Overview
In the demanding world of healthcare, mastering the SOAP note format can feel overwhelming. This comprehensive guide aims to alleviate some of that burden, offering a nurturing approach to effective medical documentation. By understanding the components—Subjective, Objective, Assessment, and Plan—you can enhance not only your documentation skills but also the care you provide to your patients.
Have you ever felt that administrative tasks take away from the time you could spend with your patients? This guide details how integrating AI tools and best practices can lighten that load, improving clarity and efficiency in your notes. Imagine a world where your documentation supports your patient care rather than hinders it.
The benefits of mastering the SOAP note format extend beyond mere efficiency; they contribute to better overall care outcomes. By embracing this structure, you can ensure that your patients receive the attention and care they deserve. Let’s take this journey together towards a more streamlined and compassionate approach to healthcare documentation.
As you explore this guide, consider how these insights can transform your practice. Are you ready to enhance your skills and improve patient care? Together, we can make a difference, one SOAP note at a time.
Introduction
Mastering the art of medical documentation is not merely about efficiency; it stands as a vital cornerstone of effective patient care. The SOAP note format—comprising Subjective, Objective, Assessment, and Plan—provides healthcare providers with a structured framework to capture essential patient information and enhance clinical decision-making. However, many practitioners face emotional challenges as they navigate common pitfalls in documentation that can significantly impact patient outcomes.
How can providers refine their approach to ensure that every note not only meets the standards of clarity and completeness but also truly reflects the complexities of patient care?
By addressing these challenges, we can foster a more supportive environment for both providers and patients. The journey toward effective documentation is not just about meeting requirements; it's about nurturing the patient-provider relationship and ensuring that every detail is captured with care.
Let’s explore how we can work together to overcome these hurdles and enhance the quality of care we provide.
Understand the SOAP Note Structure
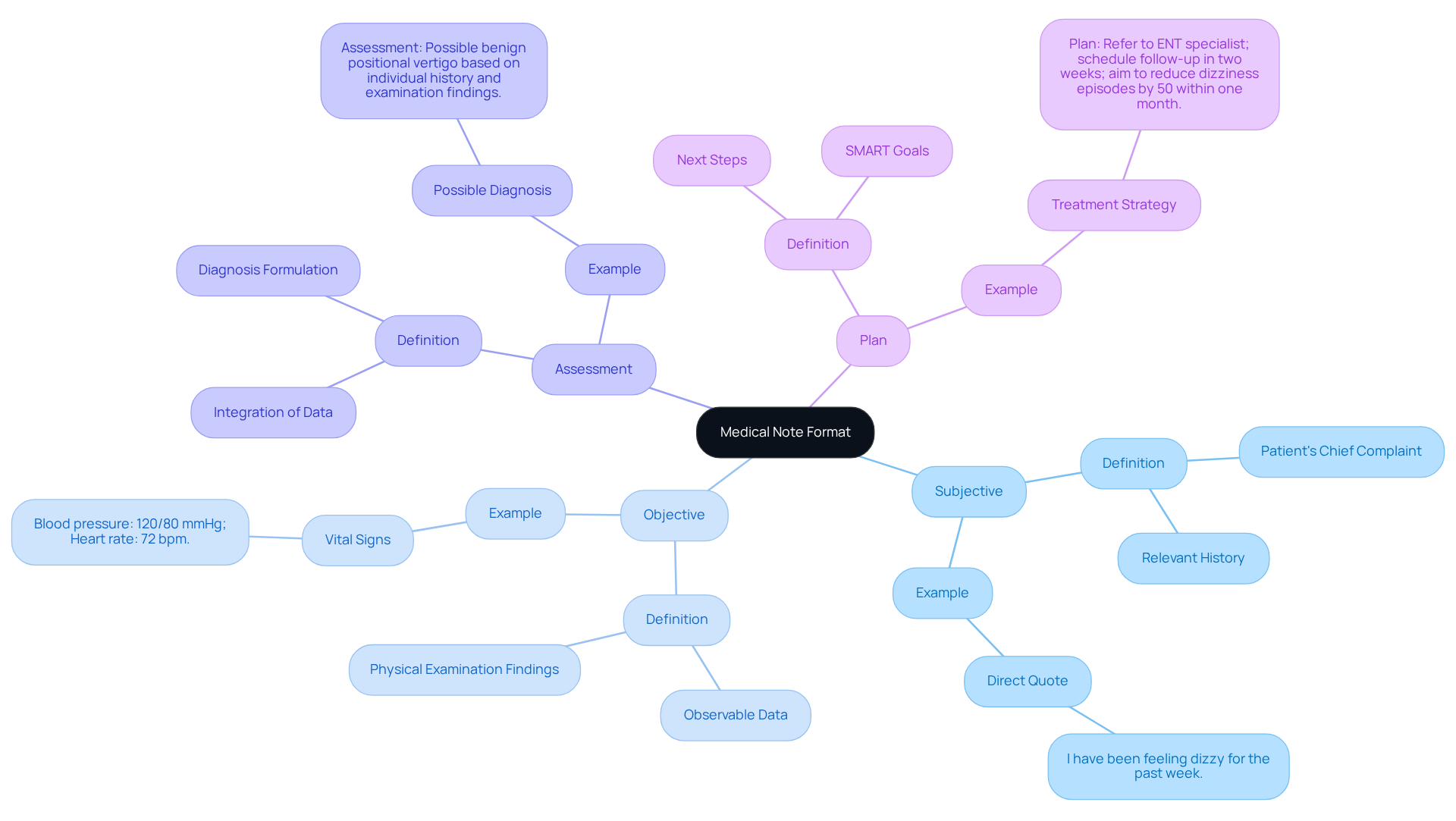
The medical note format, which is an acronym for Subjective, Objective, Assessment, and Plan (SOAP), provides a compassionate and systematic approach for healthcare providers to effectively document their interactions with individuals. Each component plays a crucial role in enhancing patient care:
-
Subjective: This section captures the patient's perspective, including symptoms, feelings, and concerns. Understanding the individual's experience is vital for tailoring care. By leveraging generative AI, healthcare professionals can enrich this section, using AI-powered tools to analyze data and gain insights, ensuring a deeper understanding of each individual's needs.
-
Objective: Here, practitioners document measurable data, such as vital signs, physical examination findings, and laboratory results. This information is essential for clinical evaluation, creating a complete picture of the individual's health status. AI can streamline the collection and analysis of this data, reducing the administrative burden on healthcare professionals.
