Overview
This article addresses the emotional challenges healthcare providers face when mastering the abdominal pain SOAP note. It emphasizes a structured approach that includes four essential components: Subjective, Objective, Assessment, and Plan. By gathering thorough patient information and practicing clear documentation, providers can alleviate some of the administrative burdens that often impact patient care.
Moreover, integrating technology, such as AI, can significantly enhance clinical efficiency and improve patient outcomes. Imagine how much more effective your practice could be with streamlined processes that allow you to focus on what truly matters—your patients.
We understand that the demands of healthcare can be overwhelming. However, by adopting these strategies, you not only foster a more organized practice but also create a nurturing environment for your patients.
Consider taking the next step towards refining your approach. Engage with the tools and techniques discussed here to transform your SOAP note mastery into a seamless part of your patient care routine. Together, we can make a meaningful difference in the lives of those we serve.
Introduction
Mastering the art of effective patient documentation is essential for healthcare providers, especially when addressing common complaints like abdominal pain. It’s understandable to feel overwhelmed by the demands of documentation, but the SOAP note framework can be a guiding light. This approach not only streamlines the documentation process but also fosters communication and continuity of care among medical professionals.
But how can clinicians ensure that their SOAP notes are both comprehensive and clear? This is a question that resonates deeply with many in the field. By focusing on the essential steps for mastering the abdominal pain SOAP note, healthcare providers can enhance their practice and strengthen patient-provider relationships.
Imagine the positive impact on patient outcomes when documentation is clear and effective. This article delves into these vital steps, empowering you to elevate your practice. Together, let’s explore how we can improve our documentation and ultimately, the care we provide.
Understand the SOAP Note Framework
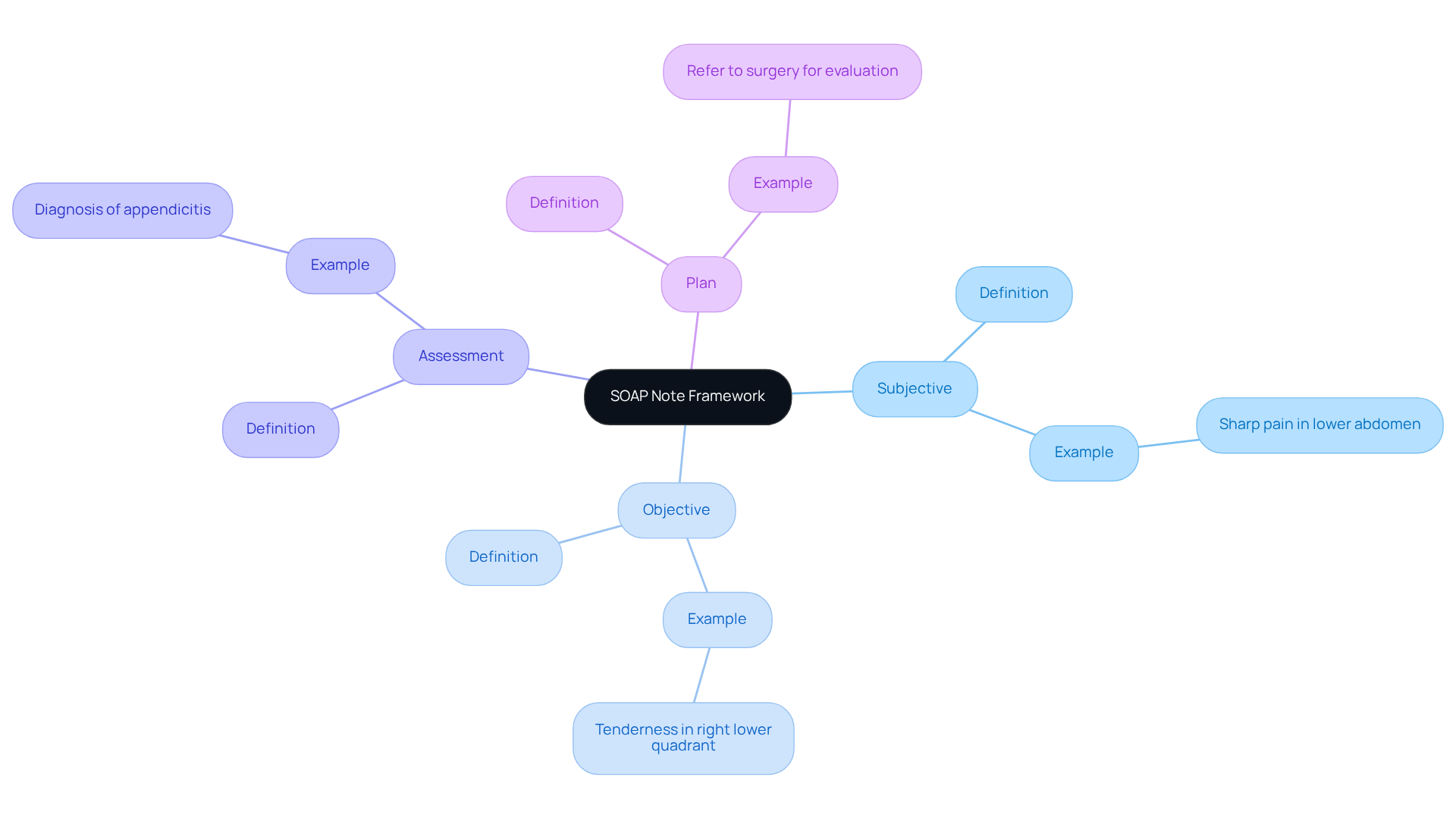
The SOAP note framework serves as a crucial element of effective patient documentation in healthcare, encompassing four essential components that support both clinicians and patients alike:
-
