Overview
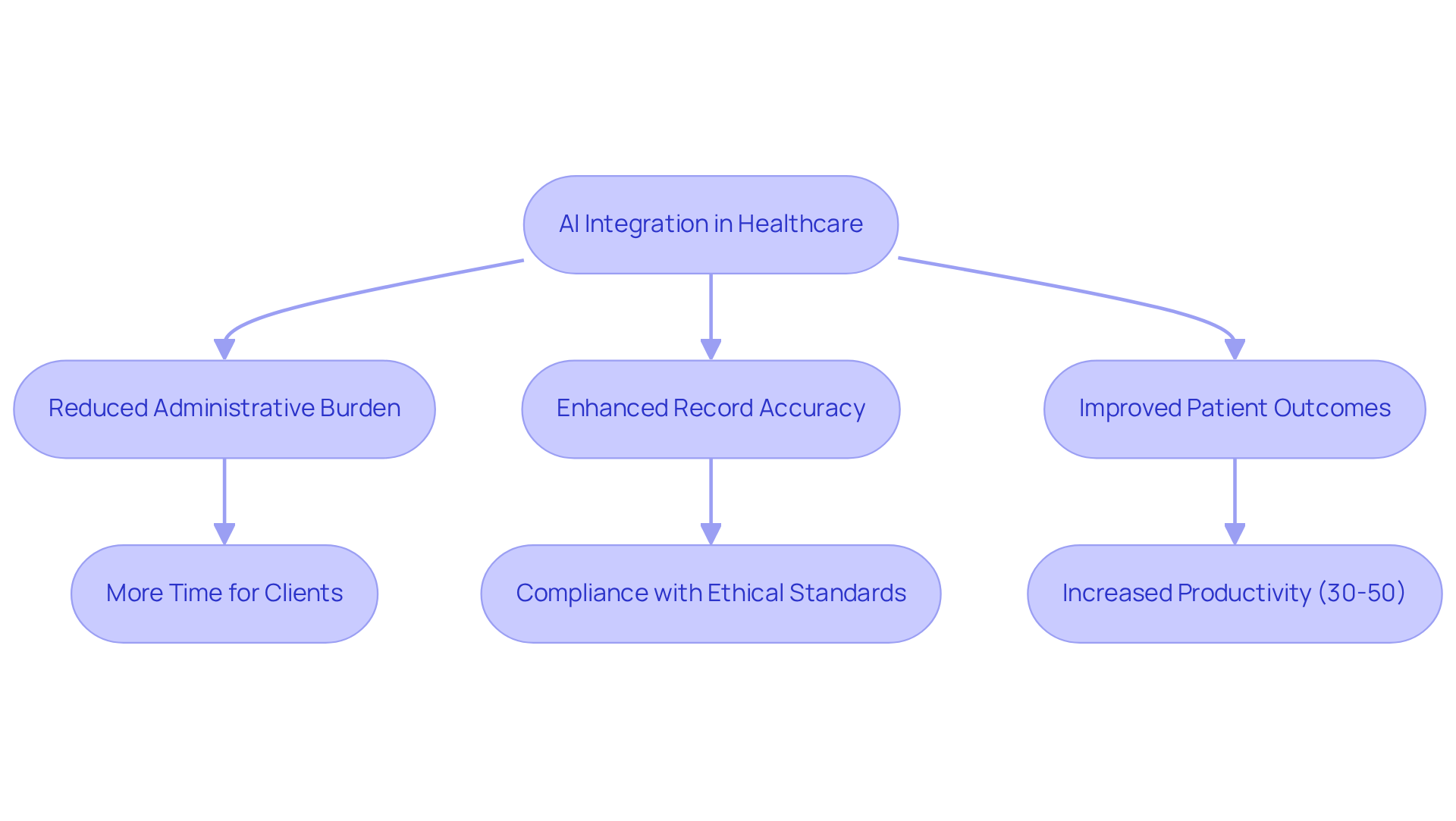
In the demanding world of healthcare, providers often face emotional challenges that can weigh heavily on their ability to deliver quality patient care. Administrative burdens can detract from the time and attention they wish to devote to their patients. This article focuses on enhancing patient documentation through effective SOAP plans, emphasizing the integration of AI to streamline these administrative processes.
Structured SOAP notes play a vital role in improving communication among healthcare teams. They significantly reduce documentation errors, allowing providers to concentrate more on what truly matters: patient care. As a result, this leads to better clinical outcomes, fostering a nurturing environment where patients feel valued and understood.
By adopting these practices, healthcare providers can alleviate some of their burdens, ultimately enriching their interactions with patients. We encourage you to explore how implementing structured SOAP plans can transform your documentation process and enhance the care you provide. Together, let’s work towards a future where administrative tasks no longer overshadow the compassionate care that every patient deserves.
Introduction
Healthcare providers often find themselves overwhelmed by administrative tasks that pull their focus away from what truly matters: patient care. This burden can lead to frustration and a sense of disconnect from their patients. However, the integration of AI-driven solutions, like those offered by CosmaNeura, presents a transformative opportunity to streamline the SOAP documentation process. By embracing these innovations, providers can enhance their efficiency and ultimately improve patient outcomes.
As the healthcare landscape continues to evolve, it’s crucial for practitioners to adapt their documentation practices. How can they harness these advancements while ensuring compliance and maintaining the quality of care? By reflecting on these questions, healthcare providers can take proactive steps toward a more efficient and compassionate practice. Together, we can navigate these challenges and foster a healthcare environment that prioritizes both provider well-being and patient care.
CosmaNeura: AI-Driven SOAP Plan Automation for Healthcare Providers
often face overwhelming administrative burdens that distract from their primary mission: caring for clients. and utilizes advanced to enhance the development of care plans. By , our platform enables providers to concentrate more on their clients instead of becoming overwhelmed by paperwork.
Imagine a world where , particularly for faith-centered healthcare practices. This innovative strategy significantly reduces the time spent on , enabling healthcare providers to devote more energy to those they serve. Recent advancements in AI demonstrate that automated systems can improve record accuracy and speed, with studies showing that AI can boost healthcare employee productivity by 30-50%.
Furthermore, expert insights reveal that for documentation leads to better outcomes for individuals through . As the healthcare landscape evolves, the role of AI in alleviating administrative burdens becomes increasingly clear, positioning it as an essential tool for providers seeking to .
CosmaNeura's solutions directly address the concerns of healthcare providers, particularly regarding the quality of care and interactions with individuals. By doing so, we help alleviate resistance to innovation. However, we must also acknowledge the importance of individual privacy and data security, ensuring these concerns are addressed as AI technologies integrate into healthcare workflows. Together, we can create a more compassionate and .
