Overview
This article serves as a compassionate guide for healthcare providers, addressing the emotional challenges they face in writing effective sample medical notes. It underscores the critical role of documentation in patient care and legal compliance, recognizing how administrative burdens can impact the quality of care delivered. By highlighting key components of medical notes and various formats like SOAP notes, the article presents practical solutions to enhance record-keeping.
Moreover, it emphasizes the transformative role of technology in improving communication among healthcare teams. Well-structured notes are not just bureaucratic necessities; they are vital for ensuring continuity of care and fostering collaboration. This understanding invites healthcare providers to reflect on their practices and consider how they can improve their documentation processes.
In conclusion, we encourage you to engage with this guide and explore the benefits of effective medical note-taking. By doing so, you can enhance the quality of care you provide and support your colleagues in the healthcare field. Together, let's strive for excellence in patient care through thoughtful documentation.
Introduction
In the intricate world of healthcare, medical notes play a crucial role in fostering effective communication and compassionate patient care. These vital documents not only capture the nuances of a patient's journey but also ensure that every member of the healthcare team is aligned in their approach. As we increasingly rely on electronic health records (EHRs), it becomes essential to understand the significance of thorough and accurate documentation. How often do we consider the emotional weight of these notes?
This article explores the multifaceted role of medical notes, shedding light on their importance in:
- Continuity of care
- Legal protection
- The integration of advanced technologies like AI solutions
By examining various types of medical notes and best practices for effective documentation, we highlight how these practices enhance patient outcomes and align with ethical standards in healthcare. Let’s take a moment to reflect on how we can improve our documentation processes and, in turn, the care we provide.
Understanding the Importance of Medical Notes in Healthcare
A sample medical note is not just a record; it is the cornerstone of communication among healthcare providers, ensuring that every member of the support team is fully informed about an individual's condition, treatment plan, and progress. This record is essential for continuity of treatment, as it creates a thorough account of interactions and clinical decisions. Have you ever considered how efficient medical records can significantly enhance patient outcomes? They enable informed clinical choices and foster collaborative support, making a real difference in patient care.
Moreover, well-documented notes serve as a vital legal safeguard for healthcare providers. Precise records can offer crucial proof in legal circumstances, showcasing compliance with set standards of practice and aiding in correct billing procedures. As we look ahead to 2025, the importance of medical notes is underscored by the increasing reliance on electronic health records (EHRs). Yet, despite their benefits, many face challenges in adoption due to various barriers.
According to a case study titled "Challenges of EHR Adoption," these barriers include behavioral, technical, legal, socio-demographic, and knowledge-related factors, particularly pronounced in developing countries. Addressing these challenges is essential for enhancing the implementation of EHRs and ensuring that medical documentation remains effective and beneficial.
The role of medical notes extends beyond simple record-keeping; they are essential to the continuity of treatment. When healthcare providers keep detailed and precise notes, they ensure that all team members are aligned in their approach to client support. This alignment is critical, especially in complex cases where multiple providers are involved.
As emphasized in recent case studies, the absence of effective documentation can lead to disjointed support, ultimately affecting individual outcomes adversely. Additionally, the S. Census Bureau highlights that the average American relocates 11.7 times during their lifetime, which complicates the continuity of treatment as patient histories may be scattered among various providers.
In summary, the significance of a sample medical note in cannot be overstated. They not only improve the quality of service but also safeguard medical providers legally. Creating a sample medical note to record and communicate suitable treatment effectively is crucial. As the medical field continues to evolve, the focus on strong health records will remain a vital element in providing excellent service to individuals.
Furthermore, CosmaNeura stands out as the sole enterprise developing AI solutions for the billion-dollar faith-centered medical market. The incorporation of advanced technology, like computerized physician order entry applications with decision-support capabilities, can further enhance medical records and minimize errors, ultimately benefiting individuals receiving treatment. This specialized approach to integrating AI solutions is essential for medical startups aiming to enhance patient support and streamline administrative tasks. CosmaNeura's AI solutions specifically tackle the challenges of conventional B2B SaaS models by offering customized features that improve record-keeping processes, ensuring that medical providers can deliver comprehensive and coordinated care.
