Overview
In the demanding world of healthcare, providers often face overwhelming administrative burdens that can detract from their primary focus: patient care. This article highlights the emotional challenges that arise from these pressures, emphasizing the need for effective solutions.
One such solution is the use of SOAP progress notes examples and AI automation. Implementing structured templates and AI tools can significantly reduce documentation time, allowing healthcare professionals to dedicate more time to their patients. Imagine the relief of knowing that your documentation is both efficient and accurate.
The benefits are clear: increased compliance rates and positive feedback from professionals demonstrate that these tools not only enhance efficiency but also improve the quality of care provided. By embracing these innovations, healthcare providers can transform their workflow and ultimately foster a more compassionate environment for their patients.
Are you ready to explore how these solutions can make a difference in your practice? Let’s take the first step together towards a more efficient and caring healthcare experience.
Introduction
In the fast-paced realm of healthcare, the burden of documentation can often overshadow the core mission of patient care. Many healthcare professionals feel overwhelmed by administrative tasks, which can detract from their ability to provide compassionate care. With the advent of advanced technologies, particularly AI, there is a hopeful opportunity to streamline documentation processes, significantly enhancing efficiency. But amidst these innovations, a pressing question arises: how can clinicians effectively integrate structured SOAP progress notes to improve both their workflow and patient outcomes? This article delves into practical examples and best practices that not only alleviate these administrative pressures but also elevate the quality of care delivered. Together, let’s explore how we can make a meaningful difference in the lives of both providers and patients.
CosmaNeura: Streamline SOAP Progress Notes with AI Automation
In today’s demanding healthcare environment, professionals often grapple with overwhelming documentation burdens. This can detract from the precious time they have to devote to patient care. CosmaNeura offers a compassionate solution through advanced AI technology, automating the generation of a SOAP progress notes example. By seamlessly integrating AI into clinical processes, clinicians can reclaim valuable time, allowing them to focus more on caring for individuals rather than getting lost in administrative tasks.
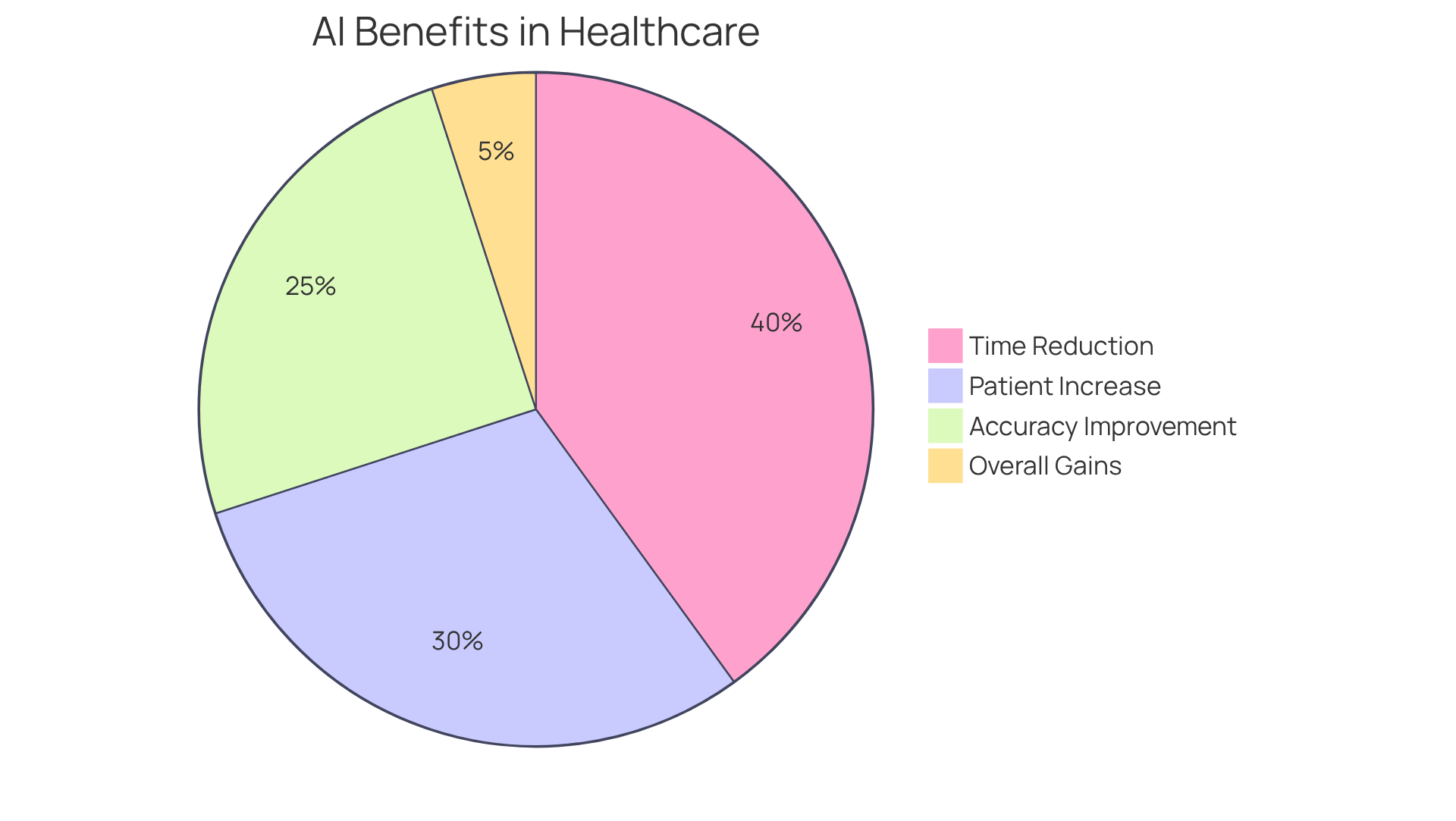
Imagine reducing record-keeping time by up to 40%! This remarkable efficiency not only enhances workflow but also ensures that the SOAP progress notes example is consistently structured and aligned with healthcare standards, reflecting the ethical guidelines of Catholic teachings. Many doctors have observed that the application of AI tools can improve record accuracy by up to 25%, particularly through AI-driven medical scribing. This fosters a more effective practice setting, where professionals can truly thrive in their roles.