SOAP Note Structure: Key Components for Effective Documentation
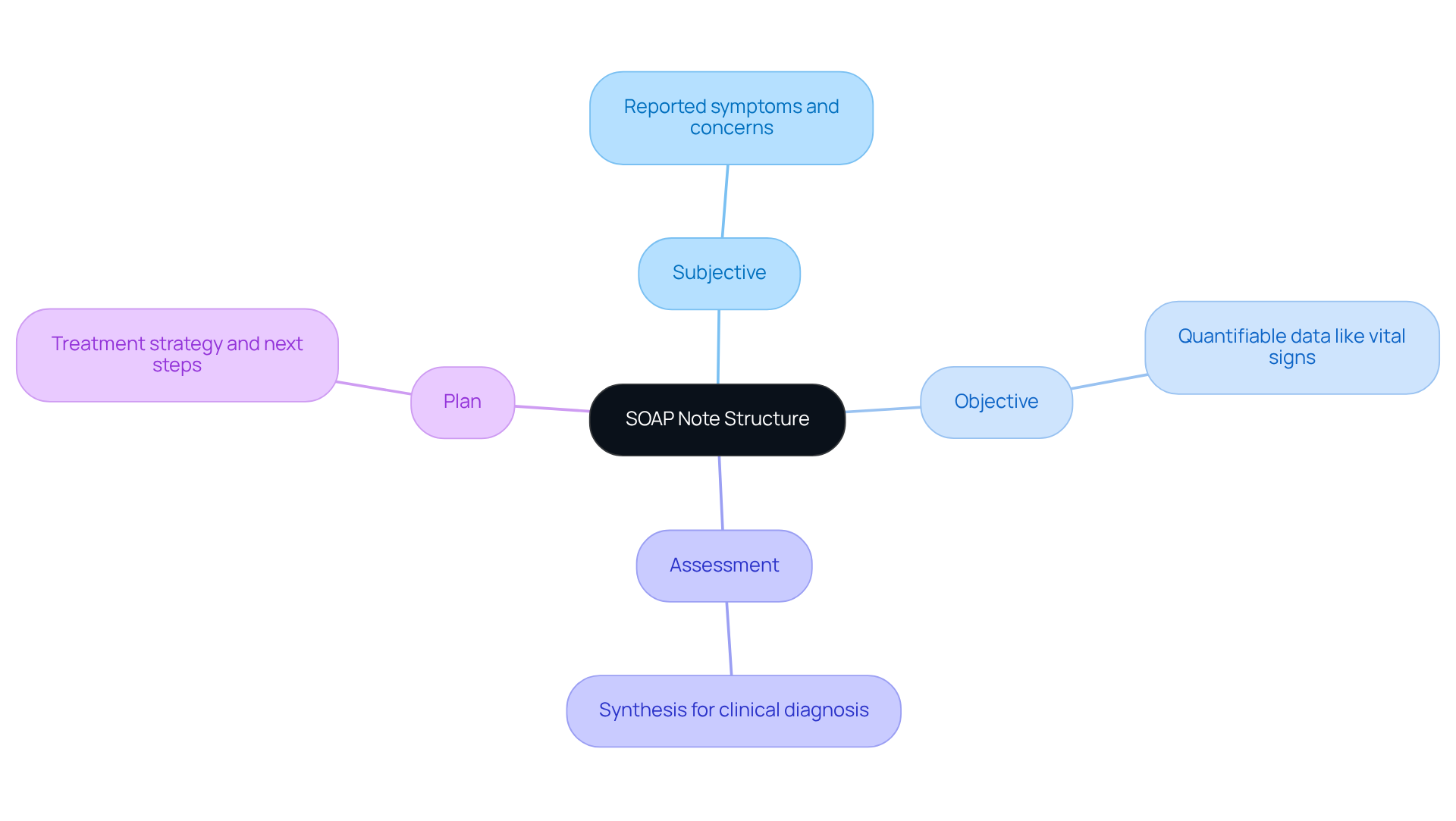
SOAP notes are structured around four essential components: Subjective, Objective, Assessment, and Plan. The Subjective section captures the individual's reported symptoms and concerns, offering valuable insight into their health experience. For instance, when someone expresses feelings of fatigue and anxiety, it becomes crucial for understanding their condition. The Objective section includes quantifiable data, such as vital signs and laboratory test results, which provide measurable evidence of the individual's health status. This data is vital for accurate .
The Assessment section synthesizes the information from both the Subjective and Objective components to formulate a clinical diagnosis. This integration is essential, as it enables to make informed decisions regarding care management. For example, a clinician might conclude that an individual with elevated blood pressure and reported stress is experiencing hypertension, guiding further treatment.
Finally, the outlines the treatment strategy moving forward, detailing next steps such as medication adjustments, referrals, or lifestyle changes. This organized method not only enhances documentation but also , ensuring that all team members are aligned in their understanding of the individual's care. As noted, SOAP records provide a framework for recording and assist in capturing essential information efficiently. Additionally, helps healthcare professionals monitor patient development by preserving initial assessments, diagnoses, and treatment details in a consistent format. By maintaining all essential information documented methodically, clinical records decrease the likelihood of mistakes and oversights during medical practice.
Integrating into the record-keeping process can further improve the effectiveness of SOAP notes. By automating such as data entry, appointment scheduling, and managing medical records, physicians can focus more on client interactions and less on paperwork. This not only enhances the quality of records but also reduces the administrative load that contributes to physician burnout. Understanding and employing this framework, particularly with the assistance of AI tools, is crucial for to individuals. Historically, communication records were devised by Dr. Lawrence Weed in the 1970s, transforming medical record-keeping. In contemporary healthcare, the shift to electronic documentation has further improved the efficiency and reliability of SOAP notes, contributing to reduced physician burnout and better outcomes for individuals receiving care.
