Overview
In the demanding world of healthcare, providers often face emotional challenges that can weigh heavily on their ability to deliver care. Have you ever felt overwhelmed by the administrative tasks that seem to pile up, taking time away from your patients? The SOAP framework—Subjective, Objective, Assessment, and Plan—offers a compassionate solution to this common struggle.
By utilizing SOAP, healthcare providers can streamline their documentation process, allowing for more meaningful interactions with patients. Each component of SOAP enhances communication, ensuring that no detail is overlooked. This structured approach not only captures essential patient information but also fosters a deeper understanding of their needs, ultimately leading to improved patient outcomes.
Imagine the relief of knowing that your documentation is thorough and organized. With SOAP, you can focus on what truly matters—your patients. This method empowers you to provide comprehensive care while alleviating some of the burdens that come with administrative tasks.
Key Benefits of the SOAP Framework:
- Enhances communication between providers and patients.
- Ensures comprehensive care by capturing all relevant information.
- Improves patient outcomes through structured analysis.
As you consider implementing the SOAP framework, remember that it’s not just about efficiency; it’s about nurturing the patient-provider relationship. Take a moment to reflect on how this approach could transform your practice. Are you ready to embrace a method that prioritizes both your well-being and that of your patients? Let's engage further and explore how SOAP can make a difference in your daily practice.
Introduction
Understanding the SOAP acronym—Subjective, Objective, Assessment, and Plan—reveals a crucial framework that healthcare providers rely on to document patient encounters effectively. This structured method not only enhances clarity and communication among medical professionals but also plays a pivotal role in improving patient care outcomes.
Yet, many healthcare providers face emotional challenges as they navigate the complexities of documentation. The increasing administrative burdens can feel overwhelming, often detracting from the time and attention they wish to devote to their patients. How can practitioners ensure they are utilizing the SOAP method to its fullest potential amidst these pressures?