Types of Medical Notes: An Overview for Healthcare Providers
Healthcare providers often face emotional challenges in their roles, navigating the complexities of patient care while managing administrative tasks. To alleviate these burdens, various types of medical notes have been developed, each serving a specific purpose that enhances communication within the healthcare system.
- SOAP Notes: This structured format—Subjective, Objective, Assessment, and Plan—provides a clear method for documenting encounters with individuals. SOAP notes simplify the monitoring of progress, enabling providers to make informed decisions with confidence.
- Progress Notes: Essential for tracking an individual's ongoing treatment and response to therapy, these notes are updated during each visit. They create a continuous narrative of the individual's health journey, ensuring that all members of the healthcare team are informed of the latest developments.
- Discharge Summaries: Comprehensive discharge summaries encapsulate an individual's hospital stay, detailing treatments received and providing follow-up instructions. These documents are crucial for ensuring continuity of treatment and preventing readmissions, as they inform subsequent providers about the individual's condition and treatment plan.
- History and Physical (H&P) Notes: Created during the initial visit, H&P notes provide a thorough record of an individual's medical history and physical examination findings. This foundational documentation is vital for establishing a baseline for future care and guiding clinical decision-making.
- Referral Notes: When an individual is referred to another provider, referral notes convey pertinent medical history and the rationale for the referral. These documents ensure that the receiving provider has the necessary context to deliver appropriate care.
Understanding the distinct purposes of these medical notes is essential for effective communication in the medical field. Each type plays a crucial role in recording interactions, fostering collaboration among providers, and ultimately enhancing patient care. Notably, as of 2016, over 95% of qualified and Critical Access hospitals demonstrated meaningful use of certified health IT, underscoring the importance of organized record-keeping in modern medical practices.
Platforms like CosmaNeura significantly enhance the efficiency of . By integrating AI solutions, CosmaNeura allows service providers to focus more on client support and less on administrative burdens. This integration not only streamlines documentation but also ensures that healthcare providers can deliver high-quality service while upholding ethical standards.
In this evolving landscape, let’s embrace the tools and practices that can lighten our load and enhance our ability to care for those who depend on us.
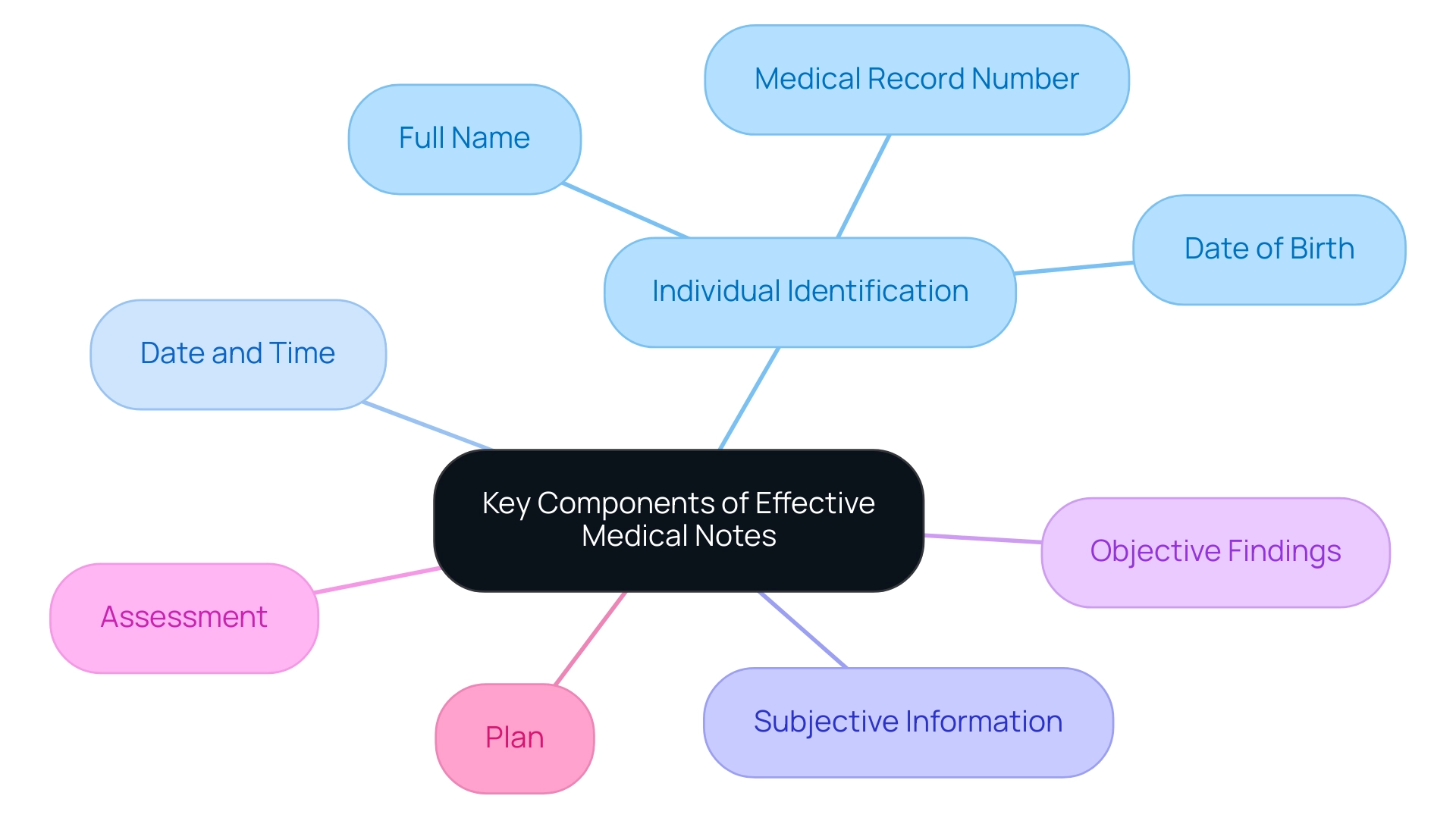
Key Components of Effective Medical Notes
