Overview
In the demanding world of healthcare, clinical learning and effective documentation play a crucial role in direct patient care. Have you ever felt overwhelmed by the sheer volume of paperwork? Accurate records are not just a formality; they are essential for clinical decision-making, continuity of care, and meeting legal standards.
Imagine a scenario where integrating AI tools alleviates these administrative burdens. This shift allows healthcare providers to focus more on what truly matters—patient interactions. By improving the quality of care, we can address the inefficiencies that often arise from current documentation practices.
The benefits of such integration are profound. When healthcare professionals can dedicate more time to their patients, it fosters a deeper connection and enhances the overall patient experience. Let’s embrace these innovative solutions together, ensuring that we prioritize compassionate care in our practices.
As we navigate these challenges, it’s vital to remember that support is available. By exploring AI tools, we can transform our approach to documentation, ultimately leading to a more fulfilling practice for both providers and patients alike.
Introduction
In the rapidly evolving landscape of healthcare, the significance of clinical documentation is profound. It serves as a cornerstone for effective patient care, facilitating communication among providers, ensuring compliance with regulations, and supporting billing processes. Yet, as the demands on healthcare professionals grow, many face an emotional challenge: the balance between thorough documentation and direct patient interaction is often skewed.
With advanced technologies like AI emerging, there is hope for alleviating the administrative burdens that contribute to clinician burnout. Imagine a world where documentation is streamlined, allowing more time for meaningful patient interactions. This article delves into the multifaceted purposes of clinical documentation, explores strategies for achieving a healthier balance, and outlines best practices that can enhance the quality and efficiency of documentation in modern healthcare settings.
As the industry moves forward, understanding and adapting to these changes will be crucial for delivering high-quality patient care. Together, we can navigate these challenges and foster an environment that prioritizes both documentation and patient connection.
Understand the Evolving Purposes of Clinical Documentation
Understand the Evolving Purposes of Clinical Documentation
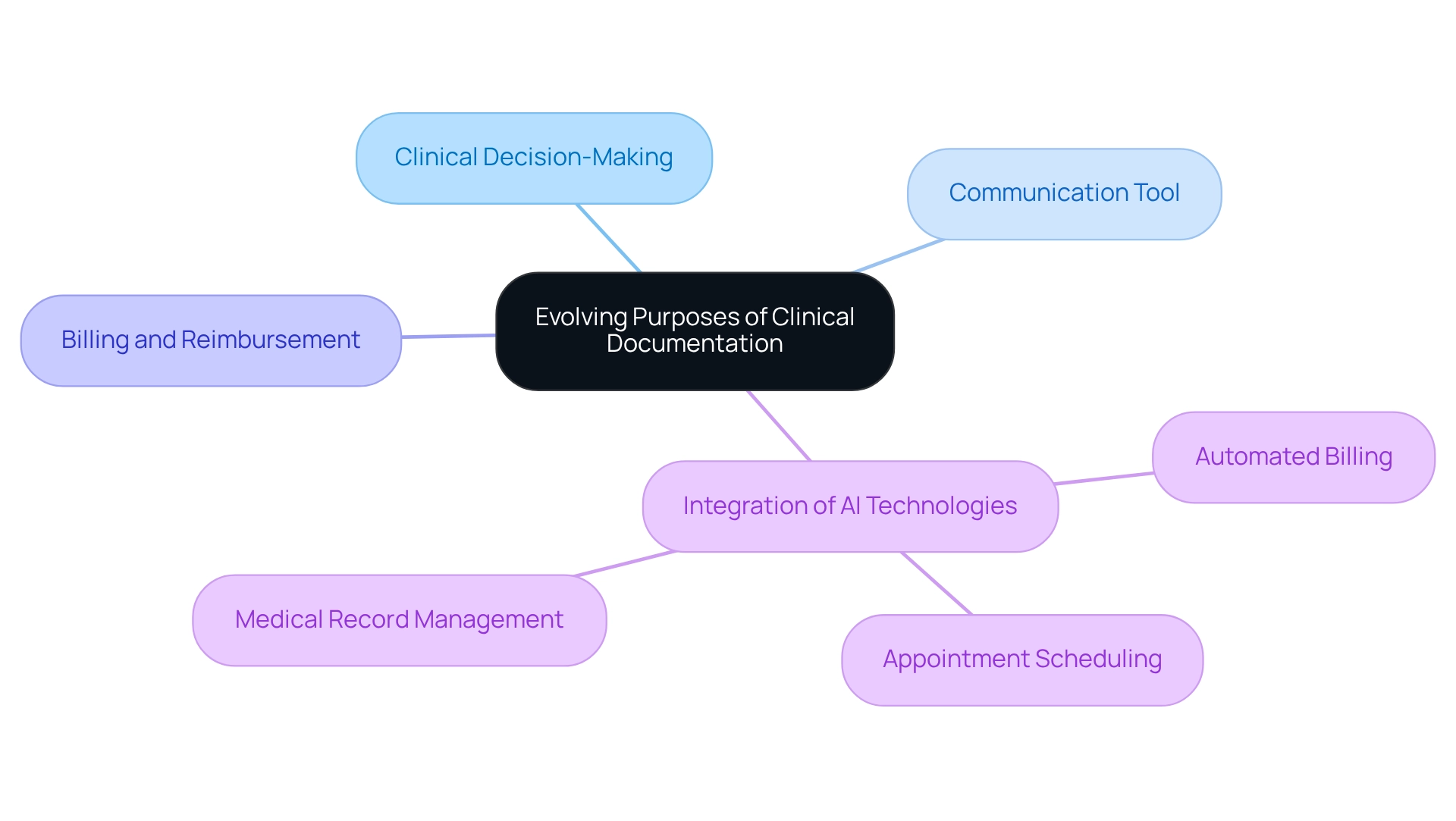
Clinical documentation is not just a requirement; it plays a vital role in supporting clinical decision-making, ensuring continuity of care, and meeting legal obligations. It acts as a crucial communication tool among healthcare providers, fostering a shared understanding of patients' histories and treatment plans. Accurate records are essential for billing and reimbursement processes, as they validate the services provided. However, recent trends reveal that the current Evaluation and Management (E&M) guidelines may be creating an imbalance, prioritizing compliance and coding over the crucial aspect of patient care, which can impede effective clinical practice.