By embracing the SOAP framework, healthcare providers can streamline their documentation processes, ultimately benefiting both themselves and their patients. Here are some key solutions to consider:
- Prioritize clarity in documentation to enhance communication.
- Utilize technology that simplifies the documentation process.
- Engage in regular training to stay updated on best practices.
These strategies not only alleviate the stress of documentation overload but also foster a more compassionate approach to patient care. As the demands of healthcare continue to evolve, it’s essential to reflect on how we can adapt and thrive. Let’s explore how the SOAP method can be a guiding light in these challenging times.
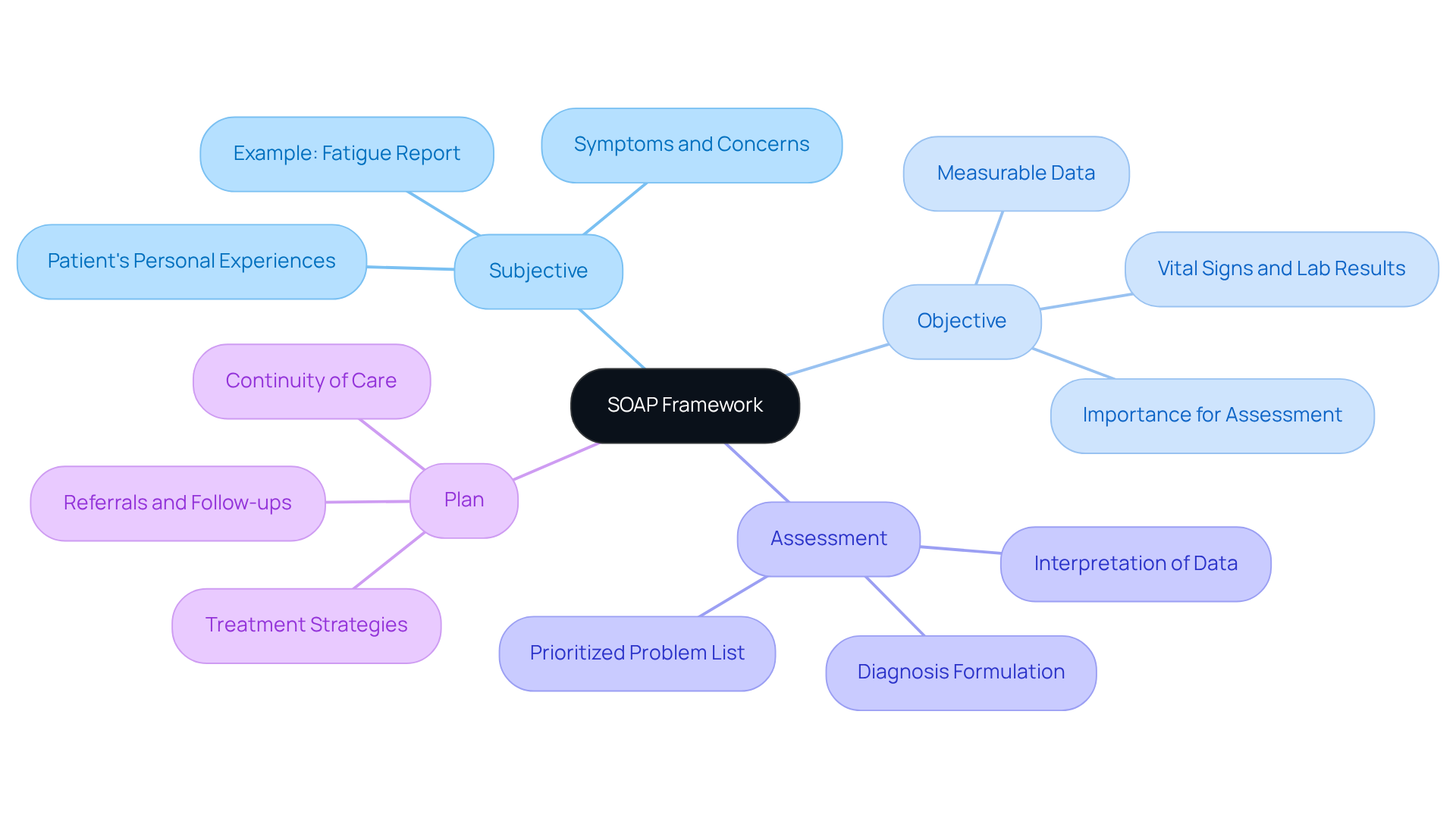
Define SOAP: The Acronym and Its Meaning
What is the SOAP acronym? It represents Subjective, Objective, Assessment, and Plan, and is a vital documentation method that healthcare providers use to record their encounters with patients. Each part of this framework plays a significant role in delivering comprehensive care, and understanding it can truly enhance your practice.
-
Subjective: This section captures the patient’s personal experiences, symptoms, and concerns. It’s where you get to hear their story. For example, if a patient mentions feeling fatigued, that insight can greatly influence treatment decisions.
-
Objective: Here, you document measurable data like vital signs and lab results. This objective information is crucial for assessing the patient’s current health status and tracking their progress over time.
-
Assessment: This is where you interpret the subjective and objective data. By synthesizing this information, you can formulate a diagnosis or identify issues that need addressing. A well-structured assessment can lead to a prioritized problem list, connecting impairments to functional limitations.
-
Plan: The plan outlines the proposed treatment strategies, including referrals and follow-up actions. It ensures continuity of care by detailing the next steps in the patient’s treatment journey.
The organized format of SOAP documentation not only improves clarity but also fosters effective communication among medical professionals. Have you ever felt overwhelmed by administrative tasks? Research shows that healthcare providers using electronic documentation systems are 2.2 times more likely to document their practices thoroughly compared to those relying on manual forms. This familiarity within the medical sector ultimately enhances care outcomes.