Real-World SOAP Plan Examples: Practical Applications in Patient Care
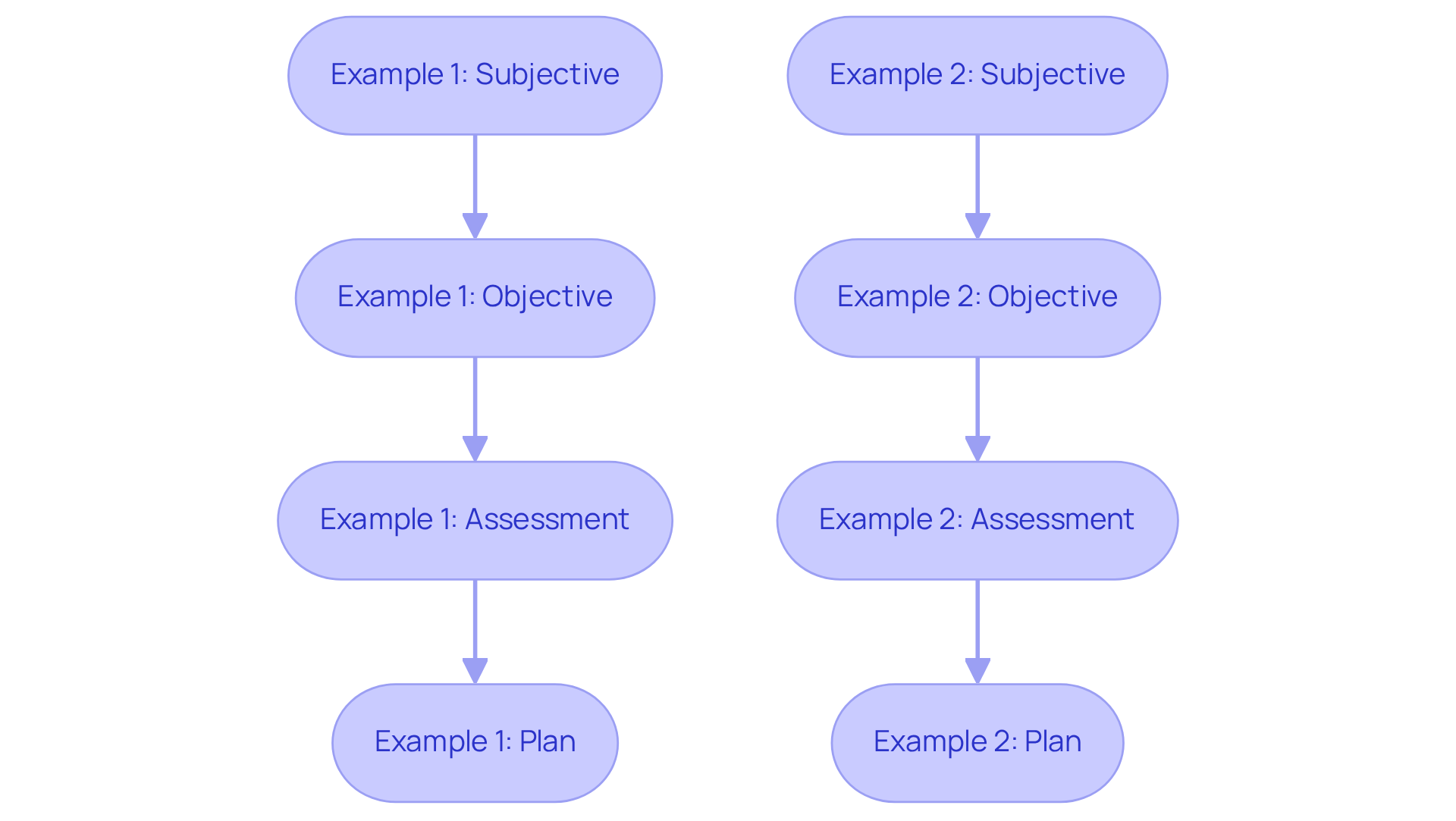
- Example 1: An individual presents with chest pain, expressing feelings of anxiety about their health (Subjective). Vital signs are stable, and an ECG shows no abnormalities (Objective). The evaluation suggests potential anxiety-related symptoms, as indicated by the individual's reported distress levels. The plan includes arranging a follow-up appointment and referring the individual to a mental health expert for additional assessment and support. Utilizing CosmaNeura's can facilitate communication and improve engagement, by reducing administrative loads.
- Example 2: A diabetic individual reports increased thirst and urination, signaling a change in their condition (Subjective). Blood glucose levels are elevated at 250 mg/dL (Objective). The assessment indicates uncontrolled diabetes, necessitating immediate intervention. The plan involves modifying the individual's medication regimen and providing dietary guidance to help manage their blood sugar levels effectively. Generative AI tools can alleviate administrative burdens and enhance care coordination, addressing resistance to innovation in healthcare delivery.
These instances highlight the importance of using a structured format. Have you considered how efficient a can lead to ? Enhanced communication among and better continuity of care are just some of the benefits. By employing organized records, practitioners can ensure that crucial information is captured accurately, facilitating .
Moreover, by incorporating , like those offered by CosmaNeura, we can boost organizational capabilities and enhance client care. It's vital to use the individual's own words in the Subjective section for an accurate representation of their experiences. Additionally, reviewing documentation for accuracy is essential for effective healthcare. Let's work together to embrace these changes and improve the quality of care we provide.
Common Mistakes in SOAP Plans: What to Avoid for Better Documentation
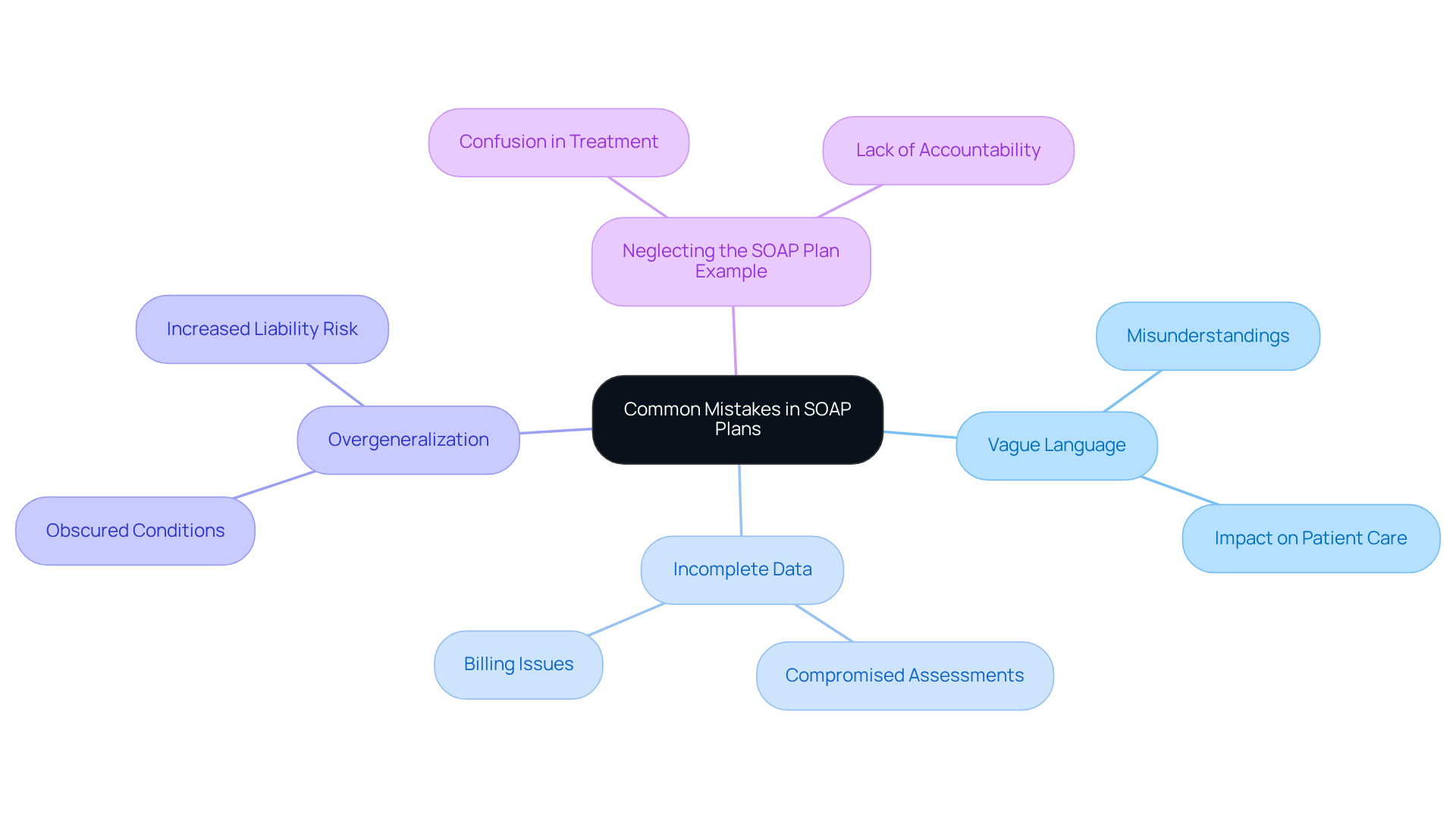
- Vague Language: Using non-specific terms in the Subjective section can lead to misunderstandings that may affect . Documenting the individual's exact words is crucial. Studies show that when individuals read their notes, they often identify serious errors, with 21.1% reporting mistakes. Moreover, over 40% of perceived mistakes were deemed serious by patients. This highlights the to enhance clarity and ensure patient safety.
