Overview
Navigating the complexities of patient care can be overwhelming, especially when faced with the administrative burdens of documentation. Many healthcare providers struggle with the emotional weight of ensuring every detail is captured accurately while still providing compassionate care. This is where mastering the chief complaint SOAP note can make a significant difference.
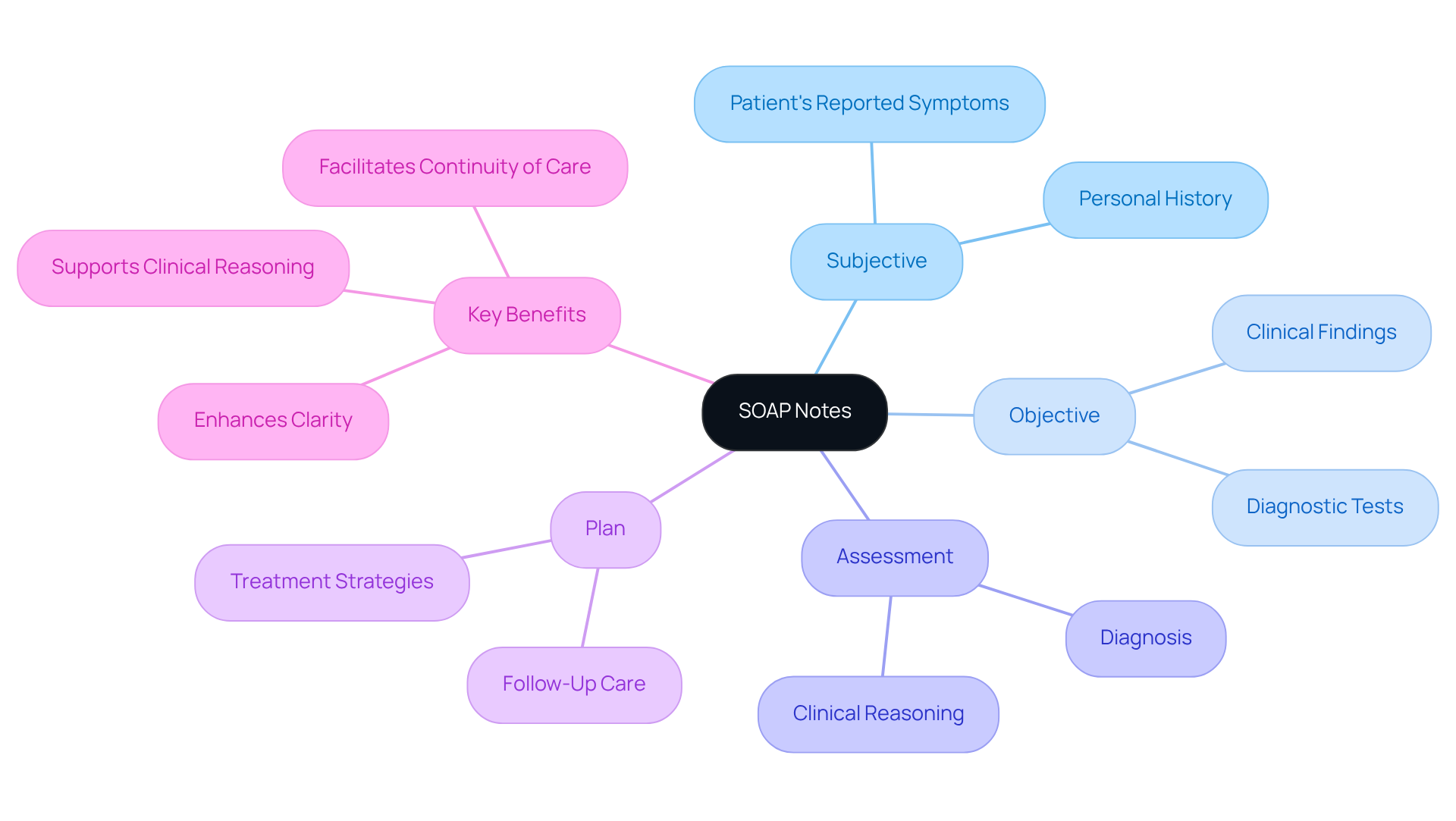
The SOAP note offers a structured approach to documenting patient encounters, breaking down the process into four essential components: Subjective, Objective, Assessment, and Plan. By utilizing this framework, you can enhance communication with your team, support your clinical reasoning, and ensure continuity of care for your patients.