For instance, consider a clinical record for a patient with COPD and pneumonia. Using the SOAP format allows you to efficiently monitor their progress, adherence to treatment, and necessary adjustments in care. This approach showcases the practical advantages of structured documentation.
As emphasized by the American Physical Therapy Association, it’s our professional duty to ensure that documentation is clear and comprehensive. By embracing structured notes in clinical practice, we can better support our patients and improve their care experience. How can you incorporate this method into your routine to enhance your practice?
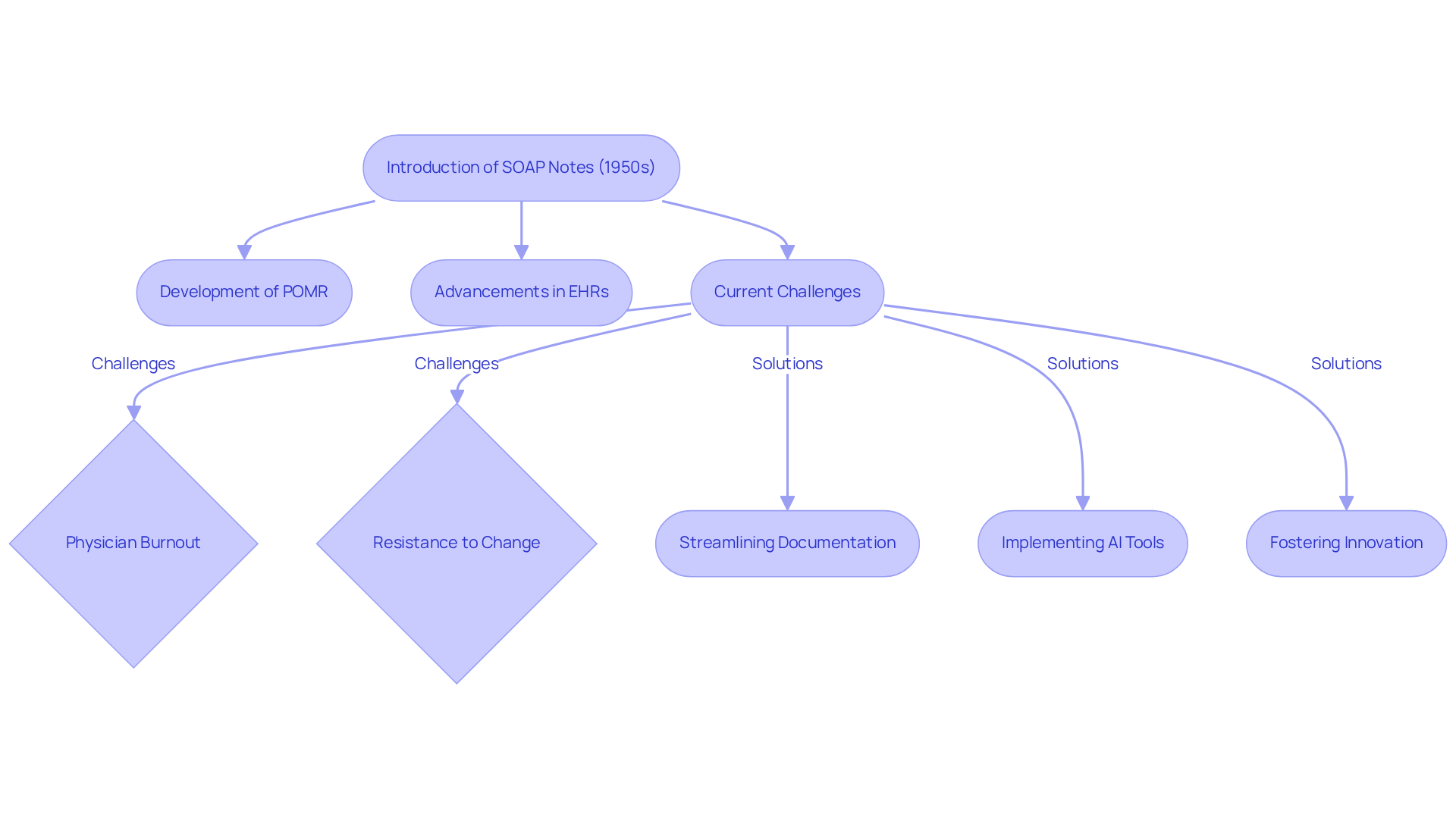
Trace the Origins and Evolution of SOAP Notes
In the demanding world of healthcare, providers often face emotional challenges that can weigh heavily on their practice. The documentation format, introduced in the 1950s by Dr. Lawrence Weed, aimed to alleviate some of these burdens. He recognized the need for a consistent way to record care, which led to the development of SOAP notes, also known as what is SOAP acronym, as part of the Problem-Oriented Medical Record (POMR). Dr. Weed emphasized, "The main aim of the POMR is to offer medical providers with organization when recording client sessions."
