Overview
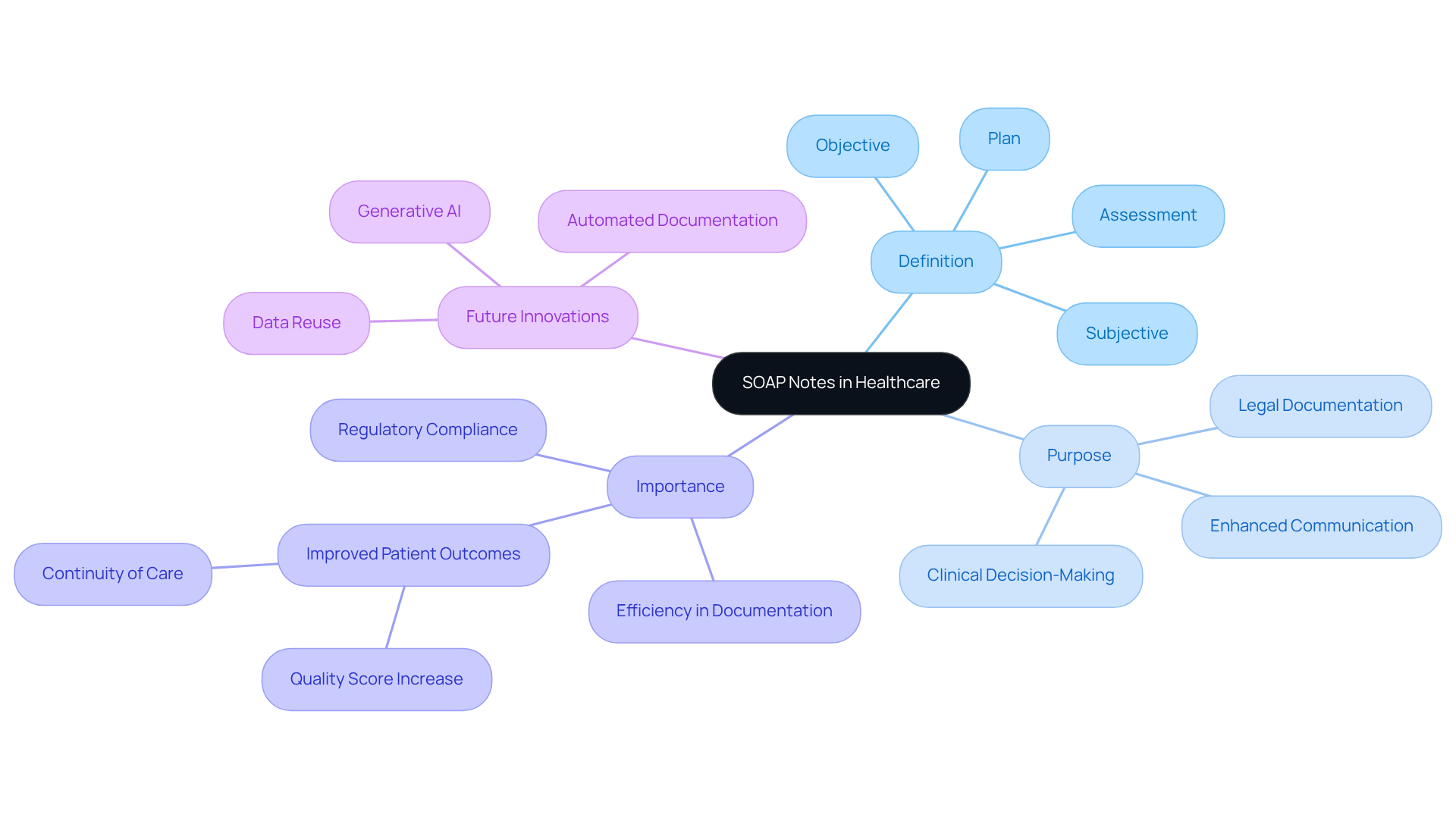
SOAP notes—standing for Subjective, Objective, Assessment, and Plan—are invaluable tools in healthcare. They provide structured documentation that not only enhances patient care but also fosters effective communication among providers.
