Introduction
In the demanding world of healthcare, providers often face emotional challenges that can weigh heavily on their ability to deliver quality patient care. The structured approach to medical documentation, known as SOAP, offers a beacon of hope amidst the chaos. By breaking down clinical notes into four key components - Subjective, Objective, Assessment, and Plan - healthcare professionals can not only enhance communication but also streamline workflows, ultimately leading to improved patient outcomes.
However, as the complexities of patient interactions grow, many practitioners find themselves grappling with documentation overload. This burden can detract from the time and attention they wish to devote to their patients. How can we navigate these challenges while ensuring that our documentation remains effective and compassionate?
Exploring the significance of SOAP notes reveals their historical roots and transformative potential in modern clinical practice. By embracing this framework, healthcare providers can foster a more nurturing environment for their patients. Here are some key benefits of implementing SOAP notes:
- Enhanced Communication: Clear documentation fosters better collaboration among healthcare teams.
- Streamlined Workflows: A structured approach saves time and reduces stress.
- Improved Patient Outcomes: Focused assessments lead to more effective care plans.
As we delve deeper into the world of SOAP notes, let’s reflect on how this framework can alleviate some of the administrative burdens we face. Together, we can create a more supportive and effective healthcare environment.
Defining SOAP Notes: Purpose and Structure
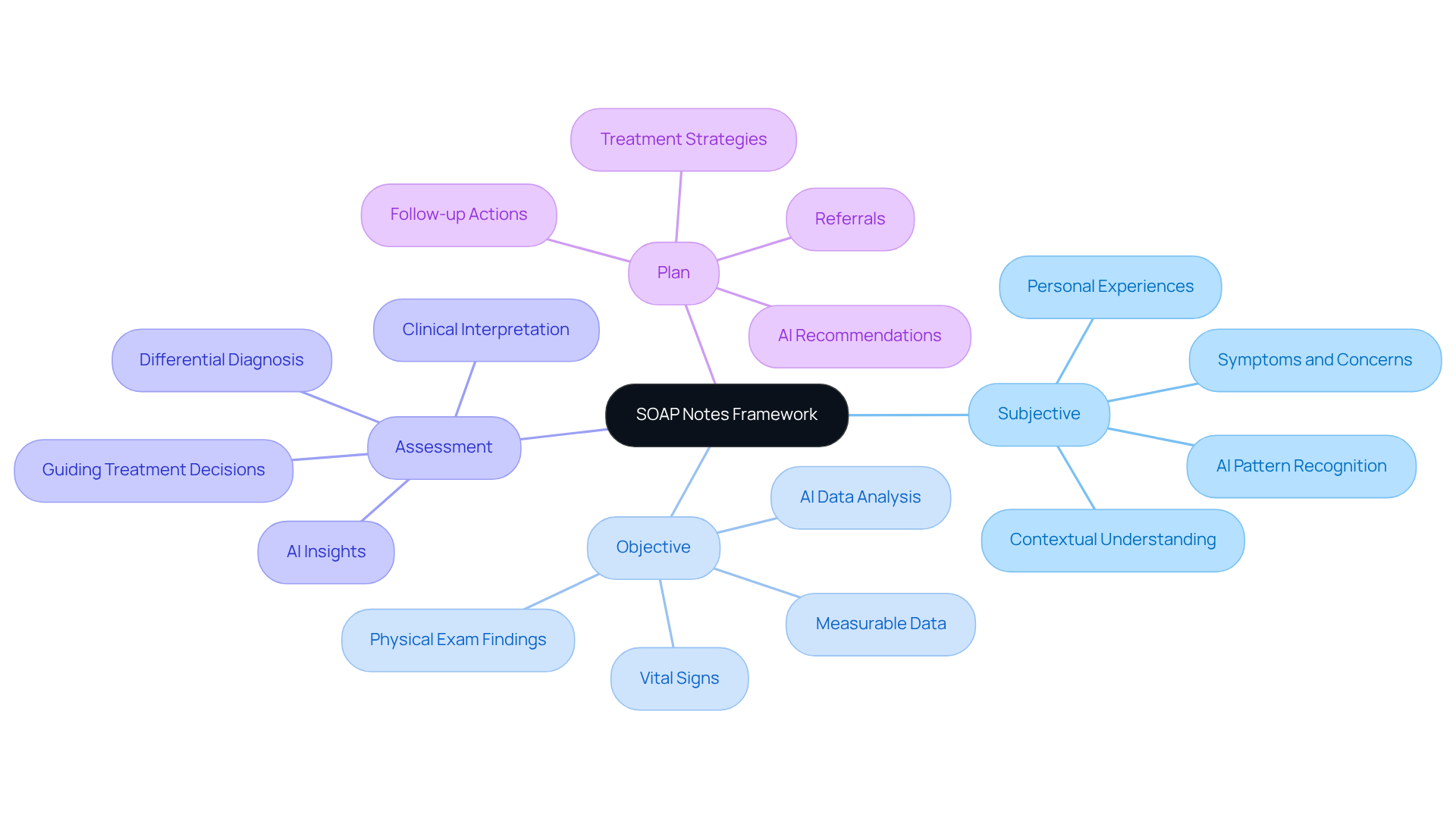
Structured notes represent a vital documentation approach that can significantly ease the burdens faced by healthcare professionals. Have you ever felt overwhelmed by the sheer volume of client interactions? The medical term soap, which stands for Subjective, Objective, Assessment, and Plan, provides a clear framework that not only organizes information but also enhances the quality of care delivered.
