Overview
This article offers a compassionate guide on writing a SOAP note, recognizing its vital role in healthcare documentation for effective patient care. It highlights emotional challenges faced by healthcare providers, acknowledging the stress of administrative burdens that can impact patient interactions. By detailing each component—Subjective, Objective, Assessment, and Plan—and illustrating best practices, it shows how structured documentation can enhance clinical decision-making and communication among providers. Ultimately, this approach leads to improved patient outcomes, reminding us of the profound difference we can make in our patients' lives.
Have you ever felt overwhelmed by the demands of documentation? You’re not alone. Many healthcare professionals share this experience, and it’s crucial to address these challenges. By adopting a structured approach like the SOAP note, we can alleviate some of this burden. It not only streamlines our documentation process but also fosters better communication and collaboration among our teams.
The benefits of effective SOAP notes are significant. They provide clarity in patient care, ensuring that all team members are on the same page. This structured documentation empowers us to make informed decisions, ultimately leading to better patient outcomes. Let’s embrace these practices together, supporting each other in our commitment to exceptional care.
As you move forward, consider how implementing these best practices can transform your approach to patient care. Together, we can create a nurturing environment that prioritizes our patients’ needs, making each interaction meaningful and impactful.
Introduction
In the realm of healthcare, effective communication and precise documentation are essential for ensuring high-quality patient care. Have you ever felt overwhelmed by the sheer volume of information that needs to be captured? SOAP notes—an acronym for Subjective, Objective, Assessment, and Plan—provide a vital framework for healthcare providers. They enable you to systematically capture and convey critical patient information, helping to alleviate some of that burden.
Each component of SOAP notes plays a unique role, from understanding the patient's personal experiences to outlining actionable treatment plans. This structured approach not only enhances clarity but also fosters a deeper connection with your patients. As the healthcare landscape evolves, particularly with the integration of technology and artificial intelligence, the significance of SOAP notes becomes increasingly pronounced.
This article delves into the intricacies of SOAP notes, exploring their structure, common pitfalls, and the transformative impact they have on patient care and clinical communication. Let’s embark on this journey together, understanding how these notes can empower you to provide the compassionate care your patients deserve.
Understanding SOAP Notes: Definition and Purpose
SOAP notes represent a vital documentation method that healthcare providers must master for accurately recording encounters. The acronym stands for Subjective, Objective, Assessment, and Plan, with each component playing a crucial role in delivering effective care.
- Subjective: This section captures the individual's personal experiences, symptoms, and feelings regarding their health. It offers invaluable insights into their condition, allowing for a more tailored approach.
- Objective: Here, healthcare providers document measurable data, such as vital signs and physical examination findings. This information is critical for clinical assessments, enhancing the understanding of each patient's situation.
- Assessment: This part involves the clinician's interpretation of both subjective and objective data, leading to a diagnosis or clinical impression that informs treatment decisions.
- Plan: Finally, the plan outlines the next steps in care, including treatments, referrals, and follow-up appointments. This structured approach ensures ongoing care is both effective and compassionate.
The significance of documentation in healthcare cannot be overstated. It enhances clinical efficiency by organizing information for easy retrieval, which is vital for fostering clear communication among healthcare providers. As we look towards 2025, the incorporation of technology—such as and potential automation through artificial intelligence—promises to transform documentation practices, ultimately improving care outcomes.
Have you ever wondered how structured records can impact your daily practice? Recent research indicates that healthcare professionals utilizing structured records experience substantial benefits, including improved record accuracy and enhanced care quality. For example, a case study titled 'The Future of SOAP Notes in Healthcare' illustrates how the evolution of healthcare delivery relies on the continued relevance of SOAP notes for dependable care. The integration of AI technology, like that offered by CosmaNeura, can further enhance communication and care by streamlining documentation processes and leveraging predictive analytics to identify individuals at higher risk of developing certain conditions.
By analyzing individual data and patterns, AI algorithms can provide early warnings, enabling preventive measures that lead to better outcomes and reduced healthcare costs. Isn’t it reassuring to know that technology can support your efforts?
Professional insights reinforce the importance of documentation. Dr. Lawrence Weed, a pioneer in medical record-keeping, emphasizes that "the application of structured formats simplifies healthcare workflows, improves care quality, and aids in effective practice administration." By adopting uniform record-keeping methods, healthcare providers can anticipate significant improvements in care results, leading to and greater satisfaction among individuals.
Moreover, healthcare providers using CosmaNeura can expect specific advantages such as time efficiency, revenue growth through AI-driven billing suggestions, and adherence to Catholic values in healthcare. These benefits create a strong connection between effective documentation and the advantages of the platform, particularly in improving patient outcomes through predictive analytics. CosmaNeura's functionalities, including automated record-keeping and smooth integration with electronic health records, further assist healthcare providers in maintaining precise and effective clinical records.