Effective medical notes are essential for high-quality patient care, and they should encompass several key components that truly matter:
- Individual Identification: Include the individual's full name, date of birth, and medical record number. This ensures accurate identification and helps prevent errors in treatment.
- Date and Time: Documenting the date and time when the note is written is crucial for tracking progress and maintaining a chronological record of care.
- Subjective Information: Capture patient-reported symptoms, concerns, and relevant medical history. This information offers essential context for clinical decisions and aids in comprehending the individual's perspective.
- Objective Findings: Record clinician observations, vital signs, and results from physical examinations or diagnostic tests. This objective information is essential for creating a thorough perspective on the individual's health status.
- Assessment: Summarize the clinician's evaluation of the individual's condition, integrating both subjective and objective data. This section reflects the clinician's clinical judgment and reasoning.
- Plan: Outline detailed instructions for further treatment, referrals, or follow-up appointments. A clear plan guarantees continuity of care and establishes expectations for both the individual and the care team.
Incorporating these components not only enhances the comprehensiveness of sample medical notes but also improves communication among healthcare providers. Have you considered how efficient record-keeping methods can lower the chance of miscommunication? This is vital in intricate situations, such as those involving individuals with resistant hypertension. In the Hex trial, where was evaluated, careful recording of participant responses and treatment plans was essential for assessing the intervention's efficacy.
Moreover, the significance of individual identification in medical documentation cannot be overstated. Precise identification is essential to ensuring that the correct individual receives the appropriate care. A case study demonstrated that errors in individual identification can lead to adverse outcomes, underscoring the need for diligence in this area.
Indeed, a case series investigation revealed that 47 individuals experienced new or worsening heart failure during TNF antagonist treatment. This emphasizes the essential importance of comprehensive record-keeping in avoiding such negative results.
By following these best practices in taking a sample medical note, providers can improve the quality of care given, ultimately benefiting outcomes for individuals. Furthermore, these practices align with the ethical guidelines of Catholic teachings, ensuring that documentation not only serves clinical purposes but also upholds the moral responsibilities of healthcare providers. Together, let’s strive to enhance our documentation practices for the benefit of all.
