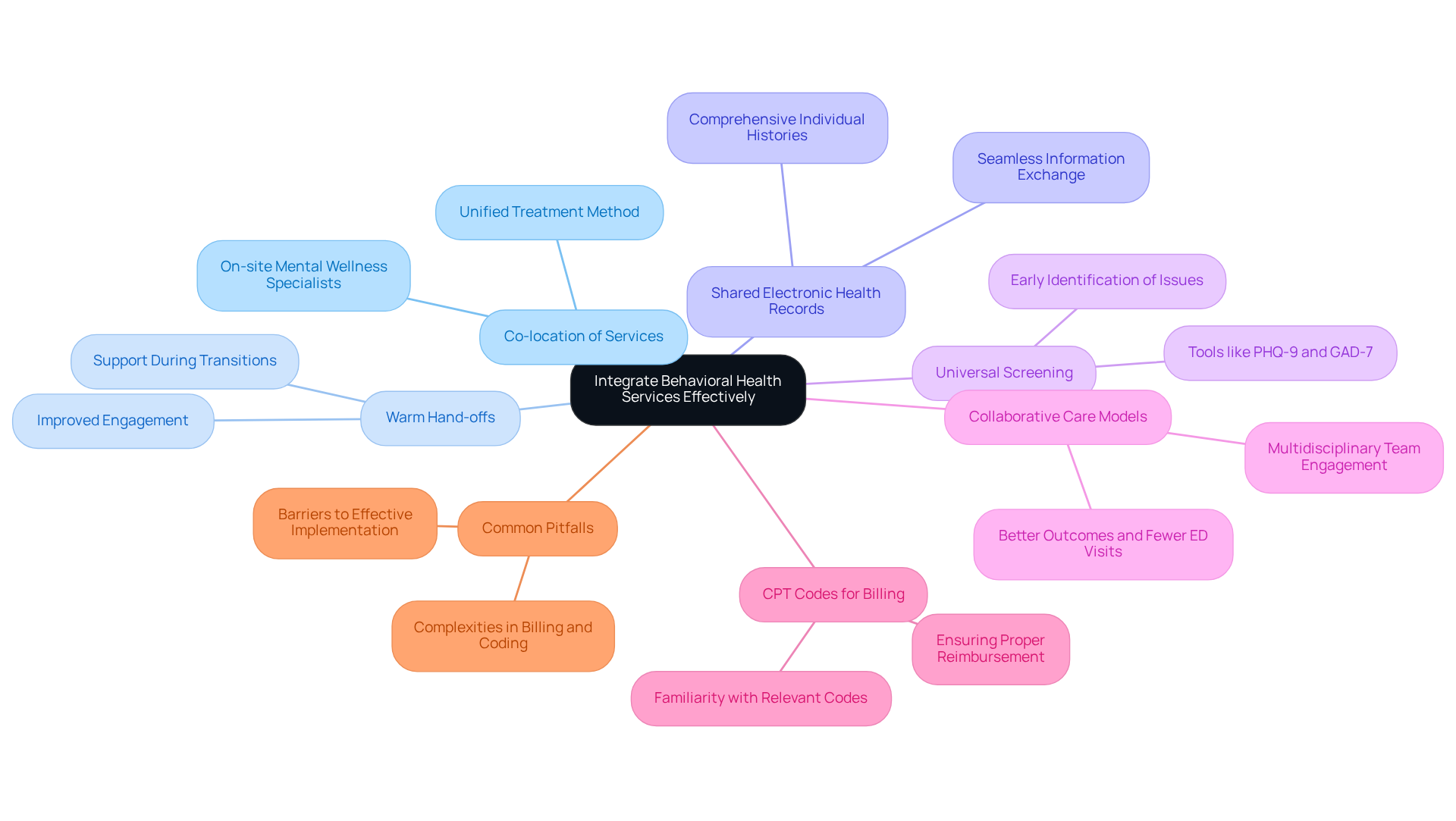
To effectively integrate behavioral health services, primary care practices can adopt several key strategies:
- Co-location of Services: Positioning mental wellness specialists on-site enables prompt consultation and teamwork, improving communication and continuity of support. Research shows that co-located services greatly enhance outcomes for individuals who encounter behavioral health challenges by promoting a more unified treatment method.
