Overview
In the demanding world of healthcare, communication is vital. SOAP, which stands for Subjective, Objective, Assessment, and Plan, represents a structured documentation method designed to enhance this communication and ultimately improve patient care. Each component of SOAP plays a critical role in capturing essential information, aiding clinical decision-making, and ensuring continuity of care.
Consider the emotional challenges healthcare providers face daily. The burden of administrative tasks can weigh heavily, detracting from the time spent with patients. This is where SOAP notes become invaluable. They streamline documentation, allowing healthcare professionals to focus on what truly matters—the well-being of their patients.
By using SOAP notes, healthcare providers can foster better clinical outcomes. This method not only organizes vital information but also enhances collaboration among care teams. Imagine the peace of mind that comes from knowing that every detail is documented clearly, enabling seamless transitions in patient care.
We encourage healthcare professionals to embrace the SOAP framework. Reflect on your current documentation practices and consider how adopting SOAP notes can alleviate some of the pressures you face. Together, we can enhance the quality of care provided to patients, ensuring they receive the attention and support they deserve.
Introduction
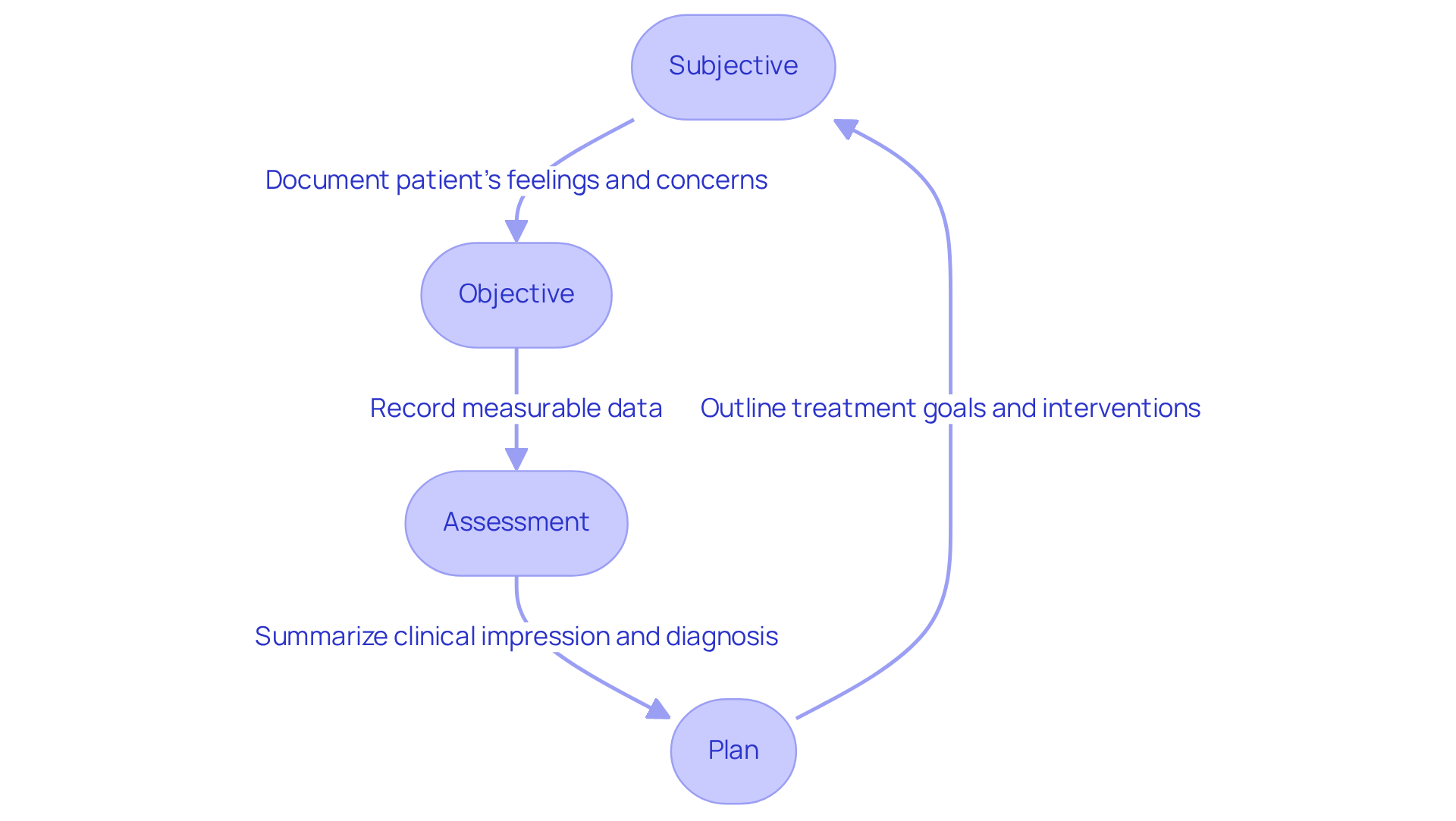
Structured documentation has become a cornerstone of effective healthcare communication. Yet, many healthcare providers grapple with the specifics of its implementation. Have you ever felt overwhelmed by the demands of documentation? The SOAP format—an acronym for Subjective, Objective, Assessment, and Plan—offers a systematic approach for recording patient information. This method not only enhances clinical decision-making but also plays a vital role in improving patient outcomes.