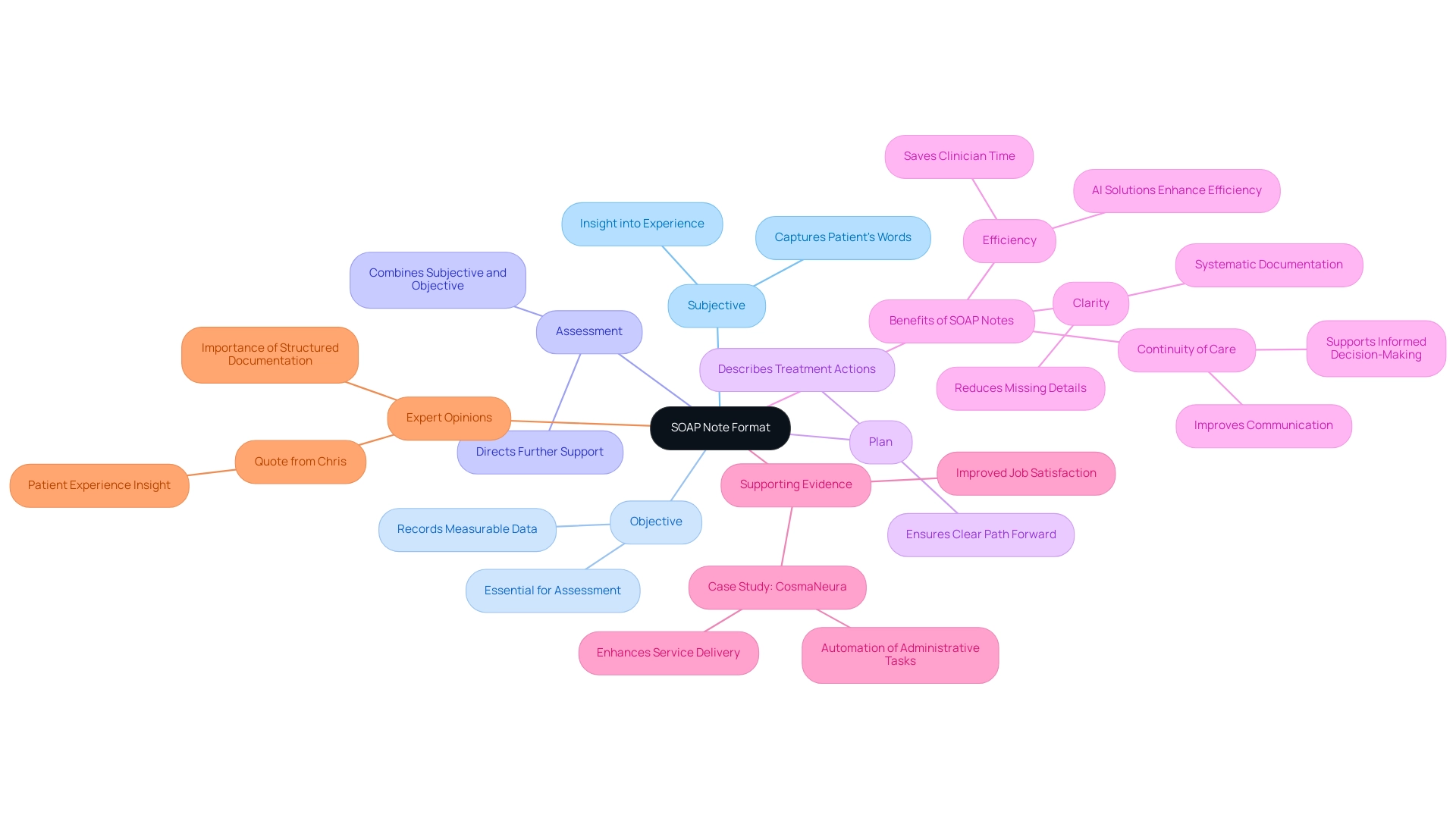
The SOAP Note Format: Structure and Benefits
stands as a compassionate and effective method for documenting patient encounters, comprising four distinct sections:
- Subjective: This section captures the individual's own words regarding their symptoms and concerns, offering valuable insight into their experience and emotional state.
