Overview
This article delves into the essential steps for mastering the SOAP format in progress notes, a vital skill for enhancing clarity in healthcare documentation. Have you ever felt overwhelmed by the complexities of documenting patient care? Understanding and effectively utilizing each component—Subjective, Objective, Assessment, and Plan—can significantly alleviate these concerns. By improving communication among healthcare professionals, we can foster an environment that ultimately leads to better patient care outcomes.
Consider the impact of clear documentation practices. They not only streamline workflows but also enhance collaboration among team members. With evidence supporting improved documentation practices, it’s clear that mastering the SOAP format is not just beneficial; it’s essential. Imagine the difference it could make in your daily interactions and the care you provide.
We encourage you to explore these steps further. By embracing the SOAP format, you can transform your documentation process and, in turn, enhance the quality of care you deliver. Together, let’s work towards a future where effective communication is at the heart of healthcare.
Introduction
In the realm of healthcare, effective communication and documentation are essential for delivering quality patient care. Have you ever felt overwhelmed by the administrative demands of your role? The SOAP format—an acronym for Subjective, Objective, Assessment, and Plan—offers a compassionate framework for healthcare professionals to systematically record patient interactions.
By breaking down each component, this approach not only enhances clarity but also fosters collaboration among providers. This ensures that every aspect of a patient's health is meticulously documented.
As the healthcare landscape evolves, mastering the SOAP format becomes increasingly vital for professionals like you, who strive to improve patient outcomes amidst the complexities of modern documentation practices. Imagine a future where technology and best practices seamlessly integrate to revolutionize how patient information is managed and utilized. Together, we can navigate these challenges and embrace the potential of SOAP notes to enhance the care we provide.
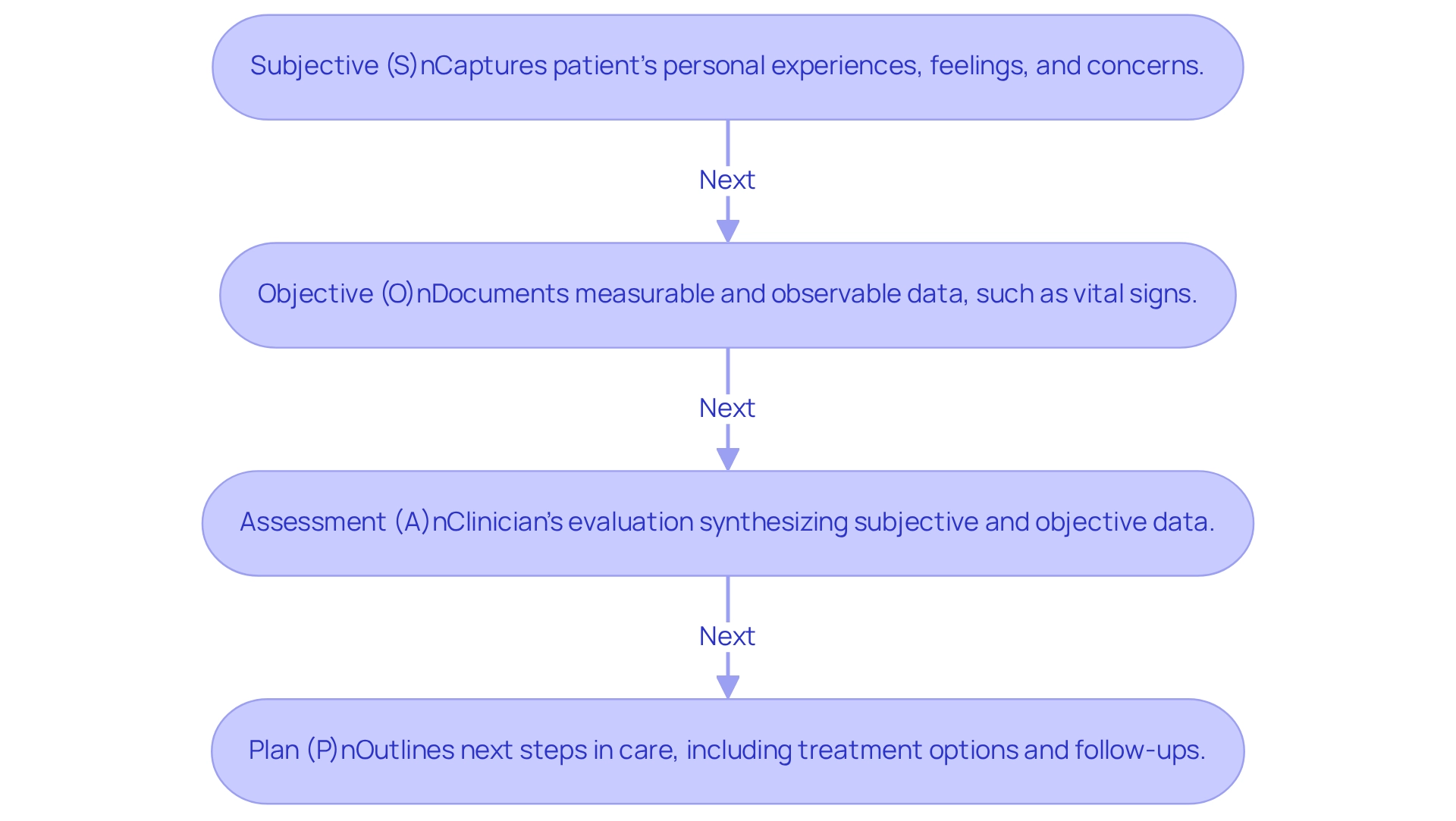
Understand the SOAP Format: Structure and Purpose
The progress notes SOAP format—Subjective, Objective, Assessment, and Plan—serves as a systematic method that healthcare professionals use to efficiently record their interactions with individuals. Each component plays a vital role in ensuring comprehensive patient care, addressing the emotional and practical needs of both providers and patients.