Here are some key benefits of effective SOAP note writing:
- Improved clarity in communication with colleagues and patients.
- Enhanced clinical reasoning that supports better decision-making.
- Streamlined documentation that saves time and reduces stress.
By implementing best practices and utilizing available resources, you can improve your SOAP note writing efficiency. Consider reflecting on your current documentation process: Are there areas where you feel overwhelmed? What changes could help alleviate that burden?
We encourage you to explore the resources provided in this guide and take actionable steps toward mastering the SOAP note. Remember, every effort you make not only benefits your workflow but ultimately enhances the care you provide to your patients.
Introduction
Mastering the art of SOAP notes is crucial for healthcare professionals who seek clarity and efficiency in patient documentation. This structured approach—comprising Subjective, Objective, Assessment, and Plan—enhances communication among providers and improves patient care outcomes. Yet, amidst the complexities of modern healthcare, many practitioners feel overwhelmed.
Have you ever found yourself struggling to write a chief complaint SOAP note while ensuring comprehensive and accurate documentation? The emotional challenges faced by healthcare providers can be significant. Administrative burdens often distract from the core mission of patient care, leaving many feeling frustrated and fatigued.
But there’s hope! By embracing a structured approach to SOAP notes, you can alleviate some of that stress. Here are a few key solutions to consider:
- Streamline your documentation process to save time.
- Enhance communication with your team to ensure everyone is on the same page.
- Focus on patient outcomes by prioritizing clarity in your notes.
Imagine the difference it would make in your practice if you could navigate these challenges with confidence. By mastering SOAP notes, you not only improve your documentation but also enhance the quality of care you provide. Let’s take this journey together, ensuring that every patient receives the attention and care they deserve.
Define SOAP Notes and Their Importance in Healthcare
Structured notes offer a compassionate approach for healthcare professionals, helping them document their encounters with individuals in a systematic way. This method, known as SOAP—Subjective, Objective, Assessment, and Plan—standardizes documentation and fosters better communication among providers. Have you ever felt overwhelmed by the need to convey essential information clearly? In fragmented healthcare systems, where care is often split among various providers, effective documentation becomes vital in bridging communication gaps and enhancing coordination.
By providing a comprehensive summary of an individual's condition, the chief complaint SOAP note not only aids clinical reasoning but also serves as a legal document of the care delivered. This structured approach is crucial for improving healthcare delivery. It allows for better documentation practices, ultimately leading to more effective treatment plans and continuity of care.