-
Subjective: This section captures the individual's personal experiences, symptoms, and concerns. It’s essential for understanding the context of their health. For instance, when a patient reports fatigue and significant weight loss, these insights are crucial for the clinician's evaluation. Imagine how AI algorithms can analyze this subjective data to identify patterns that may inform diagnosis and treatment planning.
-
Objective: Here, measurable data such as vital signs, physical examination findings, and laboratory results come into play. This objective information is critical for distinguishing between reported symptoms and observable signs, aiding in accurate diagnosis. Picture how AI can enhance this process by quickly analyzing large datasets to highlight significant findings, allowing you to focus more on patient care.
-
Assessment: This component synthesizes both subjective and objective data to formulate a clinical interpretation. It often includes a differential diagnosis, ranking possible conditions based on likelihood. This is essential for guiding treatment decisions. How might AI assist in this area? By providing insights based on historical data and trends, it can support your clinical reasoning.
-
Plan: The final section outlines proposed treatment strategies, follow-up actions, and necessary referrals. A well-organized strategy ensures continuity of care and offers clear guidance for both the patient and other medical professionals. Imagine AI recommending evidence-based treatment options tailored to each individual's unique profile, making your job easier and more effective.
The organized format of clinical notes not only enhances clarity but also fosters better communication among medical professionals. Research shows that efficient documentation, especially when enhanced by AI insights, can lead to improved healthcare outcomes. By mastering this structured format known as the medical term soap and leveraging advanced algorithms, you can elevate your clinical reasoning and ultimately provide higher-quality care to your patients.
So, how can you start implementing these strategies today? Embrace the structured approach and consider how AI can be a partner in your practice, helping you focus on what truly matters-your patients.
Historical Development of SOAP Notes in Healthcare
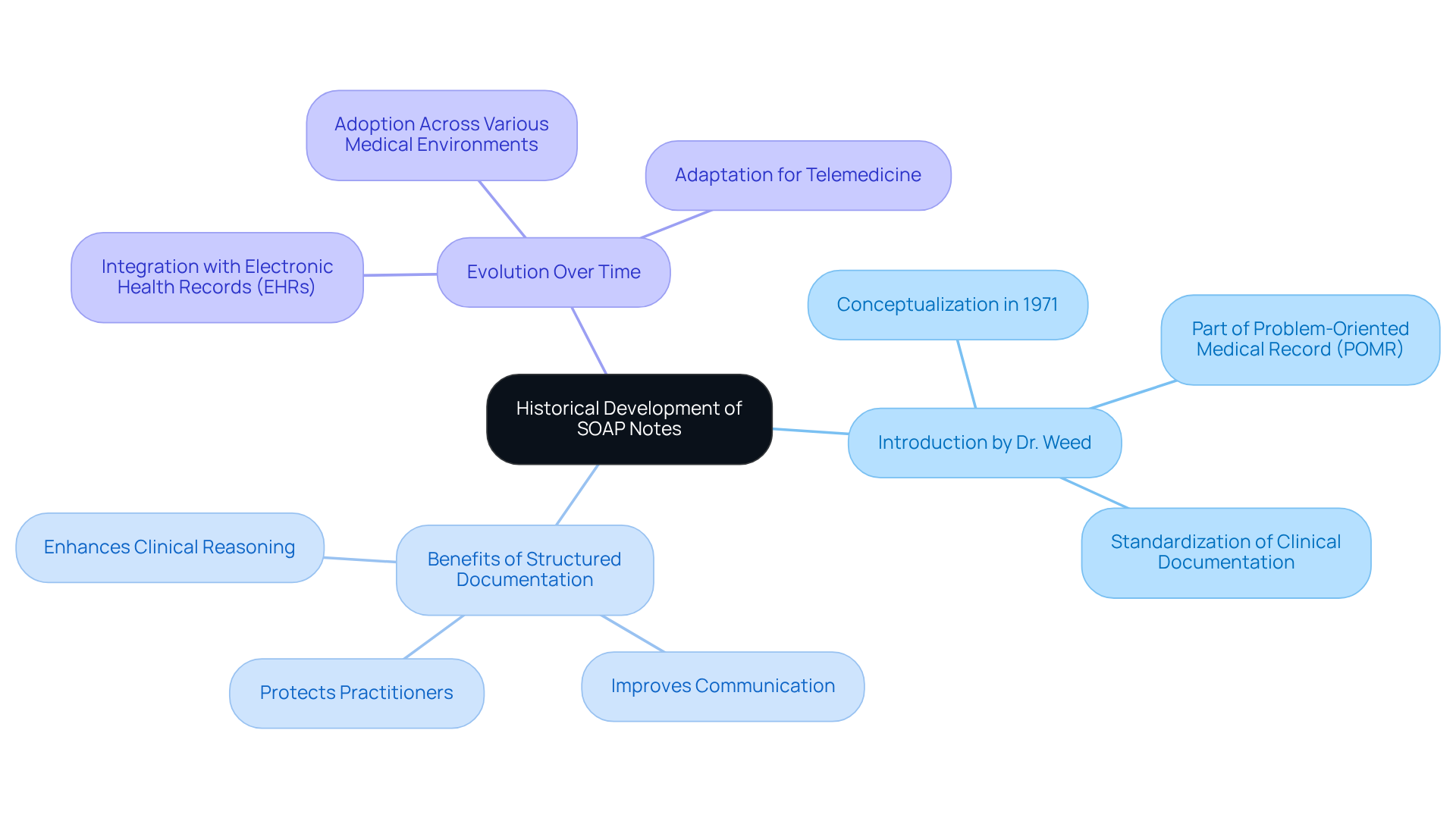
