Overview
In the demanding world of healthcare, providers often face emotional challenges that can impact patient care. The article sheds light on the significance of the SOAP format in healthcare documentation, which stands for Subjective, Objective, Assessment, and Plan. This structured approach is not just a bureaucratic necessity; it plays a crucial role in enhancing communication among providers and improving patient outcomes.
Have you ever felt overwhelmed by administrative burdens? The article illustrates how the SOAP format alleviates some of these pressures by providing clear and organized records. This clarity not only supports clinical decision-making but also fosters continuity of care, ensuring that patients receive the attention they deserve.
Moreover, accurate documentation has financial implications in today’s healthcare landscape. By embracing the SOAP format, providers can navigate these complexities more effectively, ultimately benefiting both their practice and their patients.
Isn’t it time to consider how such a simple yet powerful tool can transform the way we care for our patients? The article encourages healthcare professionals to engage with this format, recognizing that it can lead to better patient care and improved communication among teams. Together, let’s strive for a more compassionate and efficient healthcare experience.
Introduction
In the intricate realm of healthcare, we understand that effective documentation is crucial for ensuring quality patient care. SOAP notes—standing for Subjective, Objective, Assessment, and Plan—offer a structured approach that empowers healthcare professionals to record patient interactions with clarity and precision. This standardized format not only enhances communication among providers but also plays a vital role in clinical decision-making and continuity of care.
As healthcare systems increasingly emphasize accurate documentation for billing and patient safety, it becomes essential for practitioners to grasp the nuances of SOAP notes. By doing so, they can optimize treatment outcomes and foster collaborative care. Have you ever considered how meticulous documentation can profoundly impact patient care? Delving into the components of SOAP notes highlights the importance of this practice in today’s evolving healthcare landscape.
We invite you to explore the benefits of embracing SOAP notes in your daily practice. Together, we can navigate the challenges of documentation and enhance the quality of care we provide to our patients.
Understanding SOAP Notes: A Comprehensive Overview
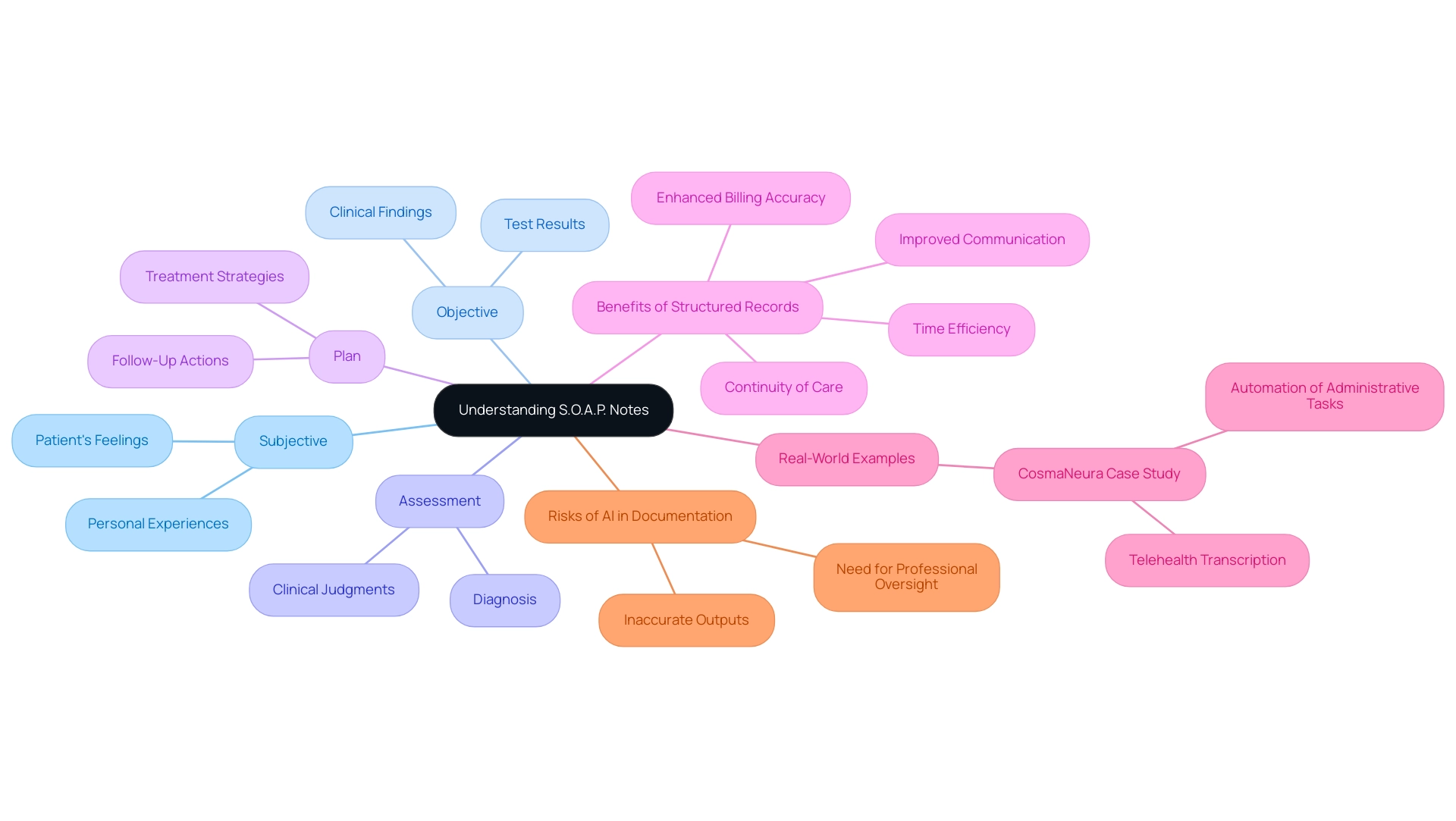
Structured records represent a vital support system for healthcare professionals, allowing them to document client interactions with efficiency and care. The acronym S.O.A.P. stands for Subjective, Objective, Assessment, and Plan, with each component playing a crucial role in capturing the individual’s experience and the clinician's insights.