As the medical landscape evolves, integrating technology into record-keeping practices becomes increasingly important. AI-powered tools, such as , have demonstrated significant potential in streamlining record-keeping processes and alleviating the administrative burdens that contribute to physician burnout. By automating time-consuming tasks like appointment scheduling and medical record management, these solutions allow healthcare providers to reclaim valuable time to focus on delivering high-quality care. A recent assessment titled 'Evaluating the Effectiveness of AI Scribes' revealed that users experienced a notable reduction in record-keeping time, leading to enhanced engagement and satisfaction. This underscores the necessity for ongoing monitoring and evaluation of such technologies, as illustrated in TPMG's plans to ensure they uphold quality and safety standards in clinical records.
Key Features of AI Solutions for Administrative Efficiency:
- Automated Billing: Streamlines the billing process, reducing errors and improving revenue cycle management.
- Appointment Scheduling: Simplifies scheduling, minimizing no-shows and optimizing provider time.
- Medical Record Management: Enhances the organization and retrieval of client records, ensuring quick access to critical information.
The importance of clinical learning and direct patient care documentation transcends mere administrative efficiency; it is fundamental for informed decision-making and continuity of service. Healthcare leaders emphasize that effective clinical learning and direct patient care documentation are crucial for delivering high-quality treatment, enabling providers to make informed choices based on comprehensive client information. As we move deeper into 2025, the impact of AI on clinical record practices will continue to reshape how medical professionals interact with patients, allowing them to devote more time to direct individual support while maintaining the integrity and accuracy of medical records. As Sir William Osler wisely stated, 'record, tabulate, communicate,' highlighting the essential role of record-keeping in medical care.
Balance Documentation with Direct Patient Care Activities
Finding a balance between clinical learning, direct patient care, documentation, and direct client care is vital for enhancing service delivery in the medical field. Many providers express concern, noting they spend an average of 1.77 hours each day on paperwork outside of office hours. This burden is exacerbated by billing-related tasks and clinical learning documentation, which detracts from valuable patient interactions and contributes to feelings of burnout. How can we alleviate this strain? Healthcare organizations can adopt several effective strategies.
- Utilize Electronic Health Records (EHRs) Efficiently: Ensure that EHR systems are optimized for ease of use, allowing for quick data entry and retrieval.