-
Assessment: This part synthesizes the subjective and objective data to provide a clinical judgment or diagnosis. It reflects the caregiver's understanding of the individual's condition and guides future clinical decisions. Generative AI can support this process by identifying patterns in user data, leading to more precise assessments and diagnoses.
-
Plan: The final section outlines proposed interventions, treatments, and follow-up plans, ensuring alignment between the provider and individual on the next steps in care. AI tools can help develop tailored treatment plans based on extensive medical data analysis, ultimately improving care outcomes.
Mastering this structured approach not only enhances record-keeping efficiency but also significantly improves patient care outcomes. For instance, a national health system that embraced organized record-keeping methods reported a decrease in antibiotic prescribing, saving $80,000 each quarter. Healthcare experts emphasize that clear and consistent records are vital for delivering high-quality care, as they enhance communication between practitioners and support clinical reasoning. Additionally, adopting the APSO order (Assessment, Plan, Subjective, Objective) can further improve usability and speed for clinicians.
By utilizing the medical note format, providers can ensure their records are comprehensive, precise, and beneficial for managing individuals' care. However, it is essential to acknowledge the limitations of the SOAP format, such as its inability to document changes over time, which can impact continuity of care. How can we better adapt our practices to ensure we meet the evolving needs of our patients?

Explore Each Component: Subjective, Objective, Assessment, and Plan
Each component of the medical note format plays a vital role in patient documentation, and understanding this can significantly ease the administrative burdens faced by healthcare providers.
-
Subjective: Start by documenting the patient's chief complaint and any relevant history. Using direct quotes can truly capture the individual's voice. For instance, consider the statement, "I have been feeling dizzy for the past week." This not only reflects their experience but also fosters a deeper connection.
-
Objective: Next, record observable data such as blood pressure, heart rate, and any physical examination findings. For example, you might note, "Blood pressure: 120/80 mmHg; Heart rate: 72 bpm." These details are crucial for accurate assessments.
-
Assessment: Combine the subjective and objective data to formulate a diagnosis. For instance, you could say, "Assessment: Possible benign positional vertigo based on individual history and examination findings." This integration ensures a comprehensive understanding of the patient's condition.
-
Plan: Finally, outline the next steps, including tests, treatments, and follow-up appointments. Incorporating SMART goals clarifies expectations and promotes accountability. An example might be, "Plan: Refer to ENT specialist; schedule follow-up in two weeks; aim to reduce dizziness episodes by 50% within one month." This structured approach not only guides care but also reassures patients of their path forward.