However, as the healthcare landscape evolves with technology, how can professionals ensure that the benefits of SOAP notes are fully realized? It’s essential to address the inherent challenges of documentation that can often feel burdensome. The administrative tasks can weigh heavily on your ability to provide compassionate care.
Consider the following key solutions to streamline your documentation process:
- Embrace technology that integrates with SOAP notes to reduce manual entry.
- Collaborate with your team to share best practices and tips.
- Allocate time for training and support to ensure everyone is comfortable with the format.
By implementing these strategies, you can alleviate some of the pressures of documentation. Imagine the peace of mind that comes from knowing your notes are clear, concise, and beneficial for your patients. Let’s work together to ensure that the true potential of SOAP notes is realized, allowing you to focus on what truly matters—providing exceptional care.
Defining SOAP Notes: Purpose and Importance in Healthcare
Structured documentation methods represent a systematic approach that healthcare professionals use to record vital information and clinical encounters. The abbreviation for Subjective, Objective, Assessment, and Plan raises the question of what does soap stand for, as it encompasses four components, each serving a specific purpose in the documentation process. This structured format not only facilitates clear and concise communication among healthcare professionals but also ensures that all pertinent information is captured effectively.
The importance of clinical records extends beyond mere documentation; they are essential for improving healthcare. By providing a detailed summary of an individual's condition, these records assist in clinical decision-making and enhance continuity of care among various providers and environments. Regulatory issues, such as HIPAA, create communication obstacles that effective documentation helps alleviate, ultimately leading to better health outcomes. Studies indicate that structured documentation reduces miscommunication and enhances coordination among healthcare teams.