As we navigate the complexities of healthcare, consider how combining these records with advanced AI diagnostic tools can personalize treatment strategies. This integration addresses the challenges posed by fragmented communication in healthcare.
Key Benefits of Structured Notes:
- Enhances clarity in communication among healthcare providers.
- Supports clinical reasoning with thorough documentation.
- Facilitates continuity of care for individuals.
Let’s work together to embrace these practices, ensuring that we provide the best possible care for those we serve. Your commitment to improving documentation can make a significant difference in the lives of individuals seeking care.
Break Down the Components: Subjective, Objective, Assessment, and Plan
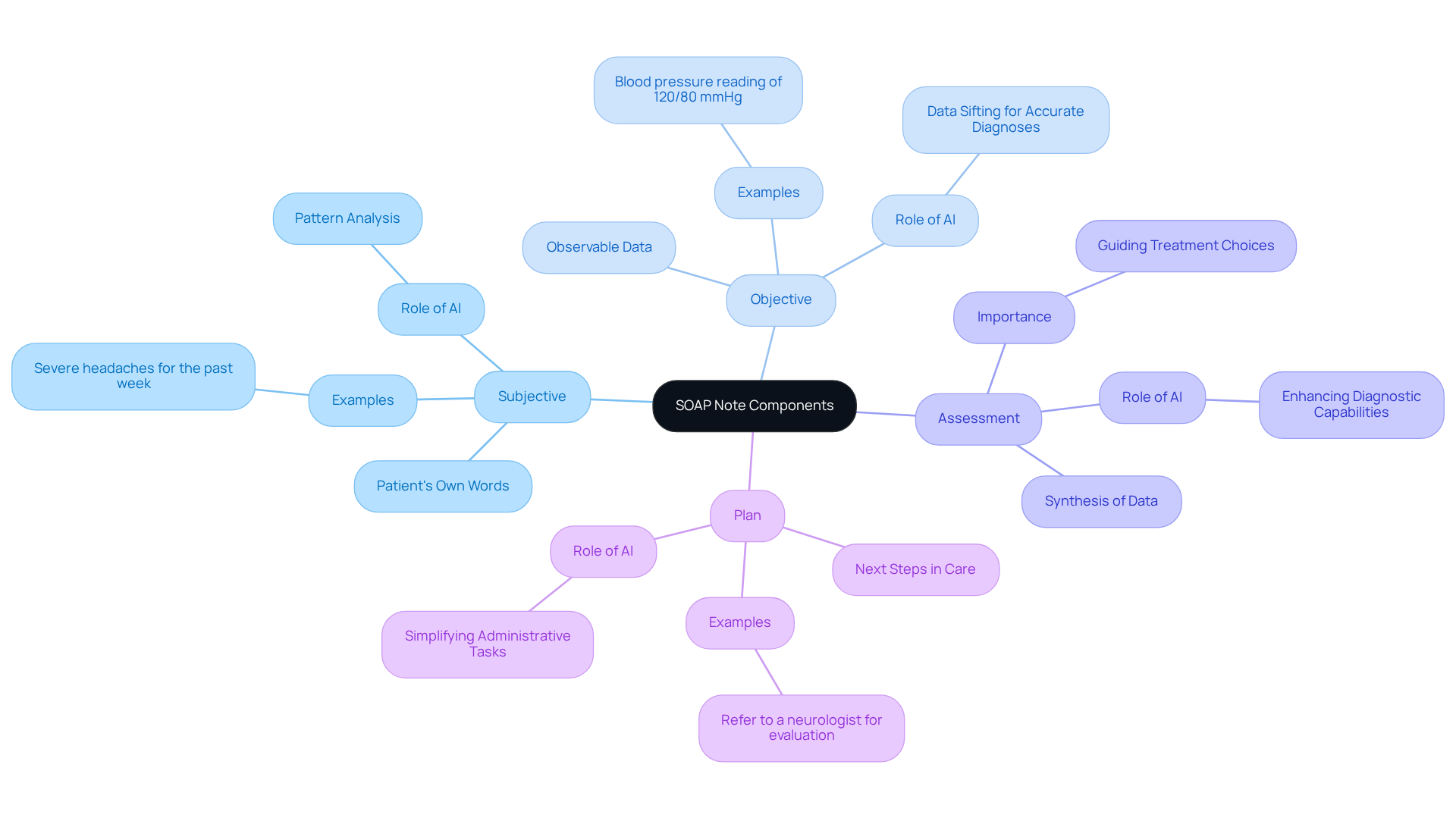
Each component of a SOAP note plays a vital role in clinical practice, and understanding these can truly enhance patient care:
-
Subjective: This section captures the patient’s own words about their symptoms, feelings, and experiences. For instance, when someone says, "I have been experiencing severe headaches for the past week," it provides essential context for the clinician. Have you ever noticed how AI algorithms can help analyze this reported data? They can identify patterns that deepen our understanding of a patient’s condition.
-
Objective: Here, clinicians document observable and measurable data, like vital signs and lab results. For example, a blood pressure reading of 120/80 mmHg is recorded, offering concrete evidence to support clinical assessments. Imagine how AI can sift through vast amounts of medical data, including these objective measures, to assist physicians in making accurate diagnoses and crafting personalized treatment plans.
-
Assessment: This section synthesizes both subjective and objective data, which is essential for the chief complaint soap note leading to a diagnosis or differential diagnosis. It’s where the clinician analyzes the collected information, summarizing the individual’s condition and guiding treatment choices. By utilizing advanced algorithms, physicians can enhance their diagnostic capabilities, ultimately improving outcomes for patients and reducing stress levels.
-
Plan: The final section outlines the next steps in care, such as further tests, treatments, or referrals. For instance, a note might read, "Refer to a neurologist for further evaluation of headaches," ensuring a clear path forward for the patient. Generative AI can simplify administrative tasks related to the plan, like scheduling follow-ups and managing referrals, allowing physicians to focus more on what truly matters—patient care.
Grasping these elements is crucial for crafting an effective documentation process, such as a chief complaint soap note, that enhances care. When combined with AI technologies, we can boost diagnostic precision and alleviate administrative burdens. Let’s embrace these tools together to improve our practice and, most importantly, the lives of those we serve.