- Subjective (S): This section captures the patient's personal experiences, feelings, and concerns regarding their health. By incorporating direct quotes from individuals, we gain valuable insights into their condition, allowing us to understand their perspective better.
- Objective (O): Here, clinicians document measurable and observable data, such as vital signs, physical examination findings, and diagnostic test results. This factual information establishes a baseline for the individual’s condition, facilitating accurate assessments and fostering trust in the care process.
- Assessment (A): This section includes the clinician's professional evaluation, synthesizing both subjective and objective data. It may encompass a diagnosis or a summary of the individual's progress, providing clarity on their health status and reassuring them that their concerns are being addressed.
- Plan (P): The final section outlines the next steps in the individual's care, detailing treatment options, referrals, and follow-up appointments. This ensures continuity of care and establishes clear expectations for both the clinician and the individual receiving care, nurturing a supportive environment.
The organized format of clinical documentation significantly improves communication among healthcare professionals. Recent reports highlight that effective documentation is crucial for preserving a clear understanding of an individual's health condition. Case studies, such as 'Enhancing Interdisciplinary Communication with Structured Documentation,' illustrate that structured documentation fosters smooth communication among various professionals caring for a single patient, ultimately enhancing .
As we look toward 2025, the significance of documentation remains dynamic, adapting to current recording requirements while preserving its core aim of promoting cooperative problem-solving and informed decision-making. As healthcare expert Austin Chia states, 'Documentation isn’t solely for the practitioner who creates it. They keep all healthcare professionals on the same page, reducing miscommunication and ensuring continuity of care.' Furthermore, Mousa Kadaei Moses emphasizes that using the progress notes SOAP format for documentation represents a lasting method to guarantee cooperative problem-solving and comprehensive care in the medical field. Mastering the progress notes SOAP format is essential for healthcare professionals, not only to improve care quality but also to ensure effective communication within the medical team. Reflect on how adopting this approach can transform your practice and enhance the care you provide.
Break Down Each Component: Subjective, Objective, Assessment, and Plan
To effectively write SOAP notes, it’s essential to understand each component, as they play a crucial role in patient care:
- Subjective: This section captures the patient's own words, including their chief complaint, history of present illness, and relevant past medical history. For instance, if an individual expresses, "I've been feeling anxious and unable to sleep," this should be documented verbatim to reflect their experience accurately.
- Objective: Here, measurable data is documented, such as vital signs, lab results, and findings from physical examinations. An example would be: "Blood pressure: 120/80 mmHg; Heart rate: 72 bpm; No abnormalities noted during the physical exam." This data provides a factual basis for clinical assessments.
- Assessment: This component summarizes the clinician's interpretation of both subjective and objective data. For example, one might note, "Patient presents with generalized anxiety disorder, likely exacerbated by recent life stressors." This synthesis is vital for guiding treatment decisions.
- Plan: The treatment plan outlines the next steps, including medications, referrals, and follow-up appointments. An example might be: "Start individual on SSRIs; schedule follow-up in four weeks to assess progress." This guarantees continuity of care and establishes clear expectations for the individual receiving treatment.
By clearly defining each component, healthcare providers can create in SOAP format that enhance individual care and facilitate effective communication among the care team.
Yet, we recognize that administrative duties can often feel overwhelming. Optimizing these tasks with AI tools, like automated appointment booking and medical record handling, can significantly improve record-keeping methods. Imagine being able to focus more on meaningful interactions with your clients! Statistics suggest that efficient record-keeping methods can greatly enhance user involvement, with projections revealing there are more than 40,000 health-related applications currently accessible, and 1 in 5 smartphone owners possessing at least one health app.