Moreover, ScribeRyte AI has been shown to increase the number of individuals seen daily by 30%, illustrating the transformative impact of AI on healthcare throughput. The positive feedback from healthcare professionals underscores the importance of AI in making clinical documentation a more efficient and reliable process. As Dr. Smith from Springfield Clinic shared, “AI has greatly enhanced my productivity, enabling me to concentrate more on healthcare.”
Isn’t it time to embrace this change? By leveraging AI, healthcare providers can not only lighten their documentation load but also enhance the quality of care they deliver. Together, let’s explore how these innovative solutions can support your practice and ultimately benefit your patients.
SOAP Note Guide Examples & Prompts: Enhance Documentation Efficiency
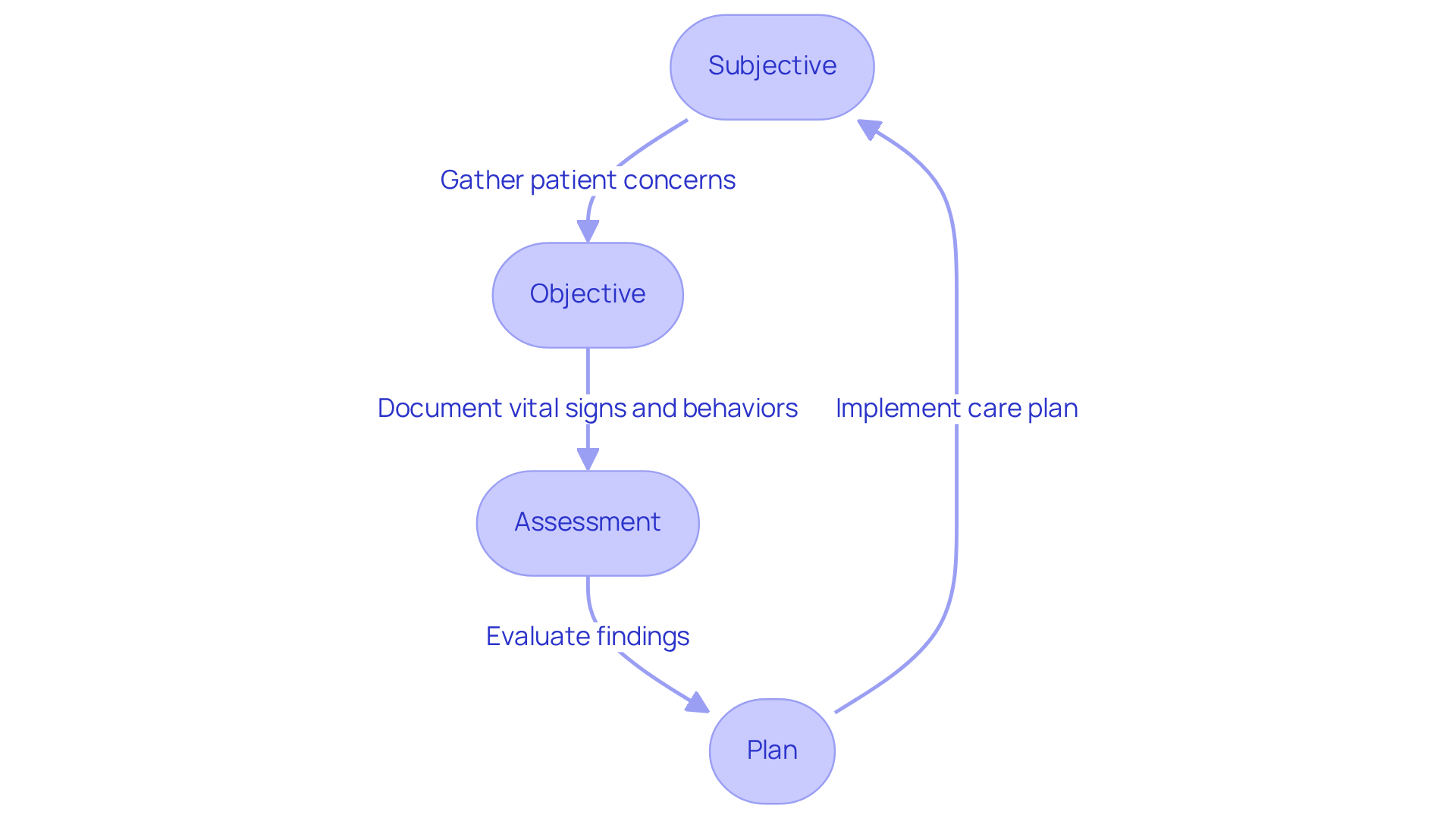
Effective SOAP progress notes examples are essential tools that help healthcare providers navigate the complexities of patient encounters. Have you ever wondered how organized prompts can make a difference in your daily practice? In the 'Subjective' section, clinicians might reflect on, 'What are the individual's main concerns today?' This approach fosters a deeper understanding of the patient’s perspective, allowing for more compassionate care.
In the 'Objective' section, it is crucial to document vital signs and observable behaviors. By ensuring that critical clinical data is recorded, we can support our patients more effectively. Research indicates that healthcare workers who adopt organized record-keeping formats are significantly more likely to maintain high-quality entries. In fact, trained individuals are 2.89 times more likely to document efficiently. Imagine the positive impact this can have on your practice and patient outcomes.
By utilizing these organized prompts, providers can enhance their record-keeping efficiency by incorporating a SOAP progress notes example, capturing all pertinent information and ultimately improving care outcomes. Optimal methods for recording client interactions in primary care involve consistently applying these prompts and regularly reviewing the SOAP progress notes example guidelines. This practice not only promotes a culture of comprehensive and precise record maintenance but also supports you in providing the best possible care for your patients. Let’s embrace these strategies together for a brighter future in patient care.