- Objective: Here, clinicians record measurable data, such as vital signs and physical examination findings, which are essential for accurate clinical assessment.
- Assessment: This section combines the subjective and objective information, resulting in a diagnosis or clinical impression that directs additional support.
- Plan: The final section describes the subsequent actions in the individual's treatment, including therapies, referrals, and follow-up appointments, ensuring a clear path forward.
Benefits of SOAP Notes:
- Clarity: The structured format of SOAP notes ensures that all relevant information is documented systematically, reducing the risk of missing critical details.
- Efficiency: By simplifying the record-keeping process, SOAP notes enable medical providers to log and access information more easily, greatly minimizing the time spent on administrative duties. In fact, studies indicate that effective documentation practices can save clinicians several hours each week, enabling them to concentrate more on care. This efficiency is further enhanced by AI solutions, such as those offered by CosmaNeura, which automate administrative tasks like appointment scheduling and billing through intuitive interfaces and seamless integration with existing systems, alleviating the burden on service providers.
- Continuity of Care: SOAP notes improve communication among medical professionals by offering a clear and concise summary of encounters with individuals. This continuity is vital for maintaining high-quality care, as it allows for better collaboration and informed decision-making across different providers.
Supporting Evidence:
Research highlights that the use of SOAP notes can lead to improved job satisfaction among healthcare providers, as they reduce the administrative burden associated with patient documentation. A case study on CostaNera illustrates this point, showing how the platform's automation of administrative tasks not only enhances service delivery but also promotes revenue growth through optimized billing practices, all while adhering to ethical guidelines of Catholic institutions. CosmaNeura is distinctly situated as the sole enterprise developing AI solutions for the billion-dollar faith-oriented medical sector, further highlighting the significance of effective record-keeping methods like SOAP notes.
Expert Opinions:
Experts in the field emphasize the importance of structured documentation formats like SOAP notes in improving clinical efficiency. By making clinically relevant data easier to locate, SOAP notes act as a sample medical note that assists in reducing clinician burden and potential individual harm, ensuring that healthcare providers can deliver the highest quality service. As one individual, Chris, noted, "I haven’t been eating well lately and I’ve lost my appetite," highlighting the significance of capturing experiences in SOAP notes to enhance the quality of care.
Sample SOAP Notes: Practical Examples for Reference
Here are some illustrative examples of SOAP notes that exemplify effective documentation:
Example 1:
- Subjective: "I have been experiencing severe headaches for the past week. They are worse in the morning."
- Objective: Patient appears in mild distress. Blood Pressure: 130/85, Heart Rate: 72, Temperature: 98.6°F. Neurological examination is normal.
- Assessment: Likely tension headaches; consider migraine if symptoms persist.
- Plan: Recommend over-the-counter pain relief, hydration, and follow-up in one week.
Example 2:
- Subjective: "I feel anxious and have trouble sleeping."
- Objective: Patient reports a sleep duration of 4 hours per night. No significant findings on physical examination.
- Assessment: Generalized anxiety disorder.
- Plan: Initiate therapy sessions and consider medication if symptoms do not improve.
These examples illustrate how the SOAP format can be utilized to create a sample medical note for documenting patient encounters. By adhering to this structure, healthcare providers can ensure that their sample medical note is clear and concise, facilitating better communication and care delivery.
Research indicates that utilizing the SOAP format can significantly improve record-keeping practices. For instance, one study found that the APSO order outperformed in terms of speed, task success, and usability for physician users. This emphasizes the significance of adopting efficient record-keeping strategies to alleviate the administrative burden on clinicians.
As mentioned in a recent quote, "By writing SOAP notes, specialists can spend less time trying to decipher medical notes, and more time providing assistance to those they serve." This strengthens the importance of organized records in enhancing healthcare.
