Overview
In the demanding world of healthcare, providers often face emotional challenges that can weigh heavily on their ability to deliver quality care. Administrative burdens can distract from what truly matters—patient interactions and outcomes. This is where SOAP notes come in, offering a structured documentation method that can ease some of that pressure.
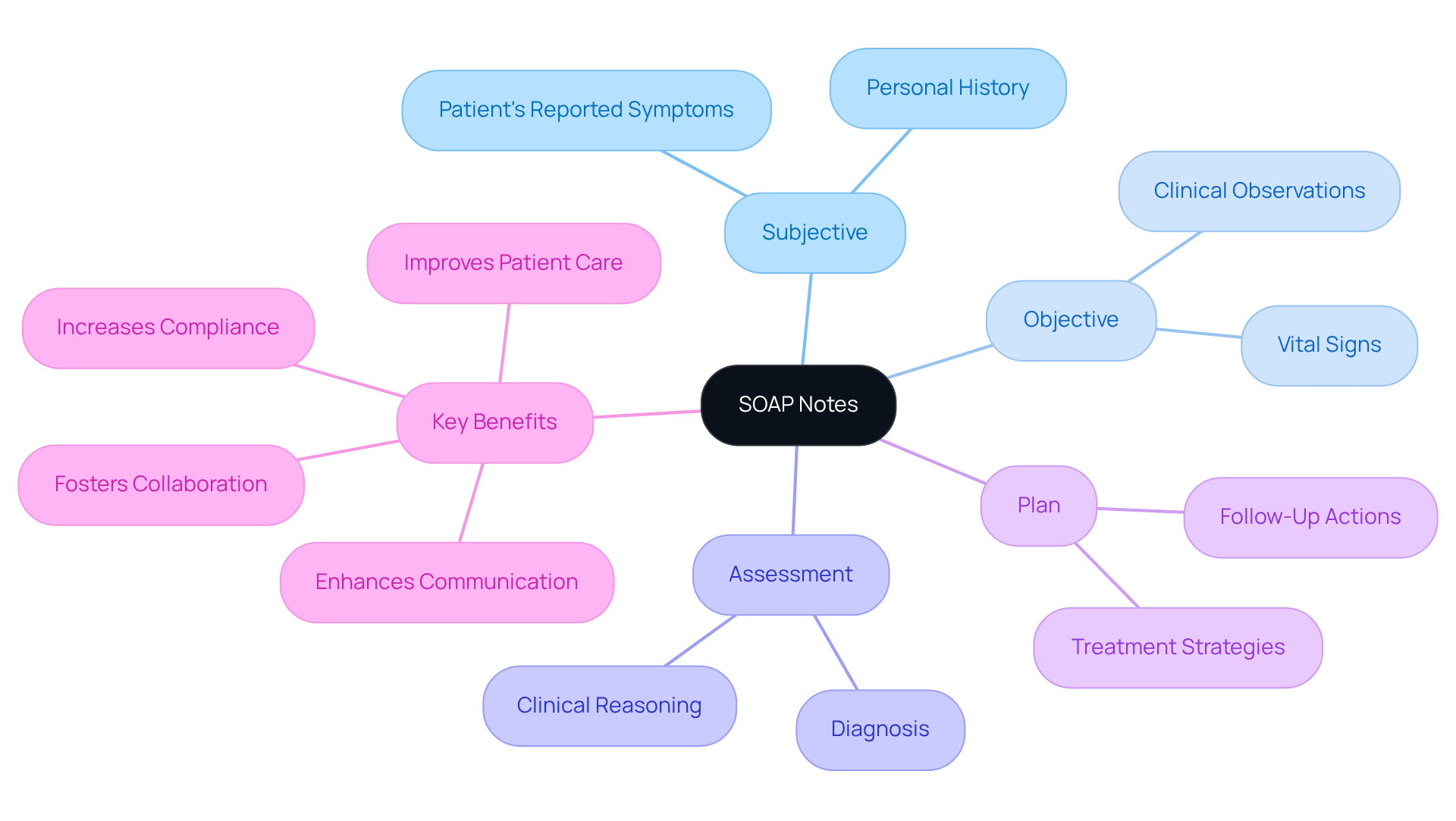
SOAP notes consist of four key components: Subjective, Objective, Assessment, and Plan. By utilizing this standardized approach, healthcare providers can enhance clinical decision-making and foster collaboration among their peers. This not only improves communication but also ensures compliance with regulations, ultimately leading to better patient outcomes.
