Introduction
Structured documentation has truly transformed the landscape of healthcare, offering a systematic way to capture patient interactions and clinical insights. Have you ever felt overwhelmed by the demands of efficient documentation? SOAP notes—standing for Subjective, Objective, Assessment, and Plan—are more than just a framework; they enhance communication among healthcare professionals and significantly improve patient outcomes.
Yet, as the pressures for accurate documentation continue to rise, how can practitioners effectively navigate the complexities of this method? The intricacies and applications of SOAP notes reveal their essential role in fostering comprehensive patient care. They help address the challenges faced in modern medical practices, allowing you to focus more on what truly matters—your patients.
Consider the following benefits of utilizing SOAP notes:
- Improved communication among team members.
- Enhanced patient outcomes through thorough documentation.
- Streamlined processes that reduce administrative burdens.
By embracing structured documentation, you can alleviate some of the stress that comes with administrative tasks. Let’s explore how SOAP notes can support you in providing the best care possible, ensuring that your focus remains on your patients' needs.
Define SOAP Notes: Purpose and Structure
Structured notes, which are what are soap notes in the medical field, represent a standardized way for healthcare professionals to document client interactions effectively. Have you ever felt overwhelmed by the sheer volume of information you need to manage? The SOAP acronym—Subjective, Objective, Assessment, and Plan—defines what are soap notes in the medical field and provides a clear framework to help you navigate these challenges. The Subjective section captures personal experiences, including symptoms and concerns, while the Objective section records measurable data like vital signs and test results. The Assessment synthesizes this information, offering the clinician's interpretation and diagnosis, and the Plan outlines proposed treatment strategies and follow-up actions.
This structured approach not only enhances communication among healthcare providers but also plays a vital role in ensuring comprehensive patient care, which is essential for understanding what are soap notes in the medical field. Research shows that structured documentation can significantly reduce medical record mistakes, which are linked to 37% of severe injury cases. Furthermore, about 70% of healthcare practitioners now use structured documentation in their practice. This highlights its importance in facilitating effective clinical interactions. By adopting this method, clinicians can improve outcomes through better diagnosis, treatment planning, and progress tracking, which illustrates what are soap notes in the medical field, ultimately fostering a more efficient healthcare environment.
Incorporating generative AI into the documentation workflow can further enhance the efficiency of administrative tasks related to clinical records. Imagine having AI streamline the documentation of client interactions, arrange appointments, and send reminders. This allows healthcare professionals to focus more on providing care. Not only does this improve the quality of documentation, but it also helps reduce physician burnout by handling repetitive tasks and optimizing workflows. Additionally, clinical documentation promotes interoperability in healthcare, enhancing communication among various EHR systems, which is essential for coordinated and effective care.
Key Benefits of Structured Documentation and AI Integration:
- Improved Communication: Enhances collaboration among healthcare providers.
- Reduced Errors: Lowers the risk of mistakes in medical records.
- Increased Efficiency: Frees up time for healthcare professionals to focus on patient care.
- Enhanced Patient Outcomes: Leads to better diagnosis and treatment planning.