Step-by-Step Process to Write a Chief Complaint SOAP Note
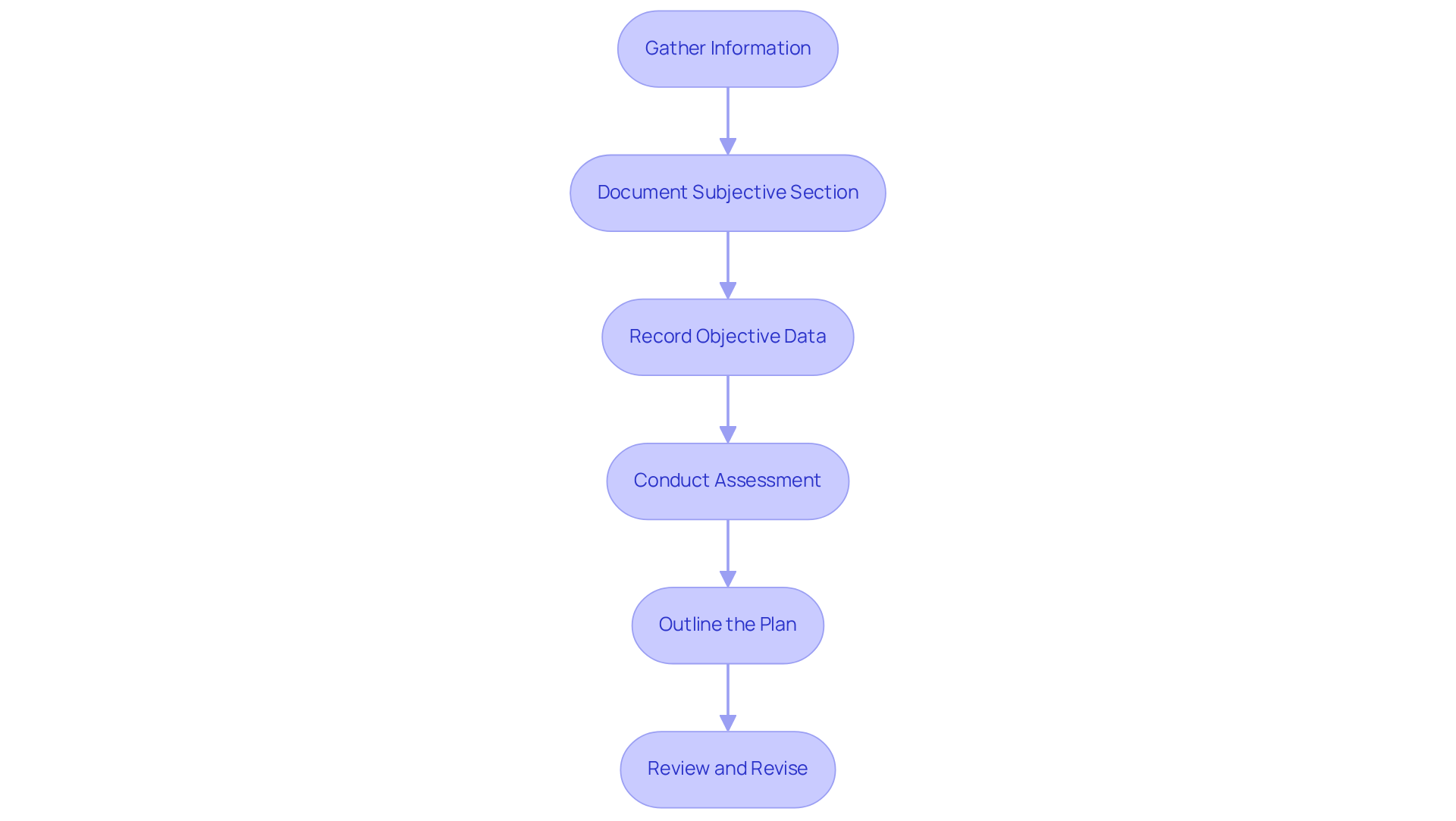
Writing a chief complaint SOAP note can feel overwhelming, particularly when you're managing multiple responsibilities. But by following a few structured steps, you can create effective documentation that truly reflects your patient’s needs.
-
Gather Information: Begin by collecting comprehensive information about the individual, focusing on their chief complaint SOAP note and relevant medical history. This foundational step is crucial for understanding their unique situation.
-
Document the Subjective Section by capturing the individual’s chief complaint SOAP note in their own words. Include additional subjective details, like the duration and severity of symptoms. This section is vital for grasping their perspective and context, allowing you to connect with their experience.