Have you ever felt overwhelmed by the administrative burdens that can distract from patient interactions? This organized format, developed by Dr. Lawrence Weed, addresses these challenges head-on. It facilitates better clinical reasoning and improves patient outcomes, adapting seamlessly to various healthcare settings.
In a rapidly evolving landscape of medical documentation, embracing SOAP notes is essential for nurturing both patient relationships and professional collaboration.
Let’s explore how these notes can transform your practice and ultimately benefit your patients.
Introduction
Since their introduction in the 1960s, SOAP notes have profoundly changed the landscape of healthcare documentation, becoming a vital framework for nurturing effective patient care. They offer a structured approach that includes Subjective, Objective, Assessment, and Plan components. This not only fosters better communication among healthcare providers but also significantly enhances patient outcomes. However, as the demands of modern healthcare continue to evolve, practitioners may wonder: how can we adapt this time-tested method to navigate today’s fast-paced environment?
The emotional challenges faced by healthcare providers are significant. The increasing administrative burdens can often overshadow the core mission of patient care. This can leave professionals feeling overwhelmed, impacting their ability to connect meaningfully with patients. It’s essential to explore solutions that alleviate these pressures while maintaining the quality of care that patients deserve.
By embracing innovative strategies and tools, we can transform the way SOAP notes are utilized in practice. Imagine a system that streamlines documentation, allowing more time for patient interaction. This not only benefits healthcare providers but also leads to better outcomes for patients.
As we reflect on these challenges, let’s consider how we can work together to implement these changes. Your experiences and insights are invaluable in this journey. Together, we can foster a healthcare environment that prioritizes compassionate care while effectively managing the complexities of modern practice.
Define SOAP Notes: Purpose and Importance in Healthcare
SOAP note stands for Subjective, Objective, Assessment, and Plan, and these records serve as more than just a documentation method; they are a vital tool for healthcare providers navigating the complexities of patient care. Have you ever felt overwhelmed by fragmented communication in healthcare? These records encourage clear, organized communication among clinicians, which is essential in addressing the emotional and logistical challenges that arise in our healthcare systems.
Regulatory concerns, like HIPAA, often create barriers that complicate care. By organizing records in a structured way, healthcare providers can effectively document individual patient information, monitor progress, and ensure continuity of care. This organized approach not only enhances clinical reasoning but also significantly improves patient outcomes. Research indicates that well-structured records can lead to a remarkable increase in the quality of clinical entries—studies show a quality score rise from 64.35 to 77.2, reflecting a 12.8-point difference (p < 0.001).
Imagine the impact of such clarity on your daily practice. This method not only aids in clinical decision-making but also serves as a legal record of the care provided. Experts in the field highlight that clear documentation facilitates better management of patients and validates clinician fees during evaluations. Furthermore, structured records have been linked to improved client outcomes, underscoring their essential role in today’s healthcare landscape.
As we look to the future, the integration of generative AI holds promise for further enhancing the efficiency of clinical records. This technology can simplify record-keeping and enrich patient interactions, revolutionizing the way we provide care. Embracing such innovations can help alleviate administrative burdens, allowing you to focus more on what truly matters—your patients. How can you leverage these advancements to improve your practice today?
