Overview
The clinical documentation of a patient visit begins with capturing essential information, such as medical history, treatment strategies, and examination findings. This process is vital for ensuring continuity of care and fostering effective communication among the healthcare team. Have you ever considered how overwhelming it can be to manage these details amidst daily pressures?
Triggers for documentation often arise during:
- Initial encounters
- Changes in conditions
- The introduction of new treatments
Each of these moments underscores the critical need for precise record-keeping. Such diligence not only enhances patient safety but also ensures compliance and promotes better health outcomes for everyone involved.
By recognizing the emotional and administrative burdens that healthcare providers face, we can better appreciate the significance of thorough documentation. It’s not just about keeping records; it’s about safeguarding the well-being of our patients and supporting each other in this demanding field. Let’s continue to prioritize effective communication and compassionate care in our practices.
Introduction
In the intricate web of clinical documentation, we find the cornerstone of effective healthcare. This foundation ensures that vital patient information is recorded and communicated with care among providers. Yet, many healthcare professionals face emotional challenges when it comes to maintaining this crucial documentation. How do administrative burdens affect the quality of patient interactions?
As we explore the essential triggers that initiate clinical documentation during patient visits, we uncover the profound impact that accurate records have on patient care and administrative efficiency. It's not just about paperwork; it's about enhancing the patient experience and ensuring that every detail is captured with compassion.
As healthcare evolves, practitioners are left wondering: how can we overcome the challenges of comprehensive documentation while fostering meaningful patient connections? By addressing these concerns, we can highlight the significance of robust record-keeping practices and the innovative solutions that can transform the documentation landscape for the better.