This organized method not only streamlines clinical decision-making but also fosters continuity of care among various providers and settings. Have you ever considered how much easier it would be to navigate patient care with clear, structured documentation?
The importance of structured records in healthcare is particularly pronounced in 2025, as systems increasingly rely on accurate documentation for billing and coding. Precise records provide the necessary justification for treatments, ensuring the financial health of medical practices. Recent statistics show that effective documentation can significantly enhance billing accuracy, highlighting the essential role of standardized records in achieving the best possible outcomes.
Utilizing structured formats, such as S.O.A.P., brings numerous benefits to healthcare documentation, including improved communication among providers. This clarity is vital for coordinated care, as it clearly delineates subjective reports, objective findings, assessments, and actionable plans. In multidisciplinary teams, where collaboration is key, this shared understanding of needs and treatment strategies is invaluable.
Real-world examples of structured documentation illustrate their effectiveness in clinical environments. For instance, a case study involving CosmaNeura reveals how this platform enhances healthcare delivery by automating administrative tasks like appointment scheduling and medical record management. By optimizing workflows, providers can reclaim precious time to focus on patient care while adhering to ethical practices.
Moreover, integrating clinical records within such platforms ensures that documentation remains consistent and aligned with clinical workflows, ultimately improving care outcomes. Are we fully aware of how structured records can transform our approach to patient care?
Recent advancements in the use of clinical records indicate a growing recognition of the impact that standardized documentation has on care outcomes. Healthcare professionals are increasingly advocating for the adoption of S.O.A.P. formats, emphasizing their role in enhancing safety and treatment effectiveness. Experts agree that structured records not only assist in clinical evaluations but also elevate the overall quality of care provided to patients.
However, it’s crucial to approach record-keeping with caution. As Barry Sookman points out, relying on generative AI tools for documentation can pose risks, as they may produce inaccurate outputs that could endanger patient care. Fortunately, CosmaNeura addresses these concerns by ensuring that its record-keeping methods are robust and reliable, thereby enhancing care for individuals.
In summary, employing structured clinical records is an essential practice in modern healthcare, offering benefits that extend beyond mere documentation. By ensuring precise, consistent communication and leveraging AI solutions to ease administrative burdens, these records play a pivotal role in enhancing care and optimizing healthcare delivery. Let's continue to explore how we can improve our practices for the benefit of our patients.