GetFreed.ai: Step-by-Step Guide to Writing SOAP Notes
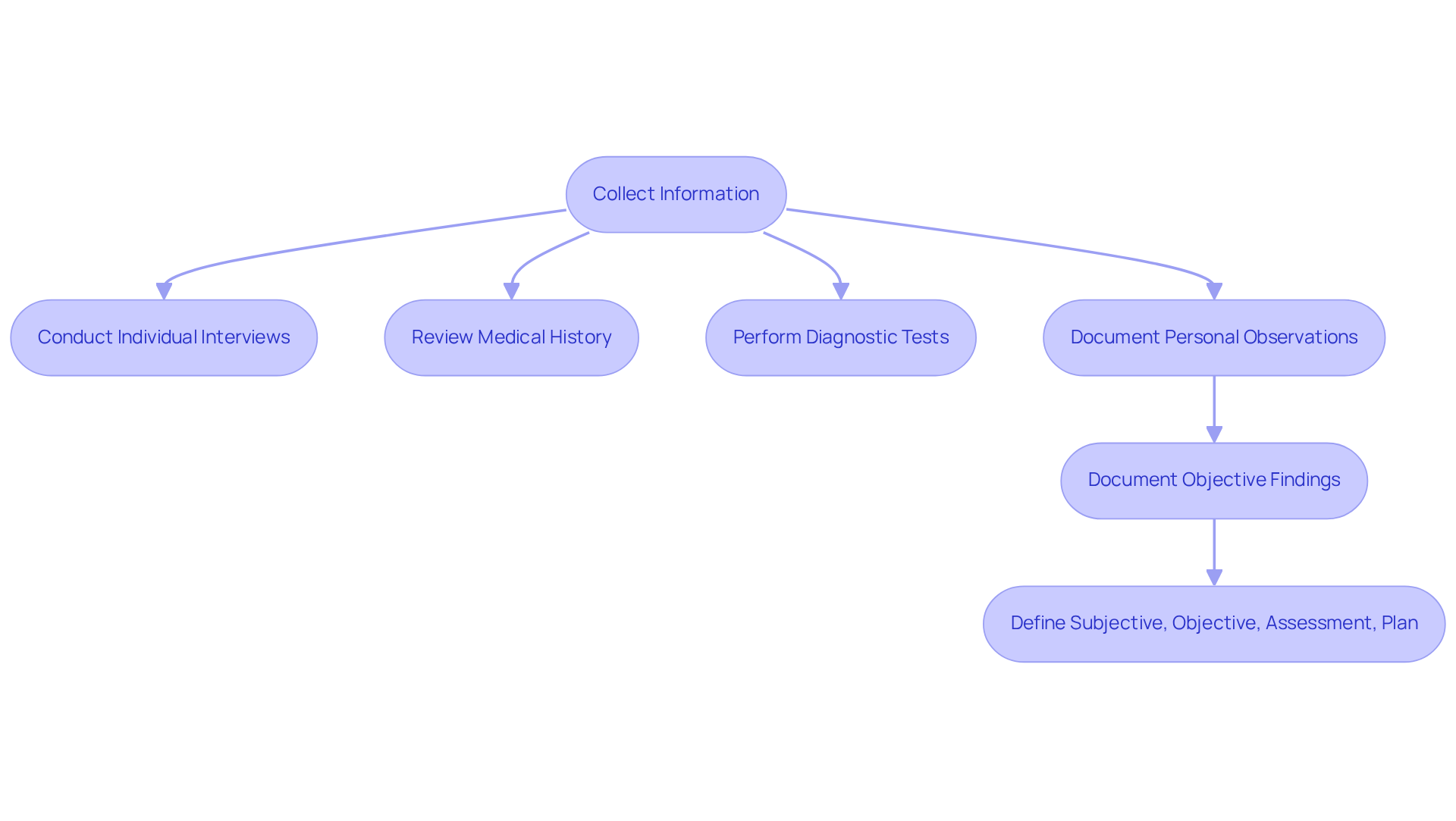
Collecting information from individuals for SOAP records is a crucial first step in enhancing clinical records. This process involves gathering comprehensive data through individual interviews, medical history reviews, and relevant diagnostic tests. Effective record-keeping begins with personal observations, where providers note the individual’s reported symptoms and concerns. Next, objective findings are documented, including measurable data such as vital signs and lab results. This structured approach ensures that each component—Subjective, Objective, Assessment, and Plan—is clearly defined, fostering better communication among healthcare teams.
The impact of organized records on healthcare outcomes is significant. Have you ever felt overwhelmed by administrative tasks? Studies reveal that using Electronic Health Records (EHRs) can save an average of 75 minutes in clinical record-keeping, allowing providers to spend more time engaging with individuals. Additionally, organized record-keeping practices have been shown to improve data quality metrics, with a 20% increase in record quality after transitioning to structured formats. This not only enhances compliance with regulatory standards but also greatly reduces the risk of record errors, which can adversely affect healthcare outcomes.
Current best practices for documenting individual information emphasize clarity and conciseness. Providers are encouraged to utilize standardized templates for a SOAP progress notes example, simplifying the record-keeping process and ensuring that all necessary information is captured efficiently. Furthermore, employing automated tools can assist in real-time transcription and summarization during client interactions, further enhancing the accuracy and thoroughness of records.
By embracing these best practices, healthcare providers can improve their record-keeping efficiency, ultimately leading to better patient care and outcomes. The adoption of organized records not only supports compliance but also nurtures a culture of accountability and quality within healthcare environments.
Key solutions to consider:
- Utilize standardized templates for SOAP notes.
- Implement automated tools for real-time transcription.
- Prioritize clarity and conciseness in documentation.
By taking these steps, we can collectively enhance our approach to patient care. Let’s work together to create a more efficient and compassionate healthcare environment.
Heidi Health: SOAP Note Template with Examples for Consistent Documentation
In the demanding world of healthcare, providers often face emotional challenges related to documentation. Administrative burdens can detract from the vital patient care that clinicians strive to deliver. CosmaNeura understands these challenges and offers customizable SOAP progress notes examples that are designed to improve documentation consistency across various clinical settings.
These templates, such as the soap progress notes example, serve as a valuable resource for clinicians, assisting them in systematically capturing essential interaction details. For instance, they encourage users to include critical information in the 'Assessment' section, such as the individual's progress and any adjustments to treatment plans. Have you ever felt overwhelmed by the paperwork? You're not alone.