Using these tools can simplify the record-keeping process, allowing you to concentrate more on client interactions. As Updox states, "Updox makes it easy to create using your mobile devices, reducing no-shows, and eliminating phone tag," highlighting the importance of effective communication in healthcare.
Moreover, a case study showed that a global pharmaceutical firm enhanced clinical trial retention from 76% to 92% by employing engagement analytics. This illustrates how better documentation practices can lead to improved health outcomes. Together, let’s embrace these tools to foster a more compassionate and efficient healthcare environment.
Implement Best Practices: Tips for Writing Clear and Effective SOAP Notes
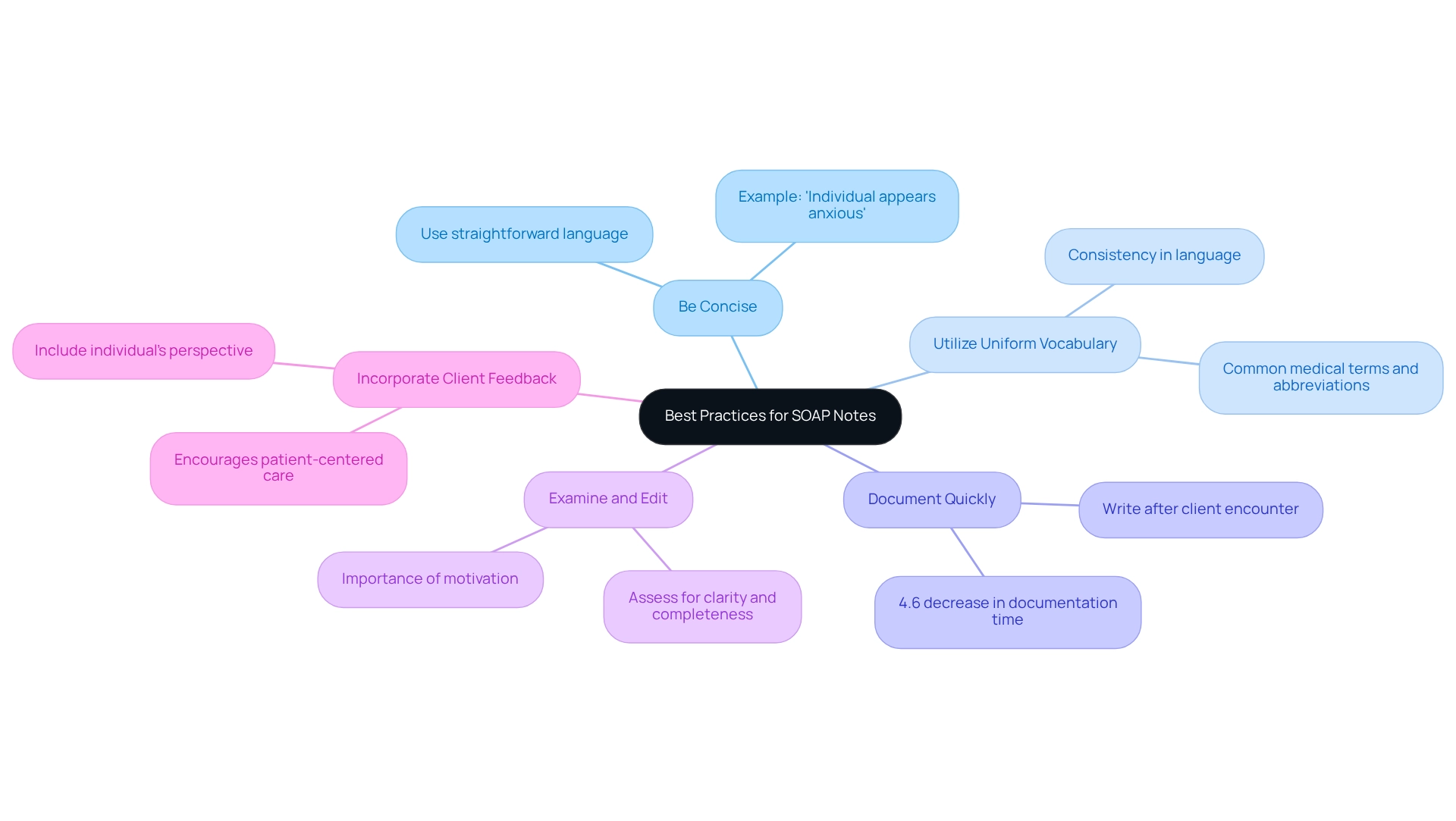
To craft clear and effective SOAP notes, it’s essential to embrace best practices that not only enhance communication but also alleviate some of the burdens you may face in your daily work.
- Be Concise: Use straightforward language to convey information succinctly. For instance, instead of saying, "The individual seems to be in a state of distress," simply state, "Individual appears anxious." This small change can make a big difference in clarity.