The Subjective Section: Capturing the Patient's Voice
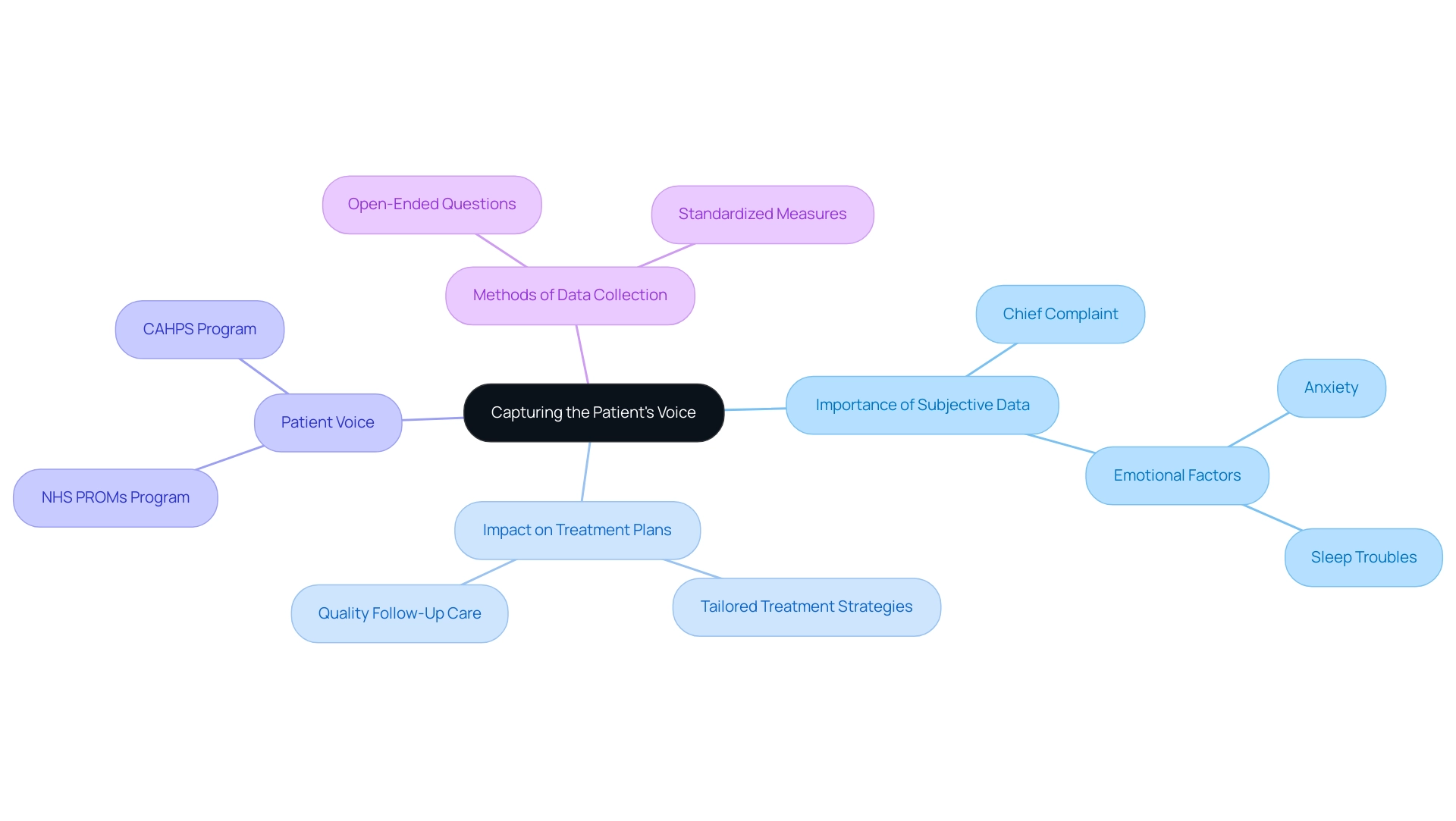
The Subjective section of SOAP format examples plays an essential role, as it captures the individual's self-reported symptoms, feelings, and concerns. This section typically includes the individual's chief complaint, relevant medical history, and any emotional or psychological factors that may influence their health. For instance, an individual might express, 'I have been feeling anxious and have trouble sleeping.'
Accurately capturing this information is vital for developing treatment plans tailored to the individual's unique needs.