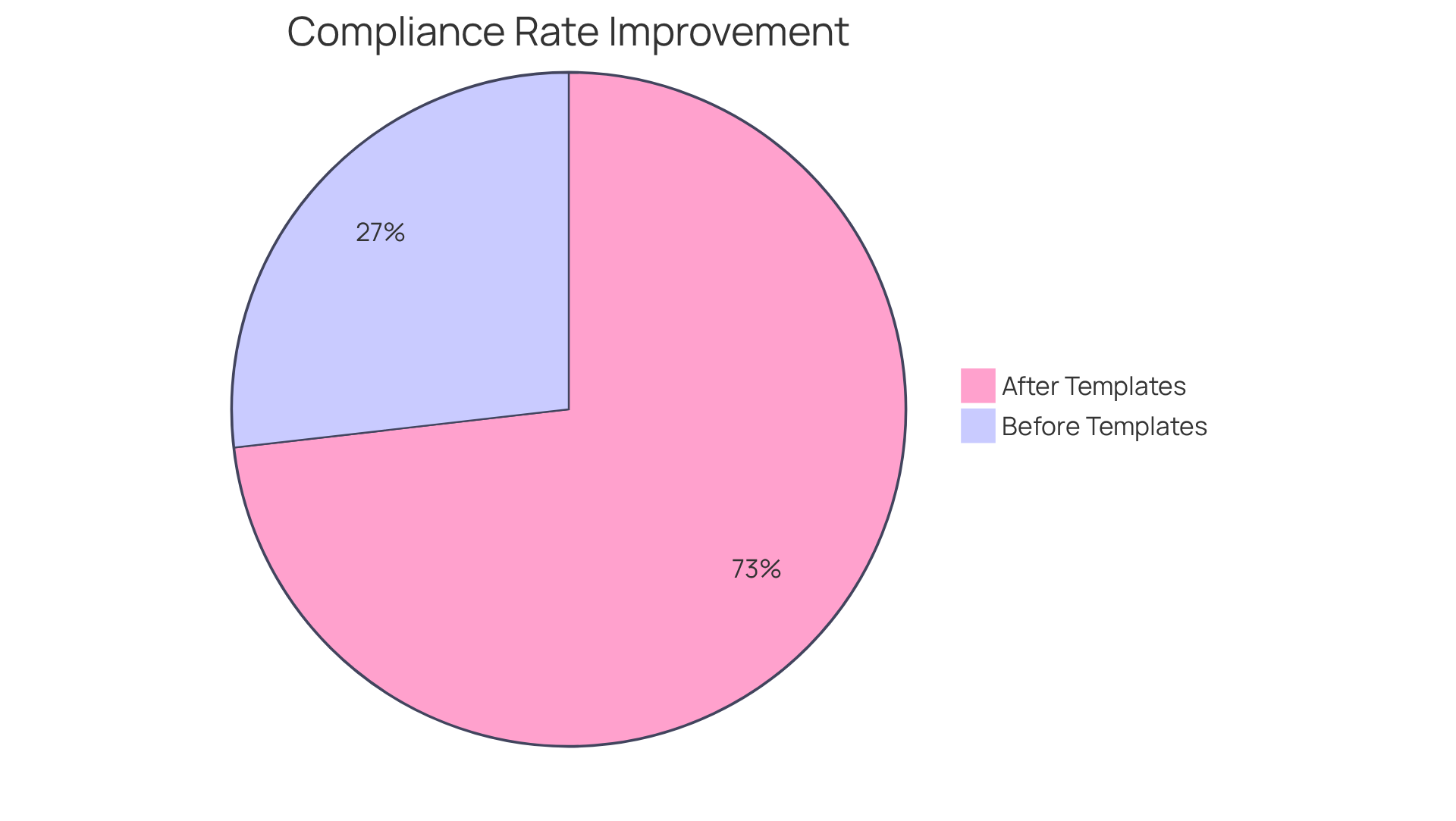
Research shows that using structured templates can lead to significant improvements in record quality. In fact, compliance rates can increase dramatically, from 31.1% to 84.9%, following their introduction. Clinicians who utilize these templates report enhanced efficiency, allowing them to focus more on providing care rather than getting bogged down by administrative tasks.
By optimizing record-keeping procedures, CosmaNeura's templates not only save time but also elevate the overall quality of clinical records. This ultimately contributes to better patient outcomes. Imagine the difference this could make in your practice—less time spent on paperwork and more time dedicated to your patients. Take the step towards a more efficient and compassionate approach to documentation today.
SimplePractice: Comprehensive Resource for Writing SOAP Notes
As healthcare providers, you often face emotional challenges in managing the complexities of documentation. SimplePractice provides a comprehensive resource for creating structured documentation, featuring best practices and a SOAP progress notes example that can alleviate this burden. It’s important to recognize how administrative tasks can impact your ability to provide the best care for your patients.
Timely record-keeping, clear language, and compliance with HIPAA guidelines are not just regulatory requirements; they are essential for effective communication. By adhering to these guidelines, you can ensure that your documentation is both compliant and effective in conveying vital patient information. This resource acts as an essential instrument for healthcare providers seeking to improve their record-keeping practices.
Imagine the peace of mind that comes from knowing your documentation is accurate and timely. You can focus more on what truly matters—your patients. Let SimplePractice guide you in transforming your documentation process, allowing you to provide the compassionate care your patients deserve. Take the first step towards enhancing your record-keeping practices today!