In 1971, Dr. Lawrence Weed, a compassionate doctor and medical instructor, introduced a structured format as part of the Problem-Oriented Medical Record (POMR) system. He recognized the emotional challenges healthcare providers face, particularly the need for a standardized approach to recording individual information. This approach not only enhances clinical reasoning but also improves patient care.
The medical term soap refers to SOAP records, which emerged from the POMR, transforming medical documentation by providing a clear structure for organizing individual data. This innovation has gained broad acceptance across various medical environments. In our fragmented healthcare systems, structured documentation is vital for improving communication and coordination among providers. It addresses the disjointed care that often occurs when individual information is isolated.
Regulatory concerns, such as HIPAA, can further complicate communication, creating barriers between individuals and providers. Over the years, clinical documentation has evolved alongside advancements in electronic health records (EHRs), simplifying processes and enhancing data accessibility. This evolution underscores the importance of documentation in clinical practice, ensuring it remains an essential resource for effective care and communication among medical professionals.
Clinical records also serve as an official account of individual interactions, providing crucial documentation that can protect medical practitioners during legal examinations or malpractice allegations. Dr. Weed's legacy continues to influence the standards for medical documentation, particularly the medical term soap, highlighting the ongoing importance of structured records in today’s healthcare environment.
Key Benefits of Structured Documentation:
- Enhances clinical reasoning and patient care.
- Improves communication and coordination among providers.
- Protects practitioners during legal scrutiny.
As we navigate the complexities of healthcare, let’s embrace structured documentation as a means to foster better care and support for both providers and patients.
Key Components of SOAP Notes: Subjective, Objective, Assessment, and Plan
The SOAP note serves as a vital tool in healthcare, structured to support both providers and patients through its four essential components:
-
Subjective: This section captures the patient's perspective, detailing their symptoms, feelings, and concerns. It often includes direct quotes, offering valuable insights into their experience. For example, when a patient says, 'I feel anxious and have trouble sleeping,' it highlights their emotional state and invites further inquiry. How often do we overlook these crucial expressions?