Research indicates that collecting subjective data significantly impacts outcomes for individuals. A study analyzing outcome measures reported by individuals highlighted that quality follow-up care, informed by feedback from those individuals, can lead to improved clinical outcomes. As WY Cheung noted, 'This study used real-world population-level, retrospective administrative data from Alberta, Canada to assess the impact that reported outcome measures have on overall survival (OS) and other clinical outcomes among individuals with lung, breast, and colorectal cancer.' This emphasizes the necessity of incorporating the individual's voice into healthcare documentation.
Moreover, statistics reveal that medication-related harm affects 1 out of every 30 individuals, with over a quarter of these incidents being severe or life-threatening. This concerning frequency underscores the need for healthcare providers to focus on documenting subjective information, as it can directly impact medication management and the safety of individuals. Successful examples of system-level PROM and PREM programs, such as the English National Health Service (NHS) Proms program and the US Consumer Assessment of Healthcare Providers and Services (CAHPS) program, illustrate the real-world applications of patient-reported outcomes and their relevance to this discussion.
To effectively capture an individual's voice in SOAP format examples, healthcare providers should focus on open-ended questions that encourage individuals to share their experiences and emotions. For example, instead of asking, 'Are you feeling anxious?' a provider might ask, 'Can you describe how you've been feeling lately?' This approach not only enriches the data gathered but also fosters a therapeutic alliance between the provider and the individual.
Incorporating subjective information into treatment plans is essential for holistic care. Expert insights from psychologists emphasize that understanding an individual's emotional state can significantly enhance clinical decision-making. As one psychologist observed, recording client emotions in clinical documentation is not just advantageous; it is essential for effective treatment.
In summary, the Subjective part of a clinical document is more than merely a formality; it is a crucial element that guides treatment strategies and improves care. By prioritizing the collection of subjective data, healthcare providers can ensure that their approach is both compassionate and clinically effective.
The Objective Section: Documenting Observable Facts
The Objective section of a SOAP note plays a vital role in healthcare, as it encompasses measurable and observable data collected during client encounters. This includes essential elements such as vital signs, physical examination findings, and results from diagnostic tests. For instance, a clinician might document, 'Blood pressure: 120/80 mmHg; heart rate: 72 bpm.' Such accurate records are fundamental for establishing a baseline and tracking changes in an individual's condition over time.
Have you ever felt overwhelmed by the demands of documentation? Studies reveal that health professionals who feel they have adequate time to complete their records are significantly less likely to experience burnout, with odds reduced to 0.33 compared to those who do not. This underscores the importance of effective record-keeping methods, which not only enhance patient care but also support the well-being of healthcare professionals. Furthermore, improved records and monitoring may reduce the incidence of cardiac arrests, highlighting the critical role of precise logs in safeguarding individuals.
Integrating objective measurements into evaluations is essential. Vital signs and physical examination findings serve as foundational components in assessing an individual's health status. Current trends indicate that healthcare providers are increasingly recognizing the importance of accurately recording vital signs, as seen in SOAP format examples, which can lead to better patient outcomes.
CosmaNeura's platform addresses these challenges by automating administrative tasks, enabling providers to concentrate on capturing accurate objective data without the burden of excessive paperwork. Consider the case studies involving Next-Generation Clinical Information Systems in Critical Care; they illustrate how objective data enhances clinical assessments. These systems aim to prevent data loss and improve data processing, allowing healthcare professionals to focus on more complex tasks. Initial findings suggest that automatic calculations of vital signs can replace manual records, thereby streamlining the record-keeping process.
As Coiera noted, 'It is possible for a well-designed set of paper forms to be far more effective in improving the quality of a medical record than a poorly designed computer-based one.' This statement emphasizes the necessity for efficient record-keeping methods.
Experts emphasize that thoroughly recorded objective data, including SOAP format examples, not only aids clinical decision-making but also elevates the overall quality of medical records. One medical expert remarked that effective documentation practices can significantly enhance care outcomes. Therefore, adhering to best practices for recording objective information in structured entries is essential for all healthcare providers. Together, we can foster an environment where both patients and professionals thrive.