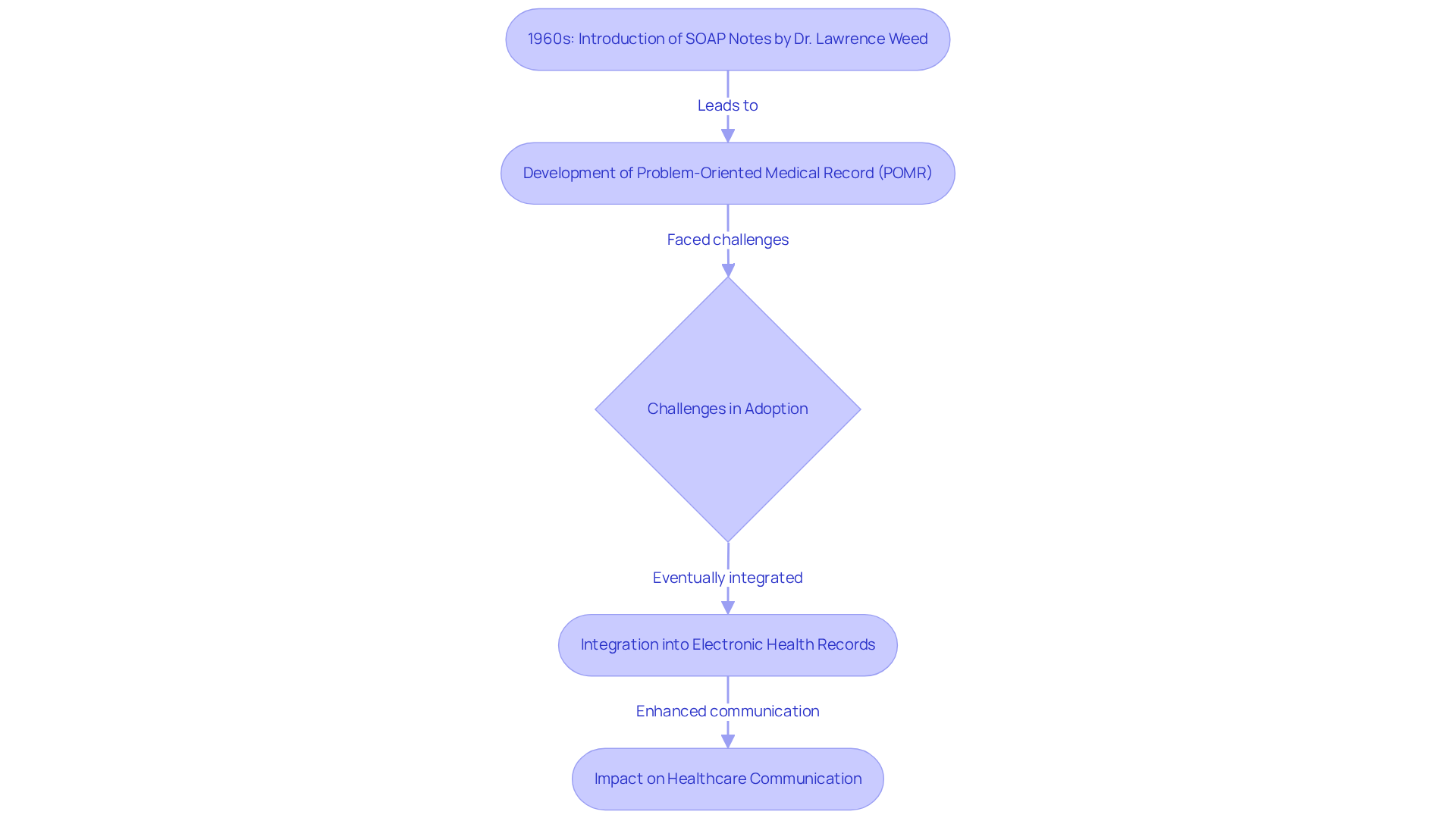
Trace the Origins and Evolution of SOAP Notes
The origins of these notes date back to the 1960s, a time when Dr. Lawrence Weed, a dedicated doctor and educator, recognized the pressing need for a standardized recording method in healthcare. His introduction of the Problem-Oriented Medical Record (POMR) laid the groundwork for a structured format that aimed to improve patient care. Although he faced challenges in convincing others to adopt this innovative approach, Weed's framework transformed medical record-keeping by organizing patient information into four essential sections: Subjective, Objective, Assessment, and Plan.
As the years have passed, structured records have evolved alongside advancements in medical practice and technology. They have become vital to electronic health records (EHRs), enhancing the effectiveness of clinical reporting. The impact of Weed's work is evident, with over 2000 academic articles describing, studying, or discussing the POMR, highlighting its profound influence on healthcare.
This organized method of documentation has proven indispensable across various healthcare settings, from primary care to specialized fields. Today, clinical summaries are celebrated for fostering transparent communication among healthcare professionals and ensuring comprehensive health records. This marks a significant leap forward in medical recording techniques, addressing the emotional challenges faced by providers.
Moreover, the flexibility of this format allows for the inclusion of functional results, underscoring the importance of client feedback and measurable data in effective documentation. By embracing these structured approaches, we can continue to support healthcare providers in their mission to deliver compassionate and comprehensive care.
