Overview
Creating an effective nursing report sheet for multiple patients is not just a task; it’s a vital part of ensuring that communication during shift transitions is accurate and compassionate. This process ultimately enhances patient safety and care continuity, which we all deeply care about.
Have you ever felt the weight of administrative burdens impacting your ability to provide the best care? This article highlights the importance of incorporating key components like:
- Client demographics
- Medical history
- Current medications
By embracing best practices such as standardization and prioritization of information, we can significantly improve the efficiency of handoffs and reduce documentation errors.
Imagine the peace of mind that comes with knowing that every detail is communicated clearly. By streamlining our reporting processes, we not only support each other as healthcare providers but also ensure our patients receive the highest level of care.
Let’s work together to enhance our communication strategies, fostering a supportive environment that prioritizes patient well-being. What steps can you take today to improve your nursing report sheets? Together, we can make a meaningful difference.
Introduction
In the fast-paced and often chaotic environment of healthcare, effective communication is essential for ensuring patient safety and delivering quality care. The nursing report sheet for multiple patients stands out as a vital tool, streamlining the handoff process and significantly reducing the risk of errors during shift transitions.
By delving into the essential components and best practices for creating these report sheets, healthcare professionals can enhance their workflow and ultimately improve patient outcomes.
Yet, how can nurses balance the demands of thorough documentation with the need for efficiency in such a high-pressure setting? This question resonates deeply with those in the field, highlighting the emotional challenges they face daily.
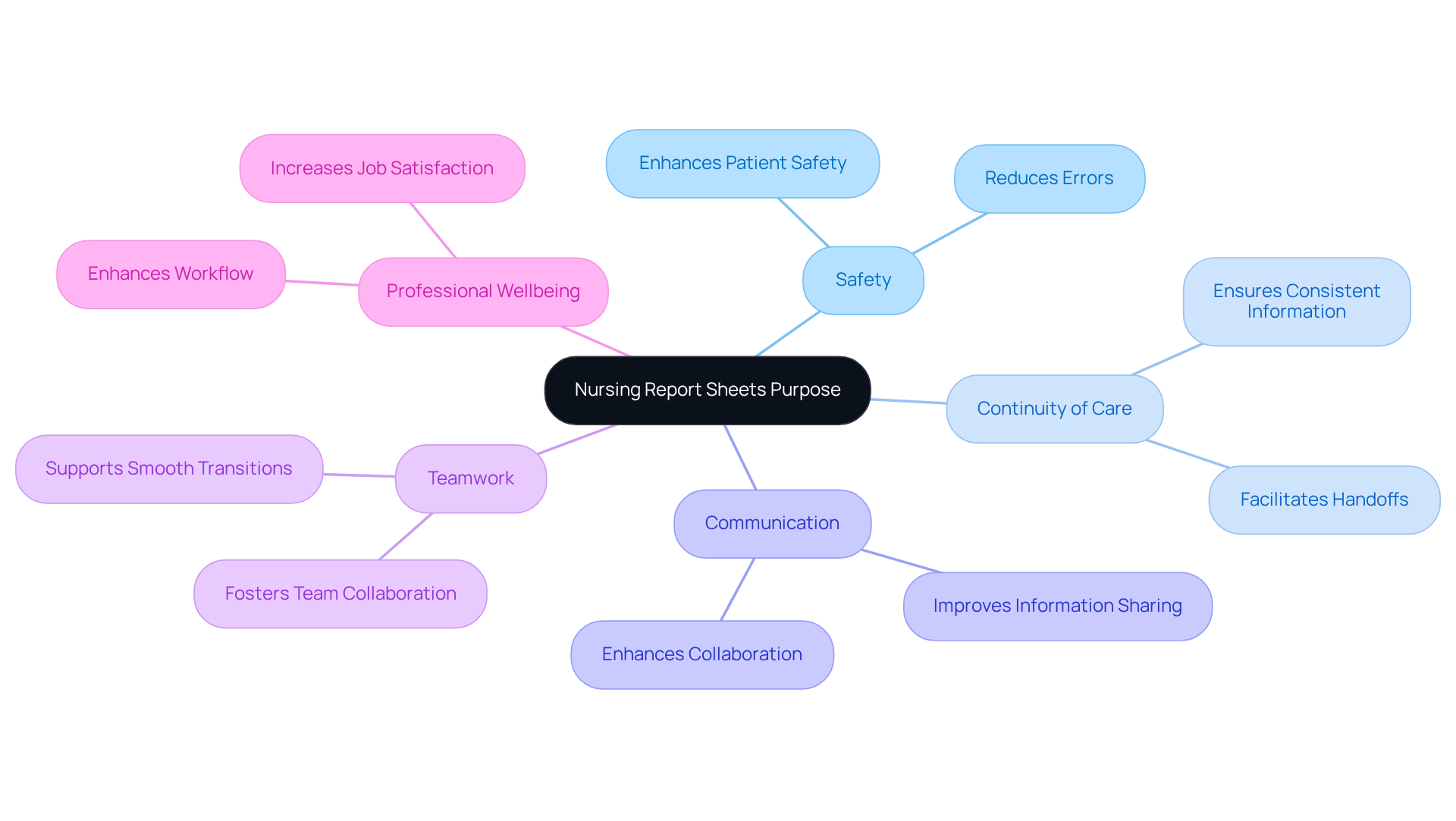