In summary, understanding the elements of documentation is essential for healthcare providers striving to deliver high-quality care. By following current best practices on how to write a SOAP note, providers can ensure that their records not only meet regulatory standards but also enhance the overall effectiveness of care in 2025 and beyond.
The Structure of SOAP Notes: Breaking Down Each Component
serves as a vital framework in clinical documentation, comprising four distinct components that facilitate effective communication and patient care:
- Subjective: This section captures the individual's own words regarding their symptoms, concerns, and medical history. It is essential to reflect the individual's perspective accurately, which may include direct quotes to enhance the authenticity of the documentation. By prioritizing the individual's voice, healthcare providers can better understand their experiences and needs.
- Objective: Here, healthcare providers document observable and measurable data, such as results from physical examinations, laboratory tests, and vital signs. This information must be factual and devoid of personal interpretation, ensuring that it serves as a reliable basis for clinical decision-making. complements the subjective insights, providing a comprehensive view of the individual's condition.
- Assessment: In this component, clinicians synthesize the subjective and objective data to formulate a clinical assessment. This may involve establishing a diagnosis or presenting differential diagnoses, showcasing the clinician's analytical reasoning. A well-articulated assessment is crucial for guiding treatment decisions and ensuring continuity of care.
- Plan: The final section outlines the proposed management plan, detailing treatments, medications, referrals, and follow-up instructions. It is crucial that this section is clear and actionable, providing a roadmap for the next steps in care. A well-structured plan not only enhances patient outcomes but also fosters accountability among healthcare providers.
Integrating best methods into structured writing is crucial for attaining efficient records. For instance, maintaining a formal tone and objective observations is critical. A case study on effective structured summaries in rehabilitation therapy highlights the significance of concise and clear records, emphasizing common mistakes to avoid and best practices to adopt.
By adhering to these guidelines on how to write a SOAP note, therapists can significantly improve the quality of their documentation, ultimately leading to better patient outcomes.
Moreover, statistics suggest that efficient documentation can improve billing precision and reveal previous billing possibilities, aiding significant financial advancement for healthcare facilities. As Kunal Sindhu, MD, suggests, 'Try to view clinical documentation as learning opportunities, and with sufficient effort and time, you’ll become skilled in composing these essential medical communications.' With commitment and practice, healthcare providers can excel in the craft of documentation writing, ensuring that their records not only meet clinical and legal standards but also improve the overall quality of care.
Step-by-Step Guide to Writing SOAP Notes
Writing can feel overwhelming at times, but following these structured steps can ease that burden:
- Gather Information: Begin by collecting comprehensive individual information, including medical history, current symptoms, and any previous notes. This foundational step is crucial for accurate documentation and sets the stage for understanding the patient's journey.
- Write the Subjective Section: Capture the individual's account of their symptoms, including relevant quotes that reflect their concerns and feelings. This section should accurately represent their perspective, as it is vital for understanding their experience. As Tague noted, "I’ve seen records that are literally two sentences per section and they’re great, and then there are records with four or five sentences for each and they still haven’t covered what they needed to cover," illustrating the variability in documentation.
- Document the Objective Data: Record measurable data such as vital signs, lab results, and findings from physical examinations. Precision is key in this section; ensure that all information is factual and clearly presented to support your assessment.
- Formulate the Assessment: Analyze the subjective and objective data to arrive at a clinical assessment. Clearly articulate your diagnosis or differential diagnoses, providing a rationale based on the gathered information to foster understanding.
- Outline the Plan: Detail the management plan, including treatments, referrals, and follow-up instructions. The plan should be clear and actionable, ensuring that both the individual and other healthcare providers can easily understand the next steps.
- Review and Revise: After drafting the SOAP note, take the time to review it for clarity, completeness, and accuracy. Modify as needed to guarantee it conforms to record standards, enhancing the quality of evaluations and treatment strategies.
Incorporating these steps not only streamlines the process of writing a SOAP note but also enhances the overall quality of care provided to patients. A study has indicated that employing a systematic method improves task success and usability for healthcare professionals, making it a vital tool in clinical practice. Furthermore, studies show that the APSO arrangement is more efficient than the conventional structure regarding speed and usability, reinforcing the advantages of a structured method.
Additionally, selecting a medical transcription service with high accuracy rates (99% or better) is essential to prevent legal issues and guarantee safety for individuals. By following best practices and consistently enhancing documentation skills, healthcare providers can ensure that their records are both effective and compliant with current standards. The structured documentation framework, developed almost 50 years ago, remains an essential approach for organizing client information and improving communication among healthcare professionals.