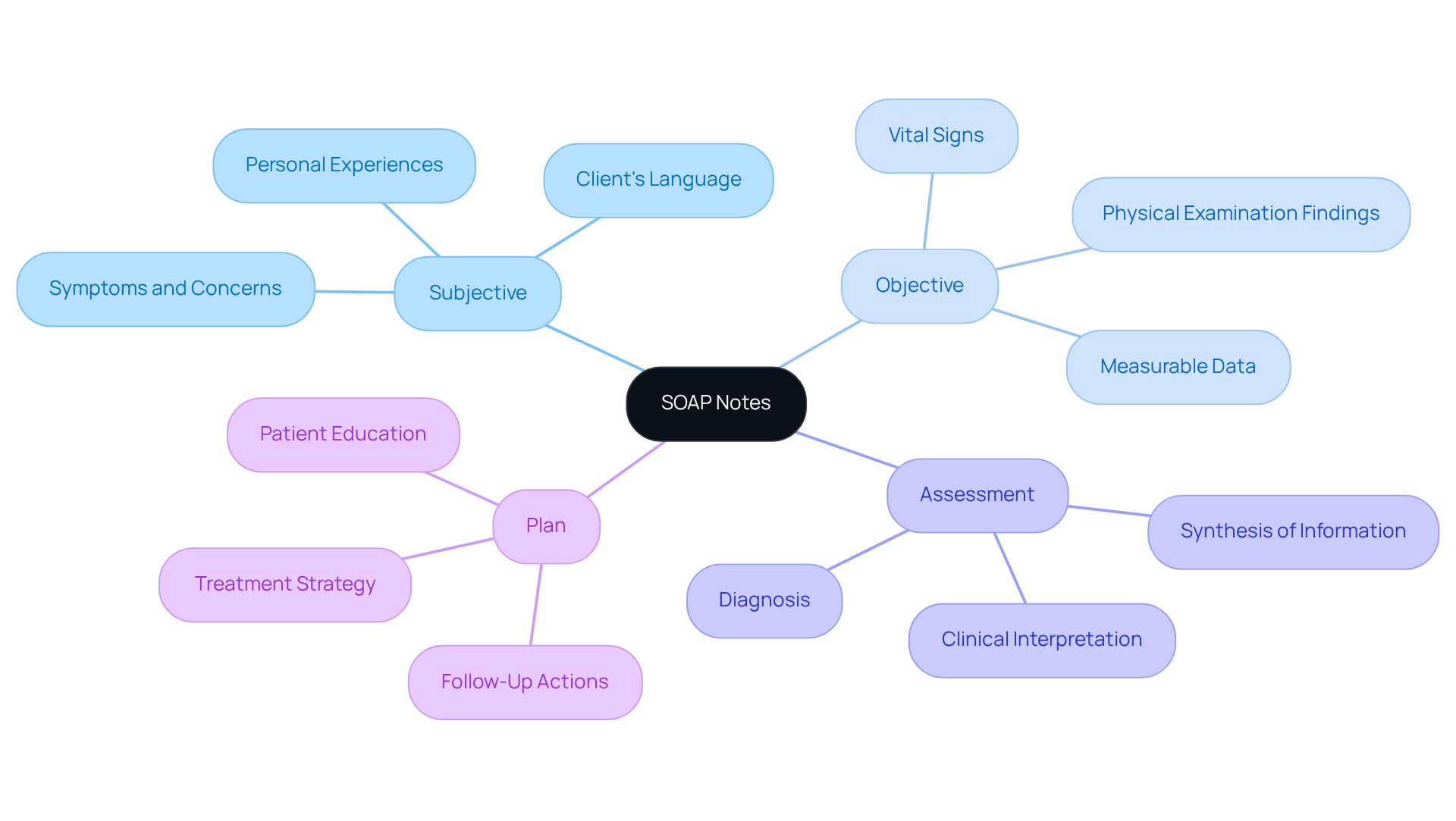
Analyze the Components of SOAP Notes: Subjective, Objective, Assessment, and Plan
SOAP note stands for essential tools that enhance our understanding and support of patients. They consist of four key components that not only help in documentation but also in fostering a more compassionate approach to care.
-
Subjective (S): This section captures the individual's personal experiences, symptoms, and concerns as reported by them. It offers vital context for the clinician's comprehension of the individual's condition, enabling a more customized approach to care. Effective documentation in this section often includes specific terminology used by individuals, which can enhance the accuracy of the recorded information. How often do we overlook the importance of truly listening to our patients?