Subjective (S): This section captures the individual's personal experience of their symptoms, detailing aspects such as discomfort description, onset, duration, and associated symptoms. For instance, a patient might share, 'I have sharp pain in my lower abdomen that started two days ago,' which should be recorded in the abdominal pain SOAP note.
-
Objective (O): Here, clinicians document observable and measurable data, including vital signs, physical examination findings, and diagnostic test results. An example would be noting tenderness in the right lower quadrant of the abdomen.
-
Assessment (A): This component involves the clinician's interpretation of the subjective and objective data, leading to a clinical impression or diagnosis. For instance, the evaluation may determine that the individual has appendicitis based on the gathered information.
-
Plan (P): The plan outlines the next steps in management, such as further tests, treatments, or referrals. An example might state, "Refer to surgery for evaluation and possible appendectomy."
The significance of SOAP notes in healthcare cannot be overstated. They not only provide a structured method for documentation but also enhance communication among medical providers, ensuring continuity of care. Have you ever considered how vital these notes are to fostering strong patient-provider relationships? Research indicates that approximately 80% of medical providers utilize SOAP notes for client encounters, reflecting their effectiveness in clinical practice. Moreover, many medical professionals have found that starting with the assessment and plan can improve the clarity and usability of notes, ultimately benefiting client outcomes.
By mastering the SOAP note framework, clinicians can significantly enhance the quality of care they provide. Additionally, the integration of generative AI in generating SOAP notes has allowed clinicians to save 6-10 minutes per visit, underscoring the efficiency benefits of adopting this framework. AI simplifies the documentation process, enabling medical professionals to focus more on client interactions and less on administrative tasks. This shift not only enhances the quality of care but also addresses the fragmentation often seen in healthcare systems, improving communication and coordination for better outcomes.
The APSO format (Assessment, Plan, Subjective, Objective) has also been positively received by clinicians, with studies showing that 80% of clinicians were 'satisfied' or 'very satisfied' with this alternative format. This approach improves speed, task success, and usability during chronic disease visits. Embracing these frameworks and technologies can lead to a more compassionate and efficient healthcare experience for both providers and patients.