Practical applications of structured documentation further illustrate their impact. For instance, a healthcare professional utilized structured notes to document an individual's progress in a rehabilitation program, detailing specific goals for ambulation and exercise. This organized approach not only improved the individual's compliance with the treatment plan but also facilitated better follow-up support, resulting in enhanced recovery outcomes.
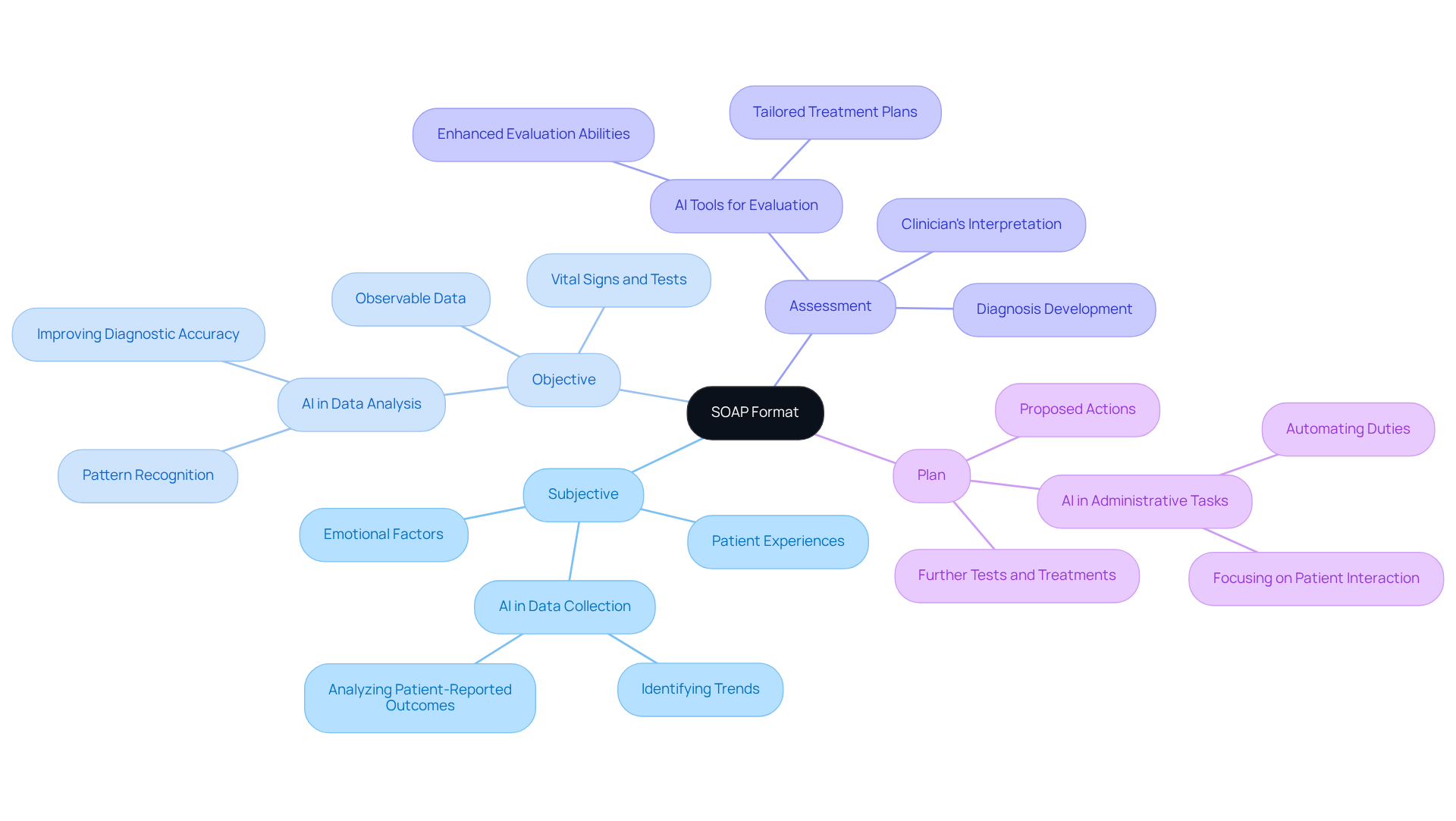
Moreover, the integration of AI tools with medical documentation has shown to improve the note-taking process. This allows clinicians to focus more on client interactions rather than administrative tasks. Such a shift not only boosts job satisfaction among healthcare providers but also fosters a more empathetic approach to service, aligning with the ethical standards upheld in faith-oriented healthcare practices. By addressing both communication barriers and administrative burdens, clinical documentation and AI solutions together enhance the overall quality of care.
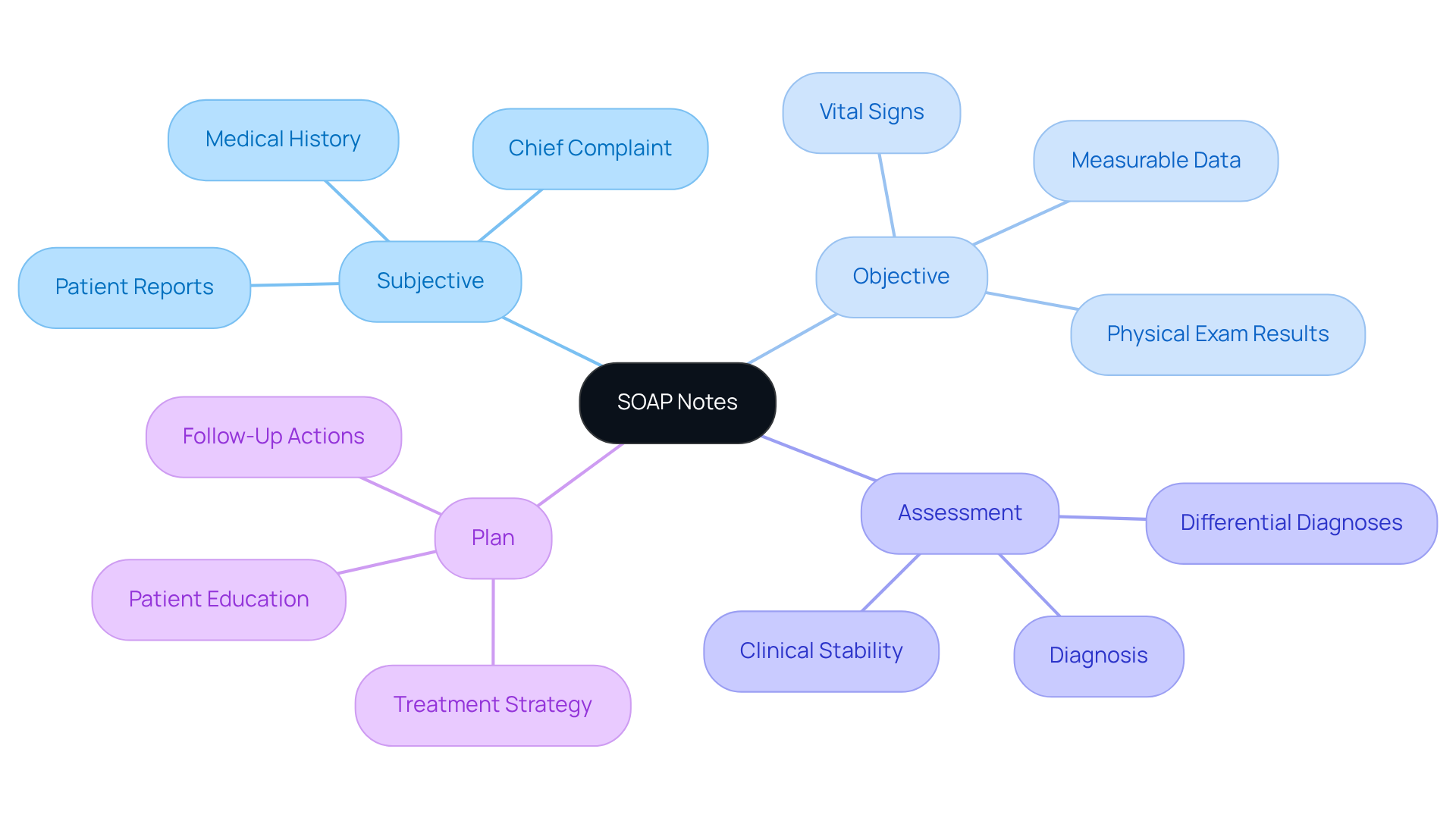
Breaking Down SOAP: Subjective, Objective, Assessment, and Plan
The SOAP format represents a structured approach to medical documentation, consisting of four essential components that aim to enhance patient care and provider efficiency:
-
Subjective: This section captures the patient's personal experiences, symptoms, and feelings as reported by them. It includes the individual's history, concerns, and any pertinent emotional or psychological factors, offering a comprehensive perspective of their health. Have you considered how leveraging AI in this section can enhance the collection of subjective data? By analyzing patient-reported outcomes and identifying trends, AI may inform better care.