Additionally, the challenges of electronic medical records have led to longer and more complex notes, which can overwhelm clinicians if not managed properly. Efficient records, such as a sample medical note, not only streamline the workflow but also contribute to enhanced outcomes for individuals, as precise and organized notes minimize the time spent interpreting medical files, allowing greater focus on individual well-being. Providers can adapt these examples to fit their specific clinical scenarios, ensuring that the most clinically relevant data is easily accessible.
The ongoing need for research in knowledge integration, as indicated by Shapley additive explanations, further emphasizes the potential for improvement in documentation practices.
Common Pitfalls in Medical Note Writing and How to Avoid Them
Common pitfalls in writing a sample medical note can significantly affect care and provider communication. It's essential to recognize these challenges to enhance the quality of care we provide. Here are key areas to focus on:
- Vague Language: Using non-specific terms can lead to misunderstandings and misinterpretations. Precision in descriptions is crucial; for instance, instead of stating an individual is 'feeling better,' specify the exact improvements observed. This aligns with the understanding that typical biases can arise from operating a small control group that is inadequately powered to identify changes, highlighting the necessity for thorough records.
- Incomplete Information: Omitting relevant details can compromise individual treatment. Thorough documentation should encompass all essential elements, such as medical history, treatment plans, and follow-up instructions, ensuring continuity of care.
- Overly Complex Language: Jargon and overly technical terms can confuse other healthcare providers. Clear and straightforward language enhances communication, ensuring that all team members comprehend the individual's condition and treatment.
- Neglecting to Date and Sign Notes: Failing to include the date and signature can undermine the legal integrity of medical records. Each entry should be properly dated and signed to maintain accountability and traceability.
- Copying and Pasting: While this practice may seem time-efficient, it can lead to inaccuracies and outdated information. Always review and edit any copied content to ensure it reflects the current individual's status and treatment plan.
Being aware of these pitfalls is crucial for medical professionals aiming to improve their record-keeping practices. Continuous education and training in medical note writing are vital for maintaining high standards and improving patient outcomes. For instance, a study on feedback environments in the workplace emphasizes how constructive feedback can greatly affect intrinsic motivation, indicating that a supportive learning atmosphere can improve record-keeping skills among healthcare professionals.
As Yousif AbdulRaheem observes, "These are just some of the common mistakes in ," which can also apply to the record-keeping process. By addressing these common pitfalls, providers can improve the quality of their sample medical notes, ultimately leading to better patient care. CostaNera, being the sole company developing AI solutions for the faith-oriented healthcare sector, is dedicated to enhancing clinical experiences through better record-keeping practices.
Leveraging Technology for Efficient Medical Note Documentation
Technology plays a pivotal role in enhancing the efficiency of sample medical note keeping. It’s essential to recognize the emotional challenges healthcare providers face amidst heavy workloads. Here are several strategies to effectively leverage these advancements:
- Electronic Health Records (EHRs): Implementing EHR systems enables smooth access and sharing of individual information, significantly simplifying the recording process. As of 2016, over 95% of eligible and Critical Access hospitals showcased meaningful use of certified health IT, highlighting the extensive adoption of EHRs in enhancing record-keeping efficiency. This widespread use underscores the critical role EHRs play in improving communication between healthcare providers and individuals.
- Voice Recognition Software: Utilizing dictation tools that convert spoken words into text can save valuable time and minimize typing errors. This technology not only speeds up the record-keeping process but also allows providers to focus more on patient interactions rather than administrative tasks.
- Templates and Macros: Standardized templates for common note types ensure consistency and completeness in records. By employing these tools, healthcare providers can reduce variability in their sample medical notes, thereby enhancing clarity and improving communication among care teams.
- AI-Powered Tools: Exploring AI solutions that assist in creating notes from client interactions can greatly lessen the time invested in record-keeping. These tools analyze patient data and interactions, offering recommendations that align with , thus improving the quality of records.
Despite these benefits, it’s important to acknowledge potential drawbacks. High volumes of clinical alerts can desensitize nurses, contributing to stress and burnout among medical providers. Furthermore, as Adam Gaffney, MD, MPH, observed, "The large majority of US physicians reported that billing-related tasks exacerbate their record-keeping burden," highlighting the challenges that still exist in the recording process.