Common Mistakes to Avoid in SOAP Note Writing
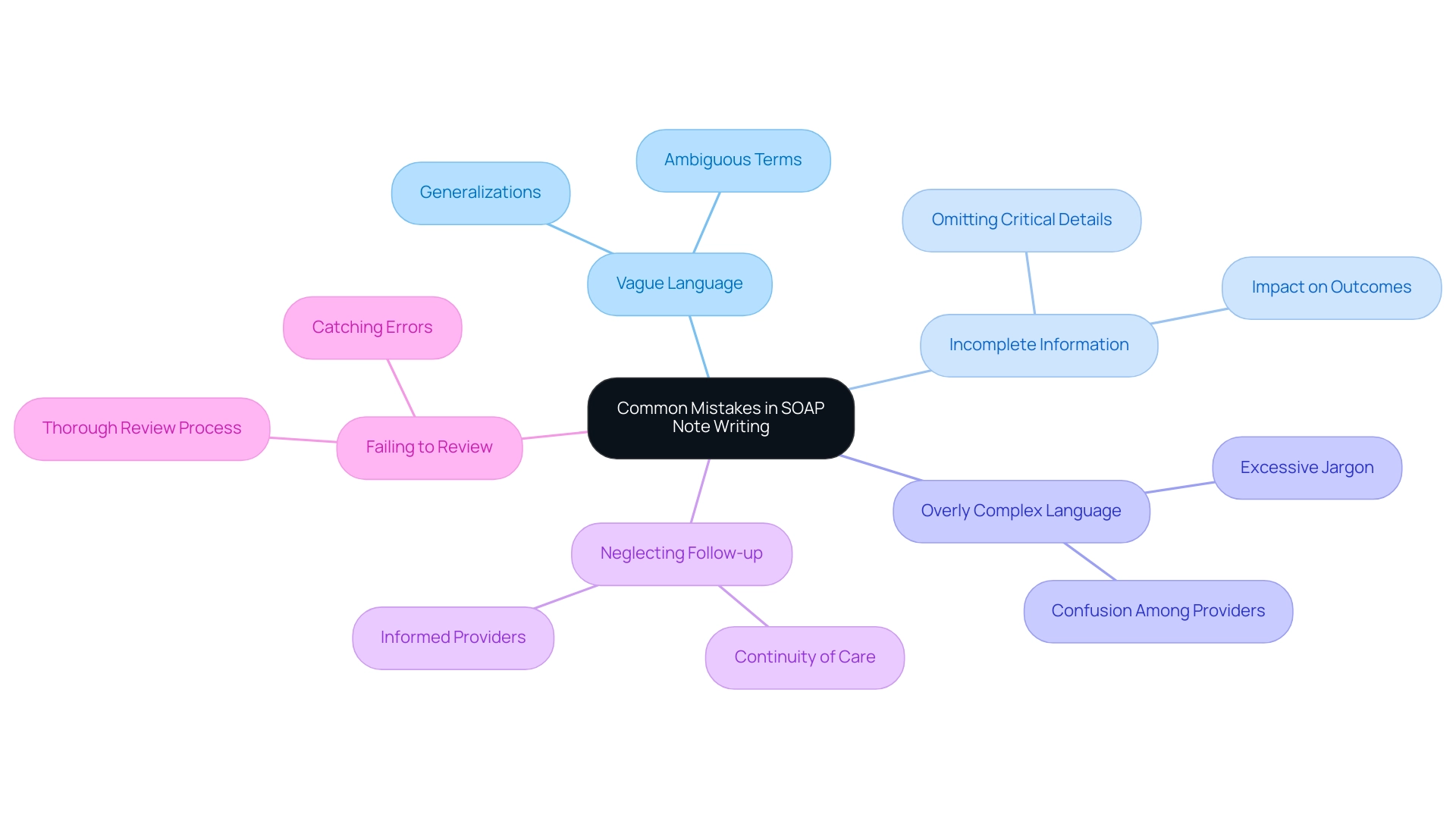
To ensure high-quality SOAP notes, it's essential to be aware of common pitfalls that can affect your documentation:
- Vague Language: It's important to avoid ambiguous terms or generalizations. Specificity in descriptions is key for conveying clear and actionable information. When you understand how to write a SOAP note, remember that vague language can lead to misunderstandings that compromise care.
- Incomplete Information: Each section of the SOAP record must include all relevant data to effectively demonstrate how to write a SOAP note. Omitting critical details can lead to miscommunication, which may negatively impact outcomes for individuals. Did you know that studies show individuals who read four or more messages reported a relative risk (RR) of 3.09 for detecting serious errors? This highlights the significance of detailed records.
