Overview
In the demanding world of healthcare, providers often face emotional challenges that can weigh heavily on their ability to deliver quality care. The administrative burdens can feel overwhelming, leaving little room for the compassionate interactions that patients truly deserve. How can we ease this strain and enhance the patient experience?
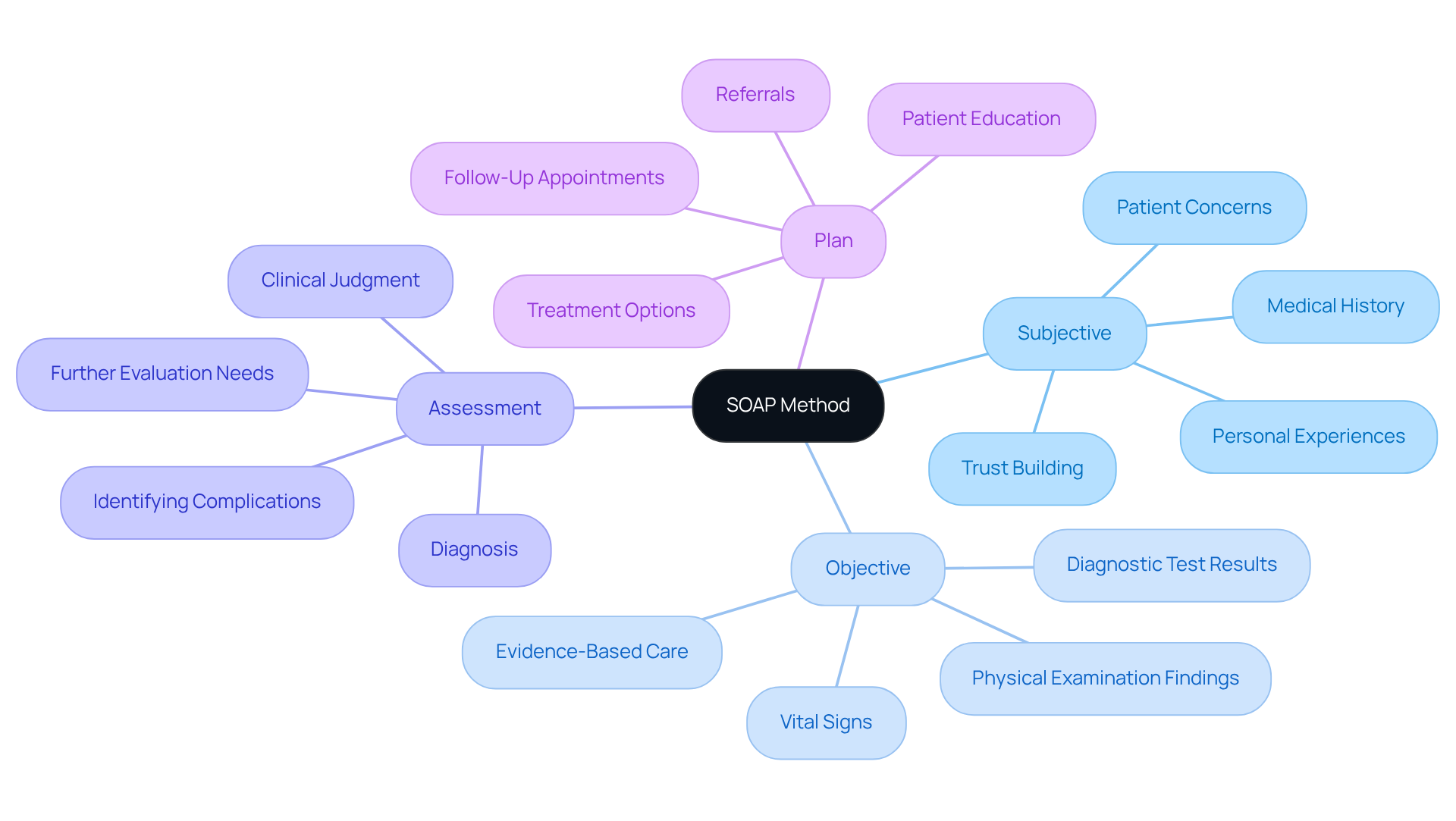
The SOAP method, which stands for Subjective, Objective, Assessment, and Plan, offers a structured approach to patient care documentation. By organizing information into these four components, healthcare providers can streamline their documentation process. This not only improves clarity and communication among team members but also ensures that all relevant details are accurately recorded and easily accessible.