-
Objective (O): Here, the clinician documents measurable and observable data, such as vital signs, physical examination findings, and results from diagnostic tests. This information is crucial for forming an accurate assessment. For instance, a clinician might note an individual's blood pressure reading of 130/85 mmHg or document that a person can walk three blocks before experiencing discomfort. These precise objective data points play a significant role in our clinical assessments. It’s a reminder that every detail matters in understanding our patients’ health journeys.
-
Assessment (A): This component involves the clinician's interpretation of the subjective and objective data, leading to a diagnosis or clinical impression. It reflects the clinician's clinical reasoning and judgment, synthesizing the information gathered to inform treatment decisions. For example, if an individual reports heightened anxiety and the clinician notices fidgeting, the evaluation may suggest a diagnosis of Generalized Anxiety Disorder (GAD). This assessment not only guides our next steps but also reassures the patient that their concerns are being taken seriously.
-
Plan (P): The final section outlines the proposed treatment strategy, including interventions, follow-up actions, and education for individuals. It acts as a guide for future care, ensuring that all team members are aligned on the individual's management. A well-structured plan might include recommendations for cognitive behavioral therapy (CBT) sessions and strategies for managing anxiety. By specifying the frequency of sessions and treatment methods, we can ensure that all aspects of the individual's care are addressed, fostering a sense of continuity and support.
Integrating objective information into clinical documentation not only aids in decision-making but also guarantees adherence to legal and insurance standards, ultimately enhancing patient results. The format created by Lawrence Weed in the 1950s, which the SOAP note stands for, has become a standardized approach widely utilized by healthcare professionals, underscoring the significance of organized records in clinical practice. Let’s continue to strive for excellence in our documentation, as it profoundly impacts the care we provide.
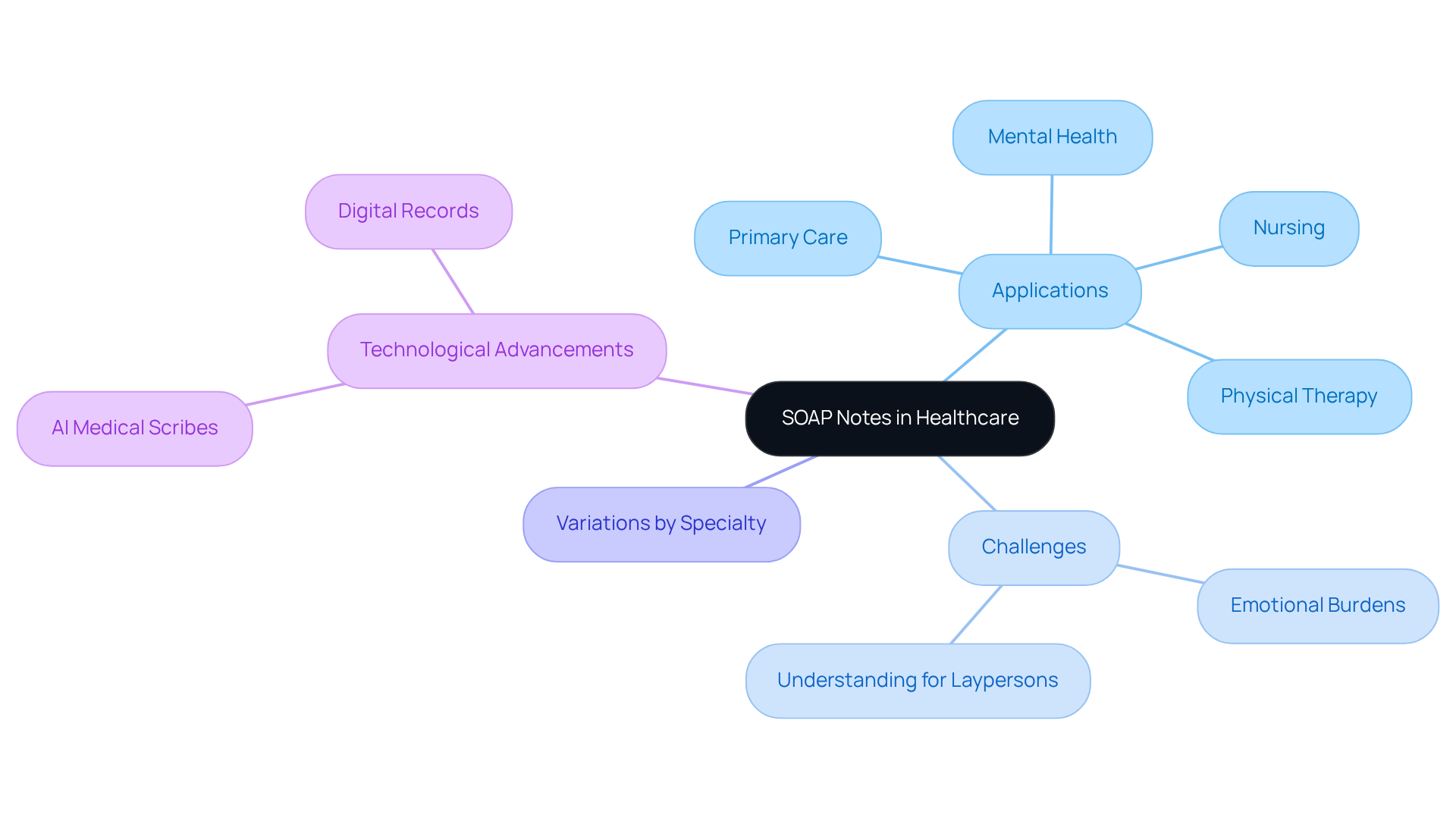
Examine Practical Applications and Variations of SOAP Notes in Healthcare
Structured documentation plays a crucial role in various healthcare fields, including primary care, mental health, physical therapy, and nursing. Created by Dr. Lawrence Weed in the 1960s as part of the Problem-oriented medical record (POMR), this organized format fosters consistent record-keeping, which is essential for effective communication among healthcare providers.
However, healthcare providers often face emotional challenges. The administrative burdens can weigh heavily, impacting the quality of patient care. Different forms of documentation may exist based on specialty; for instance, mental health specialists might emphasize the subjective aspect to better capture an individual’s emotional state.