Understand the Purpose of Nursing Report Sheets
for multiple patients serves as an essential tool for caregivers, helping to record and share vital individual details during shift transitions. Have you ever felt overwhelmed during handoffs? These documents simplify the process, ensuring that crucial information about care, such as allergies, vital signs, and medications, is communicated accurately and effectively.
By utilizing a nursing report sheet for multiple patients, which can include checklists and organized layouts, nurses can uphold continuity of care. This significantly reduces the risk of errors and enhances overall safety for individuals, especially in a fragmented healthcare system where communication barriers often arise due to regulatory challenges like HIPAA. Studies reveal that a nursing report sheet for multiple patients can save time and minimize documentation errors, ultimately leading to better outcomes for individuals. For instance, hospitals that embraced organized documentation forms experienced a notable decline in negative incidents associated with communication breakdowns.
Moreover, these documents foster teamwork among healthcare professionals, facilitating smooth transitions and a comprehensive understanding of individual needs. By recognizing the purpose and benefits of nursing documentation, including their impact on job satisfaction and professional wellbeing, nurses can enhance their workflow. This contributes to a safer, more effective healthcare environment, particularly as innovative AI solutions continue to transform healthcare delivery.
Let's work together to ensure that every detail matters, creating a nurturing atmosphere for both patients and providers.
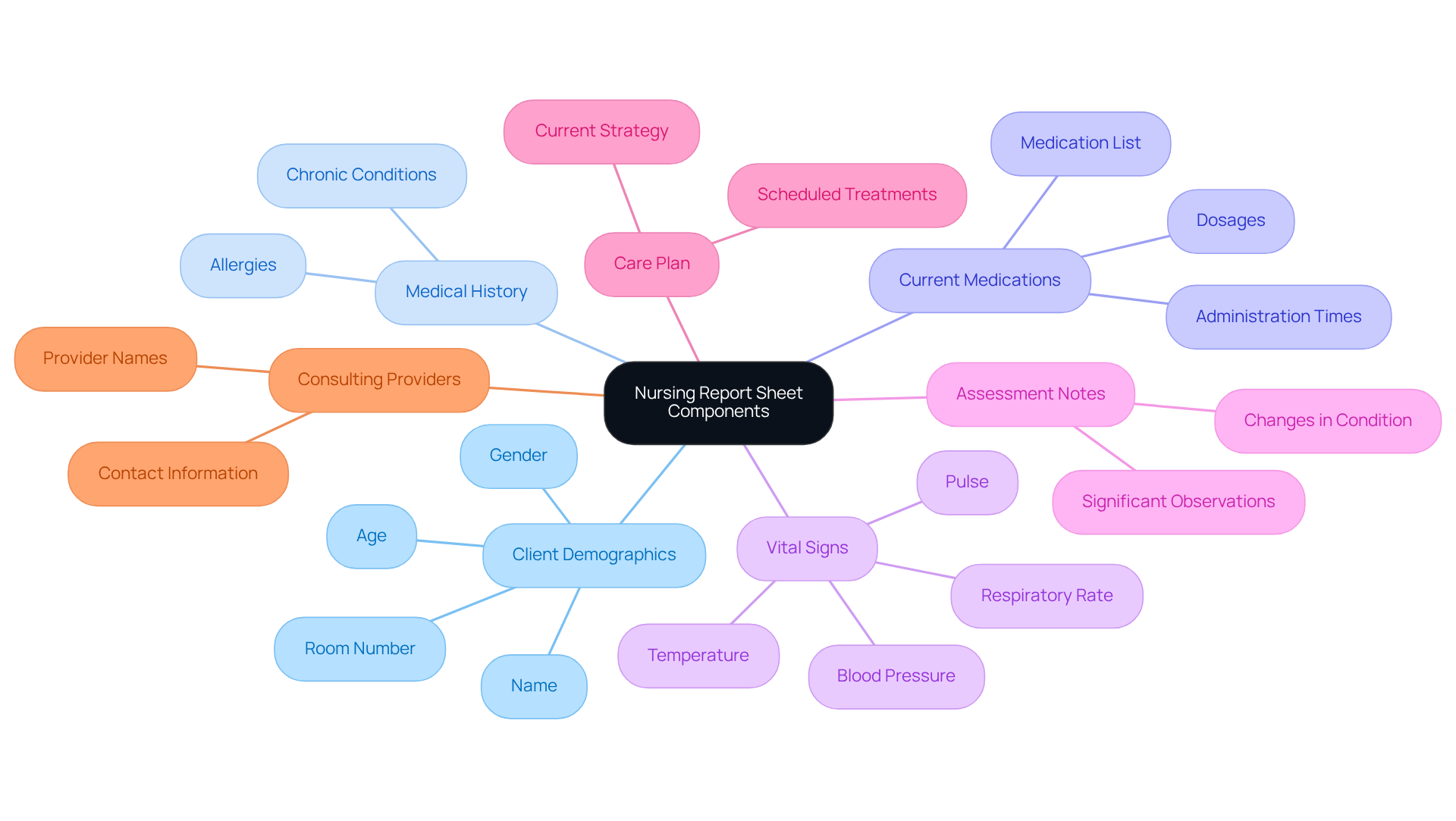
Identify Essential Components for Your Report Sheet
Creating a nursing report sheet for multiple patients that truly serves its purpose requires thoughtful attention to several essential elements. These elements not only foster clear communication but also support comprehensive care for individuals in need. Consider the following key components:
- Client Demographics: Capture the individual's name, age, gender, and room number to ensure accurate identification.
- Medical History: Record relevant medical history, including allergies and chronic conditions, which are vital for secure individual management.
- Current Medications: List all medications the individual is currently taking, specifying dosages and administration times to prevent errors.
- Vital Signs: Document the latest vital signs—temperature, pulse, blood pressure, and respiratory rate—to provide a snapshot of the individual's current health status.
- Assessment Notes: Include significant observations or changes in the individual's condition, which can inform ongoing care decisions.
- Care Plan: Outline the current care strategy, detailing treatments and interventions scheduled for the individual, ensuring continuity of care.
- Consulting Providers: Note any consulting providers involved in the individual's care for easy reference, promoting collaborative healthcare delivery.
Integrating these elements not only enhances the thoroughness of the nursing report sheet for multiple patients but also facilitates effective communication during shift transitions. It's important to acknowledge that many healthcare providers experience burnout—approximately 95% report feeling this way. By utilizing a structured documentation tool, you can enhance the handoff process, which ultimately boosts job satisfaction and improves outcomes for those receiving care.
Furthermore, consider how generative AI tools can alleviate some of the administrative burdens related to documentation preparation. This enables healthcare professionals to focus more on the they provide. By employing organized documentation and integrating AI solutions, nurses can lessen the administrative load contributing to burnout, allowing for greater focus on patient care. For practical resources, think about exploring free printable nursing documentation forms and templates available online to assist in crafting your own.