Imagine the difference it could make when every healthcare provider can quickly find the information they need to make informed decisions. Mastering the SOAP method fosters better patient outcomes, as it allows for a more thorough understanding of each patient's unique situation.
Key Benefits of the SOAP Method:
- Enhances clarity in documentation
- Improves communication among healthcare providers
- Ensures all relevant details are easily accessible
- Fosters better patient outcomes
By embracing this method, healthcare providers can reclaim valuable time and focus on what truly matters: their patients. Let’s take a step towards a more organized and compassionate approach to patient care. Are you ready to explore how the SOAP method can transform your practice?
Introduction
In the fast-paced world of healthcare, every moment truly matters. Effective communication and documentation can mean the difference between quality care and unfortunate oversights. Have you ever felt overwhelmed by the administrative burdens that can distract from patient interactions? The SOAP method—standing for Subjective, Objective, Assessment, and Plan—provides a structured framework that can help streamline these interactions and enhance record-keeping.
As the complexities of patient care continue to evolve, the challenge remains: how can you ensure your documentation not only meets regulatory standards but also fosters a deeper connection with your patients? This guide is here to support you in mastering the SOAP method, equipping you with the tools needed to transform your practice and improve patient outcomes.
Imagine a practice where documentation feels less like a chore and more like a meaningful part of patient care. By embracing the SOAP method, you can create a more efficient workflow that allows you to focus on what truly matters—your patients.
Key Benefits of the SOAP Method:
- Streamlined patient interactions
- Enhanced record-keeping
- Improved patient outcomes
Let’s explore how you can implement this method effectively and make a positive impact on your practice and your patients' lives.
Understand the SOAP Method in Patient Care
In the demanding world of healthcare, providers often face emotional challenges that can weigh heavily on their ability to deliver care. The administrative burdens can distract from what truly matters—patient care. This is where the SOAP method EMT comes into play, providing a structured approach that not only organizes individual information but also enhances communication among providers, especially in fragmented healthcare systems.
SOAP stands for Subjective, Objective, Assessment, and Plan. By mastering this method, healthcare professionals can systematically record encounters, ensuring that all relevant information is captured and easily accessible. Imagine the relief of knowing that your documentation is clear and comprehensive, allowing you to focus more on your patients rather than paperwork. This organized strategy promotes empathetic and efficient service delivery, tackling the complexities of healthcare documentation that often hinder effective communication.
As we look ahead to 2025, the importance of documentation in healthcare becomes even clearer. It enables continuity of treatment and supports evidence-based decision-making. However, regulatory concerns, like those posed by HIPAA, can create barriers that complicate patient-provider interactions. Yet, providers who embrace a structured approach often report improved clarity in their records, making it easier to monitor patient progress and identify ongoing issues. Dr. Hope Bauman aptly states, "SOAP documentation isn’t merely a recording tool—they’re a significant aspect of delivering secure, high-quality service, safeguarding yourself legally and ensuring your services are compensated appropriately."
Real-world examples illustrate the effectiveness of the SOAP method EMT. For instance, a case study highlighted how a clinic's transition to digital documentation significantly enhanced efficiency. Therapists could then dedicate more time to patient care rather than getting bogged down by paperwork. Additionally, the organized format of medical notes ensures that all team members share a common understanding of a patient’s condition, which is crucial for managing complex or chronic issues.
Ultimately, the SOAP method EMT not only enhances the quality of documentation but also plays a crucial role in improving client outcomes. It’s an indispensable tool for healthcare providers, fostering a supportive environment where both patients and providers can thrive. Are you ready to embrace this method and transform your practice?