- Employ Standardized Templates: Use templates for common record-keeping tasks to streamline the process and reduce variability.
- Train Staff: Provide training to staff on best practices for record-keeping to enhance efficiency.
- Schedule Specific Time for Records: Reserve particular periods for record-keeping following client interactions, enabling clinicians to concentrate entirely on service during appointments.
- Integrate AI Tools: Utilize AI to automate routine record-keeping tasks, significantly decreasing the administrative load by managing intake, administration, and triage autonomously.
These strategies not only empower providers to prioritize client involvement but also enhance the quality of service through clinical learning documentation. As Wong et al. highlight, numerous studies have examined the time devoted to clinical learning and client support. They suggest that time recovered from documentation, when redirected to client support, can significantly enhance service. By aligning record-keeping practices with the needs of medical providers, organizations can foster a more effective and empathetic medical environment.
Furthermore, the ongoing discussion about the influence of electronic documentation on patient treatment duration underscores the necessity for continual assessment and adjustment of documentation methods. The unique capabilities of AI-driven solutions can further streamline these processes, allowing medical professionals to focus on delivering high-quality, patient-centric care. Addressing challenges like medical fragmentation and regulatory concerns through these innovative strategies will be crucial for enhancing . Together, let’s create a supportive environment where healthcare providers can thrive and focus on what truly matters—their patients.
Implement Best Practices for Effective Clinical Documentation
To enhance , healthcare providers face the challenge of maintaining clear and concise records. These records are essential for capturing all relevant patient information and clinical decisions. It’s concerning that 15% of medical charts reviewed contain mistakes, particularly among less experienced personnel. This highlights the need for organized training methods to improve record quality and support staff in their vital roles.
Regular evaluations of clinical learning direct patient care documentation can pinpoint areas for improvement, reinforcing adherence to best practices. Utilizing structured templates and checklists simplifies the documentation process, ensuring that all essential information is captured effectively. For example, implementing a uniform format can significantly reduce variability and enhance the clarity of records, ultimately leading to better outcomes for patients.
CosmaNeura's commitment to improving record quality is exemplified in the case study 'Setting the Benchmark in Catholic Healthcare.' This study illustrates how the company's AI solutions are designed to enhance clinical record practices and patient care.
Moreover, the Clinical Documentation Improvement Market is projected to see the solutions segment represent a market share of 7.6% in 2024, underscoring the increasing importance of efficient record-keeping solutions in medicine.
To effectively implement these best practices, healthcare providers can take the following steps:
- Hold regular training sessions for staff on record-keeping standards.
- Utilize structured templates and checklists for consistency.
- Conduct regular audits to detect and resolve record errors.
- Encourage a culture of responsibility and ongoing enhancement in record-keeping practices.
Common pitfalls to avoid include neglecting to update practices in line with new regulations and failing to provide adequate training for all staff levels. By prioritizing these practices, healthcare providers can foster a culture of excellence in clinical learning direct patient care documentation, which is essential for delivering high-quality patient care.
Conclusion
The evolving landscape of clinical documentation is pivotal for enhancing patient care and ensuring compliance within the healthcare system. Have you ever felt overwhelmed by the demands of documentation? By understanding its multifaceted purposes—supporting clinical decision-making and facilitating billing processes—healthcare providers can appreciate the critical role that accurate documentation plays in delivering high-quality care. The integration of AI technologies offers promising solutions to streamline documentation practices, helping to alleviate the administrative burdens that contribute to clinician burnout. This allows providers to focus more on meaningful patient interactions.
Striking a balance between documentation and direct patient care is essential. Implementing strategies such as:
- Efficient use of Electronic Health Records
- Standardized templates
- Dedicated documentation time
can significantly improve the quality of care while reducing the time spent on administrative tasks. These efforts not only enhance provider efficiency but also lead to better patient engagement and satisfaction.
Moreover, adopting best practices for effective clinical documentation, including regular training and periodic audits, is crucial for maintaining high standards. By fostering a culture of accountability and continuous improvement, healthcare organizations can ensure that documentation practices evolve alongside the changing demands of the industry. Ultimately, prioritizing both thorough documentation and meaningful patient connections will be key to navigating the future of healthcare. This approach ensures that providers can deliver the best possible care while managing the complexities of clinical documentation.