-
Objective: In this part, healthcare providers document observable and measurable data, including vital signs, physical examination findings, and results from diagnostic tests, which relates to what does soap stand for. Accurate objective measurements are crucial. Studies indicate that they significantly enhance the reliability of clinical assessments, ensuring a precise clinical picture. Imagine AI algorithms assisting in analyzing this data, identifying patterns that might be missed, and ultimately improving diagnostic accuracy.
-
Assessment: This component involves the clinician's interpretation of both subjective and objective data, leading to a diagnosis or identification of the individual's problems, which raises the question of what does soap stand for. By incorporating AI tools, clinicians can enhance their evaluation abilities, resulting in more precise diagnoses and tailored treatment plans that meet the unique needs of each individual.
-
Plan: The final section outlines the proposed course of action, including what does soap stand for, such as further tests, treatments, referrals, and education for individuals. Generative AI can simplify this process by automating administrative duties, allowing healthcare providers to concentrate more on client interactions and less on paperwork.
Efficient documentation of clinical records not only enhances communication among healthcare professionals but also improves outcomes for individuals by ensuring that all aspects of treatment are considered and addressed. By utilizing AI, healthcare professionals can further improve the quality of service provided, ultimately transforming outcomes for individuals.
As we navigate these challenges together, consider how adopting these innovative solutions can lighten the load and enhance the compassionate care we strive to provide.