- Utilize Uniform Vocabulary: Consistency in language is vital for ensuring that all healthcare providers can understand the records precisely. Employ commonly accepted medical terms and abbreviations to enhance clarity. This shared understanding fosters better collaboration among the team.
- Document Quickly: Aim to write your SOAP records right after the client encounter. This practice not only ensures accuracy but also minimizes the risk of omitting critical details. Timely documentation can significantly improve patient care outcomes; studies indicate that implementing EHR systems is associated with a 4.6% decrease in .
- Examine and Edit: Before finalizing your records, take the time to assess them for clarity and completeness. Confirm that all pertinent information is included and that the notes are easily readable. Remember, driven healthcare professionals often exhibit exceptional record-keeping practices, highlighting the importance of motivation in this process.
- Incorporate Client Feedback: Whenever possible, include the individual’s perspective in the subjective section. This approach not only enriches the records but also encourages a patient-centered care model, fostering a deeper connection with those you serve.
By applying these best practices, you can enhance the quality of your progress notes SOAP format, fostering improved communication and ultimately leading to better care outcomes. Recent advancements in electronic health records (EHRs) have indicated a 4.6% reduction in combined patient care and record-keeping time, underscoring the importance of efficient record practices. As pointed out by Addisalem Workie Demsash, knowledge, training, and the accessibility of standard tools are statistically significant elements for routine practice recording, further highlighting the role of technology in improving recording efficiency. Embrace these strategies and see the positive impact they can have on your practice and the care you provide.
Leverage Technology: Tools for Efficient SOAP Note Management
To enhance the efficiency of SOAP note management, healthcare providers face significant challenges that can impact their ability to deliver quality patient care. The burden of administrative tasks can be overwhelming, leaving less time for what truly matters—patient interaction. Thankfully, there are technology tools that can help ease these burdens and improve the documentation process.
- Electronic Health Records (EHR): Many EHR systems offer integrated templates that simplify recording. These systems provide straightforward access to patient histories, streamlining thorough documentation. CosmaNeura's platform enhances healthcare provision through AI-driven services, significantly improving administrative effectiveness and documentation processes.
- SOAP Note Apps: A range of mobile applications is specifically designed for creating and managing SOAP notes. With features like voice dictation, these apps save time and improve accuracy in record-keeping. The rising adoption of mobile apps for healthcare record-keeping underscores their growing importance in the field.
- Practice Management Software: Comprehensive solutions often include structured record features that allow for seamless record-keeping alongside scheduling and billing, enhancing overall workflow.
- Templates and Checklists: Utilizing standardized formats and checklists ensures that all essential information is documented. This approach reduces the cognitive load on clinicians and fosters consistency across records.
- AI-Powered Tools: , such as those from CosmaNeura, can generate clinical summaries based on patient interactions, significantly reducing documentation time while maintaining accuracy. The future of AI in documentation management looks promising, with advancements expected to improve care quality and lower healthcare costs. A case study titled "Future Possibilities for AI Soap" illustrates these developments, suggesting that AI will play a vital role in enhancing healthcare delivery.
By leveraging these technological tools, healthcare providers can streamline their management of progress notes soap format, allowing them to focus more on patient care and less on administrative tasks. As John Doe noted, "This is an excellent speech recognition software that has greatly improved our clinical documentation process," highlighting the tangible benefits of integrating technology into healthcare documentation. Together, we can embrace these advancements and foster .
Conclusion
Effective communication and documentation are not just tasks; they are essential elements of delivering quality patient care. The SOAP format emerges as a vital tool for healthcare professionals, enabling them to navigate the complexities of patient interactions. By breaking down these interactions into Subjective, Objective, Assessment, and Plan components, providers can create documentation that is both comprehensive and clear. This clarity enhances collaboration among the healthcare team and supports informed decision-making, ultimately leading to improved patient outcomes. In a world where every detail matters, mastering this structure becomes indispensable.
Implementing best practices for writing SOAP notes—such as being concise, using standardized terminology, and documenting promptly—can significantly enhance the clarity and effectiveness of these notes. The integration of technology, including Electronic Health Records, SOAP note apps, and AI-powered tools, presents healthcare providers with innovative solutions to streamline documentation processes. Imagine focusing more on meaningful patient interactions rather than getting bogged down by administrative burdens. This shift not only improves efficiency but also elevates the quality of care provided.
As we witness the healthcare landscape evolve, mastering the SOAP format and embracing technological advancements will be crucial. By fostering a collaborative environment that prioritizes patient-centered care, we can ensure that every aspect of a patient's health is meticulously documented and effectively communicated. The future of healthcare depends on these tools and methodologies to navigate complexities and enhance patient outcomes. Let us embrace these practices together, reinforcing the importance of effective documentation in delivering compassionate, quality care.