-
Objective: Here, medical providers document measurable data, such as vital signs and results from diagnostic tests. This information is crucial for forming an accurate clinical picture. With AI algorithms, this data can be analyzed more efficiently, allowing for quicker identification of patterns that might be missed by human observation. This not only enhances the precision of the clinical picture but also lightens the administrative load on providers, enabling them to focus more on patient care.
-
Assessment: This component synthesizes the subjective and objective data to provide a clinical interpretation. AI can assist by offering insights derived from extensive medical data, leading to more accurate diagnoses and assessments of the patient's progress. By reducing the time spent on data analysis, AI helps alleviate the administrative burden that often contributes to physician burnout. Isn’t it time we prioritize our well-being?
-
Plan: The final section outlines the proposed treatment strategy, including medications, therapies, referrals, and follow-up appointments. By utilizing AI, providers can develop more customized treatment strategies based on thorough data analysis, ensuring a roadmap for care that is tailored to each individual's needs.
By effectively employing the medical term SOAP format alongside AI advancements, healthcare professionals can enhance communication, ensure thorough documentation, and promote improved care. Let’s embrace these tools to foster a more compassionate healthcare environment.

The Importance of SOAP Notes in Clinical Practice
In clinical practice, the medical term SOAP notes are essential, ensuring that individual information is documented clearly and organized. Have you ever felt overwhelmed by the sheer volume of information you need to manage? This framework not only improves communication among medical professionals but also promotes continuity of care as patients transition between various providers or environments.
With innovative AI solutions like CosmaNeura's Agentic Platform, the documentation process can be optimized even further. Imagine reducing administrative burdens and having more time to focus on what truly matters-your patients. Clinical records also serve as legal documents, protecting both patients and providers in case of conflicts or evaluations. By providing a detailed account of client interactions, these records help clinicians make informed decisions, track client progress, and ultimately enhance health outcomes.
