Overview
In the demanding world of healthcare, providers often face emotional challenges that can weigh heavily on their ability to deliver quality care. The administrative burdens, like writing SOAP notes, can feel overwhelming, detracting from the time spent with patients. How can we ease this burden and enhance patient outcomes?
Mastering the art of writing SOAP notes is essential for healthcare providers. These structured documentation formats not only streamline communication but also significantly improve patient care. By clearly identifying the four components—Subjective, Objective, Assessment, and Plan—providers can create a comprehensive picture of each patient's needs.
Here are some strategies to maintain clarity and efficiency in your documentation:
- Prioritize concise language to convey information effectively.
- Use templates to save time while ensuring all necessary details are included.
- Regularly review and update your notes to reflect the most current patient information.
By implementing these practices, you can enhance communication with your team and improve patient outcomes. Remember, every note you write is a step towards better care.
So, let’s take action together. Embrace these strategies and transform your documentation process. Your patients deserve the best, and with a little support, you can provide it.
Introduction
Mastering the art of writing SOAP notes is crucial for healthcare providers who navigate the complexities of patient care. This structured documentation format not only enhances communication among professionals but also ensures that vital patient information is accurately captured and easily accessible. Yet, many providers face emotional challenges in maintaining clarity and conciseness in their notes.
How often do administrative burdens impact your ability to provide the best care? It’s a common struggle, and it can feel overwhelming. By refining your SOAP note writing, you can meet documentation standards while also elevating the overall patient experience.
Consider these key solutions to enhance your SOAP notes:
- Focus on clarity: Use straightforward language to convey essential information.
- Be concise: Aim for brevity without sacrificing important details.
- Reflect on your notes: Regularly review them to identify areas for improvement.
By implementing these strategies, you not only improve your documentation but also foster a more supportive environment for your patients. Remember, every note you write is a step toward better care. Let’s work together to enhance our practices and ultimately enrich the patient experience.
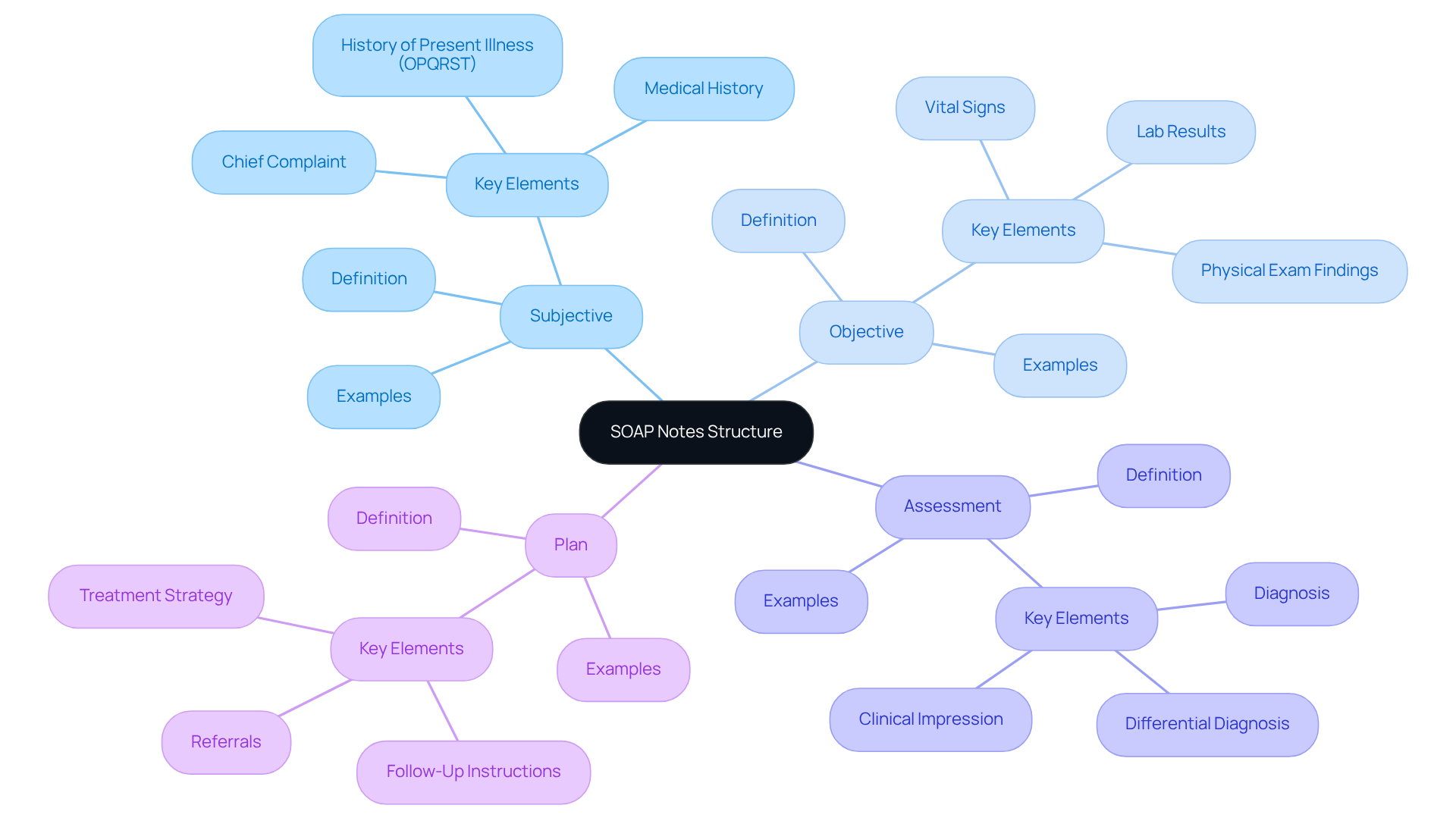
Understand the SOAP Note Format
The SOAP note format is essential in healthcare documentation, especially when it comes to writing soap notes, and it consists of four key components: Subjective, Objective, Assessment, and Plan. Each section is essential for delivering comprehensive patient care and navigating the complexities of fragmented healthcare systems.
-
Subjective: This part captures the patient's personal experiences, feelings, and symptoms as they share them, including their medical history and relevant details from the visit. Understanding this context is crucial for effective care.
-
Objective: Here, healthcare providers document measurable and observable data, such as vital signs, physical examination findings, and laboratory results. This objective data is fundamental for creating a complete clinical picture and supports the subjective reports.
-