The Assessment Section: Analyzing Patient Information
The Assessment part of a clinical document is not just a procedural step; it plays a vital role in understanding the complexities of an individual's condition. By integrating information from both the Subjective and Objective sections, this section leads to a thoughtful clinical evaluation. It may include a definitive diagnosis or a differential diagnosis, both of which are essential in shaping the treatment plan. For instance, a clinician might note, 'Patient presents with symptoms consistent with generalized anxiety disorder.' This reflects a clear analytical process. Moreover, current trends in clinical assessment highlight the importance of structured documentation, such as SOAP format examples.
A study conducted at an 805-bed community hospital in Sarasota, Florida, found that implementing Clinical Decision Support Systems (CDSS) significantly increased the proportion of hospitalizations lasting 7 days or less. This underscores how structured assessments can improve patient outcomes.
The importance of clinical judgment in the Assessment section cannot be overstated. It requires healthcare providers to synthesize information effectively, drawing on both subjective reports and objective findings. Expert insights emphasize that this synthesis is crucial for accurate diagnosis and treatment planning.
For example, during the COVID-19 pandemic, a study at the Mayo Clinic revealed an 86.9% concordance rate between provisional diagnoses made during video telemedicine visits and subsequent in-person evaluations. Bart M. Demaerschalk, MD, MSc, observed that these findings suggest that video telemedicine visits may serve as valuable adjuncts to in-person care. This indicates that structured assessments can reliably inform clinical decisions, even in remote settings. In terms of common diagnoses derived from SOAP format examples, conditions such as hypertension, diabetes, and anxiety disorders frequently arise. The Assessment section is designed to first present the primary diagnosis, followed by any relevant differential diagnoses.
This structured approach not only enhances clarity but also improves communication among healthcare providers.
Consider a scenario where an individual presents with chest pain. The clinician might document potential differential diagnoses such as myocardial infarction, pulmonary embolism, or anxiety-related symptoms. This methodical approach ensures that all possible conditions are considered, facilitating a comprehensive treatment strategy.
In summary, the Assessment section is far more than a formality; it is a critical component of clinical decision-making that leverages both clinical judgment and structured analysis to enhance care. By recognizing the emotional challenges faced by healthcare providers and the importance of thorough assessments, we can foster a supportive environment that ultimately benefits patient outcomes.
The Plan Section: Outlining Treatment Strategies
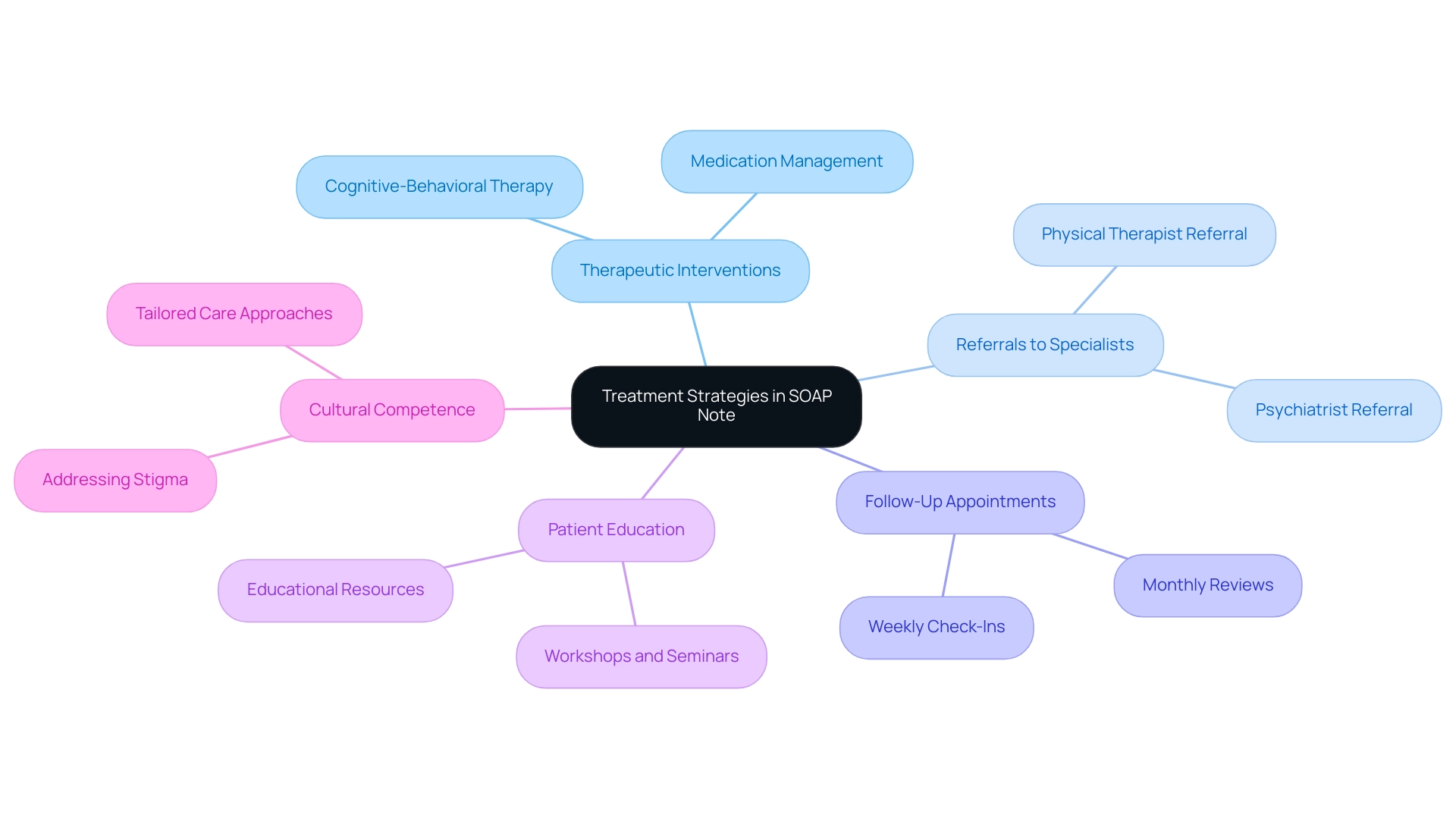