Moreover, the standardized format of the medical term SOAP notes is invaluable for training new medical professionals. It ensures they adhere to best practices in documentation while leveraging generative AI to improve efficiency and accessibility in service delivery.
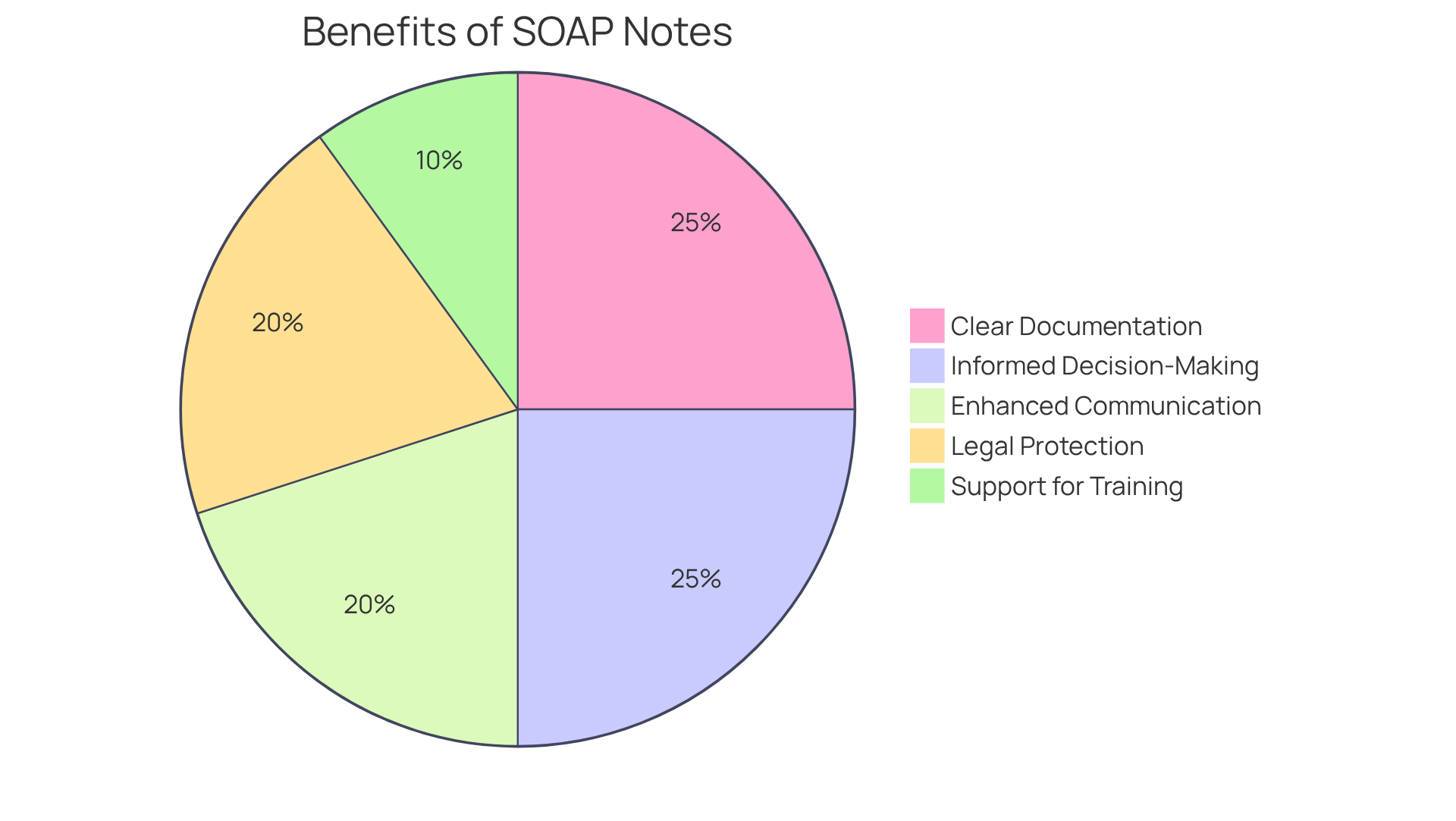
Key Benefits of SOAP Notes:
- Clear and organized documentation
- Enhanced communication among providers
- Legal protection for both parties
- Informed decision-making and progress tracking
- Support for training new professionals
In a world where every detail matters, embracing effective documentation practices can transform patient care. Let’s work together to ensure that every interaction is meaningful and impactful.
Challenges and Best Practices in Writing SOAP Notes
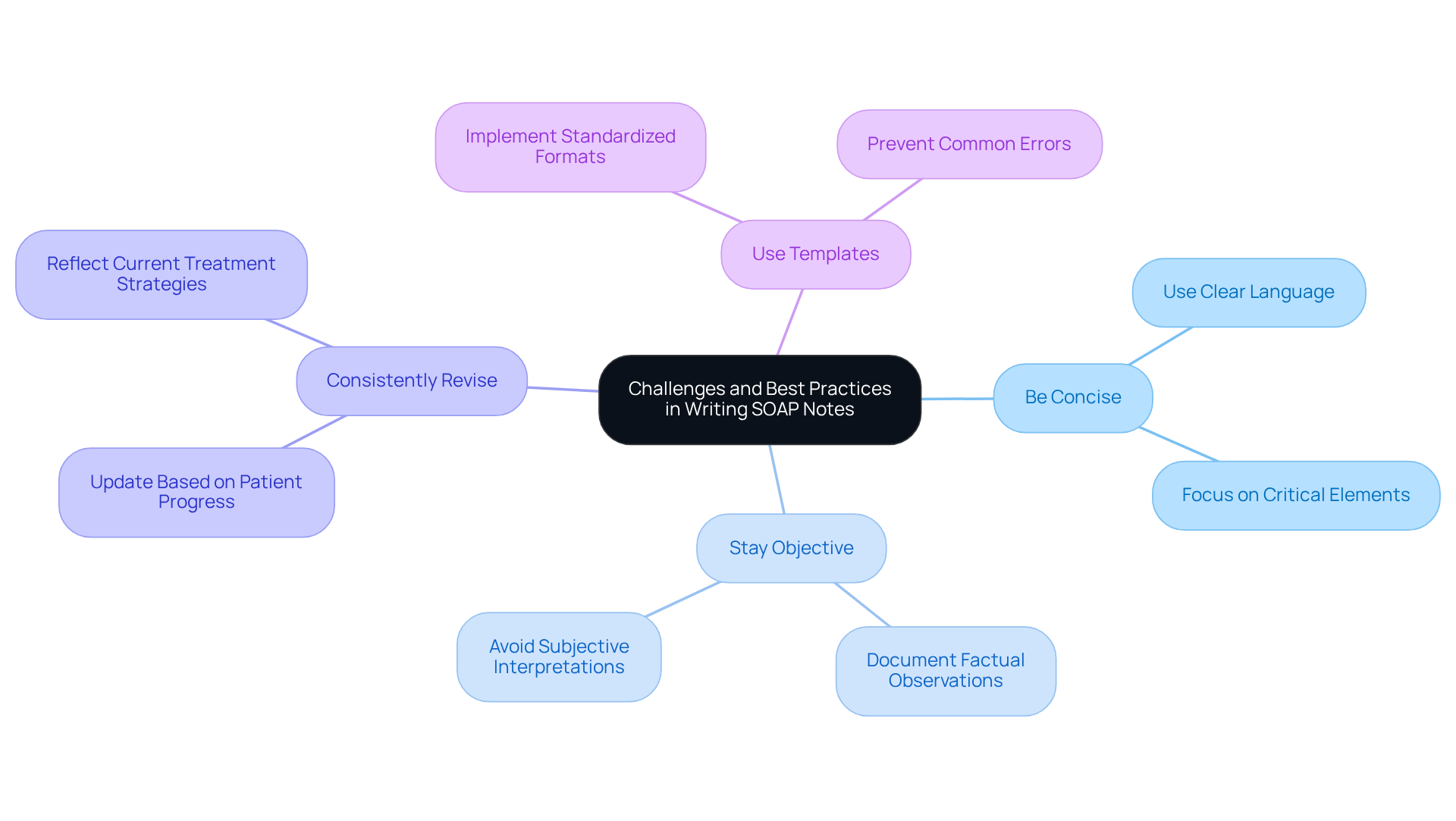
Creating effective clinical records is essential for maintaining high-quality documentation for individuals. Yet, many medical professionals encounter significant challenges in this area. Have you ever felt overwhelmed by the demands of documentation? Common pitfalls include ambiguous language, unnecessary detail, and the failure to revise records based on patient progress.
To enhance the quality and effectiveness of SOAP notes, consider these best practices:
- Be Concise: Use clear and direct language to convey essential information without unnecessary elaboration. This approach helps keep the focus on the critical elements of care.
- Stay Objective: In the Objective section, concentrate on factual observations, steering clear of subjective interpretations. This ensures that your documentation remains grounded in measurable data, such as vital signs and physical exam findings.
- Consistently Revise: Your documentation should reflect the most current client information and treatment strategies. Regular updates based on ongoing assessments are vital for accurate documentation and continuity of care.
- Use Templates: Implementing standardized templates can streamline the documentation process, ensuring consistency and thoroughness across records. Templates can also help prevent common errors, such as omitting critical information or using non-standard abbreviations.
By following these best practices, you can significantly enhance the efficiency of your documentation. This not only improves care for individuals but also fosters better communication among healthcare teams. For instance, a study published in Digital Medicine revealed that utilizing structured templates led to improved documentation quality scores and reduced consultation times by over 26%. This highlights the tangible benefits of efficient note-taking practices.