- Warm Hand-offs: Implementing warm hand-offs between primary care and those who encounter behavioral health providers ensures that individuals feel supported and understood during transitions in care. This approach has been demonstrated to improve engagement and satisfaction, as it alleviates the anxiety frequently linked with referrals to encounter behavioral health.
- Shared Electronic Health Records (EHR): Utilizing a shared EHR system allows for seamless information exchange, enabling providers to access comprehensive individual histories and treatment plans. This integration is essential for coordinated support, as it ensures all team members are informed about the individual's progress and needs.
- Universal Screening: Consistently assessing all patients can help to encounter behavioral health issues early, resulting in prompt interventions. Tools such as the can be easily incorporated into routine evaluations, encouraging proactive support. Almost one in five adults in the U.S. encounter behavioral health issues or substance use disorders annually, highlighting the significance of these evaluations.
- Collaborative Care Models: Implementing frameworks like the Collaborative Care Model (CoCM) is essential to encounter behavioral health issues by engaging a multidisciplinary team, including care managers and psychiatrists, to coordinate care efficiently. Studies indicate that CoCM can result in better outcomes and fewer emergency department visits. As Ellen Harvey observes, "Extensive studies show that when practices encounter behavioral health services alongside physical medicine, it promotes overall well-being enhancements."
- CPT Codes for Billing: Providers should familiarize themselves with relevant CPT codes, such as 96127 for Mental Wellness Screening, to ensure proper billing and reimbursement for integrated wellness services.
- Common Pitfalls: It is essential to be aware of common traps in integrating wellness services, such as complexities in billing and coding for wellness consultants, which can hinder effective implementation.
By implementing these strategies, primary service providers can cultivate a more integrated and responsive healthcare setting that addresses both physical wellness and encounter behavioral health requirements, ultimately enhancing service delivery. Case studies, like Bill's smoking cessation journey and Cecelia's integrated wellness experience, demonstrate the real-world effect of these practices.
Engage Patients with Lived Experience
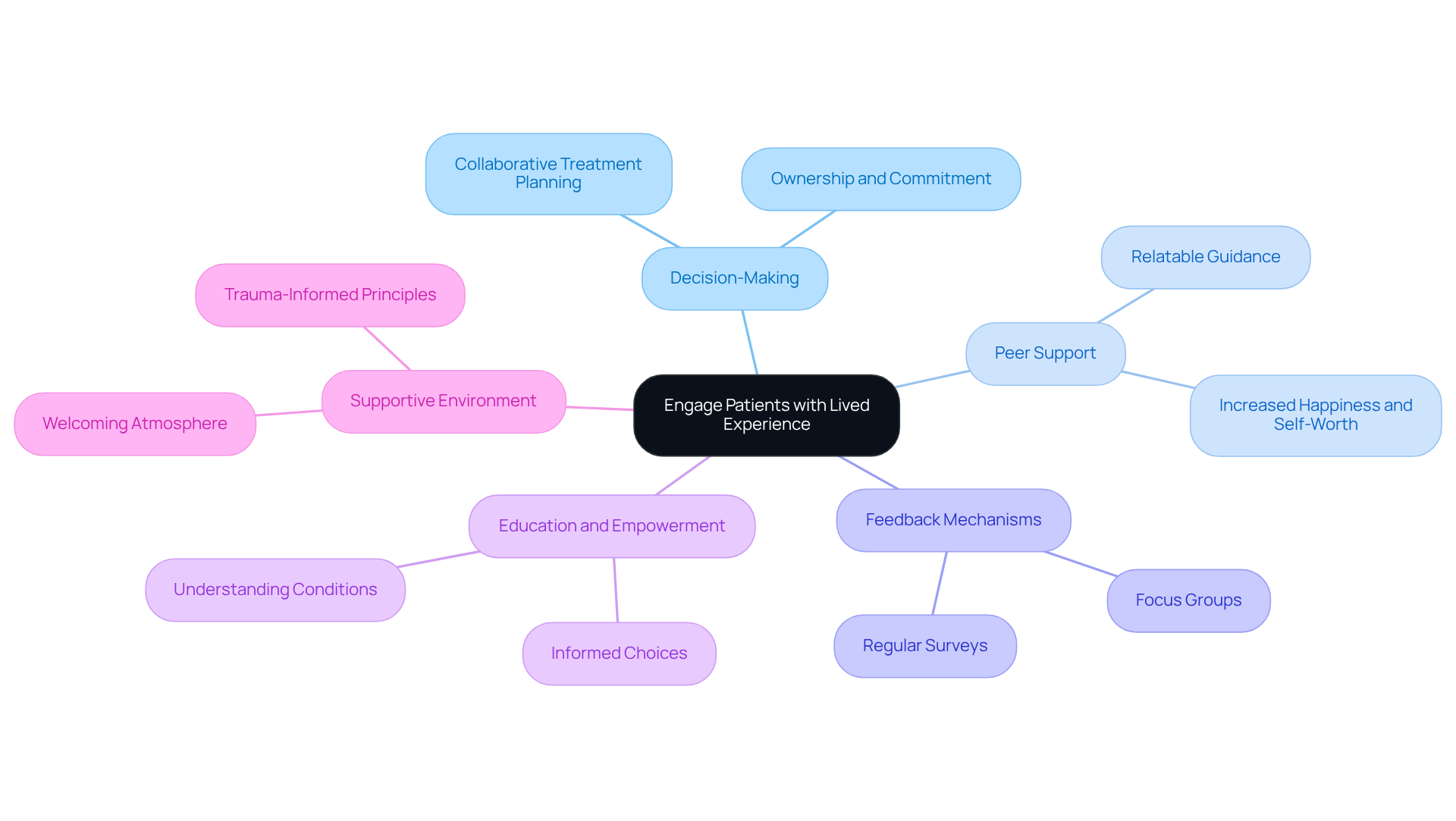
Involving individuals with lived experience to encounter behavioral health services significantly improves treatment effectiveness. Have you considered how their insights can transform care? Here are best practices for fostering this vital engagement:
- Engage Individuals in Decision-Making: Encourage individuals to actively participate in their treatment planning by discussing their preferences, goals, and concerns. This collaborative approach fosters a sense of ownership and commitment to their care, which helps to encounter behavioral health and leads to improved outcomes.