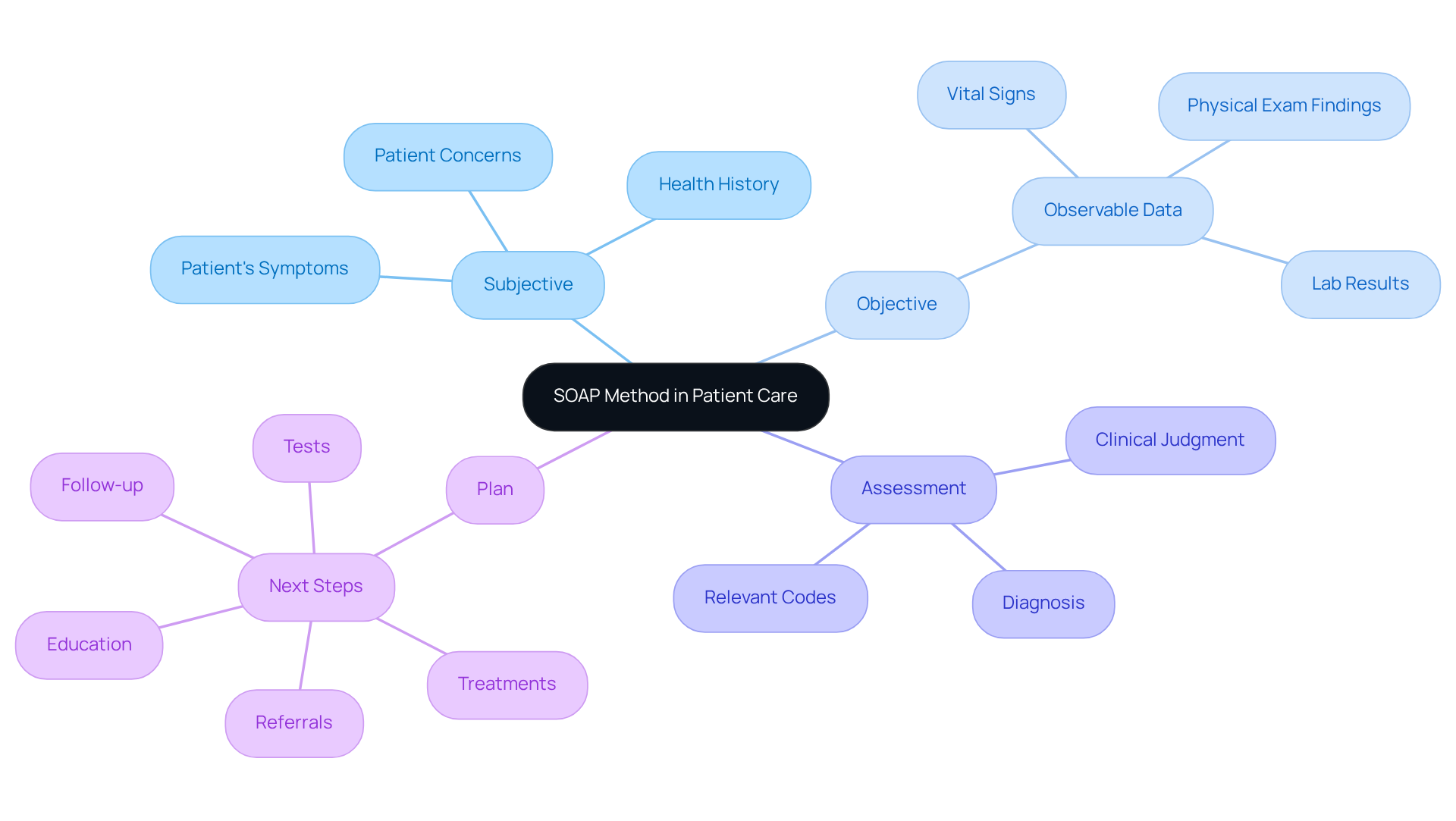
Explore the Components of SOAP: Subjective, Objective, Assessment, and Plan
-
Subjective: This component captures your personal experiences, feelings, and concerns. It includes the information you share about your symptoms, medical history, and any other relevant details. Documenting this subjective information effectively is crucial. It helps healthcare providers understand your perspective and tailor your care accordingly. When healthcare professionals capture individual viewpoints, it fosters trust and can lead to better treatment outcomes.
-
Objective: This section includes measurable and observable data collected during your visit, such as vital signs, physical examination findings, and diagnostic test results. Objective data provides a solid foundation for clinical assessments and decision-making, ensuring that your care is based on verifiable evidence. Integrating this objective data is vital in the SOAP method EMT, as it complements your subjective insights and enhances the overall assessment process.
-
Assessment: Here, your healthcare provider synthesizes both subjective and objective data to make a clinical judgment. This may involve diagnosing your condition, identifying potential complications, or recognizing the need for further evaluation. The ability to evaluate your situation effectively relies heavily on accurately documenting both subjective and objective information, which together guide clinical decisions.