By clearly outlining each element in the medical note format, providers can ensure their records are thorough and beneficial for the ongoing care of individuals. It’s also essential to acknowledge the limitations of SOAP records; they may not fully capture the complexities of certain patient conditions. Utilizing built-in templates in the medical note format for easy note-taking can significantly improve efficiency and organization in records, ultimately enhancing the quality of care provided. How can we further streamline this process to support our dedication to patient well-being?
Apply Best Practices for Writing SOAP Notes
To write effective SOAP notes, it’s essential to embrace best practices that not only enhance your documentation but also support your vital role in patient care.
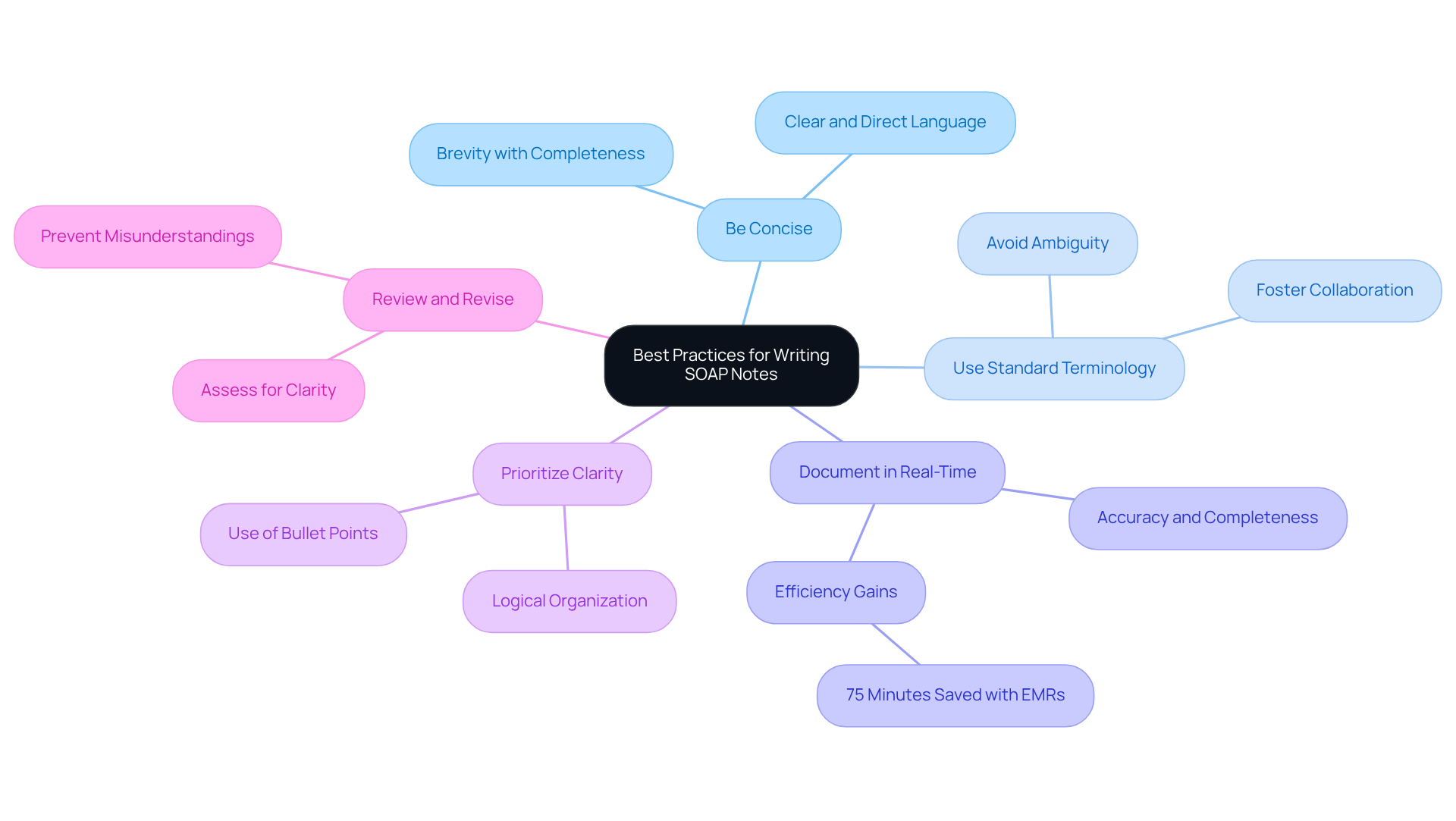
- Be Concise: Use clear and direct language to convey information without unnecessary detail. Aim for brevity while ensuring completeness; concise records significantly enhance communication and understanding among healthcare providers.