It’s important to acknowledge that clinical records can sometimes be difficult for laypersons to understand, leading to overly brief entries and an excessive reliance on abbreviations. Yet, statistics reveal that employing organized records can significantly improve health outcomes. For example, healthcare professionals utilizing electronic progress summaries have experienced a remarkable 70% decrease in charting time, allowing them to focus more on patient care.
The advancement of technology has also paved the way for digital records, including those generated by AI medical scribes like Heidi, which optimize documentation processes and enhance accessibility. This adaptability highlights the importance of soap note stands for as vital tools in delivering high-quality patient care across various medical fields.
Let’s reflect on how we can support one another in navigating these challenges. Together, we can foster an environment where effective documentation not only streamlines our work but also enhances the care we provide to our patients.
Conclusion
The significance of SOAP notes in healthcare is profound, as they offer a structured framework for documenting patient information that enhances communication among providers and improves patient outcomes. By organizing clinical data into the Subjective, Objective, Assessment, and Plan components, healthcare professionals can navigate the complexities of patient care effectively, ensuring continuity and clarity in their documentation practices.
Consider the emotional challenges faced by healthcare providers daily. The administrative burdens can often feel overwhelming, diverting focus from the very essence of care. Throughout this article, we have explored key insights into the definition, historical development, and practical applications of SOAP notes. From their origins in the 1960s with Dr. Lawrence Weed’s introduction of the Problem-Oriented Medical Record to their current role in electronic health records, SOAP notes have proven to be invaluable tools for clinicians. This structured approach not only aids in clinical decision-making but also addresses the emotional challenges providers face, reinforcing the importance of effective communication in delivering high-quality care.
As healthcare continues to evolve, embracing innovations such as generative AI can further enhance the efficiency of SOAP note documentation. Imagine a future where providers can dedicate more time to patient interactions rather than paperwork. It is essential for healthcare professionals to recognize the transformative power of organized records in their practice and to continually strive for excellence in documentation. By doing so, they can ensure that patient care remains at the forefront, ultimately leading to better health outcomes and a more compassionate healthcare system. Let us commit to this journey together, fostering a supportive environment that prioritizes both provider well-being and patient care.