Imagine a healthcare system where providers feel supported and empowered. With SOAP notes, you can streamline your documentation process, allowing more time for patient care. Here are some key benefits:
- Improved clinical decision-making
- Enhanced collaboration among providers
- Greater compliance with regulations
- Better patient outcomes
These benefits contribute to a more efficient healthcare system, where everyone can thrive. So, how can you start implementing SOAP notes in your practice? Consider reaching out to colleagues or exploring resources that can guide you in this transition. Together, we can create a nurturing environment that prioritizes patient care and supports healthcare providers in their vital roles.
Introduction
In the complex world of healthcare, effective communication is crucial for delivering quality patient care. Have you ever felt overwhelmed by the demands of documentation? The SOAP note framework—comprising Subjective, Objective, Assessment, and Plan—can be a lifeline for healthcare providers, simplifying documentation and fostering collaboration. Yet, the challenge persists: how can you ensure that your documentation not only meets compliance standards but also nurtures a compassionate, patient-centered approach?
This article explores the essential components of SOAP notes and offers best practices for their implementation. We’ll also discuss the ethical considerations that underpin effective clinical documentation. By addressing these aspects, we aim to support you in navigating the administrative burdens that can impact patient care.
Key Solutions:
- Streamline your documentation process with the SOAP framework.
- Foster collaboration among healthcare teams.
- Prioritize a compassionate approach in patient interactions.
Together, let’s delve into how you can enhance your documentation practices while keeping the focus on what truly matters: your patients.
Understanding SOAP Notes: Definition and Purpose
In the demanding world of healthcare, providers often face emotional challenges that can impact patient care. This documentation method, known as SOAP—Subjective, Objective, Assessment, and Plan—provides a standardized way to record encounters, which is what soap notes explained aims to achieve in alleviating some of these burdens. By organizing clinical information systematically, it enables healthcare providers to monitor individual progress effectively over time.
The main goal of these records is to enhance communication among providers. When all relevant information about individuals is readily available and clearly understood, it fosters a more supportive environment for both patients and providers. Clear records and structured observations not only assist in clinical decision-making but also significantly elevate the standard of care.
In fragmented healthcare systems, where care is often divided among various providers, the clarity provided by structured documentation becomes even more crucial. It helps bridge communication gaps, ensuring continuity of care and encouraging collaborative treatment approaches. Regulatory issues, such as HIPAA, can complicate communication, making clinical documentation vital for preserving safety and privacy.
Consider this: a study found that adopting organized documentation practices led to a compliance increase from 38.2% to 87.2%. This highlights how structured records can improve clinical precision and outcomes. Healthcare professionals emphasize that using standardized forms not only builds credibility but also facilitates the exchange of treatment information.
The transparency offered by structured documentation is essential in avoiding miscommunication, especially in environments with multiple providers. This approach addresses the challenges posed by disjointed healthcare systems. Furthermore, the concept of soap notes explained can enhance the effectiveness of technology, transforming healthcare delivery and enriching interactions with individuals.
Key Benefits of Structured Documentation:
- Enhances communication among providers
- Improves patient care and outcomes
- Increases compliance and clinical precision
- Fosters collaboration in treatment approaches
By embracing structured documentation, healthcare providers can navigate the complexities of their roles with greater ease and confidence. Let’s work together to create a more connected and compassionate healthcare environment.