Assessment: This section merges the subjective and objective details to provide a clinical judgment or diagnosis, reflecting the provider's interpretation of the individual's condition and guiding treatment decisions.
-
Plan: The final section outlines the proposed treatment plan, including further tests, medications, referrals, and follow-up appointments. A well-organized plan is vital for continuity of care, ensuring that all healthcare team members are aligned on the individual's treatment strategy.
As we look ahead to 2025, writing soap notes continues to be a preferred approach among healthcare professionals. Research indicates that over 70% of clinicians utilize this structure for client interactions. Its disciplined method enhances communication among providers and meets legal documentation requirements, ensuring effective and accountable care for individuals.
However, it’s important to recognize that while this format is widely used, it has limitations in capturing the temporal elements of care. This has prompted the exploration of alternative frameworks like OODA, which may better address these challenges.
Understanding and mastering writing soap notes, a structured documentation format, is crucial for healthcare professionals dedicated to providing exceptional care. How can you ensure that your documentation not only meets requirements but also enhances the patient experience? Embrace the SOAP note format and empower yourself to deliver the best care possible.

Identify the Components: Subjective, Objective, Assessment, and Plan
Writing SOAP notes can feel overwhelming for healthcare providers, particularly when they are balancing patient care with administrative tasks. Have you ever felt the weight of ensuring every detail is captured while still being present for your patients? Understanding how to effectively structure writing SOAP notes can ease that burden and enhance the quality of care you provide.
Subjective: This section captures the patient's perspective. Use open-ended questions to gather detailed information about their symptoms, concerns, and medical history. For example, asking, 'Can you describe the pain you are experiencing?' allows for a deeper understanding of the individual's condition. It’s also essential to document the individual's history of present illness using the OPQRST acronym: onset, palliating/provoking factors, quality, severity, and time course of symptoms.
Objective: Document factual data obtained through examinations and tests. This includes vital signs, lab results, and physical exam findings. For instance, stating, 'The individual's blood pressure is 120/80 mmHg,' provides concrete evidence of the person's health status. Focus on quantifiable data to aid in reassessment and monitor individual progress over time.
Assessment: Synthesize the subjective and objective data to formulate a diagnosis or clinical impression. An example could be, 'The individual presents with acute bronchitis based on symptoms and examination findings.' This section should also include a differential diagnosis, listing at least two or three possible diagnoses, which is crucial for guiding treatment decisions and ensuring comprehensive documentation.
Plan: Develop a clear and actionable strategy for the individual's care. This should encompass prescriptions, referrals, and follow-up instructions. For example, 'Prescribe albuterol inhaler and schedule a follow-up in one week' outlines the next steps in the individual's management. Additionally, recording adherence and reaction to treatment is essential for efficient clinical records.