The Plan section of a SOAP note format is vital as it outlines the proposed course of action for an individual's treatment. This section can include various elements such as therapeutic interventions, referrals to specialists, follow-up appointments, and education for individuals. For instance, a clinician might document: Continue with cognitive-behavioral therapy sessions weekly; refer to a psychiatrist for medication evaluation. Such clarity is essential, as it ensures that everyone involved in the individual's care is aligned on the next steps.
Effective communication of treatment strategies through SOAP format is crucial for enhancing adherence and outcomes. Have you considered how structured treatment plans can significantly improve adherence rates among individuals? Research shows that clear documentation can lead to better understanding and compliance with prescribed therapies. For example, among 344 eligible individuals, 41 (11.9%) refused to participate and 4 (1.2%) withdrew during the interview process, underscoring the importance of engagement in treatment plans.
Additionally, integrating pharmacists into primary care teams has been associated with improved medication adherence. This highlights the benefits of collaborative care models. As healthcare industry veteran Martha Goldberg Aronson notes, "We believe improving medication adherence is one of the #1 ways to save lives, and we are happy to play a part in that change."
In the Plan section, it is important to include specific details such as:
- The type of therapy or intervention recommended
- Frequency and duration of treatment sessions
- Any necessary referrals to specialists
- Educational resources provided to the patient
By incorporating these elements, healthcare providers can foster a more comprehensive approach to patient care, ultimately leading to better health outcomes. Furthermore, addressing cultural competence in healthcare systems can tailor care to align with individuals' belief systems, improving adherence and reducing unnecessary resource use. It's important to recognize that stigma associated with certain medical conditions can lead to shame and isolation, further impacting treatment adherence.
Clear treatment strategies not only enhance understanding for individuals but also contribute to overall job satisfaction for providers, as they can see the direct impact of their planning on health.
Common Mistakes to Avoid in SOAP Note Writing
Frequent errors in medical documentation can be frustrating for healthcare providers, often stemming from unclear language, insufficient records, and delays in revising entries. Consider a statement like 'the individual is doing well'—it lacks the detail needed to accurately convey a patient's condition, which could lead to misinterpretations in care. Research shows that vague language is common in SOAP format examples, potentially compromising the quality of care and hindering effective communication among healthcare professionals.
To address these challenges, clinicians should prioritize clarity and specificity in their documentation. Each record should provide concrete evidence of the patient's status, including specific symptoms, measurable outcomes, and clear care plans. Timeliness is crucial; promptly updating records ensures that all team members have access to the most current information, which supports better decision-making and continuity of care.