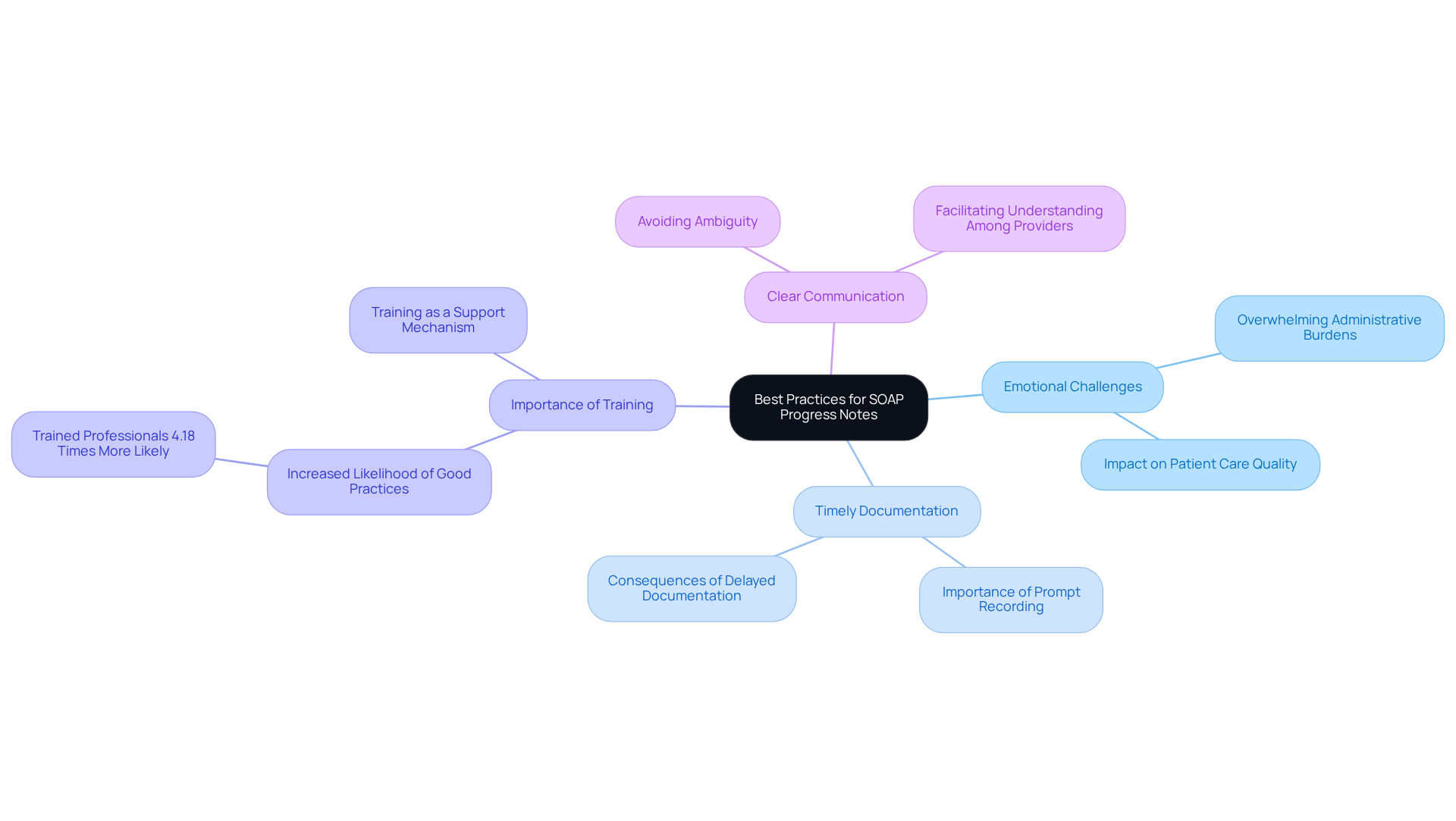
TherapyNotes: Best Practices for Completing SOAP Progress Notes
TherapyNotes recognizes the emotional challenges healthcare providers face in maintaining accurate records. The administrative burdens can often feel overwhelming, impacting the quality of patient care. It’s crucial to document information promptly after sessions, as this practice captures details accurately and alleviates stress. Research shows that health professionals who received training were 4.18 times more likely to effectively record routine practices. This statistic highlights the importance of training in enhancing record quality and supporting clinicians in their vital work.
Using clear and concise language is another essential practice. This approach helps avoid ambiguity, ensuring that other healthcare providers can easily understand the notes. Reflecting on this, it’s concerning that only 51.1% of health professionals maintain good routine practice records. This suggests a significant opportunity for improvement in this area.
By following these best practices, clinicians can enhance the quality of their records, ultimately improving patient care. Poor data quality can lead to misdiagnoses and increased patient morbidity, which is something we all strive to prevent. Let’s commit to fostering a supportive environment where we prioritize training and clear communication, ensuring that every patient receives the best possible care.
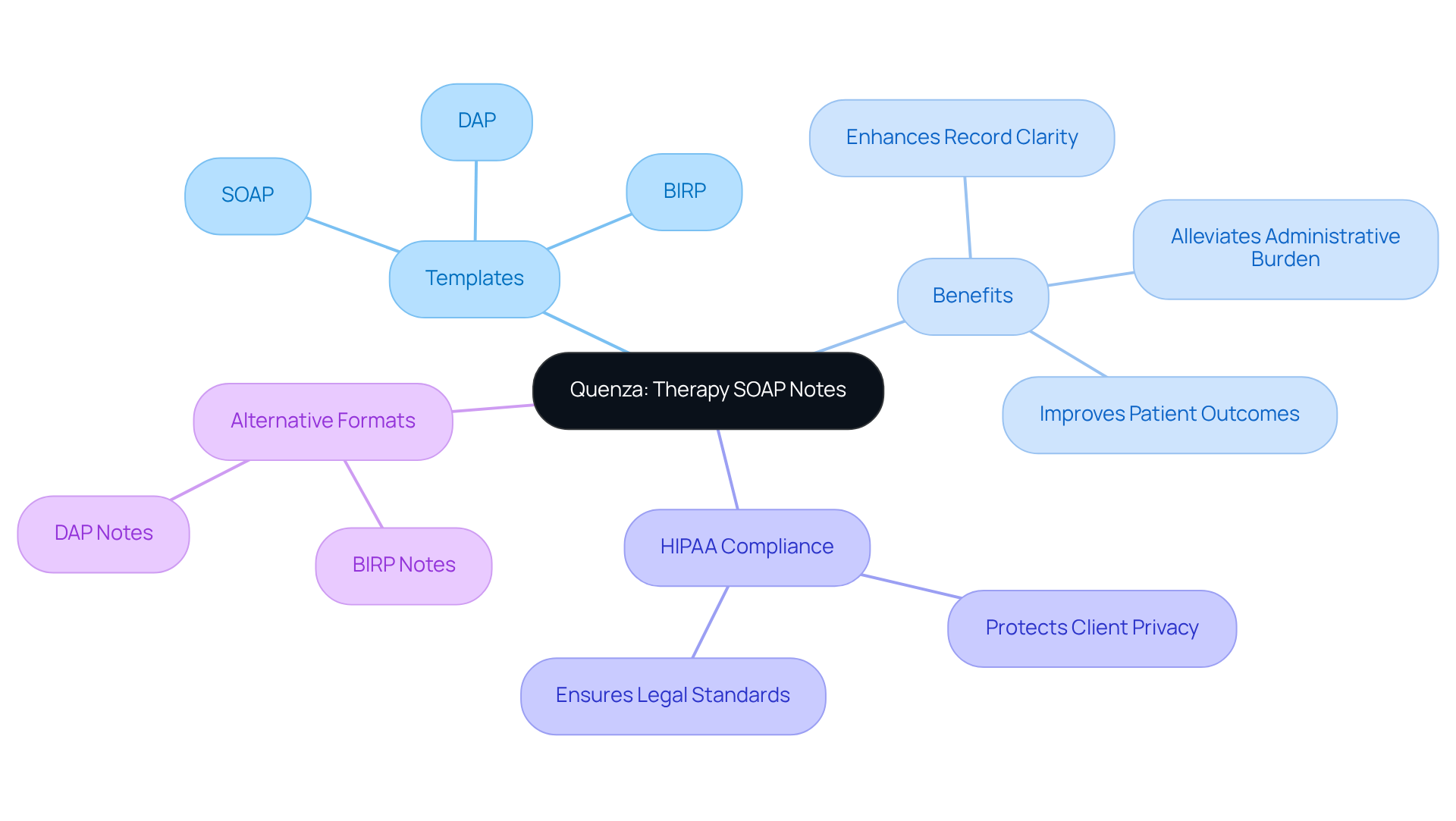
Quenza: Templates and Examples for Effective Therapy SOAP Notes
In the demanding field of healthcare, clinicians often face emotional challenges that can impact their practice. Quenza provides a comprehensive array of templates and examples that serve as a soap progress notes example, designed to enhance the effectiveness of therapy records and allowing providers to visualize the ideal format. This ensures that all relevant information is captured, helping to alleviate the administrative burdens that can detract from patient care.