As you reflect on your own experiences, consider how structured documentation and AI can transform your practice. Together, we can create a more supportive and efficient healthcare environment.

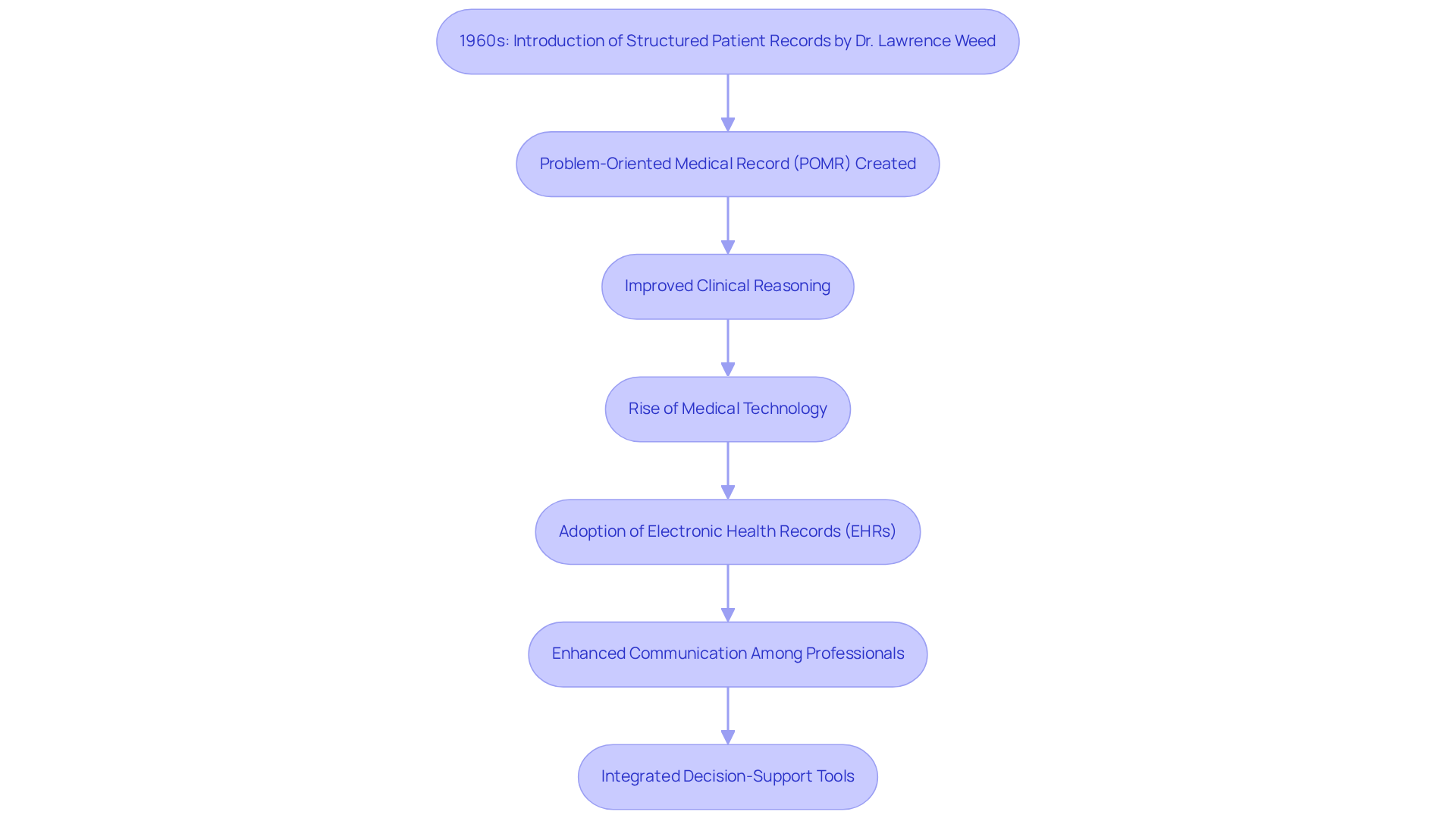
Explore the History and Evolution of SOAP Notes
The introduction of structured patient records in the 1960s by Dr. Lawrence Weed marked a significant shift in clinical documentation practices. Have you ever felt overwhelmed by the inconsistencies in patient records? Dr. Weed recognized this challenge and created structured documentation as part of the Problem-Oriented Medical Record (POMR). This approach aimed to improve clinical reasoning and ensure systematic recording of patient information, addressing the documentation issues that healthcare faced before.
Since then, structured documentation has evolved significantly, especially with the rise of medical technology and electronic health records (EHRs). Initially, it provided a clear framework that enhanced communication among healthcare professionals, leading to better continuity of treatment. As EHR systems advanced, incorporating structured documentation became essential, allowing for quick access and exchange of medical records, which further improved coordinated support.
Historical case studies show how structured documentation has positively impacted healthcare practices. For instance, its adoption has led to better inter-physician communication and improved precision in patient treatment. The organized framework of medical records not only reduces mistakes and oversights but also enhances quality care through comprehensive documentation.
Experts emphasize that the principles behind documentation remain crucial as healthcare continues to evolve. The transition from paper-based records to electronic formats has streamlined the documentation process, making it more efficient while preserving the integrity of individual information. As technology progresses, clinical documentation is expected to include integrated decision-support tools and AI-driven recommendations, further enhancing its usefulness in healthcare environments.
In summary, the development of clinical records reflects a commitment to improving treatment through organized documentation. This ensures that healthcare professionals can provide informed and coordinated assistance. Let’s continue to support each other in navigating these changes, ensuring that we can deliver the best care possible.
Break Down the Key Components of SOAP Notes
Each component of a SOAP note plays a distinct and vital role in patient care, addressing both the needs of healthcare providers and the emotional experiences of patients:
-
Subjective: This section captures the patient's perspective, encompassing their symptoms, feelings, and concerns. It often includes direct quotes, offering valuable insight into their experience and emotional state. For instance, a patient might express heightened anxiety, which can guide the clinician's treatment strategy. Additionally, the Review of Systems (ROS) can reveal further symptoms not initially mentioned, ensuring a comprehensive understanding of their condition. This thorough documentation, which includes what are soap notes in the medical field, is crucial in addressing the fragmentation often seen in healthcare systems, enhancing communication among providers.
-
Objective: Here, observable and measurable data come into play, such as vital signs, physical examination findings, and diagnostic test results. This factual basis is essential for clinical decision-making, ensuring assessments are grounded in concrete evidence. For example, noting an individual's elevated blood pressure alongside their reported symptoms can aid in diagnosing hypertension. It's important to avoid personal judgments and terms like 'good' or 'bad' in this section to maintain objectivity when understanding what are soap notes in the medical field. Accurate documentation, such as what are soap notes in the medical field, helps reduce redundancies and improve care coordination.
