Introduction
Mastering the art of documentation is crucial for healthcare providers. In a field where clarity can mean the difference between effective care and costly errors, it’s essential to approach this task with empathy. The SOAP note framework offers a structured method that not only streamlines documentation but also fosters better communication among providers. This ultimately leads to improved patient outcomes.
But how can we ensure that the History of Present Illness (HPI) is captured with both precision and compassion? It’s all too easy to fall into common pitfalls that can undermine its effectiveness. This guide explores the key elements and best practices for crafting an impactful SOAP note HPI. By equipping providers with these tools, we can elevate the standard of patient care and support one another in this vital work.
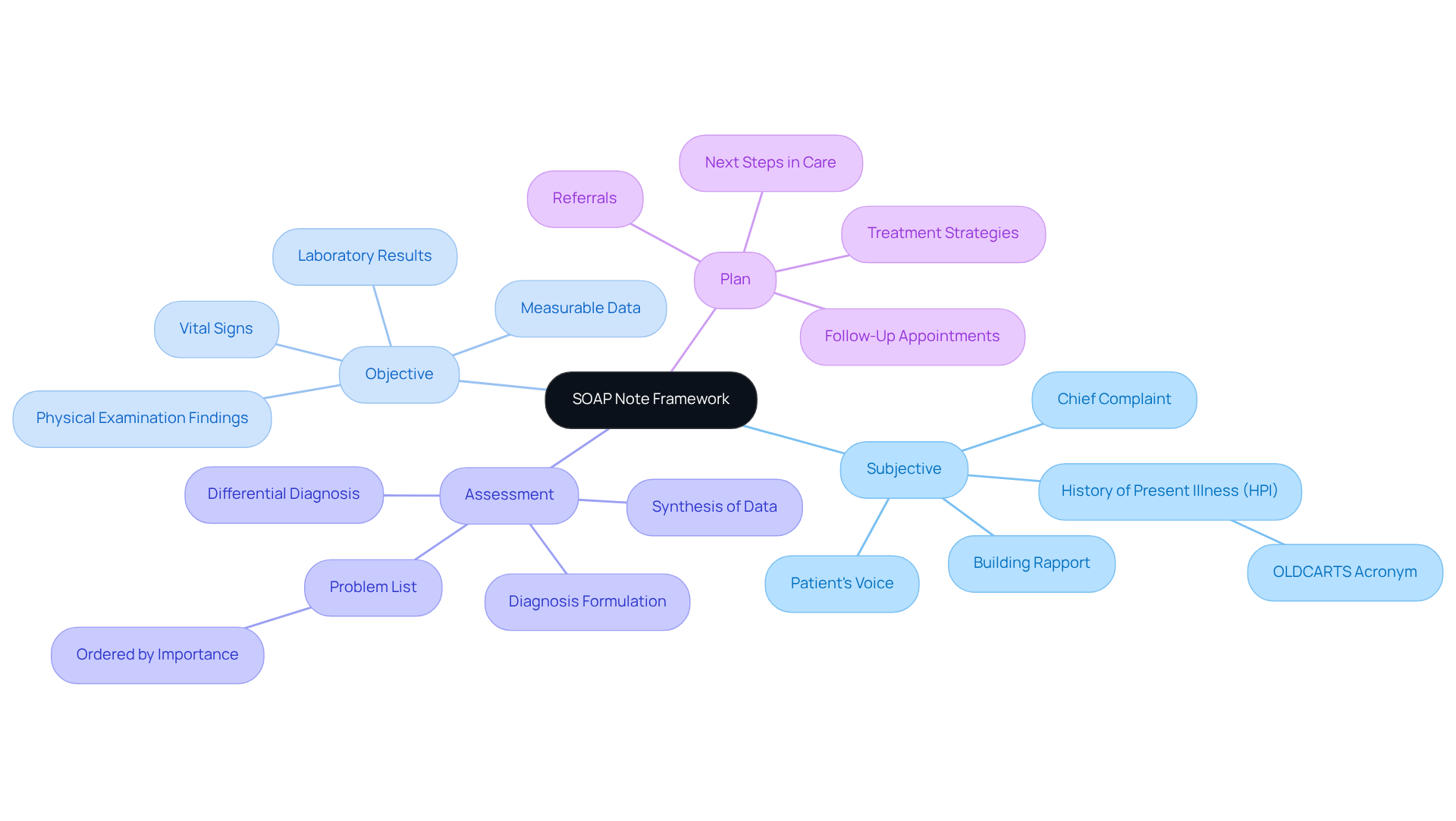
Understand the SOAP Note Framework
The SOAP note framework is more than just a tool; it’s a lifeline for healthcare providers navigating the complexities of patient care. With its four integral components - Subjective, Objective, Assessment, and Plan - it offers a structured approach that can alleviate some of the emotional burdens faced in clinical settings.