By clearly identifying these components, you can ensure thorough and effective writing SOAP notes, which are essential for continuity of care and enhancing outcomes for individuals. Precise evaluation and recording help avoid sentinel events caused by poor communication and ensure that all pertinent individual information is documented systematically.
Consider using standardized templates and instruments to simplify the documentation process. This not only enhances uniformity but also minimizes the chance of mistakes, allowing you to focus more on what truly matters—your patients.
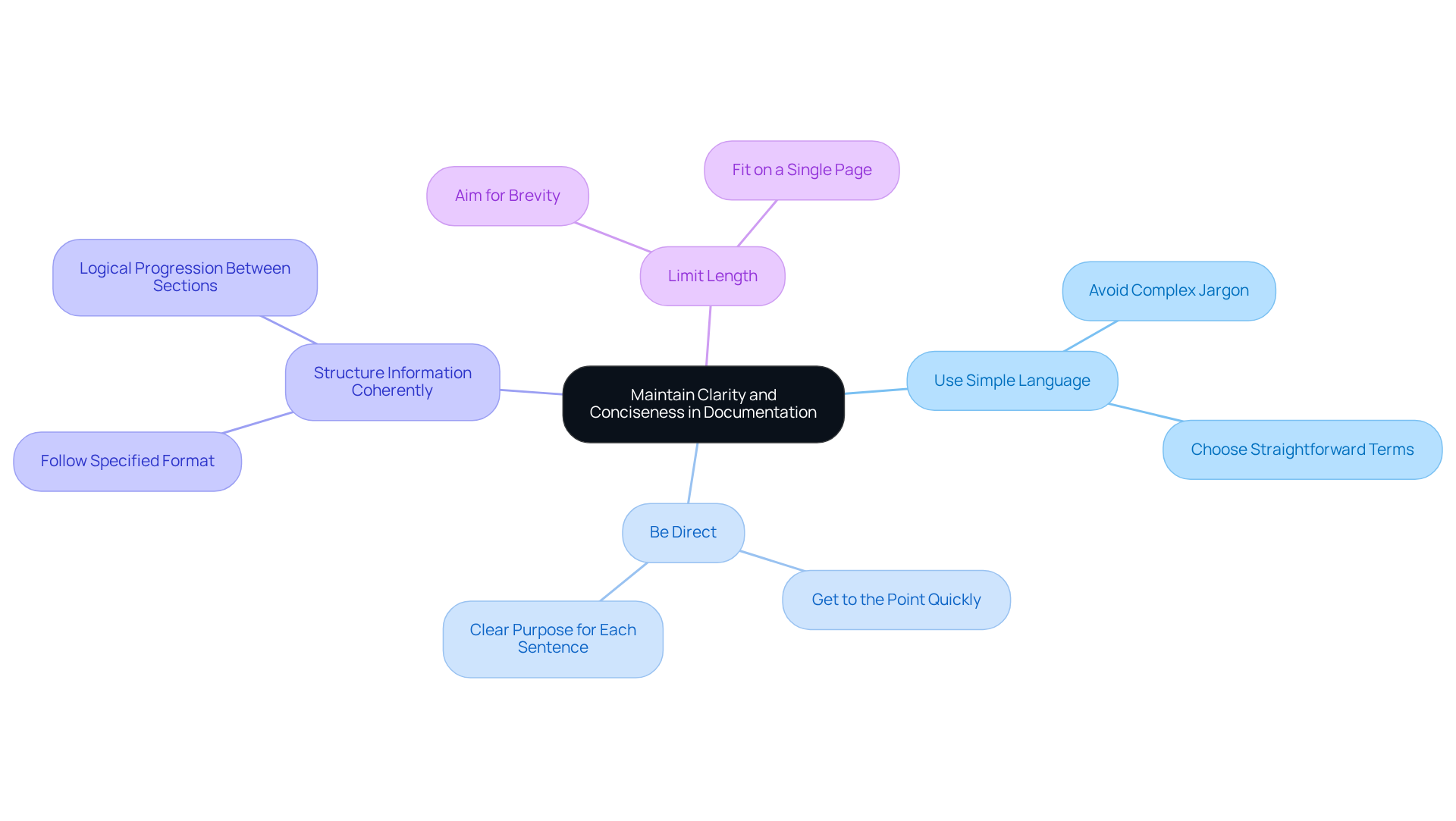
Maintain Clarity and Conciseness in Documentation
To enhance clarity and conciseness in SOAP notes, healthcare providers can adopt several supportive strategies:
- Use Simple Language: Avoid complex medical jargon that might confuse colleagues or patients. Instead, choose straightforward terms that effectively convey necessary information.