Components of SOAP Notes: Subjective, Objective, Assessment, and Plan
-
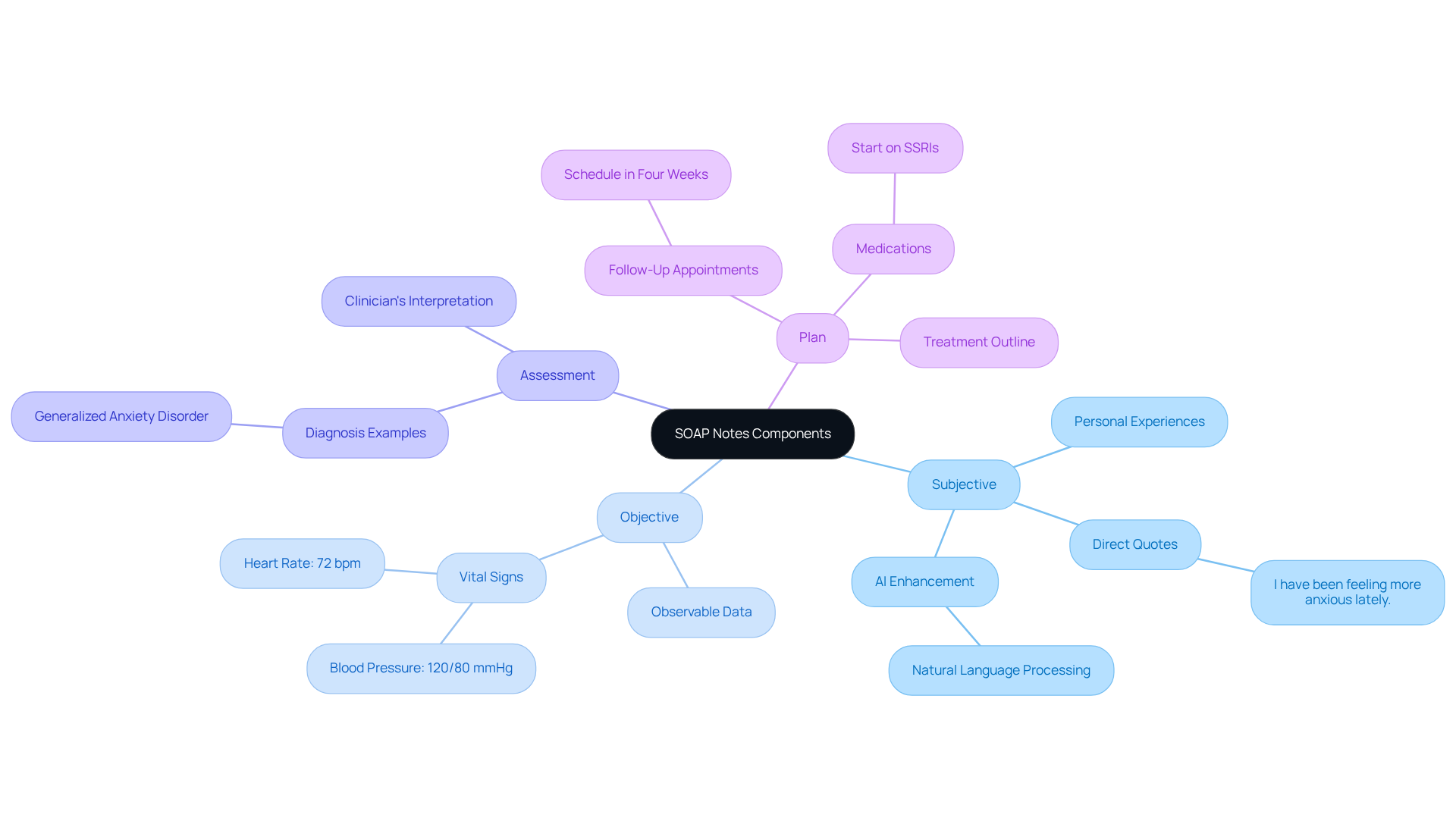
Subjective: This section captures the individual's personal experiences, feelings, and concerns regarding their health. It includes direct quotes from the individual and any relevant history they share. For example, someone might say, "I have been feeling more anxious lately." This not only conveys their emotional state but also sets the stage for further evaluation. By leveraging generative AI tools, like natural language processing applications, healthcare providers can enhance this process, making interactions more meaningful and tailored. AI can streamline the documentation of these subjective experiences, allowing clinicians to focus more on engaging with clients and less on administrative tasks. This shift ultimately elevates the quality of care delivered.
-
Objective: In this part, the clinician documents observable and measurable data, such as vital signs, physical examination findings, and diagnostic test results. For instance, a clinician might note, "Blood pressure: 120/80 mmHg; Heart rate: 72 bpm," providing a clear snapshot of the individual's physical condition during the visit.
-
Assessment: This component involves the clinician's interpretation of both subjective and objective data. It includes a diagnosis or a list of potential diagnoses based on the gathered information. An example might read, "Patient exhibits symptoms consistent with generalized anxiety disorder," reflecting a thoughtful synthesis of the collected data.