-
Plan: The final component outlines the proposed course of action based on the assessment. This may include treatment options, referrals, follow-up appointments, and education for you. A well-organized strategy ensures that both you and your provider are aligned on the next steps in your treatment. Clear communication and mutual understanding are essential in the healthcare process. By actively involving you in your care plan, providers can enhance your satisfaction and adherence to treatment.
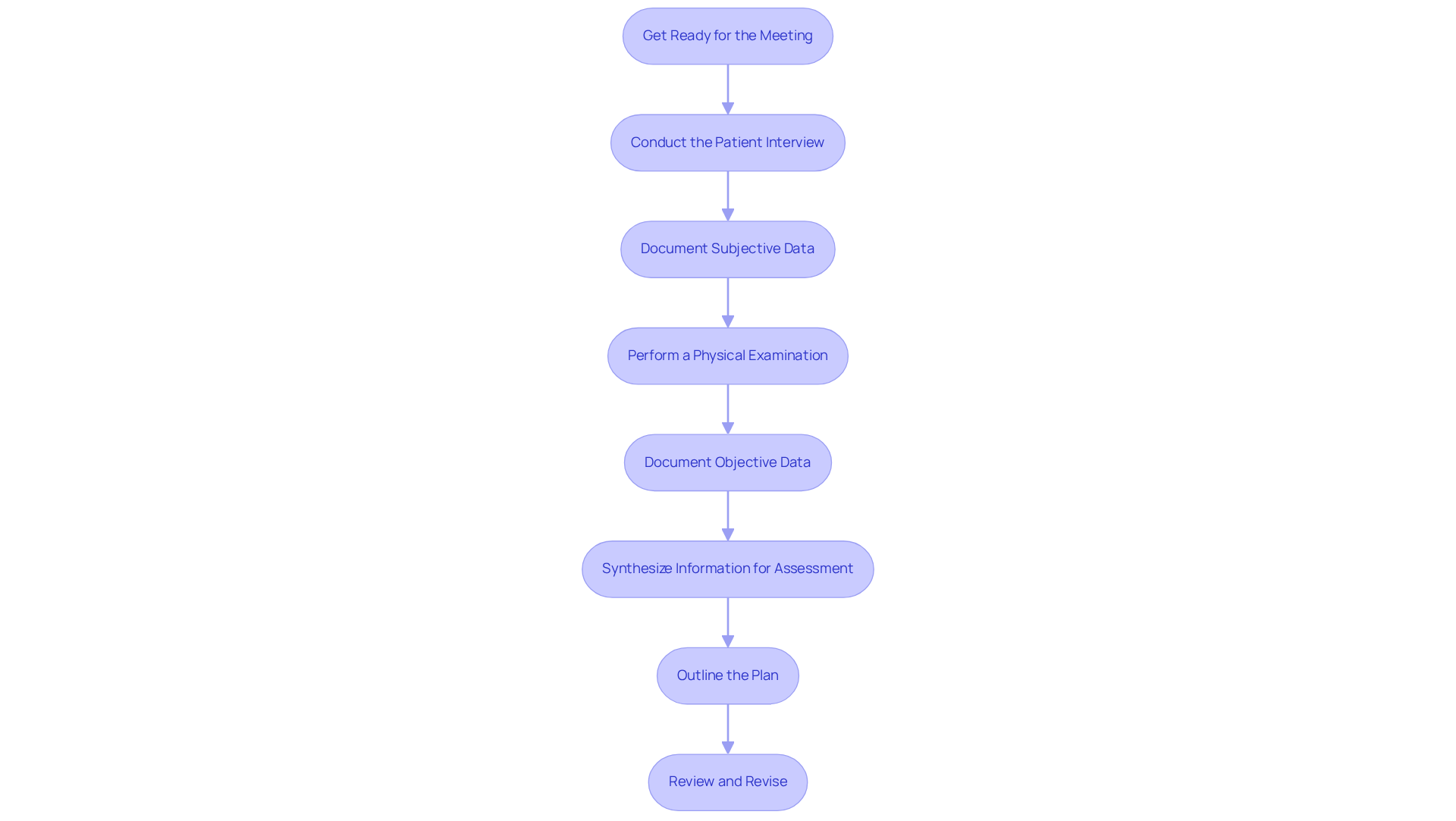
Implement the SOAP Method: A Step-by-Step Guide for Healthcare Providers
-
Get Ready for the Meeting: Before you meet with the individual, take a moment to review their medical background and any previous records. This thoughtful preparation allows you to ask informed questions and gather important information, paving the way for a meaningful interaction.