- Incomplete Data: Omitting relevant information in the Objective section can seriously compromise assessments. It’s essential to meticulously document all vital signs and test results. Insufficient records can complicate billing processes and lead to revenue loss, as over 40% of arise from such errors. Notably, poor accounts for 44% of all medical billing mistakes, underscoring the .
- Overgeneralization: Broad statements in the Assessment section can obscure the individual's true condition. Specificity is crucial; clearly articulate the individual's status and the reasoning behind your diagnosis. This practice not only aids in accurate treatment but also in malpractice claims, with 30% of such claims attributed to communication problems involving documentation mistakes.
- Neglecting the can create confusion regarding the next steps in treatment due to a poorly defined plan. and referrals. An effective soap plan example should include —Specific, Measurable, Achievable, Relevant, and Time-bound—to ensure accountability and facilitate tracking of client progress. Integrating SMART objectives in clinical documentation clarifies expectations and enhances communication. By following these best practices, healthcare providers can significantly enhance the quality of their documentation and improve overall care.
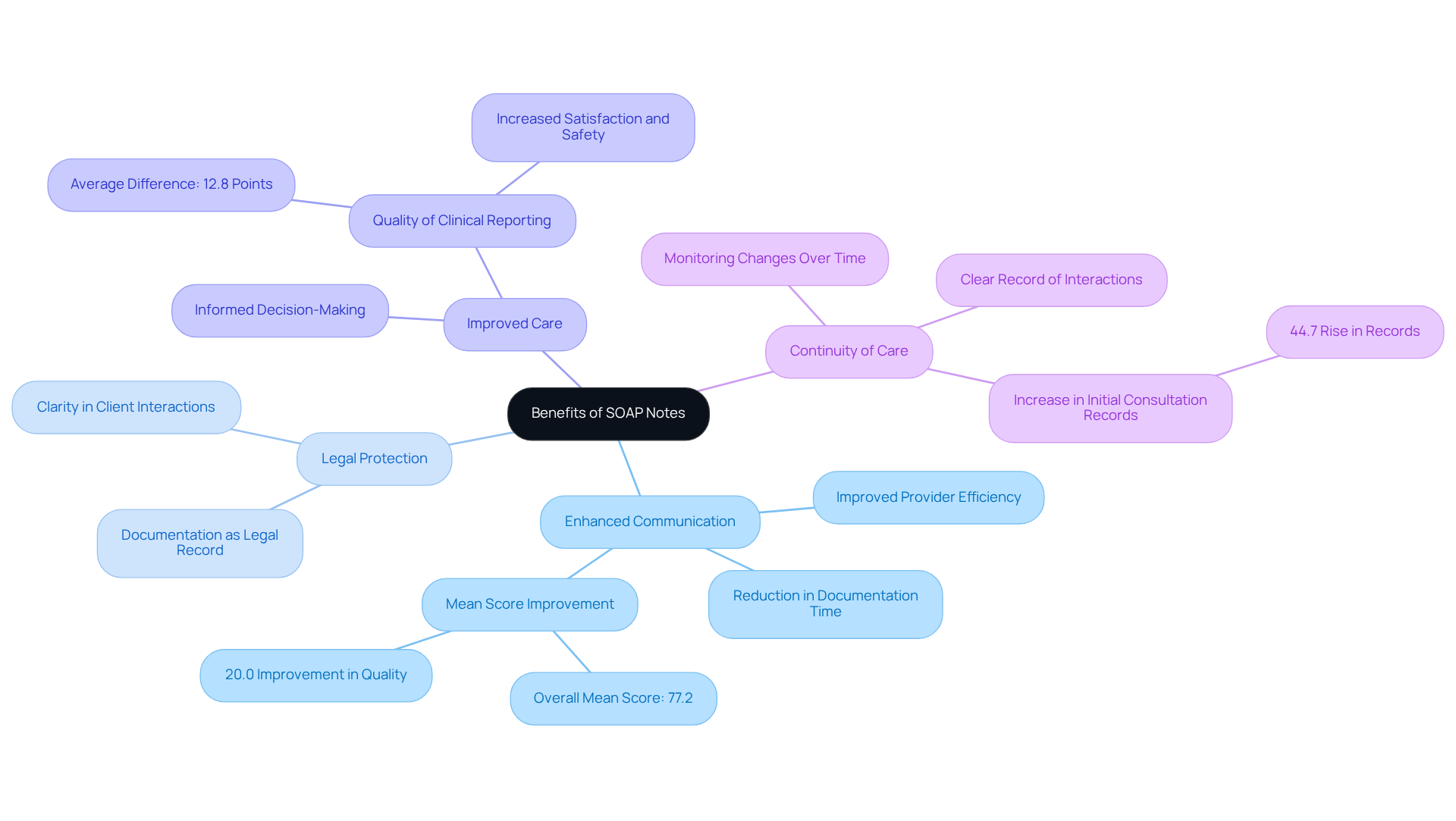
Benefits of SOAP Notes: Enhancing Patient Care and Communication
- Enhanced Communication: Have you ever felt overwhelmed by the sheer volume of information in healthcare? A illustrates how SOAP records provide a uniform structure that significantly . This consistency ensures that every team member is well-informed about the individual’s status, fostering seamless collaboration and informed decision-making. Research indicates that and reduces documentation time, with achieving an overall mean score of 77.2 (95% CI 74.18-80.21), reflecting a 20.0% improvement in the quality of entries.
- Legal Protection: In a world where misunderstandings can arise, serve as vital legal documentation of client interactions. They protect both the provider and the client in case of disputes, ensuring that all interactions are clearly documented and easily accessible. can function as a legal record during disagreements, supporting adherence to legal requirements and fostering responsibility among healthcare practitioners.