Together, let’s embrace these changes and strive for a future where documentation supports, rather than hinders, our ability to provide exceptional care.
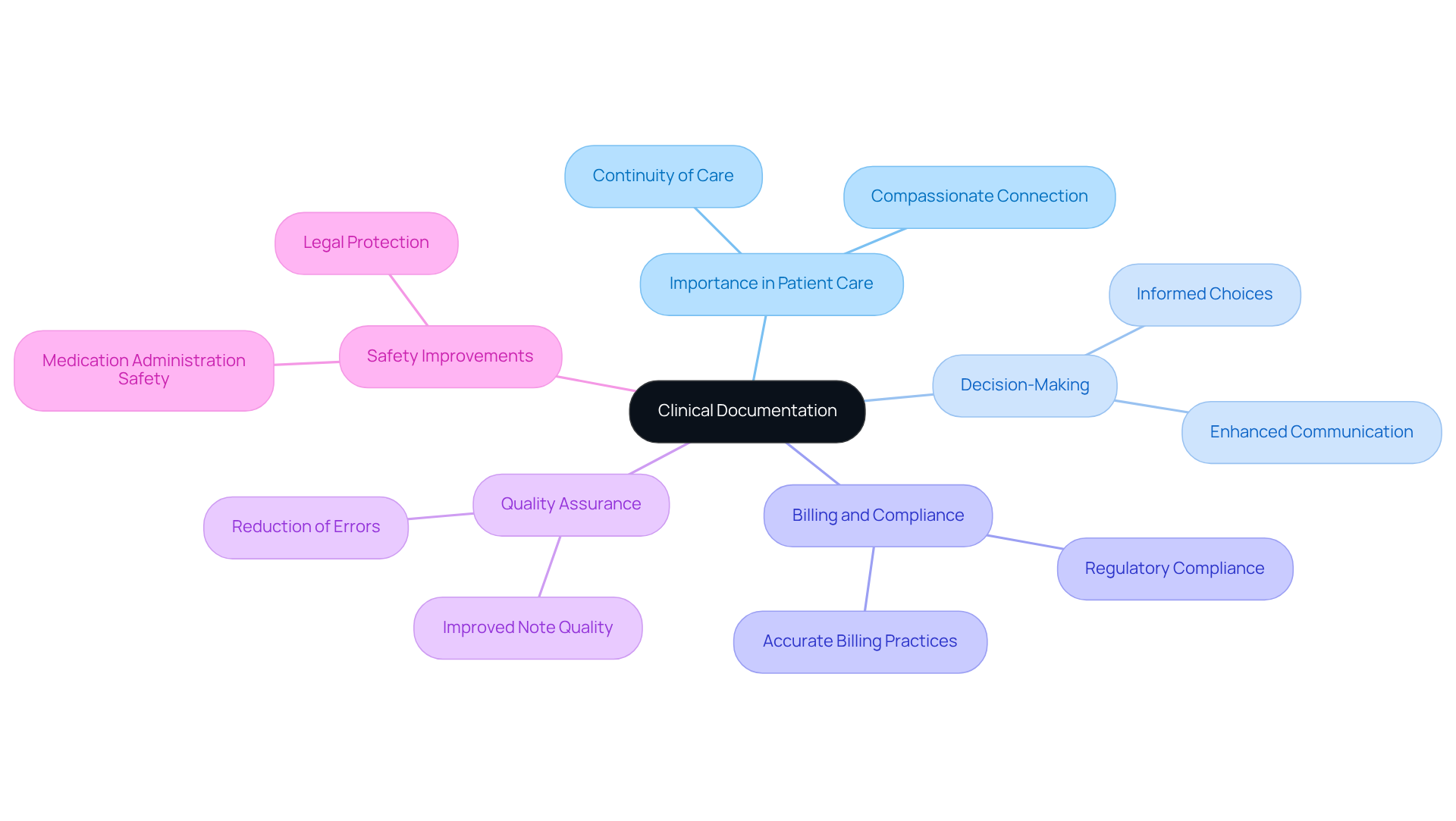
Define Clinical Documentation and Its Importance
Medical records are more than just data; they represent a compassionate connection between individuals and their healthcare providers. Capturing essential information—like medical history, treatment strategies, and examination findings—is what starts the clinical documentation of a patient visit and is crucial for ensuring continuity of care and fostering effective communication among the care team. Have you ever considered how vital these records are for the overall well-being of patients? They not only support decision-making in healthcare but also play a key role in billing, compliance, and quality assurance.
Precise medical records are essential for improving health outcomes. They provide a clear and detailed overview of what starts the clinical documentation of a patient visit, which includes an individual's health status and the care received. For instance, research has shown that well-organized medical records can reduce the frequency of medication administration errors, enhancing safety for those in our care. Additionally, a multicenter study revealed that implementing organized record-keeping practices resulted in a remarkable 20% improvement in note quality. This illustrates the tangible benefits of diligent record maintenance.
Experts often compare efficient medical records to insurance; they must be established proactively to safeguard both patients and providers from potential legal issues. As we navigate the evolving landscape of healthcare, the integration of automated clinical coding (CAC) has shown promise in improving coding accuracy and quality. This reinforces the necessity for robust record-keeping practices in clinical settings.
In light of these insights, how can we ensure that our medical records reflect the care and attention our patients deserve? Let’s engage in a conversation about how we can enhance our record-keeping practices for the benefit of everyone involved.
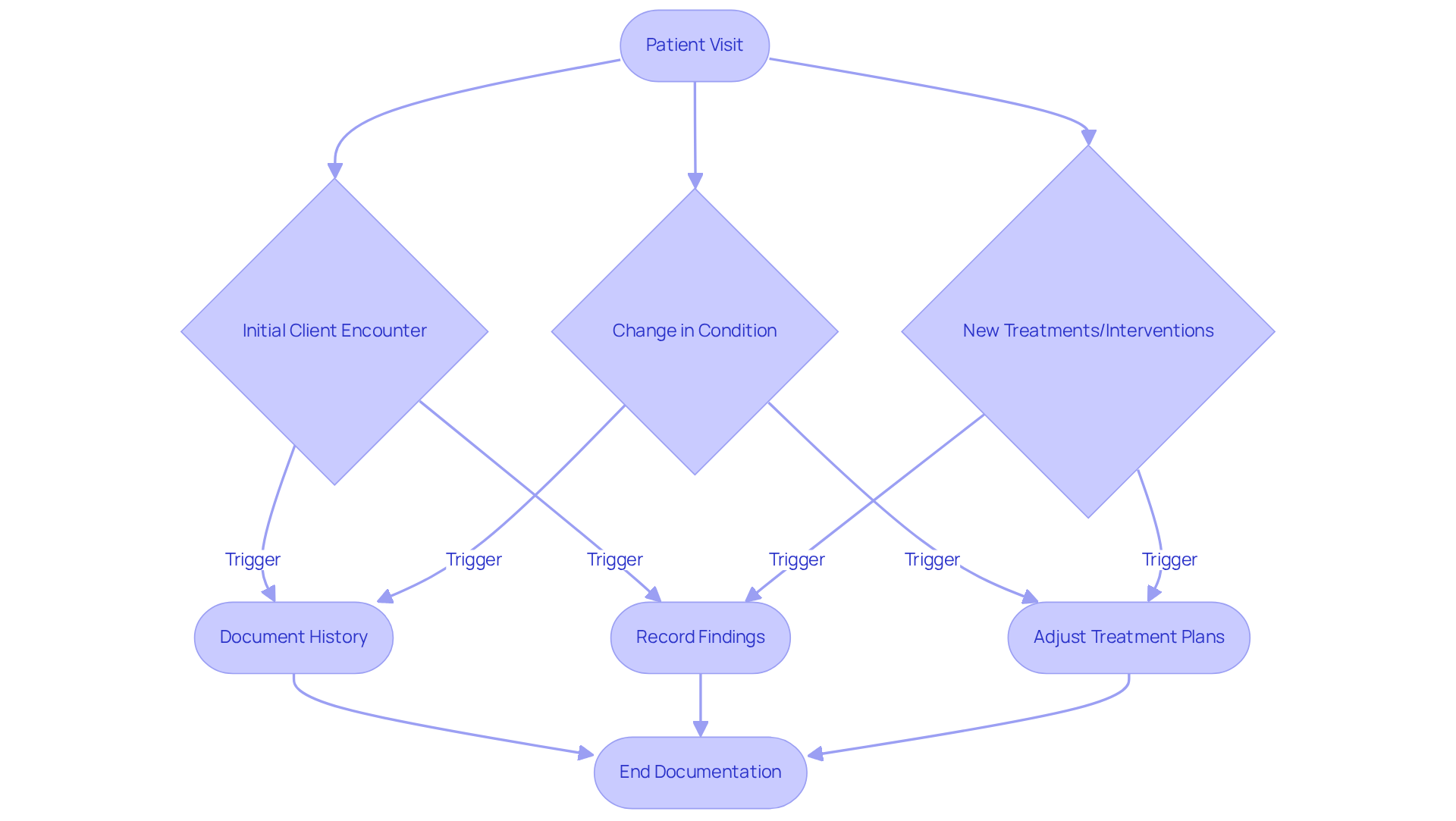
Identify Triggers for Clinical Documentation in Patient Visits