- Utilize Peer Support: Incorporating peer support specialists who have faced similar challenges offers individuals relatable guidance and encouragement. Research indicates that peer support can result in greater happiness, self-worth, and efficient coping, thus improving engagement and motivation.
- Feedback Mechanisms: Establish regular feedback channels, such as surveys or focus groups, to gather insights from individuals about their experiences and suggestions for improvement. This feedback can guide practice adjustments and improve service provision, ensuring that support aligns with individual needs.
- Education and Empowerment: Provide educational resources that enable individuals to understand their conditions and treatment options. Informed individuals are more inclined to make educated choices and engage actively in their treatment, which is vital for successful planning.
- Create a Supportive Environment: Foster a welcoming and non-judgmental atmosphere in the practice where individuals feel safe to share their experiences and challenges. Applying trauma-informed principles and educating staff to be attentive to individual needs can greatly improve the therapeutic atmosphere.
By actively engaging patients with lived experience, primary care providers can better encounter behavioral health issues and create a more inclusive and effective healthcare environment that prioritizes patient needs and enhances overall care quality. Together, let’s embrace these practices to and foster healing.
Conclusion
Integrating behavioral health into primary care is essential for addressing the comprehensive needs of patients, encompassing both mental wellness and physical health. This holistic approach not only enhances the quality of care but also leads to improved outcomes, as healthcare providers can identify and manage behavioral health issues alongside physical ailments.
Key strategies for successful integration include:
- Co-locating services
- Implementing warm hand-offs
- Utilizing shared electronic health records
- Conducting universal screenings
These practices ensure that patients receive timely and coordinated care, fostering a supportive environment that prioritizes their overall well-being. Have you considered how engaging individuals with lived experience can enrich the treatment process? Their insights can significantly enhance the effectiveness of care and promote a sense of ownership in their health journey.
The importance of integrating behavioral health services in primary care cannot be overstated. As the healthcare landscape continues to evolve, embracing these practices will not only uplift communities but also empower individuals to take charge of their health. By prioritizing behavioral health, healthcare providers can create a more inclusive, compassionate, and effective system that ultimately leads to healthier lives and stronger communities. Let’s work together to make this vision a reality.