As medical technology and electronic health records (EHRs) have advanced, the documentation format has evolved, becoming essential in both clinical and administrative settings. The transition to EHRs has significantly improved documentation efficiency, allowing for quick access and distribution of medical records. This is crucial for managing chronic conditions effectively. Yet, despite these advancements, healthcare providers still grapple with considerable challenges, such as physician burnout and resistance to change. These issues can hinder the effective use of documentation, impacting patient care.
Currently, thorough documentation forms are vital for ensuring comprehensive client records and continuity of care. They help reduce errors and foster effective collaboration among medical professionals. With innovative AI solutions like CosmaNeura's Agentic Platform, healthcare providers can enhance documentation effectiveness, addressing administrative hurdles and ultimately improving patient care.
Key Solutions to Consider:
- Streamlining documentation processes to reduce administrative burdens.
- Implementing AI tools to support healthcare providers in their daily tasks.
- Fostering a culture of innovation to embrace new technologies.
By embracing these solutions, healthcare providers can navigate the complexities of documentation with greater ease, allowing them to focus on what truly matters: the well-being of their patients. Together, we can create a more supportive environment that prioritizes compassionate care.
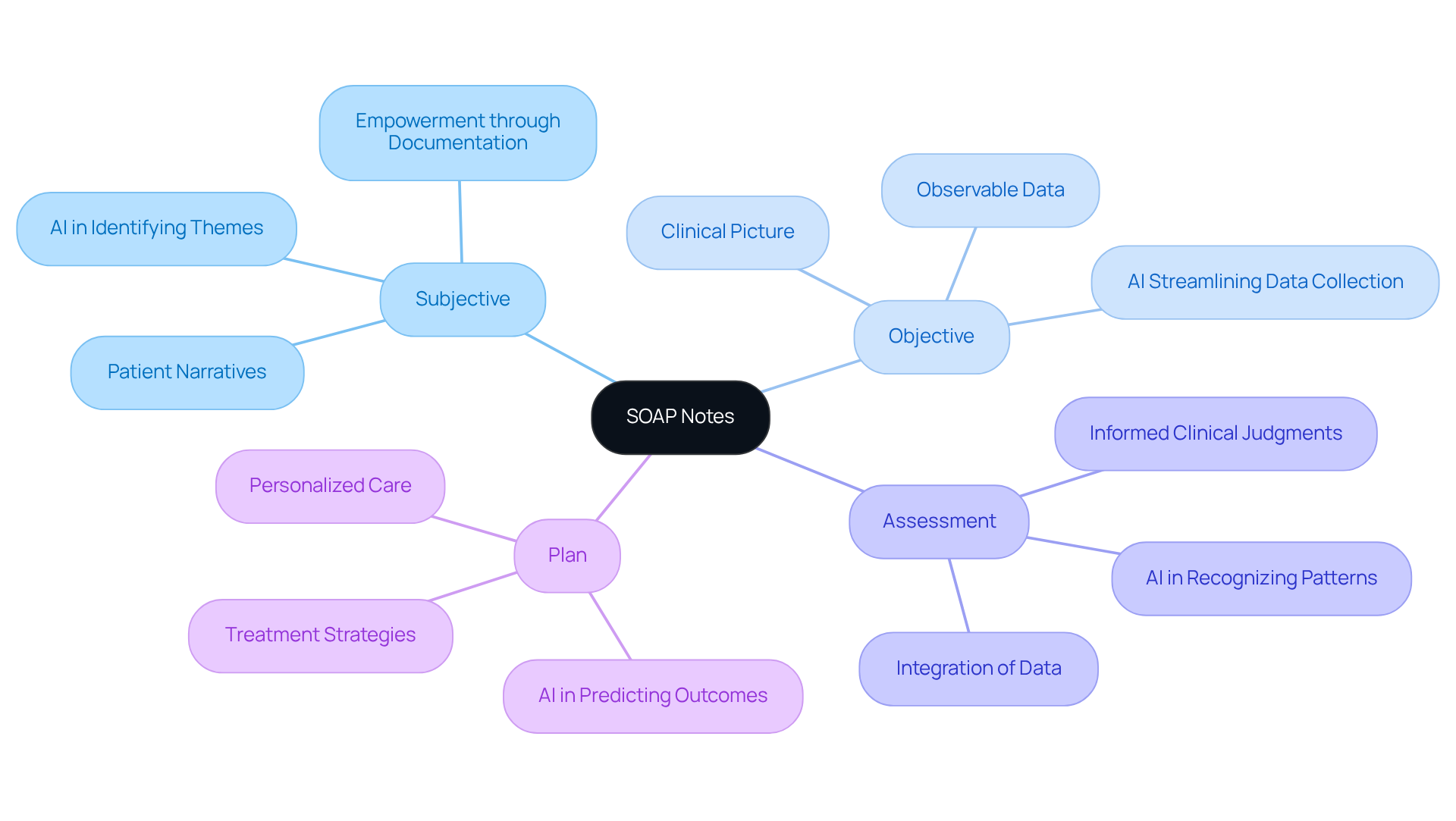
Examine the Key Components of SOAP Notes
Each component of the SOAP note plays a vital role in documenting patient encounters, and the integration of generative AI can further enhance these interactions:
-
Subjective: This section captures the patient's narrative, including their symptoms, concerns, and medical history as reported by them. It reflects the individual's perspective and is essential for understanding their experience. Effective subjective documentation can significantly enhance care by accurately capturing reported