Gather Patient Information for Abdominal Pain
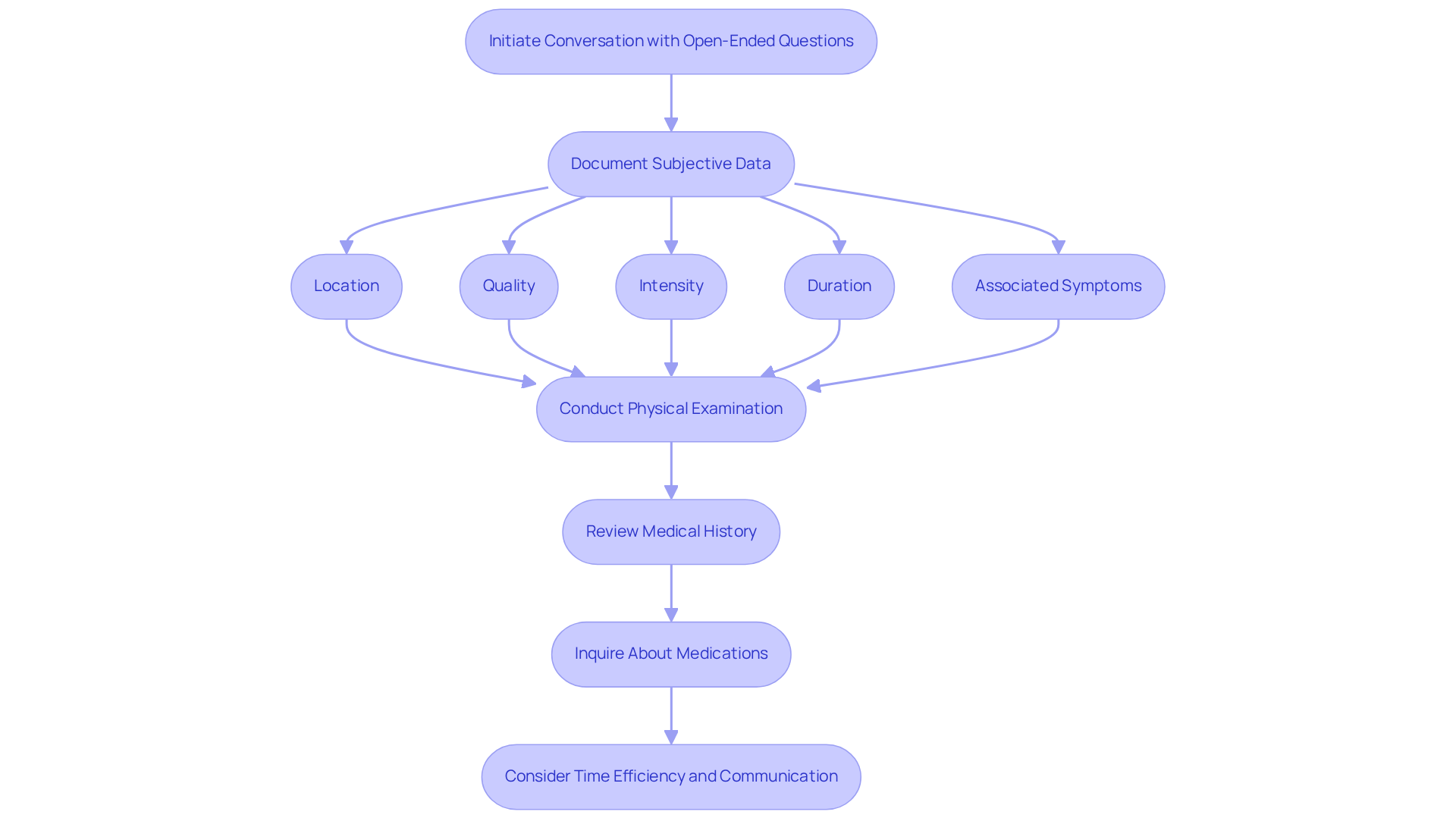
Gathering patient information effectively for the abdominal pain soap note assessment is crucial for providing compassionate care. Start by initiating the conversation with open-ended questions that allow individuals to express their symptoms. For instance, you might ask, "Can you explain the discomfort you're feeling?" This approach fosters a supportive environment.