- Improved Care: How can we ensure that our clients receive the best possible treatment? By systematically organizing client information, a soap plan example empowers providers to make informed decisions that lead to . The clarity and conciseness of organized records enhance the quality of clinical reporting, which is essential for effective management of individuals receiving care. Research has shown that organized documentation greatly improves the quality of clinical records, with an average difference of 12.8 points (p < 0.001), resulting in increased satisfaction and safety for those receiving care.
- : Have you considered the importance of continuity in patient care? Documentation plays a crucial role in ensuring this continuity by providing a clear and thorough record of individual interactions. This is vital for ongoing treatment and follow-up, as it enables healthcare providers to monitor changes in a person’s condition over time. The allows easy access to essential information, leading to lengthier entries, including a 44.7% rise in initial consultation records, thereby enhancing the overall effectiveness of patient management.
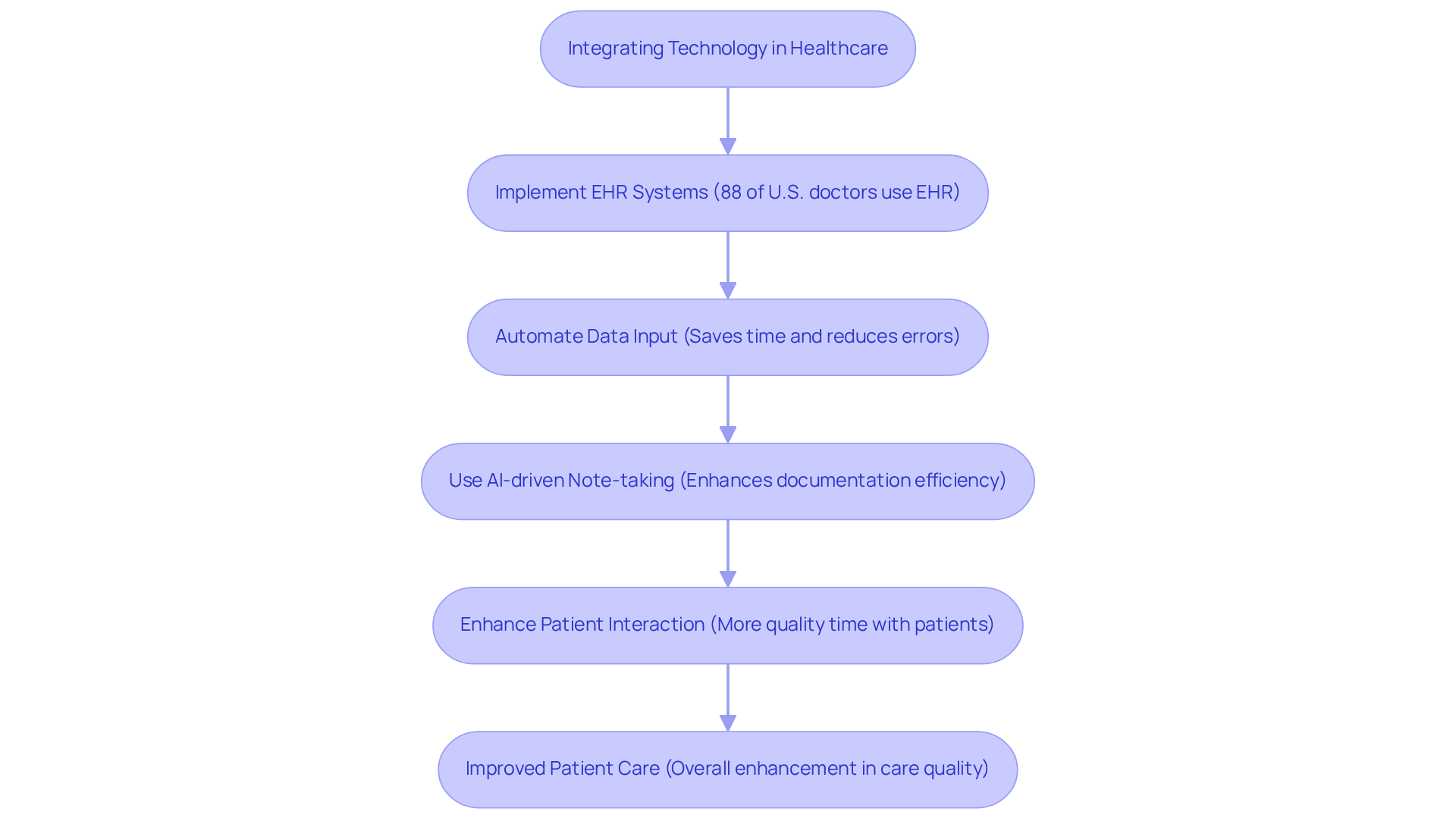
Integrating Technology: Streamlining SOAP Note Documentation
Incorporating technology into patient records addresses a significant emotional challenge faced by healthcare providers: the overwhelming . , now utilized by 88% of U.S. office-based doctors, simplify data input and ensure compliance with record-keeping standards. How much time could you save if these processes were automated? can , allowing you to focus on what truly matters—your patients.
For instance, employs that streamline the . This means you can spend more quality time interacting with clients rather than being bogged down by paperwork. Imagine reclaiming several hours each day; not only does this save valuable time, but it also minimizes the risk of documentation errors, ultimately enhancing the quality of care you provide.
As the healthcare landscape evolves, embracing these technologies is essential. They not only foster but also ensure compliance with best practices. We invite you to explore how these innovations can and .