- Be Direct: Get to the point quickly. Each sentence should have a clear purpose and contribute to understanding the patient's condition.
- Structure Information Coherently: Rigorously follow the specified format, ensuring a logical progression between sections. This organization helps readers swiftly locate relevant information.
- Limit Length: Aim for brevity while retaining essential details. A useful medical report should be thorough yet concise, ideally fitting on a single page.
Statistics indicate that the typical length of SOAP records in clinical practice often exceeds one page, which can hinder effective communication. In fact, if medical errors were included in the National Center for Health Statistics' top 10 causes of death, they would rank as the fifth leading cause in the U.S. By focusing on writing SOAP notes, healthcare professionals can significantly enhance the clarity of their documentation, ultimately improving care for individuals.
Effective communication is crucial. Studies show that communication failures are a leading cause of sentinel events in healthcare settings, with between 44,000 and 98,000 people dying each year in U.S. hospitals due to medical errors. As Michelle O'Daniel noted, "When health care professionals are not communicating effectively, patient safety is at risk for several reasons: lack of critical information, misinterpretation of information, unclear orders over the telephone, and overlooked changes in status."
Therefore, by adopting these principles, healthcare teams can streamline documentation and improve collaboration through writing SOAP notes. Additionally, utilizing structured communication tools like the SBAR (Situation-Background-Assessment-Recommendation) technique can further enhance clarity and reduce the risk of errors.
It's also important to recognize that while structured formats are beneficial, they can limit the recording of changes over time, which is essential for reevaluating diagnoses and treatments. By embracing these strategies, we can work together to improve patient safety and care.
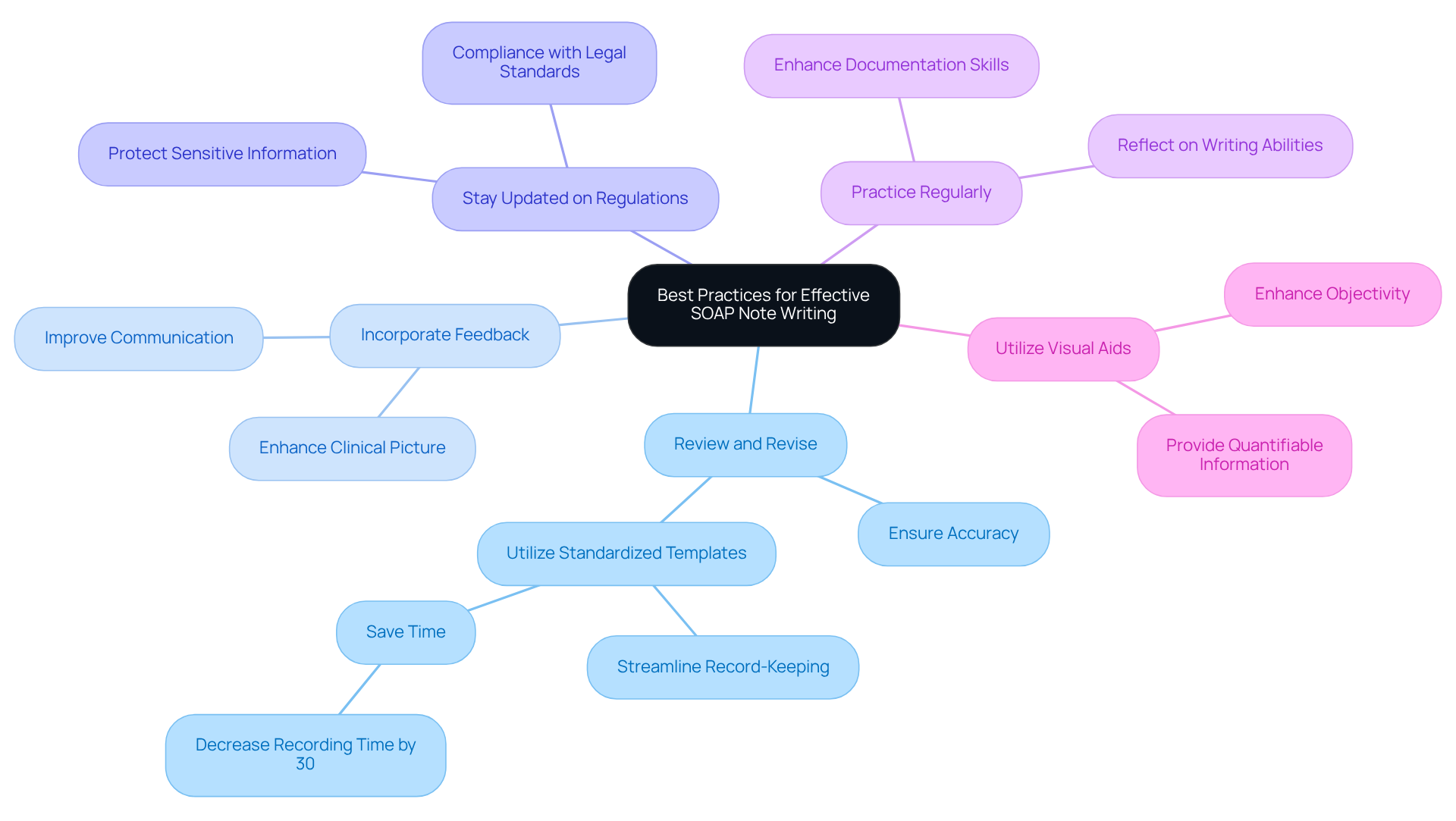
Apply Best Practices for Effective SOAP Note Writing
To enhance the effectiveness of SOAP notes, healthcare providers can adopt several supportive strategies:
-
Review and Revise: After drafting a SOAP note, take a moment to review it for accuracy and completeness. Revisions are crucial to ensure clarity and correctness, as even minor errors can significantly impact patient care. Have you ever noticed how a small detail can change the entire picture? Utilizing standardized templates for writing SOAP notes can streamline the record-keeping process, saving time and ensuring consistency across notes. Research suggests that healthcare providers who implement templates for writing SOAP notes experience enhanced efficiency in their record-keeping practices, with some studies indicating a decrease in recording time by up to 30%. Imagine what you could do with that extra time!
-
Incorporate Feedback from Individuals: Including the individual's input in the documentation enriches the clinical picture and respects their perspective. As highlighted by healthcare leaders, "Involving individuals in their care not only improves their experience but also encourages better communication and understanding of their treatment journey." This approach fosters a deeper connection and understanding, doesn’t it?