-
Conduct the Patient Interview: Start the conversation with open-ended questions that encourage the individual to share their concerns and symptoms in their own words. This approach fosters a trusting environment, promoting open communication and understanding.
-
Document Subjective Data: As the individual shares their story, make sure to take detailed notes on their responses. Focus on capturing their feelings, concerns, and relevant history that may influence their care. This ensures that their voice is truly reflected in the documentation.
-
Perform a Physical Examination: Conduct a thorough examination to gather objective data. Document vital signs and any noticeable findings that are crucial to the individual's condition. These measurements are essential for accurate evaluation and treatment planning.
-
Document Objective Data: Write down the measurable data collected during the examination with clarity and precision. This documentation forms the foundation for clinical decision-making and serves as a reliable reference for future care.
-
Synthesize Information for Assessment: Take the time to analyze both the subjective and objective data to formulate your clinical assessment. Consider potential diagnoses and any complications that may arise, ensuring a comprehensive view of the individual's health status.
-
Outline the Plan: Based on your assessment, develop a clear and actionable plan that includes treatment options, referrals, and follow-up care. This strategy promotes effective communication with the individual and other healthcare providers, ensuring everyone is on the same page.
-
Review and Revise: After documenting the SOAP entry, review it for completeness and accuracy. Make any necessary adjustments to enhance clarity and coherence, ensuring that the document serves as a trustworthy account of your encounter with the individual.
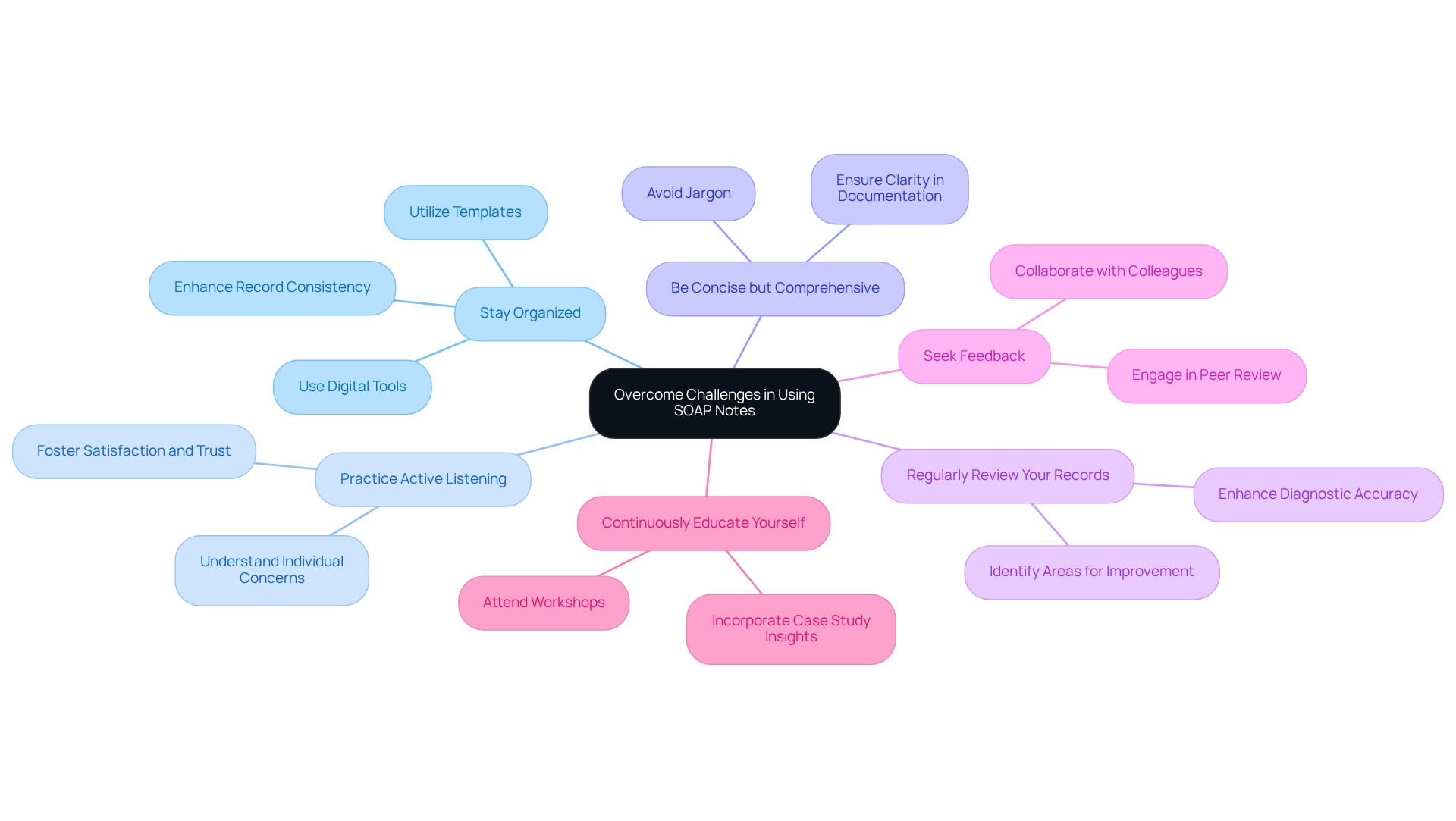
Overcome Challenges in Using SOAP Notes: Tips and Best Practices
-
Stay Organized: Have you ever felt overwhelmed by the documentation process? Utilizing templates or digital tools can really help streamline your efforts. This approach not only saves you time but also enhances the consistency of your records, ultimately leading to better care for individuals. As Richard Abrams, MD, wisely points out, "people do not always recall the details of what you did or said at the end of the day, but they will undoubtedly remember how your actions affected their feelings." This highlights just how crucial clear documentation is.
-
Practice Active Listening: During client interviews, how often do you prioritize truly understanding the individual’s concerns? Focusing on this can significantly improve the quality of the subjective data you gather, fostering greater satisfaction and trust among individuals. Research shows that when individuals feel valued and engaged, they’re more likely to follow treatment plans.
-