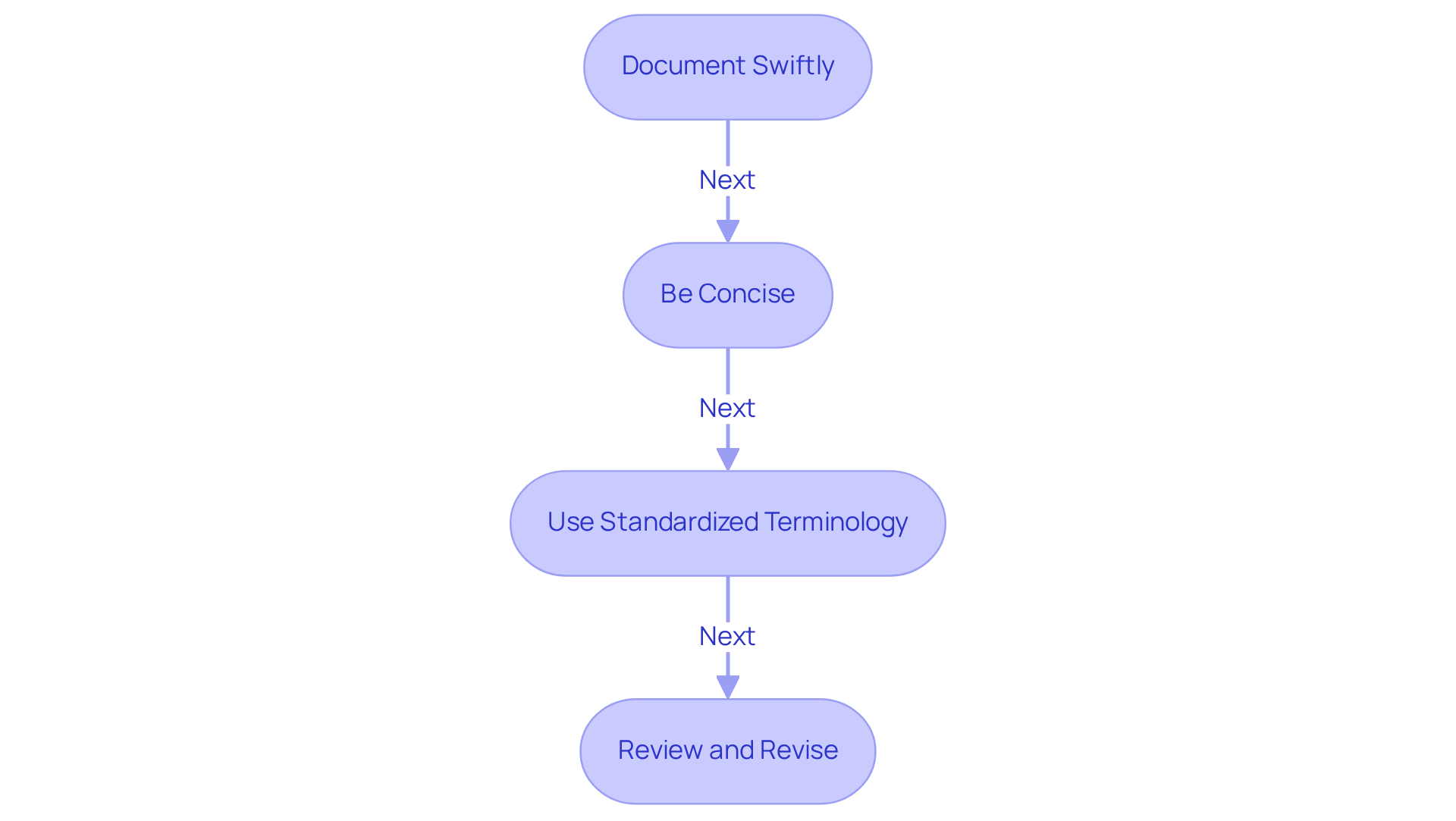
Tips for Writing Effective SOAP Plans: Best Practices for Healthcare Providers
- Document Swiftly: Have you ever felt the pressure of remembering every detail after a patient encounter? helps capture those details while they are still fresh in your mind. As the saying goes, 'Timing is everything when it comes to a .' This practice not only enhances accuracy but also reduces the risk of omitting important information, ultimately . Research indicates that are 4.2 times more likely to note routine practices effectively, highlighting the importance of .
- Be Concise: How can we ensure our notes are understood by everyone involved in ? Utilizing clear and straightforward language to convey essential information is key. Avoiding jargon helps make your notes accessible to all healthcare professionals. is crucial for maintaining clarity and compliance with legal and regulatory standards.
- Use Standardized Terminology: Have you considered the impact of standardized medical terminology on your records? Implementing this approach maintains clarity and consistency, facilitating better communication among healthcare providers. It also supports compliance with legal and regulatory standards. Recognizing challenges in record-keeping practices, such as insufficient training and resources, can help healthcare providers appreciate the significance of using standardized terminology.
- Review and Revise: Before finalizing your SOAP notes, do you take the time to ? Conducting a thorough review is essential for improving clarity and ensuring that your records accurately reflect the individual’s condition and treatment plan, providing a soap plan example. Insights from case studies, like the ',' illustrate the positive effects of thorough reviews on documentation quality.
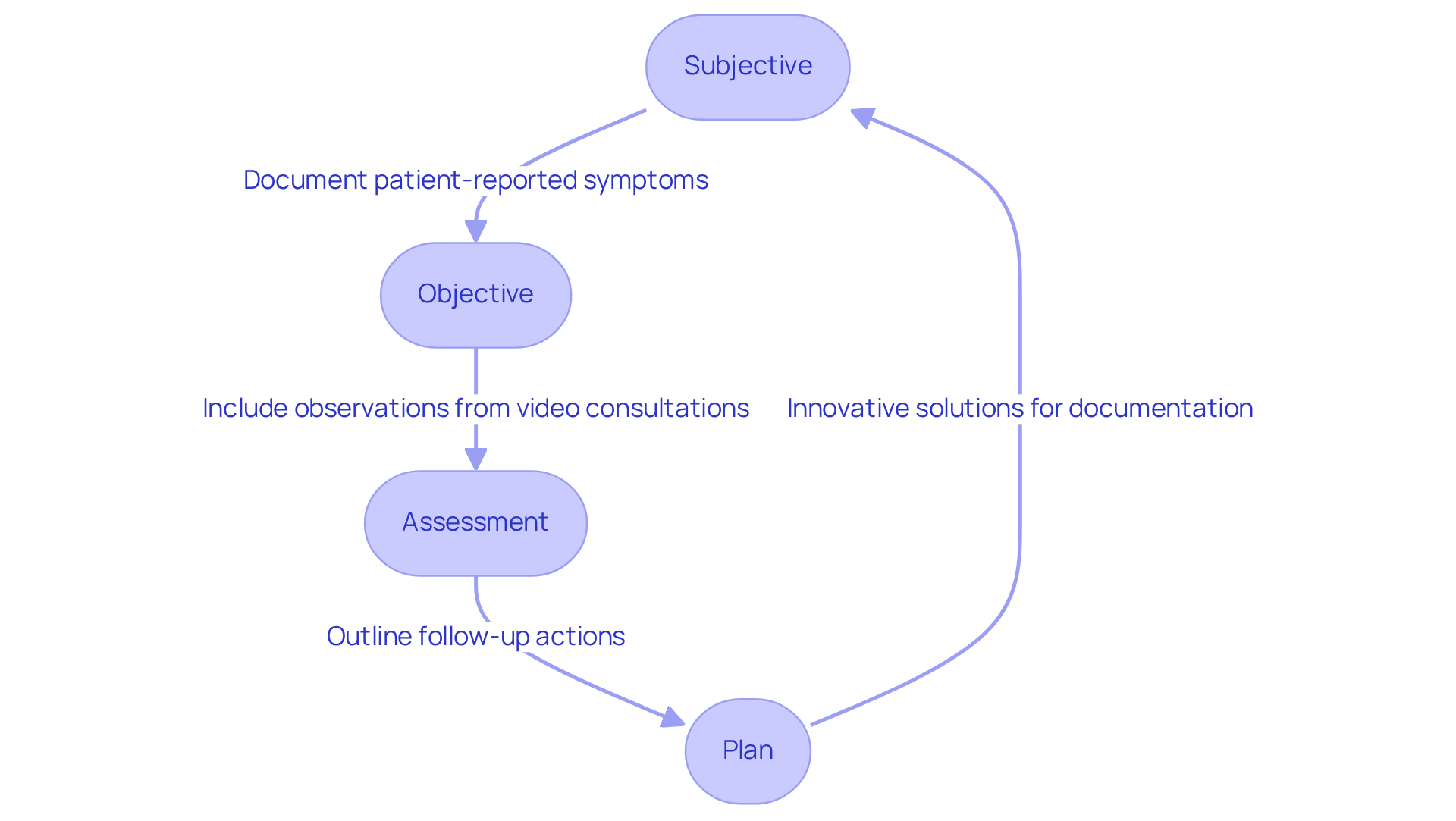
SOAP Notes in Telehealth: Adapting Documentation for Remote Care
In , it is essential to adapt the to address the unique challenges of remote consultations, ensuring . The Subjective section should capture detailed patient-reported symptoms, as physical examinations may be limited. How do individuals articulate their conditions? Including any emotional or psychological factors that may impact their health is vital for understanding their experiences.