-
Plan: The final section outlines the proposed treatment plan, including medications, referrals, or follow-up appointments. An example could be, "Start the individual on SSRIs and schedule a follow-up in four weeks to assess progress," ensuring they understand the next steps in their care journey.
Including client quotes in documentation not only enriches the clinical narrative but also underscores the importance of their involvement in their own care. This comprehensive approach to documentation, as soap notes explained, enhances the quality of care and fosters a more patient-centered healthcare environment.
Writing Effective SOAP Notes: Best Practices and Examples
-
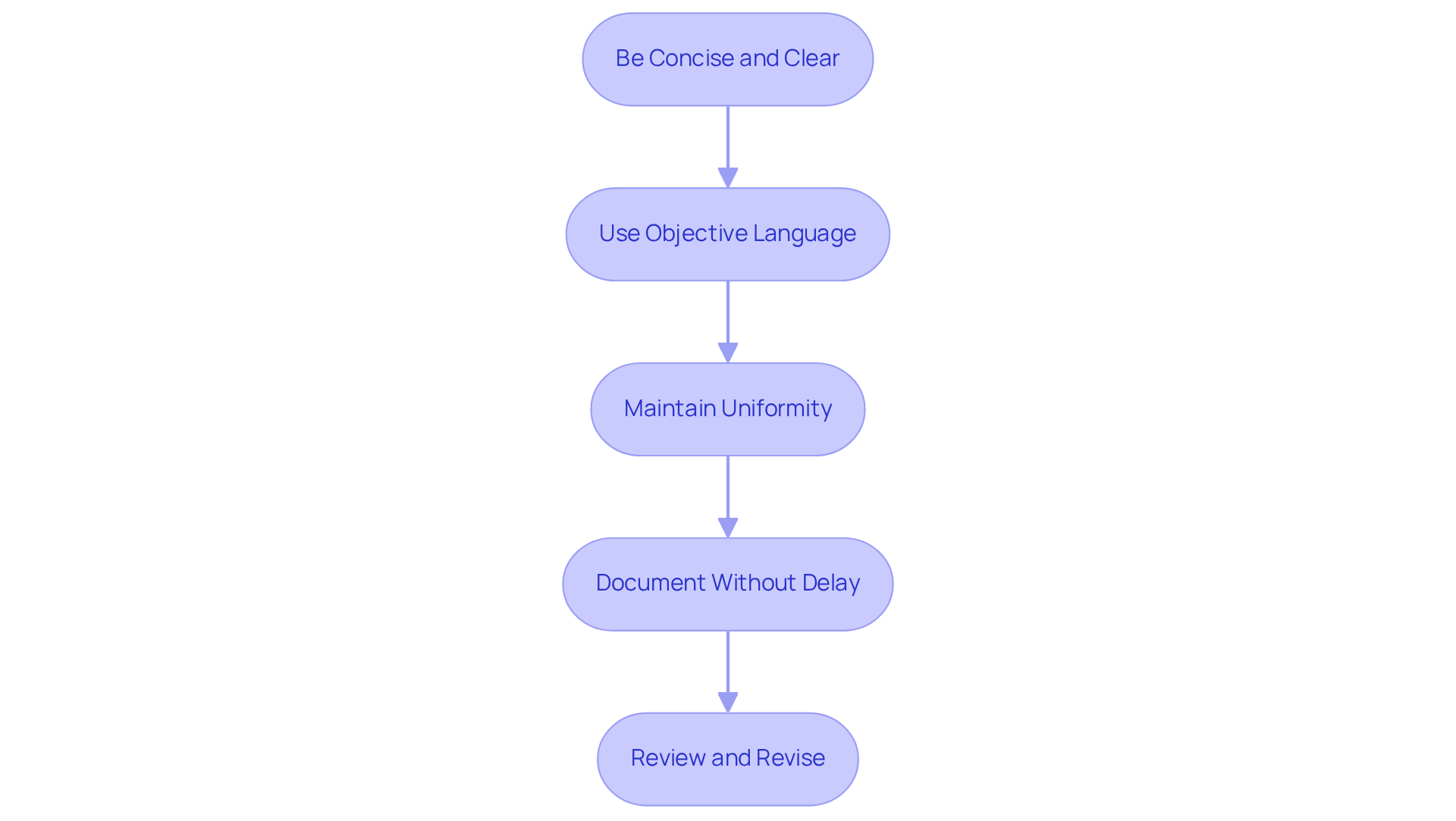
Be Concise and Clear: It's essential to use straightforward language and steer clear of jargon. This approach not only enhances readability but also ensures that each section is succinct yet comprehensive enough to convey the vital information effectively.