- Overly Complex Language: It's vital to utilize clear and concise language that all healthcare providers can easily understand. Excessive jargon can confuse readers and detract from the note's effectiveness. The goal is to ensure that all team members can quickly grasp how to write a SOAP note regarding the individual's condition and care plan.
- Neglecting Follow-up: Understanding how to write a SOAP note that includes follow-up instructions in the plan section is crucial. This practice ensures continuity of care and keeps all providers informed about the next steps, which is vital for effective management of those receiving care.
- Failing to Review: Conducting a thorough review for accuracy and completeness before concluding your documentation is critical. This step can catch any errors or omissions that could negatively affect care. Case studies have shown that organized record-keeping techniques, such as the SOAP note framework created by Larry Weed nearly 50 years ago, enhance communication among healthcare professionals and improve the quality of care for individuals.
Furthermore, many individuals have expressed frustration and emotional distress over perceived mistakes in their medical records. This highlights the real-world consequences of inadequate record-keeping practices. As Ditto aptly noted, "If you need a faster TAT, we do offer STAT files (4-hour turnaround) at 16 cents a line," emphasizing the importance of .
By addressing these frequent errors, healthcare professionals can significantly enhance the quality of their documentation. This commitment ultimately leads to improved outcomes for individuals and better clinical decision-making. How can you implement these strategies in your practice today?
The Role of SOAP Notes in Improving Patient Care and Communication
Documentation tools play a vital role in enhancing care and communication, addressing the emotional challenges healthcare providers face daily. By ensuring comprehensive and well-documented records, these tools significantly improve continuity of care. When all healthcare providers involved in a person's treatment have access to accurate and detailed information, decision-making becomes more effective, ultimately leading to better management of individuals.
- Enhancing Continuity of Care: Imagine the peace of mind that comes from knowing every clinician has the information they need to provide the best care. Structured documentation allows for systematic data analysis, resulting in informed evaluations and tailored treatment plans. For instance, a medication entry like
Motrin 600 mg orally every 4 to 6 hours for 5 daysexemplifies how precise record-keeping guides clinical choices, ensuring individuals receive care that meets their unique needs. - Enhancing Individual Engagement: Clinical records that capture individual concerns and preferences foster deeper connections between individuals and caregivers. This personalized approach not only addresses specific needs more effectively but also enhances overall satisfaction with treatment.
- Facilitating Legal Safeguarding: Accurate clinical records serve as essential legal evidence of interactions, protecting both suppliers and patients in case of disputes. They provide a clear account of the care given and the decisions made, offering reassurance in challenging situations.
- Streamlining Communication: These records establish a standardized method for documenting information, improving interactions among healthcare providers. This standardization minimizes misunderstandings and errors that may arise from inconsistent practices. Advanced transcription technologies, such as those from Augnito, further enhance the accuracy of clinical documentation without demanding infrastructure changes. As Imran Shaikh emphasizes, ensuring the correctness of patient details in documentation is crucial to prevent significant time loss and adverse health outcomes.
In summary, the effective use of structured records not only bolsters clinical decision-making but also strengthens communication among healthcare providers, ultimately leading to . As the healthcare landscape evolves, the role of documentation in fostering high-quality, patient-centered care is more critical than ever. The increasing volume of data in electronic medical records underscores the need for clinically relevant records, making the ability to write a soap note essential.
The case study titled [SOAP Note Structure and Function](https://blog.cosmaneura.com/10-essential-soap-notes-templates-for-healthcare-providers) serves as a guide for writing effective soap notes, facilitating comprehensive patient documentation and reinforcing its significance in clinical practice.
Conclusion
The significance of SOAP notes in healthcare truly resonates with the challenges faced by providers. By offering a structured framework for documenting patient encounters, SOAP notes not only enhance communication among healthcare professionals but also contribute to better patient care outcomes. Each component—Subjective, Objective, Assessment, and Plan—serves a vital purpose in capturing relevant information, fostering a comprehensive understanding of the patient's condition.
Effective SOAP notes streamline documentation processes and support clinical decision-making while enhancing patient engagement and ensuring continuity of care. By steering clear of common pitfalls, such as vague language or incomplete information, healthcare providers can maximize the effectiveness of their documentation. Furthermore, the integration of advanced technologies, including AI and digital health records, promises to elevate the role of SOAP notes in clinical practice, making them even more indispensable in modern healthcare settings.
Ultimately, crafting precise and thorough SOAP notes is essential for healthcare professionals dedicated to delivering high-quality, compassionate care. As the healthcare landscape continues to evolve, mastering the art of SOAP note writing will remain a vital skill, ensuring that patient needs are met with clarity and efficiency. Embracing this standardized documentation method is not merely about compliance; it empowers providers to offer the best possible care to their patients.