The Objective section can encompass observations made through video consultations, such as the individual's demeanor, environment, and any visible signs of distress or comfort. This approach allows providers to gather valuable context that might otherwise be missed, fostering a deeper connection with patients.
Furthermore, the Assessment and soap plan example sections must reflect the remote nature of care. This includes outlining follow-up actions that may necessitate in-person visits, such as referrals for further evaluation or diagnostic tests. For instance, if an individual reports persistent knee pain during a telehealth visit, the clinician might assess the need for an in-person examination or imaging studies to determine the underlying cause. By ensuring that every part of the clinical record is adapted to the telehealth format, providers can maintain thorough documentation that supports continuity of care and improves outcomes for individuals.
However, challenges in documenting during remote consultations exist, including the potential for incomplete information due to the lack of physical interaction. Providers must be vigilant in asking probing questions to elicit comprehensive responses from patients. As one expert noted, "In emergencies, the ability to quickly prioritize and act on information is vital," highlighting the importance of thorough documentation even in virtual settings. Frequent errors in clinical documentation often involve leaving out essential details and blending subjective and objective observations, which can undermine the quality of care.
To tackle these challenges, consider the following :
- Utilize to enhance care quality.
- Ensure all pertinent information is captured effectively.
By embracing these strategies, healthcare professionals can improve their documentation practices, leading to and a more compassionate approach to care.
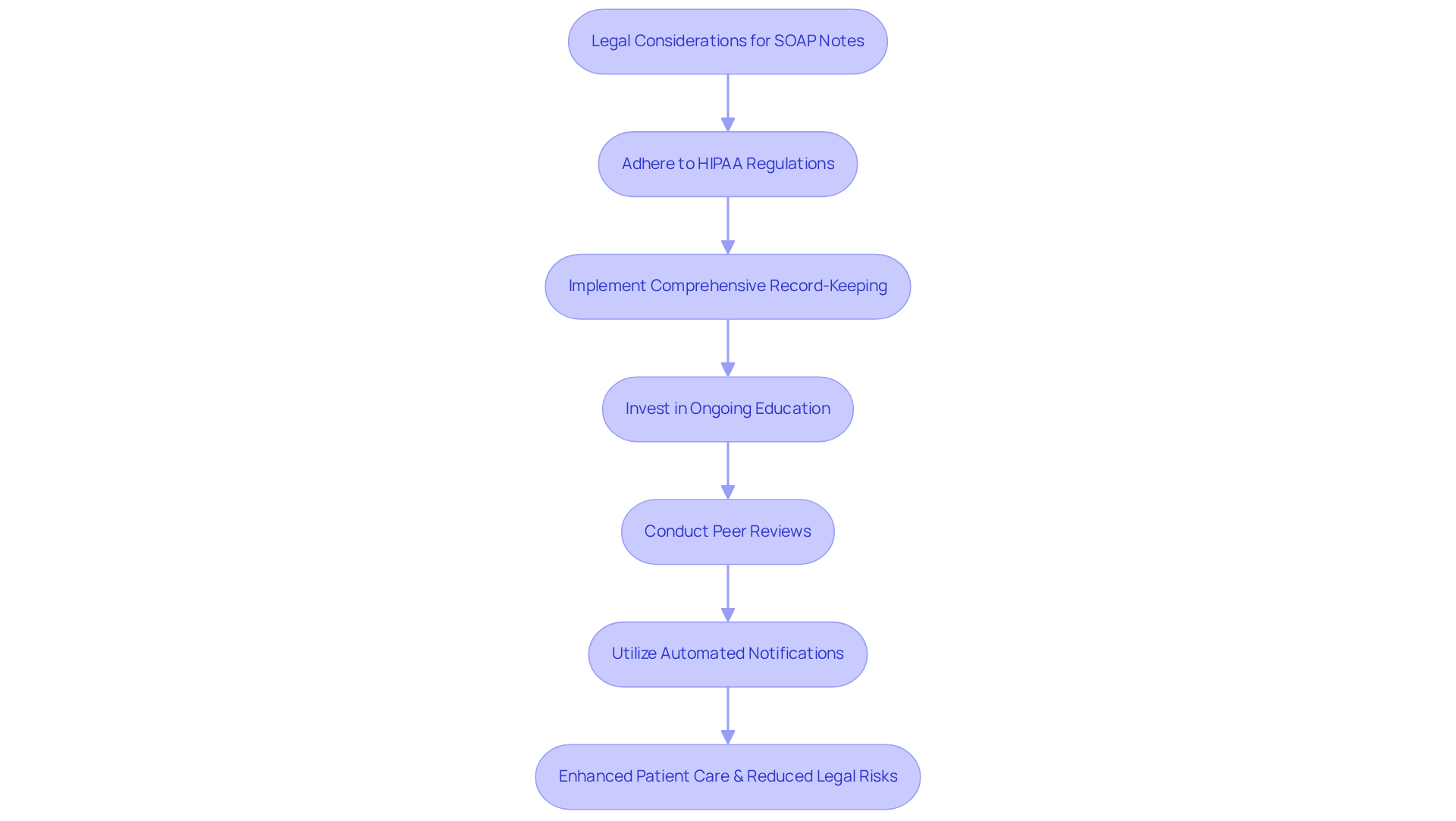
Legal Considerations for SOAP Notes: Ensuring Compliance in Documentation
often face emotional challenges when navigating the complexities of . Prioritizing legal considerations in a is crucial, particularly regarding , which are vital for safeguarding patient privacy and confidentiality. With the healthcare industry representing 79% of all reported and over 168 million exposed records in 2023, it becomes clear that strong are essential.
Non-compliance can lead to significant legal repercussions, including denied claims and financial penalties. Incomplete or flawed notes can create legal issues, making it imperative for providers to ensure their records are comprehensive and accurate. Have you considered how a SOAP plan example that includes consistent training on record-keeping standards can alleviate some of these burdens? Organizations that invest in and minimized risks.
Moreover, implementing and transparency among healthcare teams. This collaborative assessment and constructive feedback can significantly improve record quality. Additionally, employing automated notifications in EHR systems can help ensure compliance and enhance record-keeping practices.