Adopting these technologies not only results in more precise and effective record-keeping methods but also allows for the creation of a comprehensive sample medical note, thereby reducing the administrative load on medical providers. Staying updated on the newest tools and technologies accessible in medical practice is crucial for enhancing clinical workflows and improving care outcomes. Moreover, a case study showed that 41.5% of adults utilized the Internet to connect with a physician or medical office, suggesting a trend towards enhanced communication enabled by technology, which can improve record-keeping and interactions with individuals seeking care.
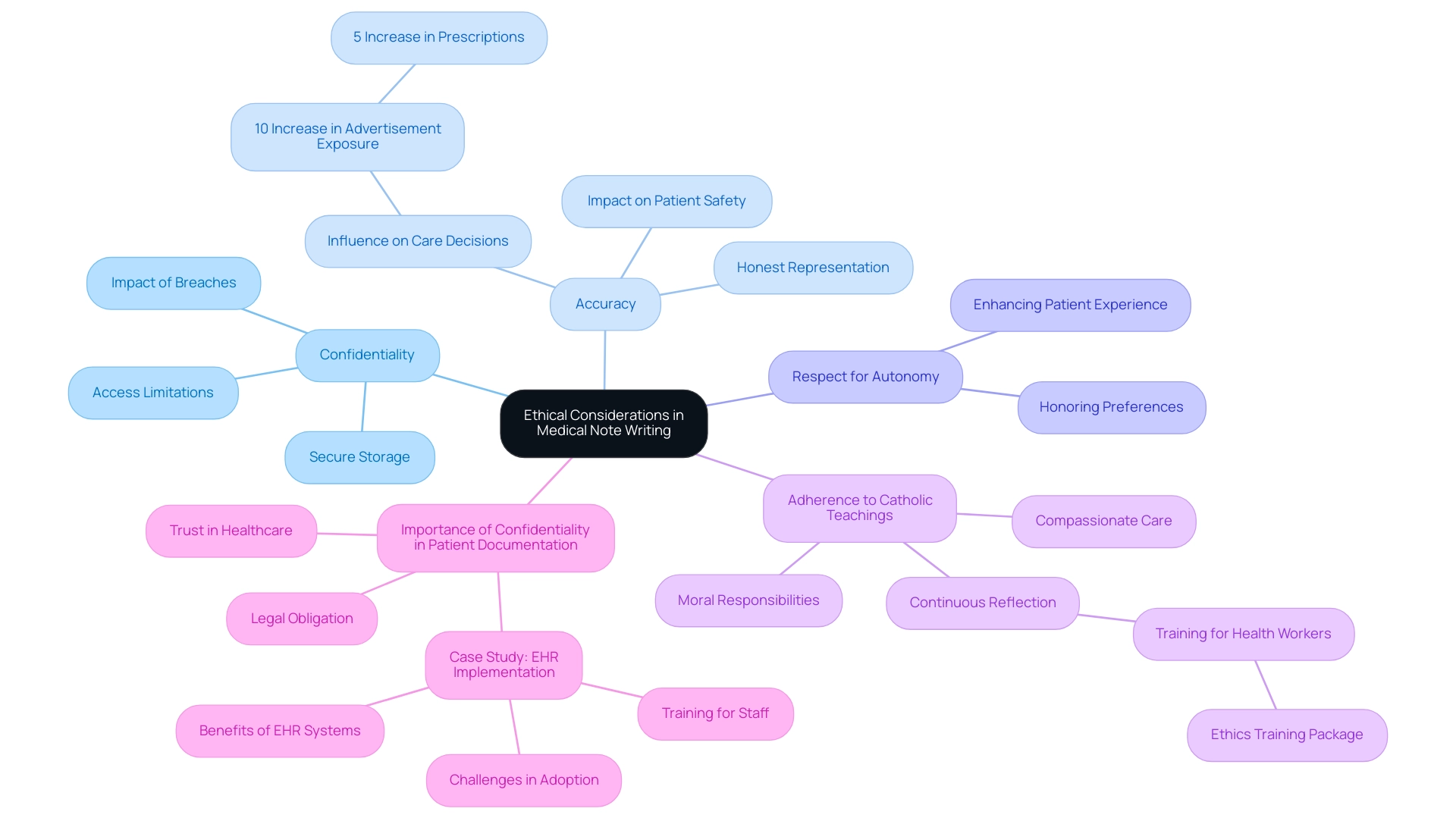
Ethical Considerations in Medical Note Writing: Aligning with Catholic Values
In the realm of healthcare, crafting medical notes is not just a task; it’s a commitment to ethical principles that resonate deeply with the values of Catholic healthcare. As providers, we face emotional challenges daily, striving to deliver compassionate care while managing documentation demands. How can we ensure our notes reflect the trust our patients place in us?