outcomes, empowering medical teams to provide personalized treatment. How can we ensure that every patient's voice is heard? Generative AI can aid in this area by examining narratives and identifying key themes, ensuring that providers have a thorough understanding of the individual's experience. A study indicated that precise subjective SOAP notes significantly enhance care by capturing outcomes reported by individuals.
-
Objective: Here, healthcare providers document observable and measurable data, such as physical examination findings, lab results, and vital signs. This information is critical for forming an accurate clinical picture. For example, recording vital signs and lab results aids clinicians in evaluating the individual's condition and monitoring changes over time, which is crucial for efficient treatment planning. Imagine having quicker access to vital information that supports clinical decision-making. AI tools can streamline the collection and analysis of this data, allowing for just that.
-
Assessment: This component integrates the subjective and objective data, enabling the clinician to make informed judgments about the individual's condition. It often includes diagnoses or differential diagnoses. However, a constraint of the structured format is its incapacity to record changes over time, which is essential in clinical contexts where evidence and individual conditions develop. By utilizing AI, healthcare providers can improve the precision of evaluations using SOAP notes, as AI can recognize patterns and trends in individual data that inform clinical reasoning and decision-making.
-
Plan: The final section outlines the proposed treatment strategy, including medications, referrals, follow-up appointments, and education for individuals. This ensures that both the provider and individual have a clear understanding of the next steps in care. How can we make treatment plans more personalized? Generative AI can assist in developing more customized and actionable plans by analyzing individual data and predicting potential outcomes, guiding future interactions and treatment modifications.