- Use Standard Terminology: Consistently employ medical terminology to avoid ambiguity. This practice improves clarity and fosters better collaboration among healthcare teams.
- Document in Real-Time: Writing notes during or promptly after interactions ensures accuracy and completeness. Research shows that real-time record-keeping positively affects the quality of patient care by capturing details that might otherwise be overlooked. For instance, findings demonstrate that EMRs led to an average time saving of 75 minutes in clinical documentation, underscoring the efficiency gained through proper documentation practices.
- Prioritize Clarity: Organize information logically within each section. Utilizing bullet points or numbered lists enhances readability, making it easier for other providers to quickly grasp essential information.
- Review and Revise: After completing the document, assess it for clarity and completeness. Ensure that all pertinent information is included and that the message is free of mistakes. Comprehensive records can prevent misunderstandings and enhance health outcomes. As Brett Shavers highlights, "if you didn’t record it, it didn’t occur," stressing the importance of careful record-keeping.
By following these best practices, you can create SOAP records that are not only informative but also enhance care for individuals. This approach effectively tackles frequent issues in record-keeping. Moreover, citing case studies on the significance of records in various situations can provide practical examples of how to address typical obstacles in SOAP record keeping. Remember, your diligent documentation is a crucial part of the compassionate care you provide.
Troubleshoot Common Issues in SOAP Note Documentation
Frequent issues in SOAP records can significantly hinder effective communication and care for individuals. As healthcare providers, it’s vital to recognize these challenges and address them with compassion. Here are some supportive troubleshooting tips to enhance your documentation practices:
-
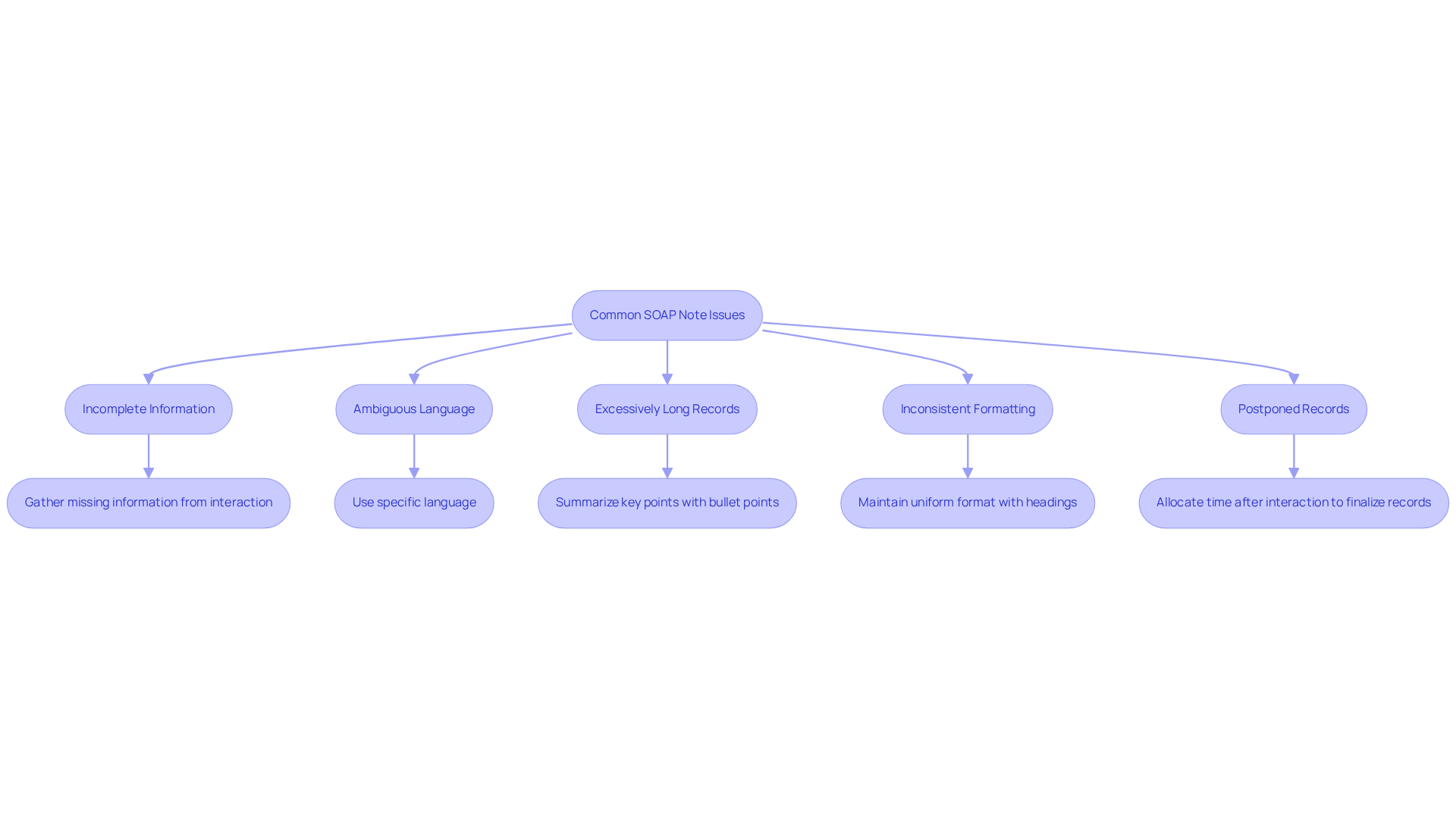
Incomplete Information: When notes lack critical details, take a moment to revisit the interaction with the individual to gather any missing information. Ensure that all components of the medical note format—Subjective, Objective, Assessment, and Plan—are thoroughly addressed. Incomplete documentation can lead to payment delays and potential legal concerns, underscoring the importance of comprehensive records. Studies show that incomplete records can weaken the position of both parties in a dispute, making it difficult to prove damages or challenge the validity of charges.
-
Ambiguous Language: It’s essential to avoid vague terms that can lead to misinterpretation. Instead, strive to use specific language that clearly conveys the individual’s condition and treatment plan. For instance, rather than saying 'the individual feels unwell,' specify the symptoms and their severity to provide a clearer picture of the individual’s status. Common errors in the Subjective section include passing judgment on the individual and documenting irrelevant information, which can undermine the quality of the documentation.
-