Moreover, the medical term SOAP format, introduced by Lawrence Weed nearly 50 years ago, remains a foundational element in clinical documentation, underscoring the importance of clarity and structure in patient records. Additionally, leveraging AI tools can assist in creating actionable plans and ensuring compliance, further enhancing the documentation process.
Remember, you’re not alone in facing these challenges. By embracing these strategies, you can make a meaningful difference in your practice and the lives of your patients.
Conclusion
In the demanding world of healthcare, the medical term SOAP represents more than just a documentation method; it embodies a structured approach that is vital for enhancing patient care and fostering communication among professionals. By organizing clinical notes into Subjective, Objective, Assessment, and Plan categories, providers can streamline their documentation process, ultimately leading to better health outcomes.
Have you ever felt overwhelmed by the sheer volume of paperwork? The emotional toll of administrative burdens can weigh heavily on healthcare providers, impacting the quality of care delivered to patients. Each component of SOAP notes plays a crucial role in alleviating this stress. The Subjective section captures the patient's personal experiences, while the Objective section provides measurable data. The Assessment synthesizes these insights to guide clinical interpretations, and the Plan outlines actionable treatment strategies. Together, these elements foster clarity, enhance communication, and protect both patients and practitioners in legal contexts.
To tackle the challenges of clinical documentation, consider adopting best practices and leveraging advancements in technology, such as AI. These tools can significantly improve the efficiency and effectiveness of SOAP notes. By embracing structured documentation techniques, healthcare professionals can not only lighten their administrative load but also devote more time to delivering compassionate, high-quality care to their patients.
Key Solutions:
- Implement best practices for documentation.
- Utilize technology to streamline processes.
- Focus on patient-centered care.
The journey toward better clinical documentation starts now. Let’s commit to making every patient interaction meaningful and impactful. Together, we can create a healthcare environment that prioritizes both efficiency and empathy.