-
Use Objective Language: In the Subjective section, whenever possible, quote the individual directly. For the Objective section, rely on measurable data rather than personal interpretations. This practice helps maintain professionalism and accuracy. As Blake Bauer wisely states, "Your documentation should represent what you notice and what the patient conveys—not your interpretations or assumptions."
-
Maintain Uniformity: Following a reliable format for all clinical records is crucial. This consistency facilitates easier review and understanding by other healthcare providers, ensuring that documentation remains both reliable and accessible.
-
Document Without Delay: Compose clinical summaries right after your interaction with the individual. This practice guarantees precision and thoroughness. Avoid creating written messages during the session to keep your focus on the patient and their needs, which is essential for effective care.
-
Review and Revise: Regularly evaluate your documentation for clarity and completeness. Seek constructive feedback from colleagues to enhance your writing skills. For instance, a well-structured SOAP note might include:
- Subjective: "Patient reports increased anxiety, especially in social situations."
- Objective: "Patient appears anxious, with a heart rate of 85 bpm, which soap notes explained."
- Assessment: "Soap notes explained for generalized anxiety disorder."
- Plan: "Refer to a therapist and consider medication management as soap notes explained."
By adhering to these best practices, healthcare providers can significantly improve the quality of their records, ensuring they meet ethical standards and support effective patient care. Remember, the structured format was created by Lawrence Weed in the 1950s, and following this framework is vital for ensuring clarity and consistency. Additionally, safe storage and adherence to applicable regulations are essential for ethical documentation practices, as is understanding the potential legal consequences of clinical records.
Compliance and Ethical Considerations in SOAP Note Documentation
-
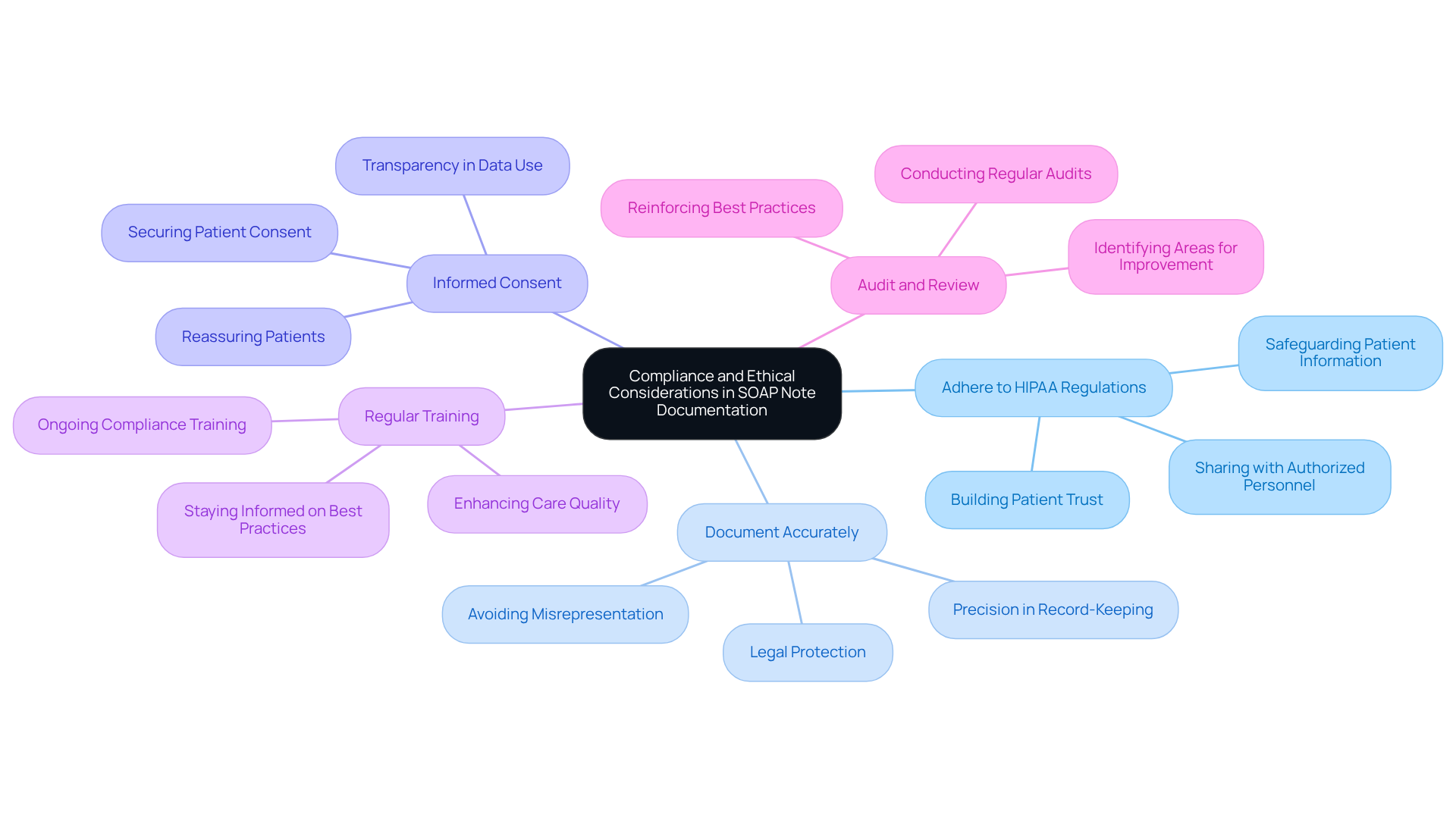
Adhere to HIPAA Regulations: Safeguarding patient information is not just a requirement; it’s a commitment to your patients’ trust. Ensure that all details documented in soap notes explained are kept confidential and secure. Share them only with authorized personnel to uphold HIPAA standards. How can we ensure our patients feel safe with us?
-
Document Accurately: Precision in record-keeping is crucial for both your practice and your patients. Avoid exaggeration or misrepresentation of client information. Remember, accurate records are essential for legal protection and providing quality care. Legal specialists remind us that "records are vital... cases will be determined based on the evidence, and not necessarily the truth." This makes accuracy not just important, but essential.
-