- Subjective (S): Here, we capture the patient’s voice. It’s about understanding their symptoms, concerns, and personal experiences related to their health. This section is crucial for building rapport and trust.
- Objective (O): This is where measurable data comes into play. Clinicians document vital signs, physical examination findings, and relevant diagnostic information, providing a solid foundation for assessment.
- Assessment (A): This part synthesizes the subjective and objective data to formulate a diagnosis. It reflects the clinician's clinical reasoning and understanding of the individual’s condition, ensuring that every patient feels seen and understood.
- Plan (P): The plan outlines the next steps in care, detailing treatments, referrals, and follow-up appointments. This ensures continuity and effectiveness in management, which is vital for patient outcomes.
Mastering this framework is essential for accurately documenting the SOAP note HPI, which is a key aspect of the Subjective section. Effective documentation using SOAP note HPI not only enhances communication among healthcare providers but also minimizes the risk of errors. This ultimately leads to better outcomes for those receiving care.
In fact, many healthcare providers now utilize the SOAP note framework, highlighting its importance in primary care settings. As healthcare experts have noted, the organized format of SOAP notes promotes clear communication and ensures that clinically relevant information is easily accessible. This clarity improves the quality of care, allowing providers to focus on what truly matters - their patients.
So, how can you integrate the SOAP note framework into your practice? Consider the emotional challenges you face daily and how this structured approach can ease some of that burden. By embracing this method, you’re not just documenting; you’re enhancing the care you provide. Let’s work together to ensure that every patient receives the compassionate care they deserve.
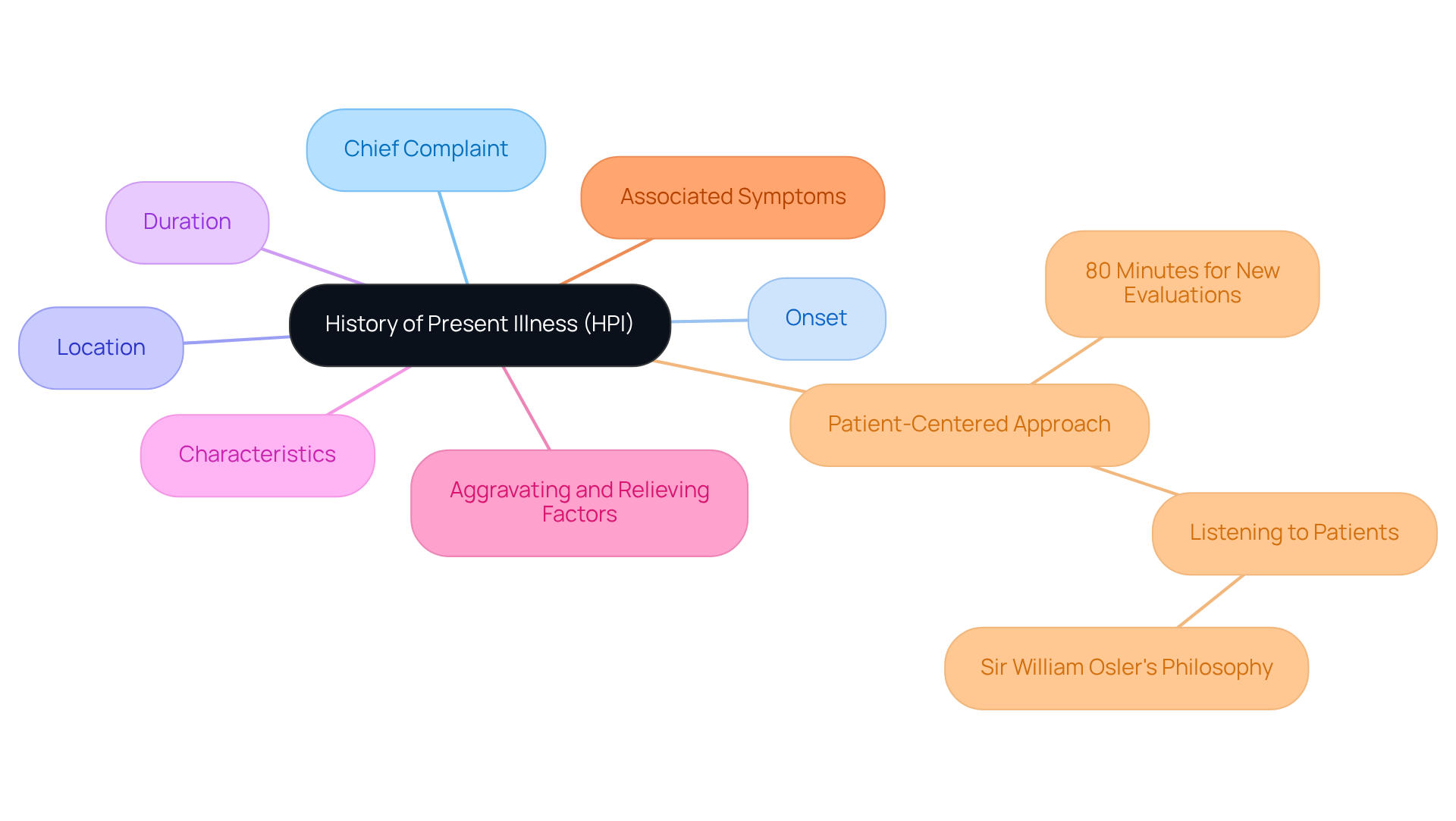
Identify Key Elements of the HPI
Understanding a patient's current condition hinges on the soap note hpi that documents the History of Present Illness. This vital component encompasses several key elements that can make a significant difference in patient care:
- Chief Complaint (CC): This is the primary reason for the patient's visit, expressed in their own words. It sets the stage for the entire evaluation.
- Onset: Knowing when the signs began provides essential context for understanding the progression of the condition.
- Location: Identifying where the signs are experienced is crucial for uncovering potential underlying issues.
- Duration: The length of time the signs have been present can indicate the severity and urgency of the condition.
- Characteristics: Detailed descriptions of the signs-whether they are sharp, dull, or throbbing-can guide diagnostic considerations.
- Aggravating and Relieving Factors: Recognizing what worsens or eases the issues helps in understanding the dynamics of the condition.
- Associated Symptoms: Any additional symptoms accompanying the chief complaint can provide critical insights into the overall health picture.
By systematically gathering this information, healthcare providers can construct a comprehensive soap note hpi that significantly aids in clinical decision-making. For instance, at SchrothDC, the commitment to spending 80 minutes on new evaluations allows clinicians to explore these aspects thoroughly. This dedication results in enhanced diagnostic accuracy and client satisfaction.
This patient-centered approach resonates with the wisdom of Sir William Osler, who emphasized the importance of listening to patients. They often reveal the diagnosis through their narratives. Such thorough documentation not only enhances the quality of care but also aligns with the ethical standards upheld by providers committed to compassionate healthcare.
In a field where administrative burdens can weigh heavily on providers, taking the time to understand each patient's story is invaluable. How often do we find ourselves rushing through evaluations, missing the nuances that could lead to better outcomes? By prioritizing these conversations, we can foster a more supportive environment for both patients and providers. Let's embrace this approach together, ensuring that every patient feels heard and valued.