Apply Best Practices for Using Nursing Report Sheets
To maximize the effectiveness of nursing report sheets, it’s important to consider best practices that can truly make a difference in your daily routine and patient care:
- Standardization: Adopting a uniform format for your documentation can ensure consistency and ease of use across shifts. For example, the Mini SBAR Nursing Report Form supports 3 individuals per form, facilitating communication and enhancing the trustworthiness of the information exchanged among nursing personnel.
- Prioritize Information: Organizing the report sheet logically, placing the most critical data at the top, allows healthcare professionals to swiftly access vital information during transitions. This prioritization not only enhances safety but also supports continuity of care, which is so crucial in our field.
- Keep It Concise: Focusing on clarity by including only essential information is key. Utilizing bullet points to present data succinctly reduces clutter and makes it easier for nurses to absorb key details at a glance.
- Refresh Frequently: It’s essential to consistently revise the document during the shift to reflect any changes in the individual's condition or care strategy. This practice sustains precise and up-to-date information, which is critical for effective management of individuals receiving care.
- Engage in Handoffs: During shift changes, actively interacting with the incoming nurse using the documentation as a guide fosters discussions around key points and addresses any questions. This collaborative method promotes improved communication and a better understanding of client needs.
- Utilize Technology: Consider leveraging digital tools or templates that simplify the creation and sharing of report documents. For instance, the Full-Size SBAR Nurse Report Template accommodates 1 individual per document, while is designed for 4 individuals, perfect for med surg and tele units. Technology can enhance efficiency and ensure that all team members have access to the most up-to-date information.
By embracing these best practices, nurses can significantly enhance their communication, ensuring a smooth transition of care between shifts and ultimately improving patient outcomes. Remember, every small step we take can lead to a greater impact on the lives we touch.

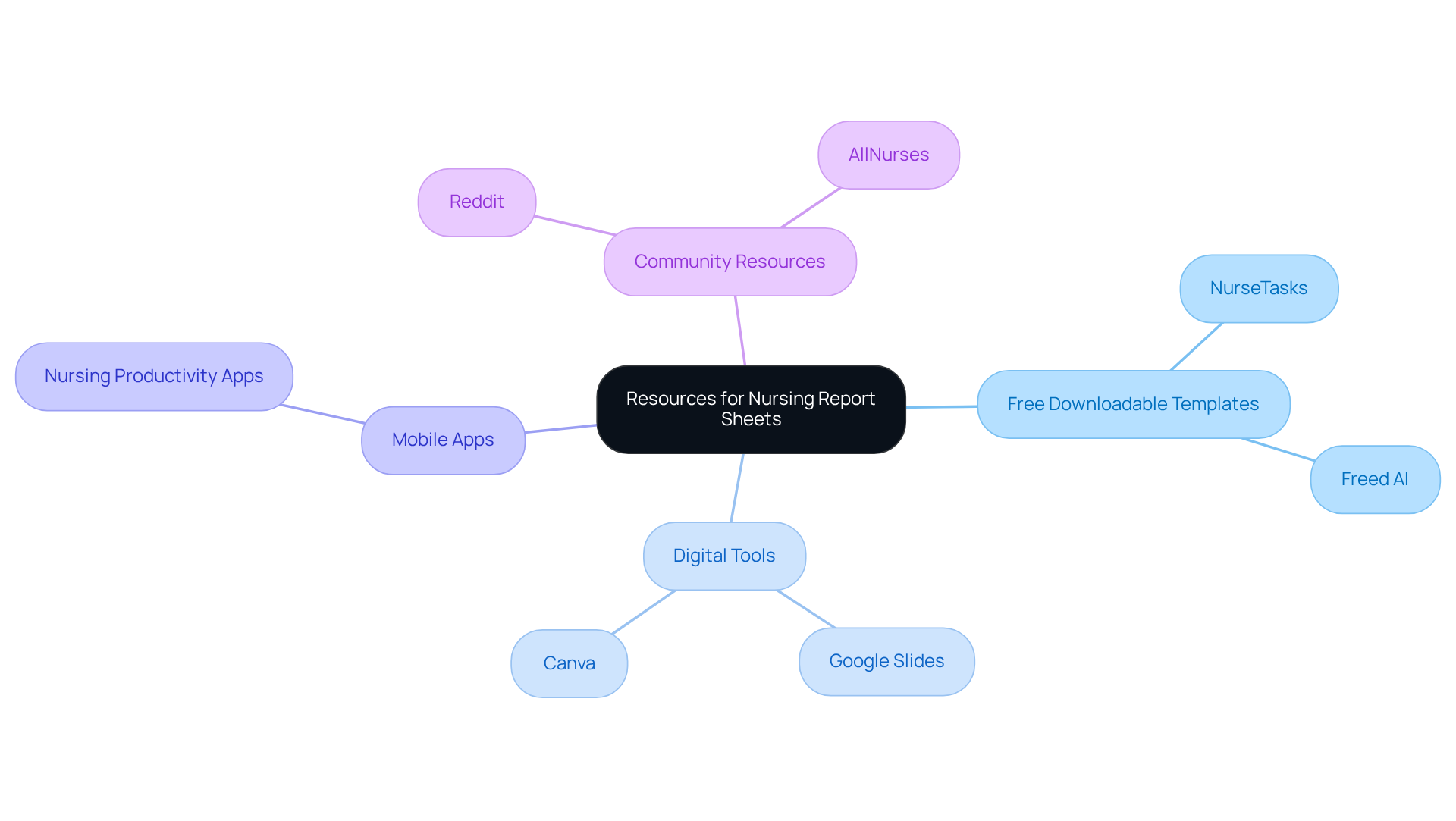
Access Templates and Tools for Report Sheet Creation
Creating nursing report sheets can often feel overwhelming, but there are several resources available to help ease this burden:
- Free Downloadable Templates: Websites like NurseTasks and Freed AI offer complimentary nursing documentation templates that can be tailored to your specific needs. Designed for up to four individuals, these templates are perfect for various nursing environments.