The Evolution of SOAP Notes: Historical Context and Development
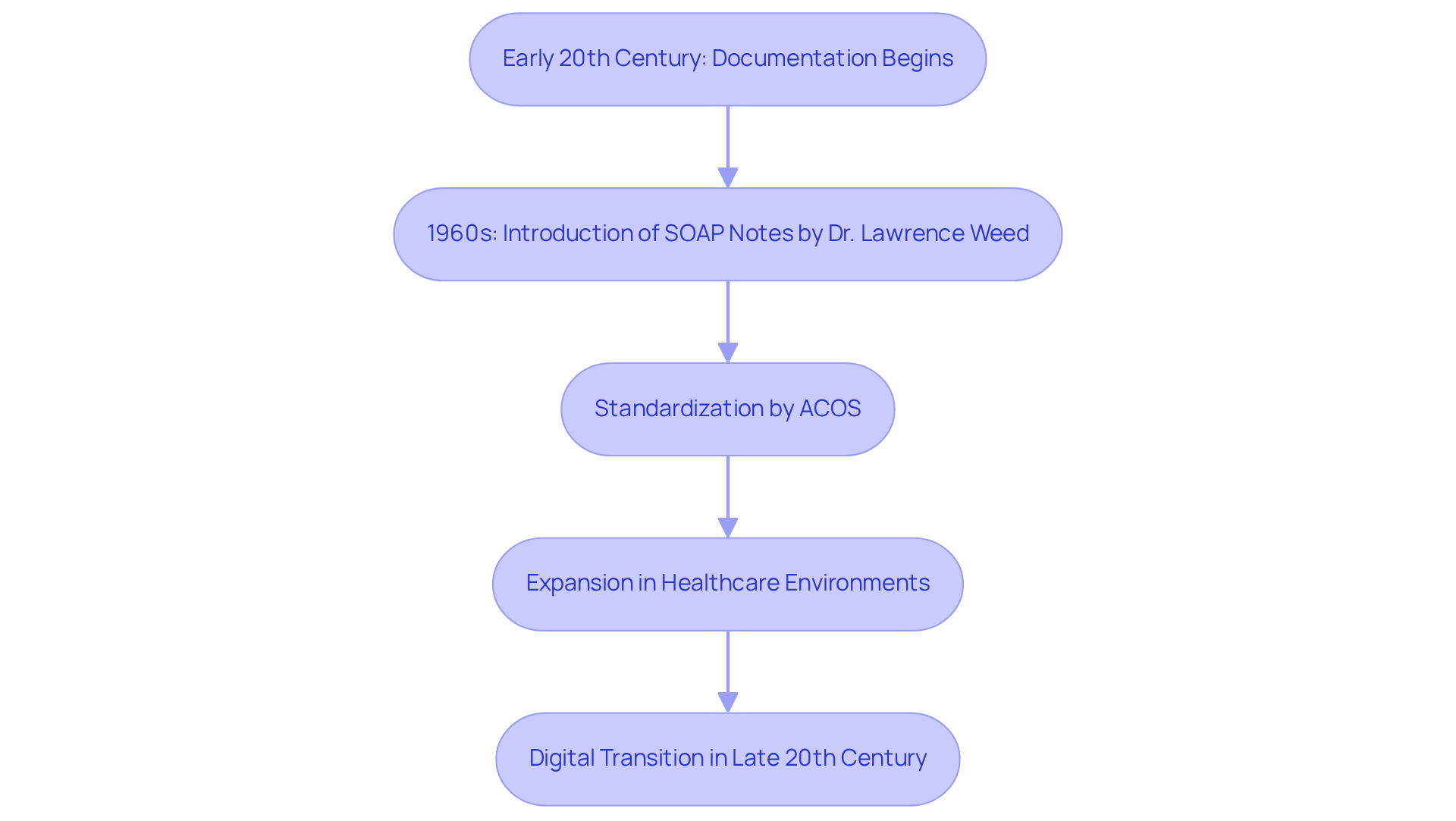
SOAP notes were first introduced in the 1960s by Dr. Lawrence Weed as part of the problem-oriented medical record (POMR) approach. This approach aimed to enhance the structure and clarity of medical records, which is essential for managing individuals and ensuring continuity of care.
The creation of medical records can be traced back to the early 20th century, when physicians began documenting details of visits and medical histories. This shift led to the standardization of practices by the American College of Surgeons (ACOS). Over the decades, structured documentation has become a standard practice in various healthcare environments, including hospitals, clinics, and private practices.