-
Assessment: In this section, the clinician synthesizes subjective and objective information to formulate a diagnosis or clinical impression. This process showcases the provider's clinical reasoning and judgment, facilitating a comprehensive understanding of the individual's condition. For example, a clinician might conclude that a patient with anxiety symptoms and an elevated heart rate is experiencing anxiety-related physiological responses. However, one limitation of the SOAP note format is its inability to document changes over time, which can be crucial in ongoing assessments. Utilizing AI tools can assist in monitoring these changes more efficiently, ultimately improving service quality.
-
Plan: The final component outlines the proposed course of action, including treatment options, referrals, and follow-up appointments. It serves as a guide for the individual's treatment moving forward, ensuring all team members are synchronized on the next steps. For instance, a plan may suggest therapy sessions combined with medication management to address the individual's anxiety. By incorporating generative AI into this process, healthcare providers can simplify administrative tasks related to care planning, allowing for greater emphasis on client interactions.
Together, these components create a comprehensive view of the individual's health status, which relates to what are soap notes in the medical field, enhancing communication among healthcare providers and effectively guiding clinical decision-making. Understanding what are soap notes in the medical field is crucial for improving provider-to-provider communication and minimizing unnecessary tests, ultimately leading to better outcomes for individuals. By addressing the challenges of fragmented healthcare systems and leveraging AI to enhance documentation and communication, we can transform the entire process, boosting both efficiency and service quality.

Illustrate Practical Applications of SOAP Notes in Healthcare
Structured notes play a vital role in various healthcare fields, including primary healthcare, mental health, and rehabilitation. Have you ever felt overwhelmed by the documentation demands in your practice? In a primary care setting, for instance, a clinician might record an individual’s hypertension management using a structured format. The Subjective section captures the individual’s report of headaches and medication adherence, while the Objective section presents vital signs, like blood pressure readings and relevant lab results. The Assessment could indicate poorly controlled hypertension, leading to a Plan that involves medication adjustments and scheduling a follow-up visit.
In mental wellness care, structured records can effectively capture client interactions. Imagine a therapist recording a client’s feelings of anxiety in the Subjective section, while the Objective section contains observations of the client’s demeanor during the session. The Assessment might reflect the severity of the anxiety, and the Plan could outline therapeutic interventions and follow-up appointments. This organized approach not only streamlines documentation but also enhances the therapeutic relationship.
Case studies illustrate what are SOAP notes in the medical field and demonstrate their effectiveness in improving outcomes for individuals. One study highlighted how organized documentation led to better communication among healthcare providers, ensuring that all team members had access to consistent and comprehensive information about individuals. This organization enhances the quality of service and serves as a legal record of the clinician’s decision-making process, protecting both the provider and the patient in potential disputes.
Furthermore, restructuring the documentation format to APSO (Assessment, Plan, Subjective, Objective) has proven to be a helpful method for enhancing communication and usability in clinical environments. Experts agree that what are SOAP notes in the medical field improves clinical reasoning and continuity of service. By clearly delineating subjective and objective data, assessments, and plans, healthcare providers can refine their documentation practices, ultimately leading to better patient care and outcomes.
However, it’s essential to recognize the limitations of the SOAP note format, particularly its inability to document changes over time, which can be crucial in evolving clinical situations. How can we address these challenges together? By embracing structured documentation, we can alleviate some of the administrative burdens and focus more on what truly matters—providing compassionate care to our patients.

Conclusion
Structured documentation, especially SOAP notes, plays a crucial role in enhancing patient care and fostering communication among healthcare providers. Have you ever felt overwhelmed by the complexities of patient interactions? By breaking these interactions into four clear components—Subjective, Objective, Assessment, and Plan—clinicians can organize information effectively. This leads to improved diagnosis, treatment strategies, and ultimately, better patient outcomes. Such a systematic approach not only reduces the risk of errors in medical records but also nurtures a collaborative healthcare environment.
Throughout this article, we’ve seen how SOAP notes help reduce documentation inconsistencies, enhance clinical reasoning, and facilitate efficient care coordination. Imagine how much more time healthcare professionals could dedicate to direct patient care if administrative tasks were streamlined. The integration of generative AI into the documentation process is a step in that direction, allowing for a more focused approach to patient needs. Historically, structured documentation has evolved significantly, adapting to technological advancements while staying true to its core purpose: improving patient outcomes.
The importance of adopting SOAP notes in healthcare is immense. As the medical field continues to advance, embracing structured documentation and leveraging AI tools can truly transform clinical practices. This ensures that patients receive the highest quality of care. By understanding and implementing SOAP notes effectively, healthcare providers can contribute to a more organized, efficient, and compassionate healthcare system. This, in turn, enhances the patient experience and outcomes.
Key Benefits of SOAP Notes:
- Reduces documentation inconsistencies
- Improves clinical reasoning
- Facilitates efficient care coordination
By taking these steps, you can help create a more supportive environment for both patients and providers. Let’s work together to embrace these tools and ensure that every patient receives the compassionate care they deserve.