By adopting these practices, providers can not only shield themselves from possible liabilities but also cultivate a that ultimately enhances care for individuals. Let's work together to create a supportive environment where compliance is not just a requirement but a shared commitment to patient well-being.
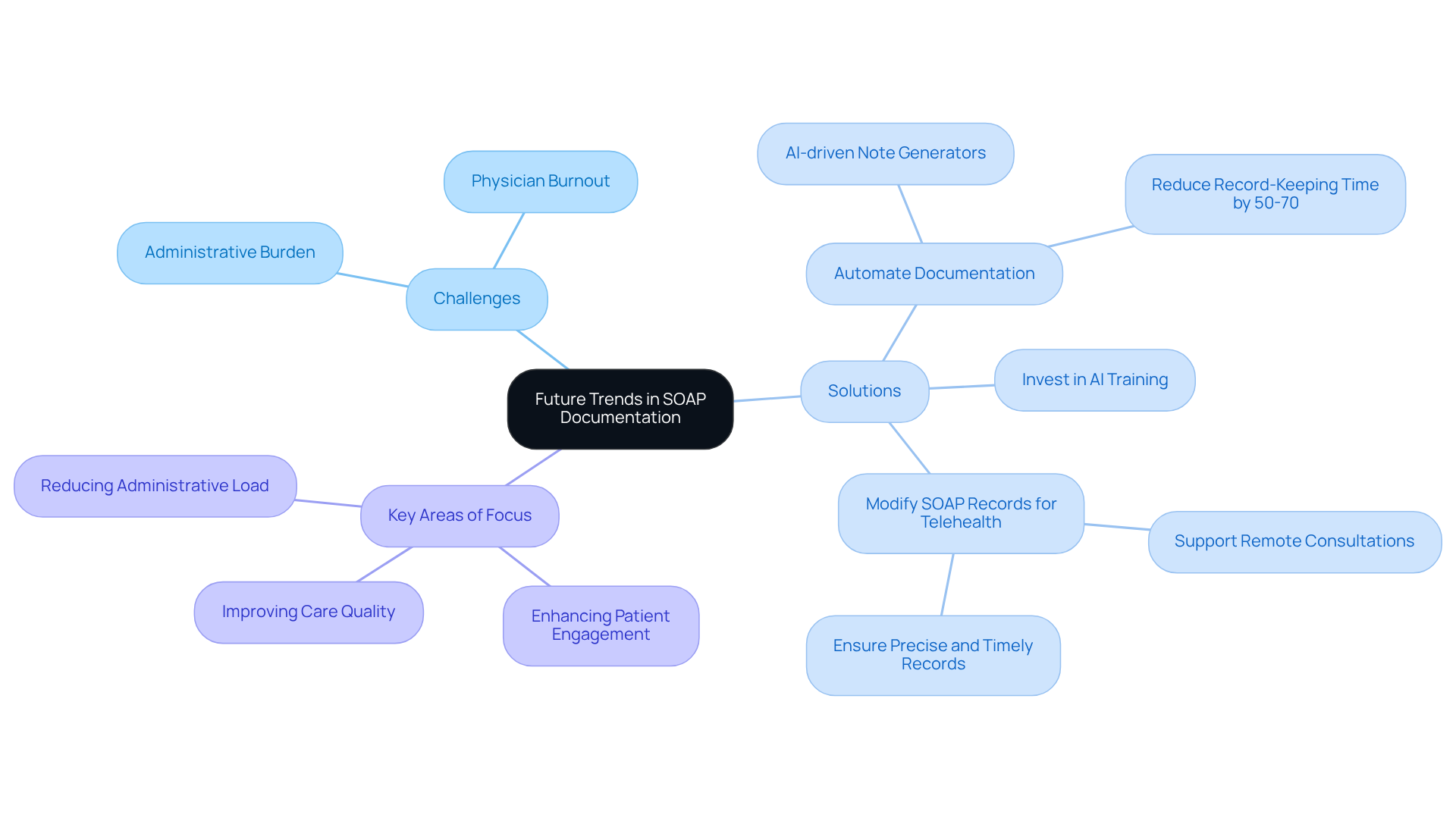
Future Trends in SOAP Documentation: Preparing for Innovations in Healthcare
Healthcare professionals often face emotional challenges due to overwhelming administrative burdens. These pressures can detract from the quality of patient care, leaving many feeling stretched thin. However, to alleviate these concerns.
Generative AI technologies can automate the creation of documentation, significantly reducing the administrative load that often hampers care quality. For instance, can decrease record-keeping time by 50-70%. This allows clinicians to focus more on direct patient engagement rather than paperwork, fostering deeper connections with those they serve.
As , a soap plan example will be necessary to to support remote consultations. This change not only boosts efficiency but also elevates the quality of care by ensuring that records are precise and timely. Providers are encouraged to stay updated on these trends and consider investing in training and tools that enhance their record-keeping practices.
By positioning themselves at the forefront of patient care in an increasingly digital landscape, healthcare providers can significantly improve their practice. A staggering 80% of physicians believe that AI can enhance healthcare quality, and 57% see the most significant opportunity for AI in reducing administrative burdens. Embracing these innovations is crucial for maintaining high standards in clinical documentation.
Furthermore, addressing challenges such as physician burnout and rising costs through the implementation of the overall healthcare delivery system.
Key Solutions:
- Automate documentation to reduce administrative load.
- Invest in training for AI tools.
- .
In this rapidly evolving landscape, embracing technology not only supports healthcare providers but ultimately leads to better care for patients. Together, we can navigate these changes and for everyone involved.
Conclusion
The integration of SOAP plans within healthcare documentation transcends mere procedural necessity; it represents a transformative approach that significantly enhances patient care. By utilizing structured SOAP notes, healthcare providers can alleviate some of the administrative burdens that often detract from meaningful patient interactions. Imagine the relief of having more time to focus on what truly matters—caring for patients. The incorporation of AI technologies, such as those offered by CosmaNeura, further amplifies these benefits by automating routine tasks, reducing the burden on providers, and improving the accuracy and efficiency of records.
Throughout this article, we have explored key insights, including the essential components of SOAP notes, common pitfalls to avoid, and the numerous advantages they offer in terms of communication, legal protection, and continuity of care. Real-world examples illustrate how effective SOAP documentation can lead to improved clinical outcomes and heightened patient satisfaction. Moreover, our discussion of future trends underscores the critical importance of adapting to technological advancements within the ever-evolving healthcare landscape.
As the healthcare industry continues to change, embracing tools that enhance documentation practices becomes increasingly vital. We encourage providers to adopt AI-driven solutions and implement best practices for writing SOAP plans to ensure compliance and elevate the quality of care. By prioritizing efficient documentation, healthcare professionals can foster a more compassionate, effective, and patient-centered approach to care—ultimately benefiting everyone involved. Together, let us strive towards a future where patient care is at the forefront of our efforts.