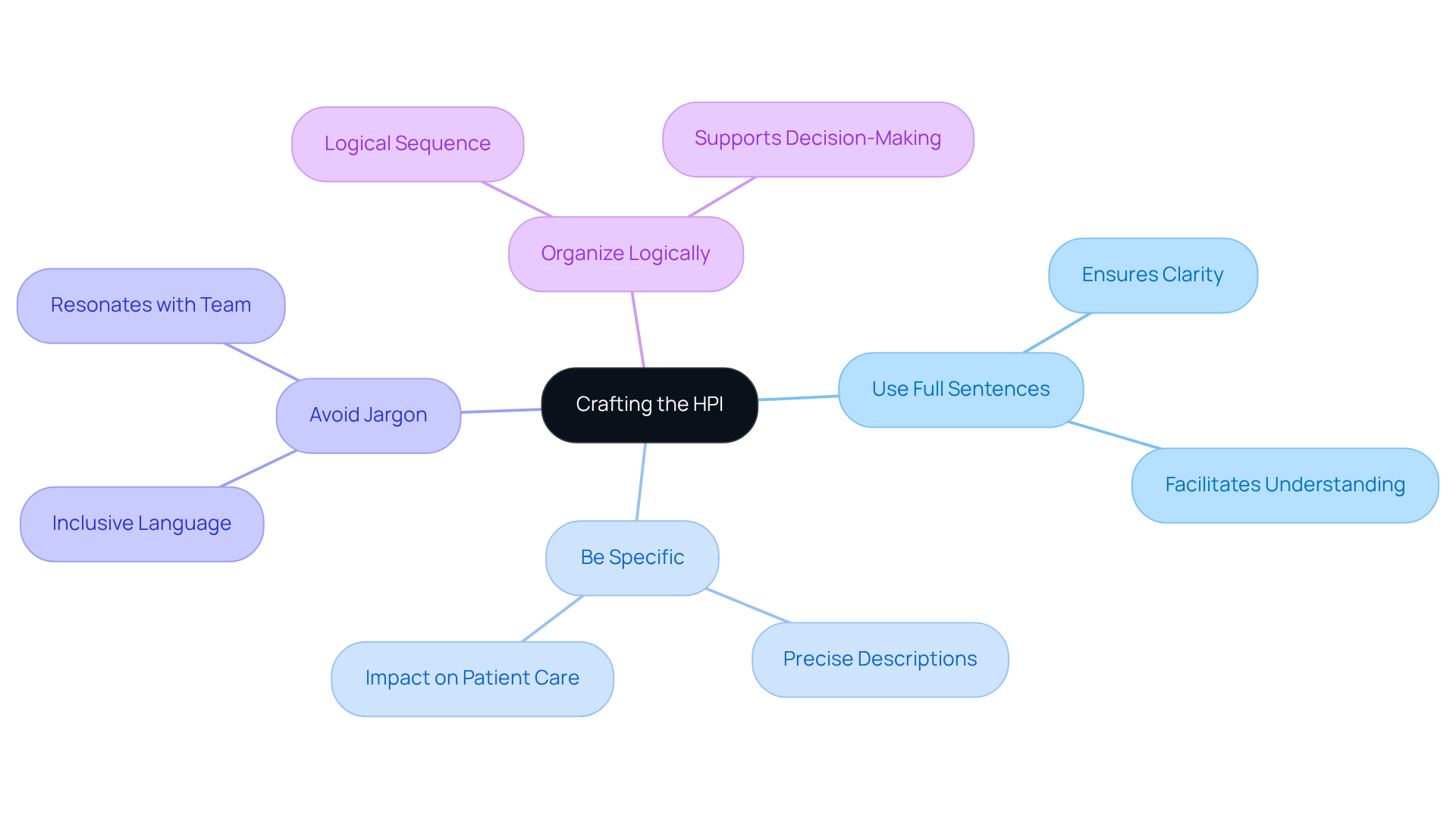
Craft the HPI with Clear and Concise Language
When writing the soap note hpi, it’s essential to communicate with clarity and compassion. Clear and concise language not only aids understanding but also fosters trust between healthcare providers and patients. Here are some thoughtful tips to enhance your writing:
- Use Full Sentences: Writing in complete sentences ensures that your message is clear and easily understood.