Have you ever considered how effective communication among healthcare providers can impact patient outcomes? The structured format of SOAP notes raises the question of what does SOAP stand for, as it has proven effective in ensuring that critical information is readily accessible and easily understood. As healthcare progresses, particularly with the transition to digital platforms in the late 20th century, these records remain an essential resource for documenting individual treatment and promoting interdisciplinary collaboration.
However, it’s important to recognize the ongoing discussions about the potential drawbacks of structured documentation. For instance, the tendency for vague records and the sequential approach they encourage may impede effective clinical reasoning. Despite these concerns, the extensive use of structured documentation highlights their importance in improving the quality of treatment and ensuring that individual stories are respected in the decision-making process.
In light of these challenges, how can we continue to support effective documentation practices while addressing the emotional and administrative burdens faced by healthcare providers? Engaging in discussions about best practices and sharing experiences can foster a more compassionate approach to patient care.
Practical Applications of SOAP Notes: Examples Across Healthcare Settings
Structured documentation is essential in various healthcare environments, including primary health, mental health, and specialty clinics. Have you ever felt overwhelmed by the administrative tasks that take time away from patient care? In primary care, for instance, a clinician may document a patient's visit for hypertension management using the SOAP format:
- Subjective: The patient reports feeling fatigued and has experienced headaches.
- Objective: Blood pressure reading is 150/95 mmHg; weight is 180 lbs.
- Assessment: The individual is diagnosed with stage 1 hypertension.
- Plan: Initiate lifestyle modifications, prescribe antihypertensive medication, and schedule a follow-up appointment in one month.
In mental health settings, structured documentation plays a vital role in tracking an individual's progress over time. Consider a patient with Generalized Anxiety Disorder (GAD) who might have a SOAP note that reflects:
- Subjective: The patient reports feeling 'constantly on edge' and experiencing panic attacks, with a 6-month history of increasing anxiety symptoms.
- Objective: The individual seems anxious, fidgety, and avoids eye contact.
- Assessment: The individual is diagnosed with GAD, considering recent job loss and family history of anxiety disorders.
- Plan: Continue weekly therapy focused on cognitive-behavioral techniques and consider medication evaluation if symptoms do not improve.
Statistics reveal that poor communication is one of the most prevalent reasons for sentinel events. This underscores the importance of organized records, such as structured documentation, in preventing such incidents. The organized layout of clinical documentation enhances usability for healthcare professionals, improving task success during consultations.
Moreover, integrating generative AI can streamline the documentation process by automating administrative tasks like data entry and record management. This allows healthcare providers to devote more time to patient-centered care, addressing challenges like physician burnout and inefficiencies in care delivery. By regularly refreshing documentation, clinicians can effectively monitor client progress and adjust interventions as needed, ultimately leading to improved patient outcomes. As noted by HealthOrbit AI, 'SOAP notes — what does soap stand for? — refers to Subjective, Objective, Assessment, and Plan, and have long been the gold standard for clinical documentation.'
Let’s embrace structured documentation as a tool not just for compliance, but as a means to enhance the quality of care we provide, ensuring that we are present for our patients in the ways they truly need.
Conclusion
In the demanding world of healthcare, the SOAP format serves as a lifeline, offering a structured approach that not only enhances communication among providers but also significantly improves patient care. By breaking down clinical encounters into Subjective, Objective, Assessment, and Plan, healthcare professionals can capture vital information comprehensively and efficiently.
Have you ever felt overwhelmed by the administrative tasks that pull your focus away from patient interactions? The significance of SOAP notes cannot be overstated; they facilitate clear communication and enhance continuity of care, supporting clinical decision-making. With the integration of AI tools, these benefits are amplified, streamlining documentation processes and allowing clinicians to prioritize what truly matters—caring for their patients.
As we reflect on the historical context of SOAP notes, it is clear that they have evolved into a standard practice in healthcare, adapting to meet the challenges of modern medical environments. Embracing the SOAP format is not just about compliance; it is a vital component of delivering high-quality care in an ever-changing landscape.
As healthcare continues to advance, our commitment to structured documentation will play an essential role in improving patient outcomes. By adopting these practices and exploring innovative solutions, we can foster a more compassionate approach to healthcare delivery. Together, let’s create a more efficient and empathetic healthcare system that prioritizes the needs of both providers and patients.