Several key triggers determine what starts the clinical documentation of a patient visit, including the initial client encounter, changes in the individual's condition, and the introduction of new treatments or interventions. Have you ever felt overwhelmed by the need to document every detail? For instance, when an individual presents with a new complaint, the clinician must carefully document the history of the present illness, relevant medical history, and findings from the physical examination. Follow-up visits that include changes to treatment plans or medication adjustments also necessitate thorough records. These triggers are essential for capturing all pertinent information, which is crucial for understanding what starts the clinical documentation of a patient visit and for ensuring effective ongoing patient care while adhering to legal standards.
Moreover, precise record-keeping plays a significant role in ensuring appropriate reimbursement. It reflects the services rendered and supports compliance with government regulations. As Dr. David Schillinger wisely states, "Medical reimbursement is indicative of what you record, not just what you do," emphasizing the vital role of record-keeping in the financial aspects of medical services. Did you know that 95% of ensuring suitable reimbursement depends on effective record-keeping practices? This highlights the need for comprehensive and accurate clinical records.
By utilizing generative AI, medical practitioners can automate documentation duties, such as recording individual histories and revising treatment plans. This not only alleviates administrative burdens but also allows for more meaningful interactions with individuals, ultimately improving the quality of care provided. Furthermore, tackling the challenges presented by disjointed medical systems, generative AI can enhance communication and coordination among providers. This ensures that all pertinent individual information is precisely recorded and readily accessible.
In summary, embracing these innovative solutions can significantly ease the emotional and administrative challenges faced by healthcare providers. Let’s work together to create a more efficient and compassionate healthcare experience for everyone involved.