- Be Specific: Instead of using vague terms, opt for precise descriptions of signs and their characteristics. This specificity can make a significant difference in patient care.
- Avoid Jargon: Choose language that resonates with all members of the healthcare team. This inclusivity helps everyone stay on the same page.
- Organize Logically: Present information in a logical sequence, typically starting with the chief complaint and then detailing the symptoms. This structure supports better understanding and decision-making, especially in the context of a soap note hpi.
For instance, rather than saying "the individual feels bad," you might specify, "the individual reports a sharp pain in the lower right abdomen that started two days ago and worsens with movement." This level of detail not only aids in accurate diagnosis but also enhances treatment planning.
By embracing these practices, you can alleviate some of the emotional burdens that come with administrative tasks, allowing you to focus more on what truly matters-your patients.
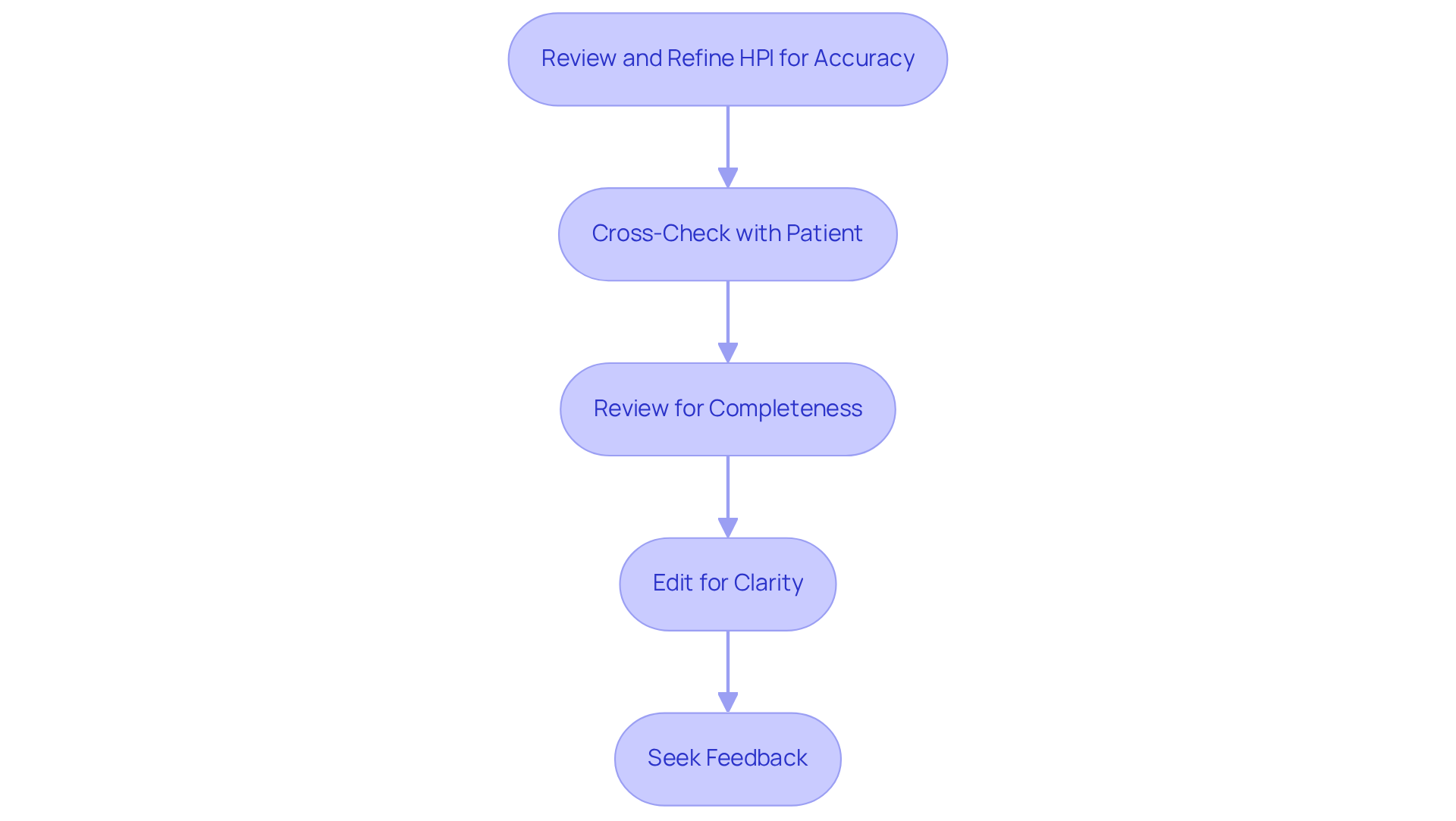
Review and Refine Your HPI for Accuracy
To ensure the accuracy of the soap note hpi, it is crucial to review and refine the documentation with care. Here are some key steps to follow:
- Cross-Check with Patient: Whenever possible, confirm details directly with the patient. This practice not only enhances accuracy but also builds trust and engagement in the patient-provider relationship.
- Review for completeness to ensure all critical elements are included in the soap note hpi. A well-structured narrative should flow logically, capturing the full scope of the individual’s condition.
- Edit for Clarity: Remove unnecessary jargon and ambiguous terms that could confuse the reader. Clear and concise language is vital for effective communication among healthcare providers.
- Seek Feedback: Collaborate with colleagues to review the HPI. Peer insights can reveal overlooked details and improve the overall quality of records.
Investing time in refining the soap note HPI not only enhances the quality of records but also significantly impacts patient outcomes. Precise soap note hpi are linked to better clinical decision-making and improved care delivery. Studies show that comprehensive record-keeping can reduce errors and boost treatment effectiveness.