For instance, these templates act as a soap progress notes example, aiding clinicians in recording progress, treatment interventions, and future plans, which fosters a comprehensive and systematic approach. As Vivian Chung Easton, LMFT, wisely notes, "Clear, effective records enhance your practice and assist clients on their journey to growth and healing." By utilizing these organized templates, clinicians can significantly simplify their record-keeping process, ultimately improving the quality of care they provide and enhancing patient outcomes.
Moreover, using these templates aligns with HIPAA compliance, guaranteeing that records meet legal standards while also alleviating the administrative load that can contribute to therapist burnout. Have you explored different record formats? Investigating options such as BIRP and DAP can offer clinicians additional choices tailored to their specific needs. Embracing these resources not only supports your practice but also nurtures the growth and healing journey of your clients.
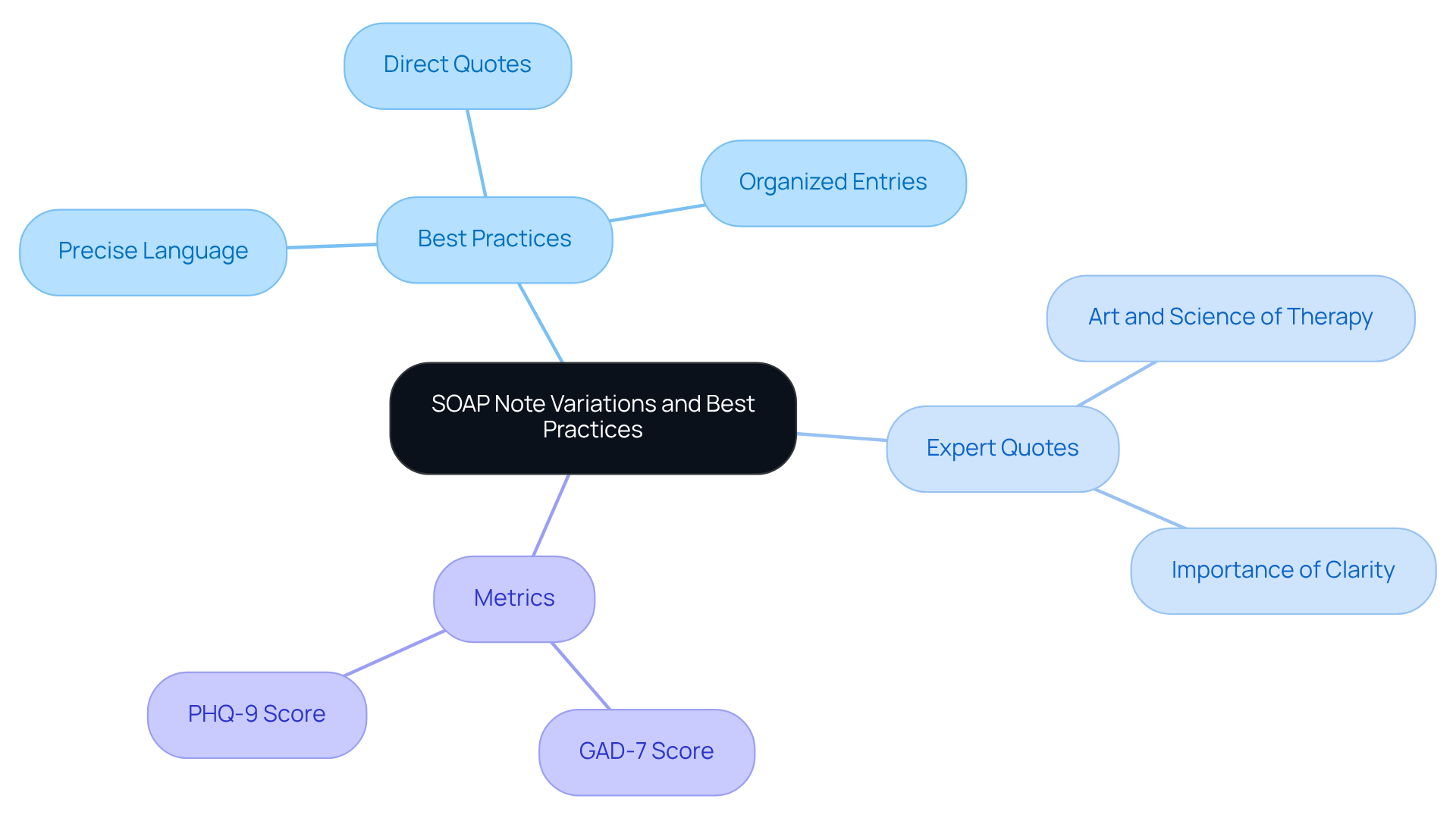
Psylio: Insights into SOAP Note Variations and Best Practices
Mental health experts face the emotional challenge of capturing therapeutic interventions and patient reactions through documentation. This customization is not just a task; it’s a vital part of upholding high standards of care. By ensuring that records reflect the nuances of mental health treatment, we can truly support our clients. Optimal approaches involve using precise language, integrating direct quotes from clients, and organizing entries to highlight both subjective experiences and objective observations. For instance, when a client expresses feelings of anxiety or depression in their own words, it enhances understanding and fosters a stronger therapeutic alliance.