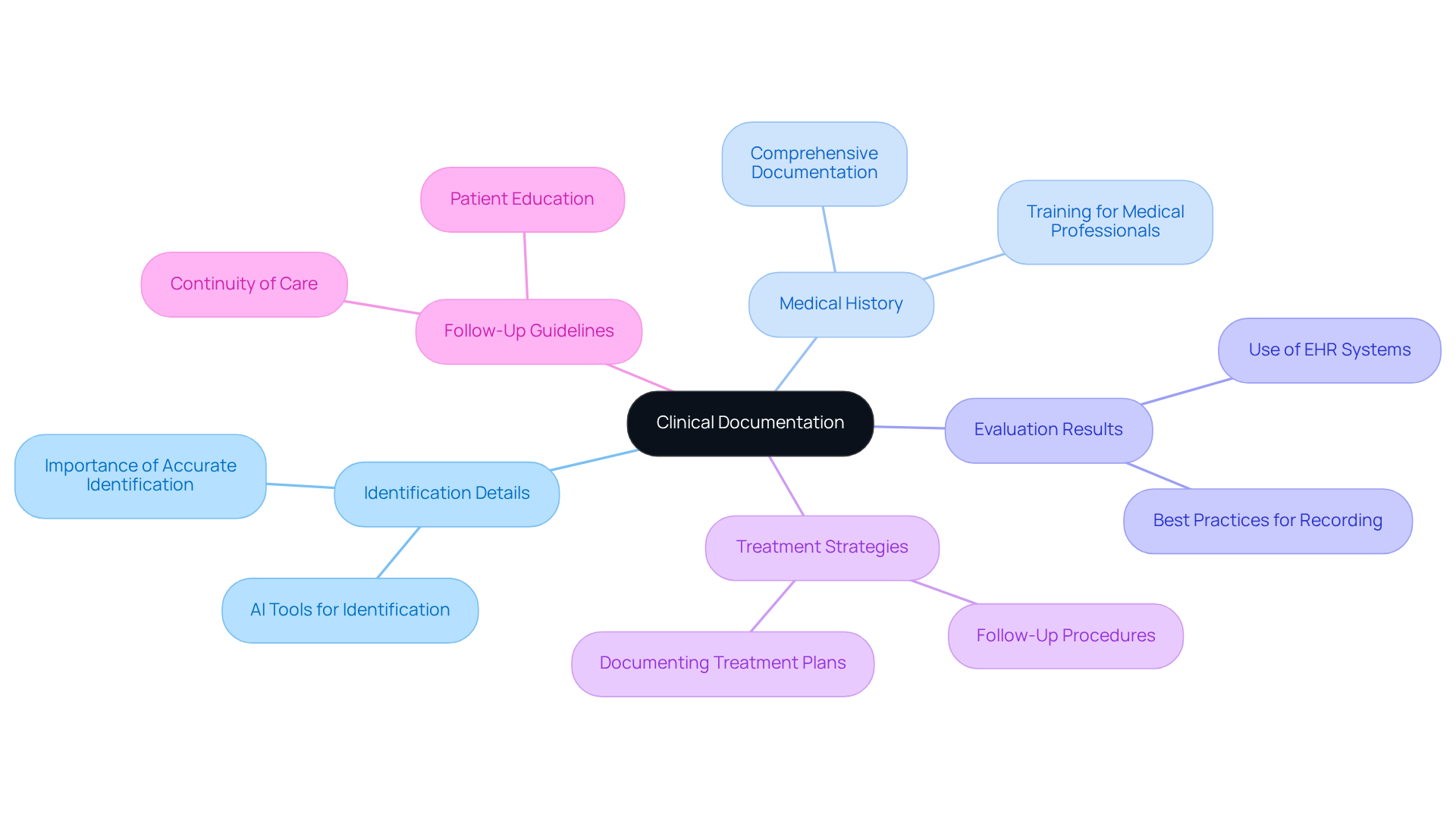
Outline Key Components of Clinical Documentation
What starts the clinical documentation of a patient visit includes key elements of medical records such as vital individual identification details, comprehensive medical history, evaluation results, treatment strategies, and follow-up guidelines. To ensure seamless understanding among healthcare providers, each entry must be clear, concise, and legible, as this is what starts the clinical documentation of a patient visit. Importantly, what starts the clinical documentation of a patient visit should elucidate the reasoning behind medical decisions, outline any education offered to the individual, and document the person's reaction to treatment. This thorough approach not only supports continuity of care but also emphasizes what starts the clinical documentation of a patient visit, fostering effective communication within the care team.
Imagine the relief that comes from utilizing generative AI to enhance the quality and efficiency of clinical records. By automating routine record-keeping tasks, AI tools can significantly alleviate the administrative burden on medical providers, allowing them to focus more on what truly matters—the care of individuals. For instance, AI can assist in accurately capturing individual identification information, which is crucial as statistics reveal that identification errors account for around 70% of negative outcomes for individuals. Furthermore, healthcare institutions face an average of $1.3 million annually in expenses related to patient identity resolution, underscoring the financial implications of record inaccuracies.