Informed Consent: Always secure informed consent from patients before documenting sensitive information. Clearly explain how their data will be utilized and stored. This transparency fosters trust in the provider-patient relationship. Given that 60% of organizations express doubts about their ability to pass a HIPAA audit, this step is crucial for compliance. How can we reassure our patients about their data?
-
Regular Training: Engage in ongoing training on compliance and ethical standards in healthcare records. With 70% of organizations having faced incidents in the past year, staying informed about best practices and legal requirements is vital for maintaining high-quality documentation. This not only protects you but also enhances the care you provide.
-
Audit and Review: Conduct regular audits to ensure compliance with legal and ethical standards, as soap notes explained are crucial in this process. The OCR initiated 220 audits and 9,136 investigations concerning HIPAA compliance in 2020, underscoring the importance of this proactive approach. Regular audits help identify areas for improvement and reinforce adherence to best practices, ultimately enhancing patient trust and care quality. What steps can we take today to improve our documentation practices?
Conclusion
The structured approach of SOAP notes—Subjective, Objective, Assessment, and Plan—serves as a vital tool in healthcare documentation. It enhances communication and continuity of care among providers, addressing the emotional challenges healthcare professionals face daily. By utilizing this standardized method, healthcare professionals can effectively capture and share important patient information, fostering a more supportive environment for both patients and providers.
Have you ever felt overwhelmed by administrative tasks? You’re not alone. The article highlights the numerous benefits of structured documentation, including improved patient care, increased compliance, and enhanced clinical precision. By focusing on best practices—like being concise, using objective language, and maintaining uniformity—we can ensure clarity and professionalism in the documentation process. Moreover, the discussion on compliance and ethical considerations reinforces the necessity of safeguarding patient information and adhering to legal standards.
In conclusion, embracing SOAP notes not only streamlines healthcare documentation but also enriches the quality of care provided. By committing to best practices and prioritizing clear communication, healthcare professionals can navigate the complexities of their roles with confidence.
Key Benefits of SOAP Notes:
- Improved patient care
- Increased compliance
- Enhanced clinical precision
Taking proactive steps today to refine documentation practices will not only enhance individual patient interactions but also contribute to a more connected and compassionate healthcare system overall. Let’s work together to create a nurturing environment for everyone involved.