Furthermore, utilizing a SOAP progress notes example can significantly influence patient care. By focusing on relevant details and maintaining a clear, organized format, as seen in a SOAP progress notes example, clinicians can improve communication among healthcare providers, thereby facilitating continuity of care. As experts in the field emphasize, effective record-keeping not only assists in treatment planning but also serves as a legal account that upholds accountability and confidentiality. It is essential to finalize complete records usually within 24-48 hours after the session to ensure accuracy and relevance.
Quotes from mental health professionals highlight the importance of this adaptation. One expert remarked, "The key is understanding how to capture both the art and science of therapy in your documentation," underscoring the need for a balanced approach. Another observed that clear and concise records are essential for understanding client progress and guiding treatment choices. For instance, a GAD-7 score of 16 signifies moderate anxiety, demonstrating how specific metrics can be effectively recorded in clinical summaries. By embracing these best practices, mental health providers can enhance the quality of care they deliver, ultimately benefiting their clients and the broader healthcare system.
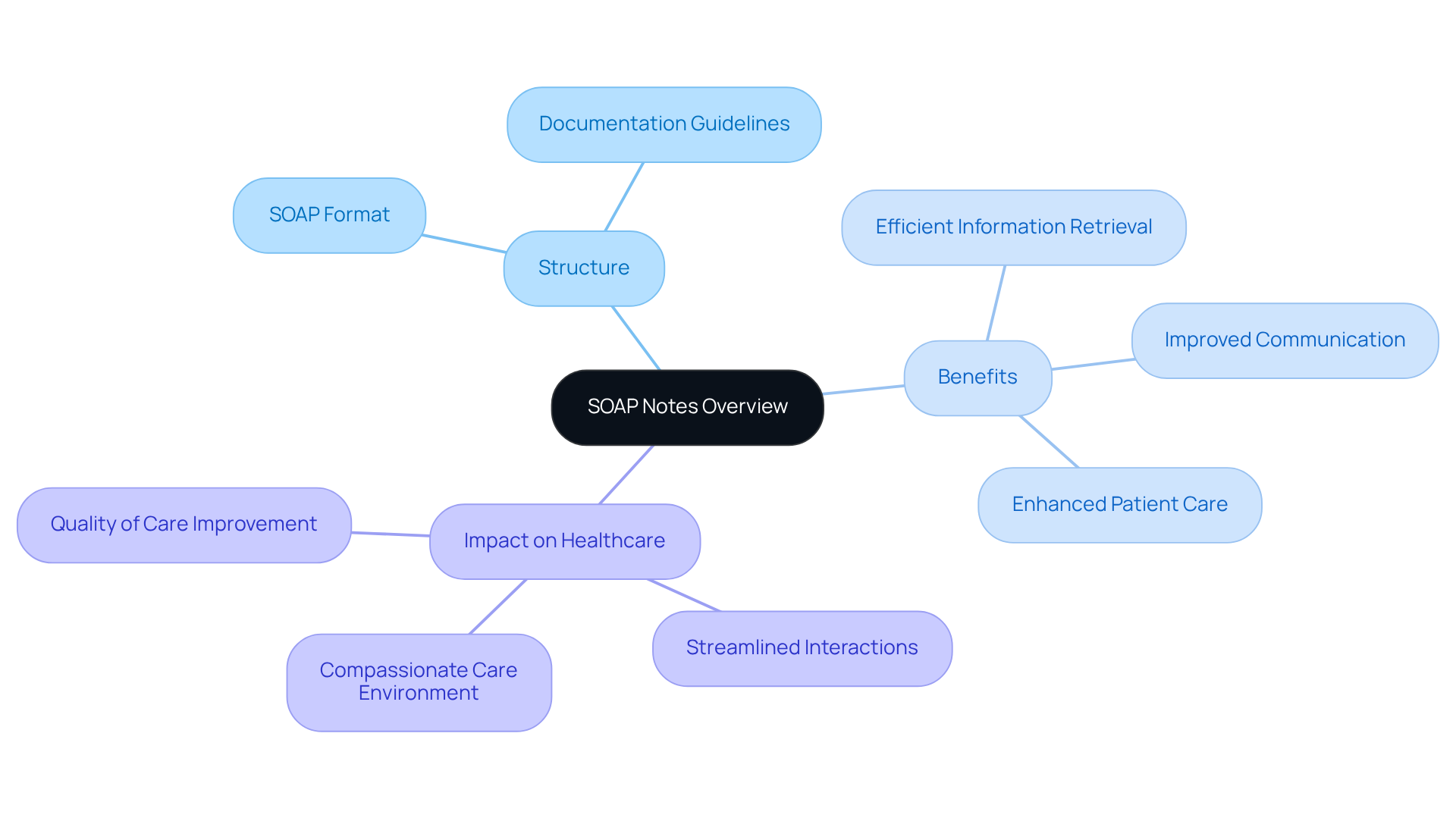
PhysioPedia: Overview of SOAP Notes and Their Advantages
In the demanding world of healthcare, providers often grapple with the emotional challenges of managing patient care alongside administrative tasks. It can feel overwhelming at times, can't it? PhysioPedia offers an extensive summary of clinical documentation, outlining its structure and benefits, which can significantly ease this burden. By adopting a structured approach to documentation, healthcare professionals can improve communication and streamline their interactions.
Imagine having a system in place that not only facilitates recording interactions but also allows for easy retrieval of information. This structured format ensures that critical details are never overlooked, fostering a more efficient and compassionate care environment. Recognizing the benefits of clinical records empowers healthcare providers to appreciate their role in enhancing care quality and record-keeping effectiveness.