Next, document the subjective data carefully, focusing on key aspects that matter to the patient. Consider the following:
- Location: Where is the pain located? (e.g., right lower quadrant)
- Quality: How would you describe the discomfort? (e.g., sharp, dull, cramping)
- Intensity: On a scale of 1 to 10, how severe is the pain?
- Duration: When did the pain start, and how long has it lasted?
- Associated Symptoms: Are there any additional symptoms, such as nausea, vomiting, or changes in bowel habits?
Conduct a physical examination next. A focused abdominal exam can reveal tenderness, distension, or abnormal bowel sounds. Be sure to document these findings in the Objective section of the abdominal pain soap note.
As you gather information, review the individual's medical history. Understanding past medical issues, surgeries, or relevant family history can provide valuable insights into their current condition.
Additionally, inquire about medications. Knowing whether the individual is taking any medications that could influence their symptoms or treatment options is essential for comprehensive care.
Time efficiency is also vital. The average time spent gathering client information can significantly impact the assessment process. Effective communication, potentially enhanced by generative AI tools, can foster trust and improve client satisfaction. Studies indicate that 80% of individuals prefer digital communication with their healthcare providers.
By systematically gathering this information and leveraging generative AI to streamline administrative tasks, you will create a comprehensive picture of the individual's condition, essential for accurate assessment and planning. Remember, as Don Berwick states, "Truly listening to individuals and incorporating their feedback is fundamental to enhancing the experience of those seeking care.
Analyze Data and Formulate Clinical Impressions
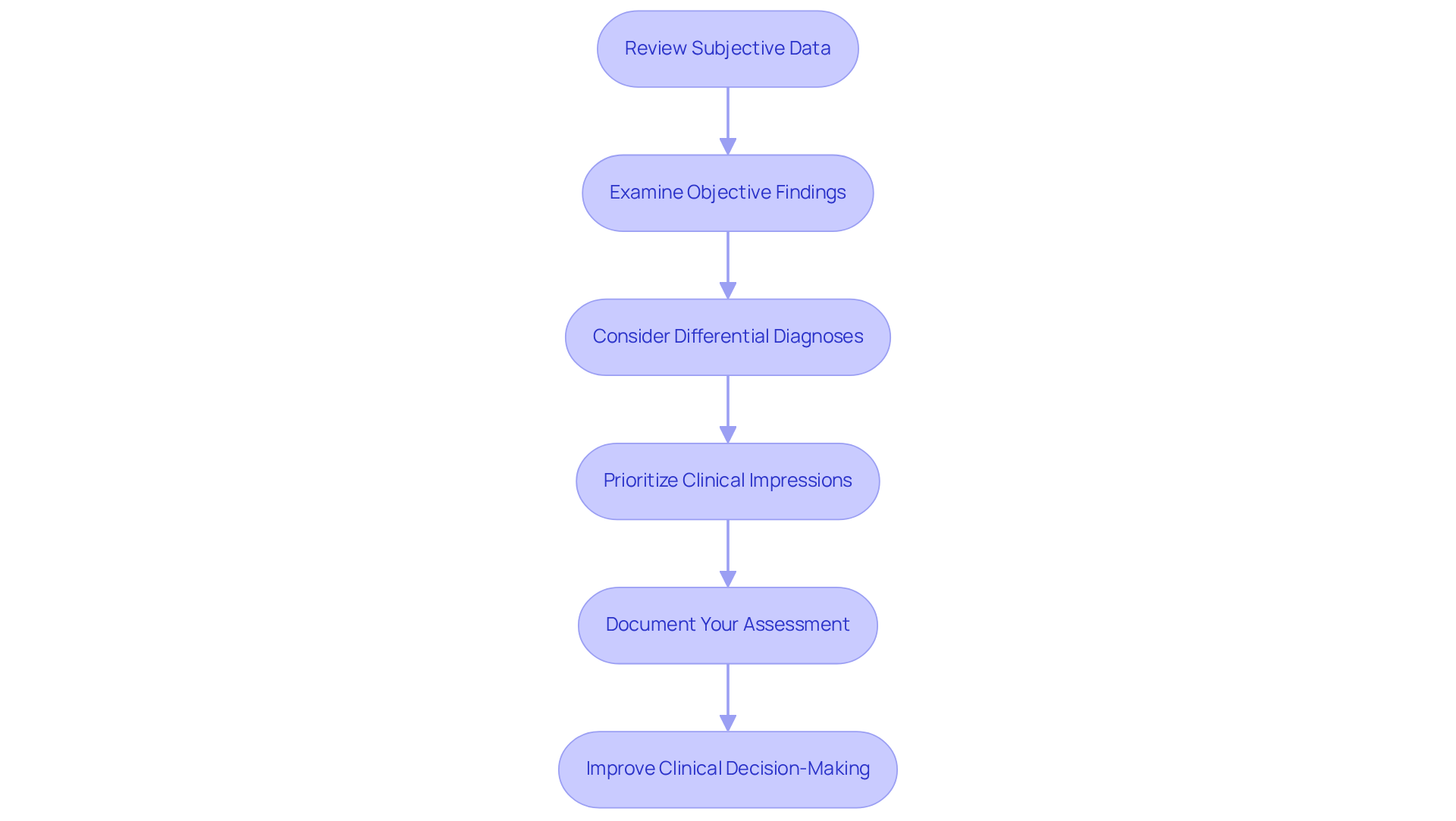
To effectively analyze patient data and formulate clinical impressions regarding abdominal pain, it is essential to follow these structured steps with care:
-
Review the Subjective Data: Begin by identifying patterns in the patient's pain description. Consider the onset and duration of pain, the quality and intensity of the pain, and any alleviating or aggravating factors. How might these details reflect the patient's experience?