-
Record Objective Data: Measure and document objective findings, such as vital signs and results from physical examinations or diagnostic tests. This factual data supports your assessment and provides a clearer picture of the individual’s health.
-
Conduct an Assessment: Analyze both the subjective and objective data to formulate a clinical assessment. This step may involve identifying potential diagnoses based on the information gathered, ensuring a thorough understanding of the individual’s condition.
-
Outline the Plan: Clearly articulate the next steps in the individual’s care. Detail any treatments, referrals, or follow-up actions required. This plan should align with your assessment findings, ensuring continuity of care and fostering trust.
-
Review and Revise: After composing the document, take a moment to examine it for clarity and completeness. Ensure that all sections are accurately filled out and that the message thoroughly represents the individual’s situation.
By adhering to these procedures, you can enhance communication among team members and improve the chief complaint SOAP note for overall patient care. Remember, common mistakes to avoid include excessive detail that obscures key points and failing to support subjective statements with objective data. As the Social Work Portal Change Management Team wisely states, "Your progress records should demonstrate not only personal change but also enhancements in the client’s living conditions, access to resources, and overall wellness within their surroundings."
Keeping records concise and focused will lead to better documentation practices. Additionally, utilizing resources like SimplePractice can simplify the writing process, enabling you to manage your records effectively. How can you streamline your documentation to better serve your patients?
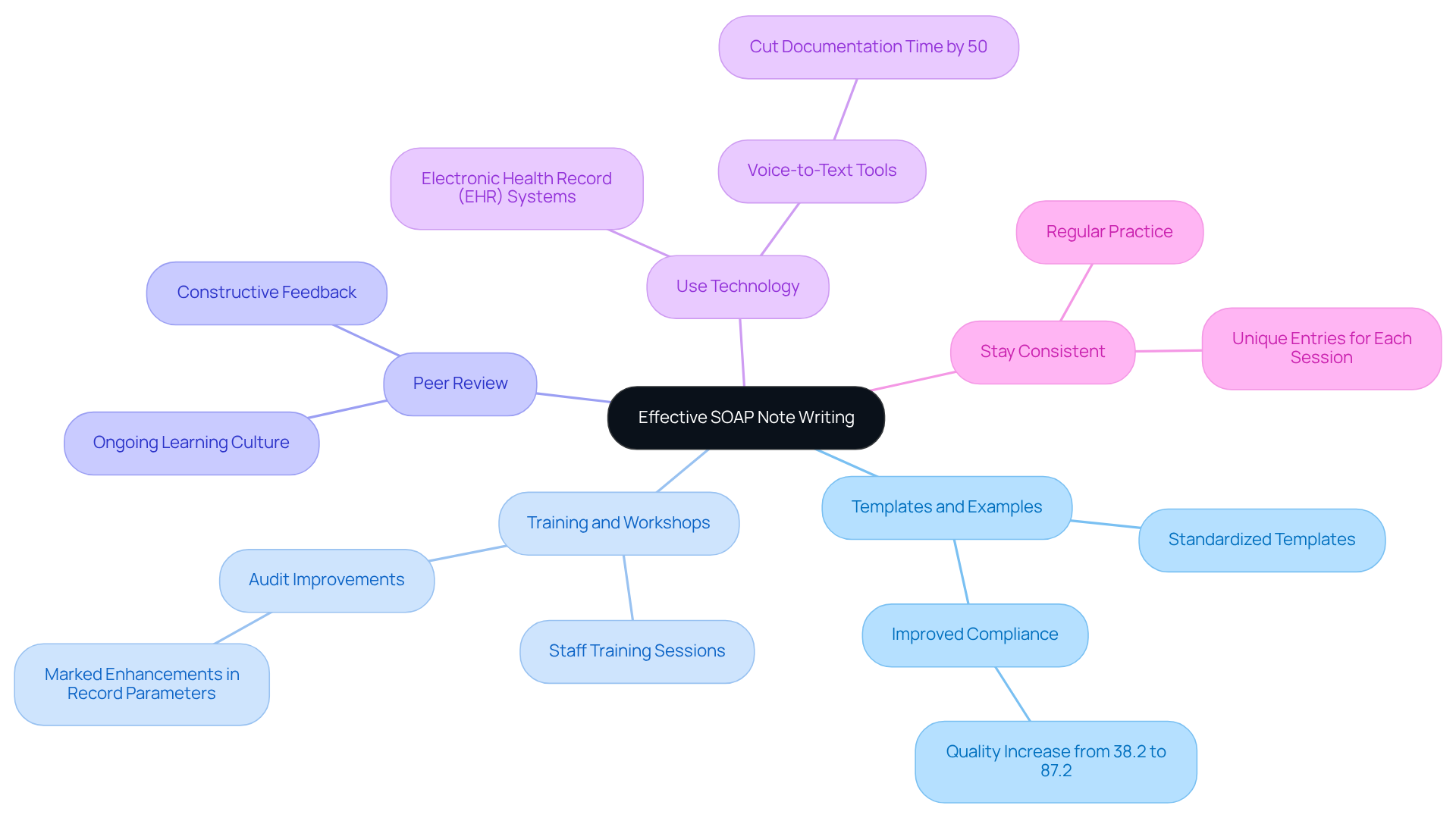
Utilize Resources and Best Practices for Effective SOAP Note Writing
To enhance your SOAP note writing, it’s important to recognize the emotional challenges you face in your daily practice. The administrative burdens can often feel overwhelming, impacting the quality of patient care you strive to provide. But there are effective resources and best practices that can help you navigate these challenges with confidence.