Be Concise but Comprehensive: Are your records clear and easy to understand? Striving for clarity in your documentation is essential. Avoiding jargon ensures that your notes are accessible to other healthcare providers, which facilitates seamless communication and continuity of care. Remember, while patients may not recall all medical details, they will certainly remember how they were treated.
-
Regularly Review Your Records: When was the last time you took a moment to review your documentation? Dedicating time to this practice can help you identify areas for improvement and deepen your understanding of the process, leading to better diagnostic accuracy. Studies on diagnostic errors reveal that thorough documentation can prevent common mistakes.
-
Seek Feedback: Have you considered collaborating with colleagues to review each other’s SOAP notes? Constructive feedback can provide valuable insights, helping you enhance your documentation skills and improve overall treatment. Engaging in peer review not only benefits you but also fosters a culture of safety and continuous improvement.
-
Continuously Educate Yourself: Are you keeping up with best practices in documentation and patient care? Staying informed is key. Attend workshops or training sessions focused on the SOAP method EMT to refine your skills and adapt to evolving healthcare standards. Incorporating insights from case studies, like "The Value of Patient Insights," can further enrich your understanding of effective patient communication.
Conclusion
Mastering the SOAP method is crucial for healthcare providers who want to enhance patient care while easing the burden of documentation. Have you ever felt overwhelmed by administrative tasks? This structured approach not only organizes vital information but also promotes effective communication among healthcare teams. By embracing the SOAP method, you can focus more on your patients and less on paperwork, ultimately improving the clarity and quality of your documentation in today’s complex healthcare landscape.
Each component of the SOAP method—Subjective, Objective, Assessment, and Plan—plays a foundational role in fostering effective patient interactions and treatment planning. By capturing personal experiences and measurable data, you can develop well-informed care plans that ensure comprehensive and empathetic care. Here are some practical tips to overcome common challenges with SOAP notes:
- Stay organized
- Practice active listening
- Engage in continuous education
In conclusion, the SOAP method is more than just a documentation tool; it’s a supportive approach that enhances patient outcomes and nurtures a collaborative healthcare environment. By implementing this method, you not only safeguard your practice but also elevate the quality of care you deliver. It’s time to embrace the SOAP method and witness its profound impact on both patient satisfaction and your professional efficiency.