Implementing organized record-keeping practices can greatly enhance the quality of SOAP format examples. For instance, adopting electronic record-keeping systems with automatic error detection can help minimize common mistakes and improve overall accuracy. As emphasized by Compliancy Group, '[they] make a highly complex process easy to understand,' highlighting the importance of simplifying record-keeping practices.
CosmaNeura stands out as the sole company developing AI solutions for the billion-dollar faith-focused healthcare sector, uniquely positioned to enhance record-keeping practices through its innovative platform. The case study titled
Practical SOAP Note Examples Across Healthcare Specialties
Practical illustrations of clinical documentation can differ greatly among healthcare specialties, showcasing the adaptability of this essential record format. In the realm of mental health, for instance, a structured record might be organized as follows:
- Subjective: 'Patient reports feeling overwhelmed and anxious.'
- Objective: 'Patient appears restless, fidgeting during the session.'
- Assessment: 'Symptoms consistent with generalized anxiety disorder.'
- Plan: 'Continue therapy sessions weekly; consider medication evaluation.'
This example highlights how the structured format can be tailored to meet the unique needs of mental health professionals while ensuring clarity and structure.
Conversely, in a primary care setting, structured documentation might center on a physical ailment:
- Subjective: 'Patient complains of persistent headaches for the past week.'
- Objective: 'Blood pressure is 130/85; no neurological deficits observed.'
- Assessment: 'Tension-type headache likely due to stress.'
- Plan: 'Recommend stress management techniques and follow-up in two weeks.'
These variations underscore the flexibility of the format across different clinical environments. Research indicates that the APSO order, which reorganizes the elements of the structured format, can enhance speed, task success, and usability for physician users. This finding emphasizes the importance of adapting recording styles to fit specific clinical situations. Moreover, specialty-specific modifications of structured formats can significantly improve communication among healthcare providers. For example, in pediatrics, a clinical note may include developmental milestones in the assessment, while in geriatrics, it may emphasize functional status and social support systems.
Expert opinions affirm that adapting the structured format is vital for effective documentation across various medical disciplines. Mental health professionals, for instance, often find that integrating additional elements, such as the SOAPE extension, facilitates better tracking of changes over time, addressing traditional limitations of the assessment model. This extension can prove especially beneficial in complex situations, such as Martin's, who reported a notable deterioration of his depressive symptoms, describing them as more frequent and intense, necessitating urgent attention and intervention.
In summary, practical examples of structured documentation, such as SOAP format examples, across diverse healthcare specialties not only illustrate the format's versatility but also highlight its effectiveness in enhancing care and communication among providers. As CosmaNeura continues to innovate within the faith-focused healthcare market, the importance of SOAP format examples remains crucial in ensuring comprehensive and ethical patient documentation.
Conclusion
The implementation of SOAP notes stands as a cornerstone of effective healthcare documentation, ensuring that patient encounters are recorded with clarity and precision. Through the structured components of Subjective, Objective, Assessment, and Plan, healthcare professionals can enhance communication, improve clinical decision-making, and foster continuity of care. This meticulous approach not only aids in justifying treatment plans for billing purposes but also plays a pivotal role in improving patient safety and treatment efficacy.
The benefits of utilizing SOAP notes extend beyond mere documentation; they facilitate a comprehensive understanding of patient needs and treatment strategies. By integrating patient-reported outcomes and objective measurements, healthcare providers can create tailored treatment plans that address both physical and emotional health. Furthermore, avoiding common pitfalls in SOAP note writing—such as vague language and incomplete documentation—ensures that patient care remains at the forefront.
As the healthcare landscape continues to evolve, the adaptability of the SOAP format across various specialties underscores its relevance. Whether in mental health, primary care, or specialized fields, the ability to customize SOAP notes enhances collaboration among providers and leads to better health outcomes. By embracing standardized documentation practices, healthcare professionals can navigate the complexities of patient care more effectively, ultimately improving the quality of care delivered.
In conclusion, SOAP notes are not just a regulatory requirement; they are a vital tool that empowers healthcare professionals to deliver high-quality, patient-centered care. By prioritizing structured documentation and addressing the nuances of each patient encounter, practitioners can significantly impact treatment outcomes and enhance the overall healthcare experience.