Best practices for clinical records involve knowing what starts the clinical documentation of a patient visit by embracing electronic health record (EHR) systems, which enhance completeness and clarity. Nearly 90% of office-based doctors rely on EHR/EMR systems, which is what starts the clinical documentation of a patient visit and highlights their widespread use and importance in refining record-keeping practices. Educating medical practitioners about the significance of precise record-keeping can greatly enhance adherence and reduce errors. Research shows that trained health professionals are 4.2 times more likely to document routine practices compared to those without training. By following these best practices and integrating AI solutions, such as automated data entry and real-time error checking, providers can ensure high-quality records that reflect what starts the clinical documentation of a patient visit, meet regulatory standards, and significantly improve care for individuals.
Let’s take action together to enhance our record-keeping practices and ultimately improve patient care. By prioritizing accuracy and efficiency, we can make a meaningful difference in our healthcare environments.
Discuss the Impact of Clinical Documentation on Patient Care and Administration
Clinical records are not merely documentation; they illustrate what starts the clinical documentation of a patient visit, forming the backbone of compassionate care and effective medical management. Precise and promptly updated records are what starts the clinical documentation of a patient visit, enabling all members of the healthcare team to access crucial patient information. This accessibility empowers informed decision-making, which is essential for what starts the clinical documentation of a patient visit, ultimately enhancing the quality of care we provide. Research indicates that health professionals trained in regular practice recording are 4.2 times more likely to accurately document their practices. This underscores the importance of training in improving the quality of our records.
Moreover, effective record-keeping is essential not only for compliance with regulatory requirements but also for understanding what starts the clinical documentation of a patient visit that sustains our practices. Inaccurate records can lead to significant financial repercussions, with nearly 56% of coding errors linked to record-keeping issues. This highlights the urgent need for healthcare organizations to prioritize high-quality clinical records, as they represent what starts the clinical documentation of a patient visit, to safeguard their financial health.
Inadequate records can impact what starts the clinical documentation of a patient visit, leading to consequences that extend beyond financial implications, such as medical errors, miscommunication among providers, and diminished patient satisfaction. For instance, a Clinical Documentation Improvement Program (CDIP) implemented in trauma centers showed a remarkable improvement in the Observed/Expected (O/E) mortality ratio, decreasing from 1.36 to 0.70. This change reflects enhanced accuracy in mortality measures and a commitment to patient safety.
Given the challenges faced by medical providers, such as fatigue and resistance to change, what starts the clinical documentation of a patient visit is the prioritization of high-quality medical records. Innovative AI solutions, like CosmaNeura's Agentic Platform, can significantly improve clinical documentation processes. By harnessing the power of generative AI, providers can alleviate administrative burdens, enhance efficiency, and ultimately foster patient-centered care. This approach not only addresses operational challenges but also supports healthcare organizations in achieving financial sustainability.
How can we, as a community, embrace these changes to improve our practices? Together, we can take steps toward a future where high-quality documentation is the norm, ensuring that our focus remains on what starts the clinical documentation of a patient visit and providing the best possible care for our patients.

Conclusion
Effective clinical documentation serves as the cornerstone of patient care, establishing a vital connection between healthcare providers and patients. Have you ever considered what triggers this documentation and its essential components? Understanding these elements is crucial for ensuring that every patient visit is recorded accurately and comprehensively. This practice not only enhances communication among healthcare teams but also safeguards the quality and continuity of care that patients deserve.
The article highlights several key aspects of clinical documentation. It underscores the importance of maintaining precise medical records, identifying documentation triggers, and outlining essential components. Well-organized records can significantly improve health outcomes, support appropriate reimbursement, and reduce the risk of medical errors. Furthermore, the integration of innovative solutions like generative AI can streamline documentation processes, allowing healthcare providers to focus more on patient care rather than administrative burdens.
As the healthcare landscape continues to evolve, prioritizing high-quality clinical documentation becomes imperative. By committing to robust record-keeping practices, embracing technology, and fostering a culture of continuous improvement, healthcare providers can enhance patient care and administration. It is essential for all stakeholders in the healthcare system to recognize the profound impact that accurate documentation has on patient outcomes. Let us take proactive steps toward refining these practices for the benefit of everyone involved.