Significantly, the Office of Inspector General (OIG) found that 25% of submitted conditions lacked support from medical records, highlighting the need for careful record-keeping practices. As Kellie Macpherson, Executive Vice President of Compliance & Security, wisely stated, "Clear records make the compliance process so much easier and ensure that no small change is overlooked."
Furthermore, case studies have demonstrated that inadequate documentation can lead to serious financial repercussions, as seen in the OIG audit findings. Providers should also be cautious about altering medical records after the fact, as this can lead to complications and undermine the integrity of patient care.
By taking these steps, you not only protect your practice but also ensure that your patients receive the best possible care. How can you start refining your HPI today?
Conclusion
Mastering the SOAP note framework, especially the History of Present Illness (HPI), is crucial for healthcare providers who genuinely care about delivering high-quality patient care. This structured approach not only simplifies documentation but also enhances communication and fosters a deeper understanding of patients' needs. By focusing on the key components of the SOAP note - Subjective, Objective, Assessment, and Plan - clinicians can capture a comprehensive view of each patient's condition.
Have you ever felt overwhelmed by the demands of documentation? The significance of clear and concise documentation cannot be overstated. Key elements of the HPI, such as the Chief Complaint, Onset, Location, Duration, Characteristics, Aggravating and Relieving Factors, and Associated Symptoms, play a vital role in guiding clinical decision-making. By using specific language and logical organization, providers can create effective SOAP notes that resonate with both their colleagues and patients, ultimately leading to better outcomes.
In light of the challenges faced in clinical settings, the call to action is clear: prioritize thorough and accurate HPI documentation. By refining the HPI and embracing best practices, healthcare providers can enhance the quality of their records, reduce errors, and improve patient satisfaction. This commitment not only benefits individual practices but also upholds the ethical standards of compassionate healthcare.
Key Solutions for Effective HPI Documentation:
- Listen actively to your patients.
- Document thoroughly and accurately.
- Embrace best practices in your notes.
Taking the time to listen and document effectively is an investment in both patient care and the overall success of the healthcare system. Together, let’s strive for excellence in our documentation practices.