By valuing these structured practices, you can transform the way you manage patient information. How might this change your daily interactions with patients? Embrace the opportunity to enhance your practice and ultimately improve patient outcomes. Let's take this step together towards a more organized and compassionate healthcare experience.
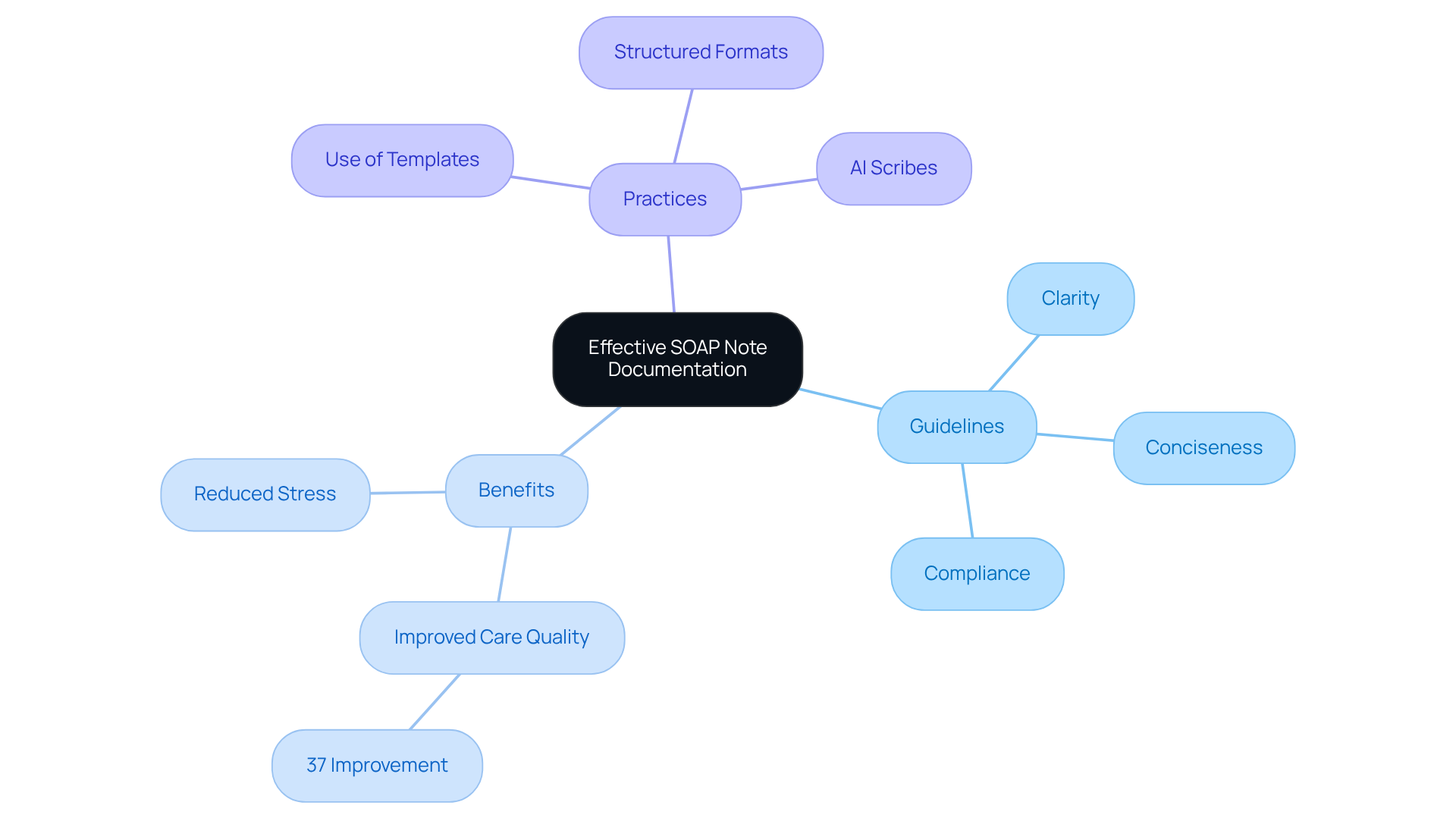
TherapyNotes Support: Guidelines for Effective SOAP Note Documentation
TherapyNotes Support understands the emotional challenges healthcare providers face when it comes to documenting progress reports. The burden of administrative tasks can often feel overwhelming, impacting the quality of patient care. That’s why we offer crucial instructions designed to make this process more manageable. Our guidelines emphasize clarity, conciseness, and compliance with healthcare regulations, allowing you to focus on what truly matters—your patients.
We encourage clinicians to document interactions swiftly and precisely, ensuring that all relevant information is captured. Have you ever felt the stress of trying to remember every detail? Organized records, such as structured formats, can significantly alleviate this pressure. Research shows that such organization can enhance treatment results by decreasing uncertainty and increasing clarity, with studies demonstrating improvements of up to 37% in care quality for individuals.
By following these supportive guidelines, healthcare providers can enhance the quality of their soap progress notes example. Imagine the positive impact this can have on overall patient care. We invite you to embrace these practices to not only improve your documentation but also to foster a nurturing environment for your patients. Together, let’s ensure that every interaction is meaningful and impactful.
Conclusion
By embracing the structured approach of SOAP progress notes, healthcare providers can alleviate the burdens of documentation and enhance the quality of patient care. Have you ever felt overwhelmed by the administrative tasks that take time away from patient interactions? This article illustrates how innovative solutions, particularly AI automation, can streamline the documentation process, allowing clinicians to focus more on what truly matters—caring for their patients.
The integration of organized templates and best practices not only improves record accuracy but also fosters a more compassionate healthcare environment. Key insights from the article highlight the efficiency gains achieved through AI tools, such as:
- Reducing record-keeping time by up to 40%
- Improving patient throughput by 30%
Imagine the positive impact on your daily routine when structured templates increase compliance rates dramatically and enhance overall documentation quality. By prioritizing clarity and consistency in record-keeping, healthcare providers can improve communication among teams and ensure better patient outcomes.
Ultimately, the significance of effective SOAP documentation transcends mere compliance; it is a vital component of delivering high-quality care. As the healthcare landscape continues to evolve, embracing these strategies and tools will empower providers to navigate their responsibilities more effectively. The call to action is clear: adopt these practices and resources to enhance documentation efficiency. Together, we can transform the patient care experience for the better.