- Confidentiality: Safeguarding individual information is paramount. We must ensure that all notes are stored securely and that access is limited to authorized personnel only. This unwavering commitment to confidentiality fosters trust between individuals and providers, which is essential for .
- Accuracy: Recording information honestly and accurately is vital. It’s our responsibility to represent each individual’s condition and the assistance provided. Faulty records can lead to miscommunication and potentially jeopardize client safety. A study highlighted that for every 10% increase in advertisement exposure, there was a corresponding 5% increase in the number of prescriptions purchased. This statistic underscores the importance of clear and precise documentation in influencing care decisions, directly affecting how we comprehend and respond to individual needs.
- Respect for Autonomy: Documentation should honor individual preferences and values, especially in decision-making processes. This respect for autonomy is crucial in ensuring our patients feel valued and understood, significantly enhancing their overall medical experience.
- Adherence to Catholic Teachings: Aligning our record-keeping practices with the ethical principles of Catholic medical services is essential. This alignment ensures that care is delivered with compassion and respect for life, reinforcing our moral responsibilities as healthcare providers. Continuous reflection on our documentation practices is necessary to uphold these ethical standards, as emphasized by experts in the field. As Masresha Derese Tegegne noted, "Providing a continuing medical ethics training package for health workers before joining the hospital and in between working times could enhance health professionals’ knowledge and attitude towards confidentiality."
- Importance of Confidentiality in Patient Documentation: Maintaining confidentiality is not just a legal obligation; it is a cornerstone of ethical medical practice. Case studies have shown that breaches in confidentiality can severely impact trust, leading to reluctance in sharing vital health information. This trust is crucial for effective diagnosis and treatment. Moreover, the case study titled "The Importance of Training in EHR Implementation" demonstrates how thorough training for medical staff can enhance record-keeping practices and improve patient support, facilitating a smoother transition to digital health records.
By incorporating these ethical considerations into our record-keeping practices, we can enhance the quality of care we deliver while ensuring that each medical note reflects our commitment to Catholic values. Continuous training and reflection on these principles empower us to navigate the complexities of medical documentation effectively, fostering a nurturing environment for both providers and patients.
Conclusion
Medical notes are a vital part of healthcare, profoundly impacting patient care and provider communication. They play a crucial role in ensuring continuity of care, offering legal protection, and integrating advanced technologies like AI solutions. Each type of medical note, from SOAP notes to discharge summaries, has a unique purpose that enhances clarity and collaboration among healthcare teams, ultimately leading to improved patient outcomes.
Effective documentation of medical notes goes beyond mere record-keeping; it embodies ethical principles that prioritize patient confidentiality, accuracy, and respect for autonomy. By adhering to best practices, healthcare providers can sidestep common pitfalls like vague language and incomplete information, thereby elevating the quality of care delivered. The integration of technology, including EHRs and AI tools, further streamlines this process, allowing providers to dedicate more time to patient interaction rather than administrative tasks.
As the healthcare landscape continues to evolve, the importance of thorough and precise medical documentation will only increase. By committing to these practices, healthcare professionals can ensure they are not only meeting clinical and legal standards but also upholding the moral responsibilities inherent in patient care. This dedication to refining documentation processes fosters a more compassionate and effective healthcare environment, ultimately benefiting both providers and patients alike.