-
Templates and Examples: Consider utilizing online SOAP note templates to guide your documentation process. These templates clarify the structure and ensure that critical elements are consistently included, enhancing the overall quality of your written materials. Research shows that employing standardized templates can significantly improve compliance rates, with record quality increasing from 38.2% to 87.2% after implementation.
-
Training and Workshops: Engaging in training sessions or workshops focused on medical record-keeping can be incredibly beneficial. These initiatives have demonstrated improvements in record-keeping practices, as audits often reveal marked enhancements in record parameters following staff training.
-
Peer Review: Participating in peer review sessions allows you to receive constructive feedback from coworkers on your documentation. This collaborative approach helps identify areas for improvement and fosters a culture of ongoing learning, which is essential for maintaining high record-keeping standards.
-
Use Technology: Embrace electronic health record (EHR) systems that offer integrated SOAP documentation templates and prompts. These tools simplify the recording process, reduce errors, and enhance the detail and narrative flow of your records. For instance, voice-to-text tools can cut recording time by fifty percent, allowing you to focus more on patient care.
-
Stay Consistent: Regularly practicing your SOAP entries is key to developing a consistent style and approach. Consistency ensures clarity and precision in documentation, which is vital for effective healthcare and legal protection. Aim for concise records that accurately reflect the individual’s condition and treatment strategy, ensuring each entry is unique to the session.
By utilizing these resources and adhering to best practices, you can significantly improve the quality and effectiveness of your SOAP notes. This, in turn, enhances patient care and fosters better communication among healthcare teams. Remember, you’re not alone in this journey—embracing these strategies can make a meaningful difference in your practice.
Conclusion
Mastering the chief complaint SOAP note is crucial for healthcare professionals who genuinely care about enhancing patient care and communication. Have you ever felt overwhelmed by the administrative burdens that can distract from patient interactions? By adopting the structured SOAP format—Subjective, Objective, Assessment, and Plan—providers can document vital information clearly and effectively. This approach bridges communication gaps that often exist in fragmented healthcare systems, ensuring that every patient’s voice is heard.
This systematic method not only sharpens clinical reasoning but also serves as a legal record of care. It reinforces the importance of thorough documentation in delivering quality healthcare. Imagine the clarity that structured notes can bring to your practice! Key benefits include:
- Enhanced clarity in communication
- Support for clinical reasoning
- Facilitation of continuity of care
Each component of the SOAP note plays a critical role in understanding a patient’s condition. From capturing their subjective experiences to documenting objective findings and outlining a clear plan for care, every detail matters. By following a step-by-step process to write these notes and utilizing resources like templates and technology, healthcare professionals can significantly improve their documentation practices.
Ultimately, embracing the SOAP note framework and its best practices is about more than just compliance—it's about committing to better patient outcomes and fostering a culture of effective communication among healthcare teams. By prioritizing structured documentation, you can ensure that you’re not only meeting legal and professional standards but also enhancing the quality of care you deliver. The journey toward improved documentation is ongoing, and by adopting these strategies, you can make a meaningful impact on your practice and the lives of your patients. Let’s take this step together for a brighter future in healthcare.