Integrating these components into medical records not only promotes improved communication among providers but also boosts the overall quality of care given to individuals. By incorporating generative AI into the documentation process, medical providers can reduce administrative loads like scheduling and handling medical records. This shift enables them to concentrate more on providing outstanding care to individuals.
Let’s embrace these advancements together, ensuring that every patient receives the compassionate care they deserve.
Explore the Benefits and Applications of SOAP Notes in Healthcare
SOAP notes play a crucial role in healthcare, addressing the emotional challenges faced by providers while enhancing patient care and operational efficiency:
-
Standardization: Have you ever felt overwhelmed by inconsistent documentation? SOAP notes establish a clear structure that improves clarity and reduces variability in patient records. This uniformity not only facilitates better communication among healthcare teams but also ensures that critical information is readily accessible. Research shows that standardized documentation can significantly enhance record quality, with scores jumping from 64.35 to 77.2 (p < 0.001).
-
Enhanced Patient Care: Imagine how much more effective your evaluations could be with organized clinical documentation. This structured approach leads to more accurate diagnoses and successful treatment strategies. By considering all relevant individual information, we can achieve better health outcomes. For instance, a systematic review found that structured documentation frameworks greatly enhance interdisciplinary collaboration and support safer transitions of care.
-
Legal Safeguard: Have you thought about the importance of well-kept documentation? These records serve as vital legal safeguards, capturing individual interactions and protecting both healthcare providers and patients in case of disputes or audits. As medical leaders emphasize, 'The more concise yet comprehensive a clinical record is, the simpler it is for practitioners to follow.'
-
Improved Efficiency: Are administrative duties taking time away from patient care? Utilizing structured documentation can streamline the record-keeping process, allowing you to focus more on your patients rather than paperwork. This efficiency is especially crucial in high-volume clinical settings, where every moment counts. Studies indicate that using documentation software can save time and boost productivity, enabling therapists to concentrate more on client care.
In summary, the SOAP acronym is indispensable in modern healthcare. They foster effective communication, ensure continuity of care, and ultimately lead to improved patient outcomes. Let's embrace this vital tool together for a brighter future in healthcare.

Conclusion
In the demanding world of healthcare, providers often face emotional challenges that can weigh heavily on their ability to deliver care. The administrative burdens can sometimes overshadow the core mission: to support and heal patients. How can we shift this narrative? By embracing the SOAP framework, we can transform documentation from a chore into a powerful tool for patient-centered care.
The SOAP acronym—Subjective, Objective, Assessment, and Plan—serves as a vital framework in healthcare. It not only clarifies medical records but also enhances the quality of patient care. By effectively utilizing SOAP notes, healthcare providers can ensure comprehensive documentation that supports informed decision-making and fosters better communication within medical teams.
Consider the benefits of structured documentation:
- Improved clarity in patient records.
- Enhanced communication among medical teams.
- Legal safeguards for providers.
- Better patient outcomes through informed care.
Each component of SOAP notes plays a crucial role. The Subjective section captures the patient's narrative, while the Objective part presents measurable data, leading to a well-informed Assessment and a clear Plan for treatment. The evolution of SOAP notes, from their origins in the 1950s to their current applications enhanced by technology and AI, highlights their ongoing relevance in modern healthcare.
Incorporating the SOAP framework into daily practice is more than just a documentation task; it’s a commitment to delivering high-quality, patient-centered care. As healthcare continues to evolve, embracing structured documentation will empower providers to focus on what truly matters: the health and well-being of their patients. By prioritizing effective communication and comprehensive records, we can pave the way for a brighter future in healthcare, ensuring that every patient receives the compassionate care they deserve.
Let’s take this step together. How can you integrate the SOAP framework into your practice today?