-
Stay Updated on Regulations: It’s essential to be aware of legal requirements and institutional policies regarding documentation. Compliance with these standards protects both the provider and the patient, ensuring that sensitive information is handled appropriately. Staying informed can feel overwhelming, but it’s a vital part of your role.
Practice regularly to enhance your skills in writing SOAP notes: Like any skill, effective documentation writing improves with practice. Consistently composing and assessing written materials aids providers in enhancing their record-keeping abilities, resulting in more precise and thorough accounts. How often do you take time to reflect on your documentation skills?
By implementing these optimal strategies, healthcare professionals can ensure that their writing SOAP notes is not only efficient but also enhances care for individuals. Additionally, utilizing visual aids in SOAP notes can enhance objectivity by providing quantifiable information about a patient's condition, further supporting the documentation process. Remember, every step you take towards improving your documentation is a step towards better patient care.
Conclusion
Mastering the art of writing SOAP notes is essential for healthcare professionals dedicated to providing high-quality patient care. Have you ever felt overwhelmed by the administrative tasks that can distract from your primary focus—your patients? This structured documentation method not only fosters effective communication among providers but also ensures that each patient's unique needs are fully understood and addressed. By embracing the SOAP format, you can enhance your documentation practices and ultimately improve patient outcomes.
Throughout this article, we’ve explored the key components of SOAP notes—Subjective, Objective, Assessment, and Plan. Each section plays a vital role in documenting patient interactions, from capturing personal experiences to outlining treatment plans. Consider how clarity and conciseness in your documentation can minimize errors and enhance patient safety. Regularly reviewing and incorporating feedback is crucial for continuous improvement in your documentation practices.
In conclusion, the importance of proficient SOAP note writing cannot be overstated. It serves as a foundational element in ensuring comprehensive patient care and fostering collaboration among healthcare teams. By prioritizing clarity, structure, and the inclusion of patient perspectives, you can transform your documentation practices. This commitment not only enhances individual patient experiences but also strengthens the overall healthcare system.
Embrace the challenge of refining your SOAP note writing skills—every improvement contributes to better patient care and safety. Here are some key solutions to consider:
- Regularly review your notes for clarity.
- Seek feedback from colleagues to enhance your approach.
- Stay updated on best practices in documentation.
Together, let’s make a difference in patient care.