- Digital Tools: Platforms such as Google Slides or Canva can be utilized to craft visually appealing and organized documents. These tools enhance , which is essential when healthcare providers may care for up to eight patients in MedSurg settings.
- Mobile Apps: Explore nursing productivity applications that come with integrated documentation templates, allowing for convenient updates while on the go. These apps can help reclaim precious hours each day that might otherwise be consumed by routine administrative tasks.
- Community Resources: Engage with healthcare communities on platforms like Reddit or AllNurses to share and obtain examples and advice from fellow professionals. As Kathleen Gaines, News and Education Editor, wisely notes, 'Some healthcare professionals will read it from top to bottom, while others will arrange it according to systems,' highlighting the importance of customizing documentation to fit personal preferences.
By tapping into these resources, nurses can streamline the process of creating a nursing report sheet for multiple patients, which ultimately enhances care and communication for their patients. The implementation of a nursing report sheet for multiple patients has been shown to bolster accountability and patient safety, ensuring that vital information is readily accessible during shifts.
Conclusion
Utilizing a nursing report sheet for multiple patients is more than just a strategy; it’s a vital tool for enhancing communication and ensuring the safety of care delivery. These resources not only streamline the handoff process between nurses but also play a significant role in maintaining continuity of care. By implementing a well-structured report sheet, healthcare professionals can effectively manage crucial information, ultimately leading to improved patient outcomes.
Key components such as client demographics, medical history, current medications, and vital signs are essential for creating an effective nursing report sheet. Best practices, including standardization, prioritization of information, and the use of digital tools, further enhance the efficiency of this documentation process. Have you ever considered how organized communication can reduce errors and alleviate burnout? The insights shared throughout this article highlight the profound impact that such communication can have, fostering teamwork among healthcare providers.
As the healthcare landscape continues to evolve, embracing innovative tools and practices becomes imperative. By prioritizing the development and utilization of nursing report sheets, caregivers can improve their workflow and create a more compassionate and effective care environment for their patients. Engaging with available resources—like templates and community support—can empower nurses to refine their documentation practices, ultimately enriching the quality of care provided to individuals in need. Let's commit to supporting one another in this journey toward better care.