Excessively Long Records: If records become too lengthy, focus on summarizing key points. Using bullet points can help condense information without losing essential details. This approach not only improves readability but also ensures that critical information is easily accessible during patient reviews.
-
Inconsistent formatting can hinder readability, so maintaining a uniform medical note format for all SOAP records is essential. Utilize headings and subheadings to clearly delineate each section. Maintaining a consistent medical note format helps other healthcare professionals quickly locate relevant information, fostering better interdisciplinary communication. The American Physical Therapy Association emphasizes that it is your professional duty to ensure that records are well-written.
-
Postponed Records: If notes are not completed promptly, consider allocating specific time after each client interaction to finalize records. This practice aids in ensuring accuracy and completeness, minimizing the risk of errors that could affect outcomes for individuals. Health professionals who received training on routine practice recording were found to be 4.2 times more likely to record effectively, indicating that motivation and training are crucial for enhancing recording practices.
By proactively addressing these common issues, providers can significantly improve the quality of their SOAP notes, ultimately leading to enhanced patient care and outcomes. Effective documentation not only supports clinical decision-making but also reinforces the ethical standards of care aligned with Catholic teachings.
Conclusion
Mastering the medical note format, particularly the SOAP structure, is essential for healthcare providers who strive to deliver high-quality patient care. This systematic approach not only enhances the clarity and effectiveness of documentation but also nurtures a deeper understanding of individual patient needs. By integrating the subjective, objective, assessment, and plan components, providers can create comprehensive records that support clinical decision-making and ultimately improve patient outcomes.
Throughout this article, we’ve explored key insights into each SOAP component. The subjective section captures the patient’s voice, while the objective portion provides measurable health data. The assessment synthesizes these elements into a clinical judgment, and the plan outlines actionable steps for treatment. By emphasizing best practices such as concise language, real-time documentation, and clarity, we can significantly enhance the quality of SOAP notes. Addressing common issues like incomplete information and ambiguous language further strengthens the documentation process.
Ultimately, effective SOAP note writing is not merely a clerical task; it is a vital aspect of compassionate patient care. By adopting these structured practices, healthcare providers can ensure that their documentation reflects the complexities of patient interactions. This leads to improved communication and better health outcomes. Embracing these strategies and continuously seeking ways to enhance documentation practices will not only benefit individual providers but also contribute to the overall effectiveness of the healthcare system. How can you implement these practices in your daily routine to foster a more compassionate approach to patient care?