-
Examine the Objective Findings: Next, correlate physical examination results with the subjective data. For instance, if a patient reports intense discomfort in the right lower abdomen and tenderness is noted during examination, appendicitis could be a probable diagnosis. This connection is vital for understanding the patient's condition.
-
Consider Differential Diagnoses: Compile a thoughtful list of potential diagnoses based on the integrated data. Common differential diagnoses for abdominal pain include:
- Appendicitis
- Gallstones
- Gastroenteritis
- Peptic ulcer disease
- Stercoral colitis, which can present with vague symptoms and may mimic diverticulitis. Reflecting on these possibilities can help clarify the situation.
-
Prioritize Clinical Impressions: Rank the differential diagnoses according to their likelihood and severity. This prioritization is crucial for guiding treatment plans and determining necessary referrals. Utilizing AI algorithms can assist in examining extensive medical data, including individual history and symptoms, to improve diagnostic precision and develop customized treatment plans. How can technology enhance our understanding?
-
Document Your Assessment: Clearly articulate your clinical impression in the Assessment section of the SOAP note. Ensure it reflects a comprehensive synthesis of both subjective and objective data. Emphasizing thorough documentation is essential, as clinical impressions were absent in 23.4% of cases, underscoring the importance of capturing all critical elements. This step is vital for continuity of care.
By carefully examining the data, healthcare providers can improve their clinical decision-making, ultimately enhancing care outcomes. As noted by John C. Beauchamp, the abdominal pain soap note is one of the most frequent chief complaints encountered in emergency departments, accounting for 5-10% of all presentations. This structured method not only assists in precise diagnosis but also promotes effective dialogue with individuals about their conditions, transforming outcomes through advanced algorithms. Together, we can navigate these challenges with compassion and expertise.
Document Findings and Recommendations Clearly
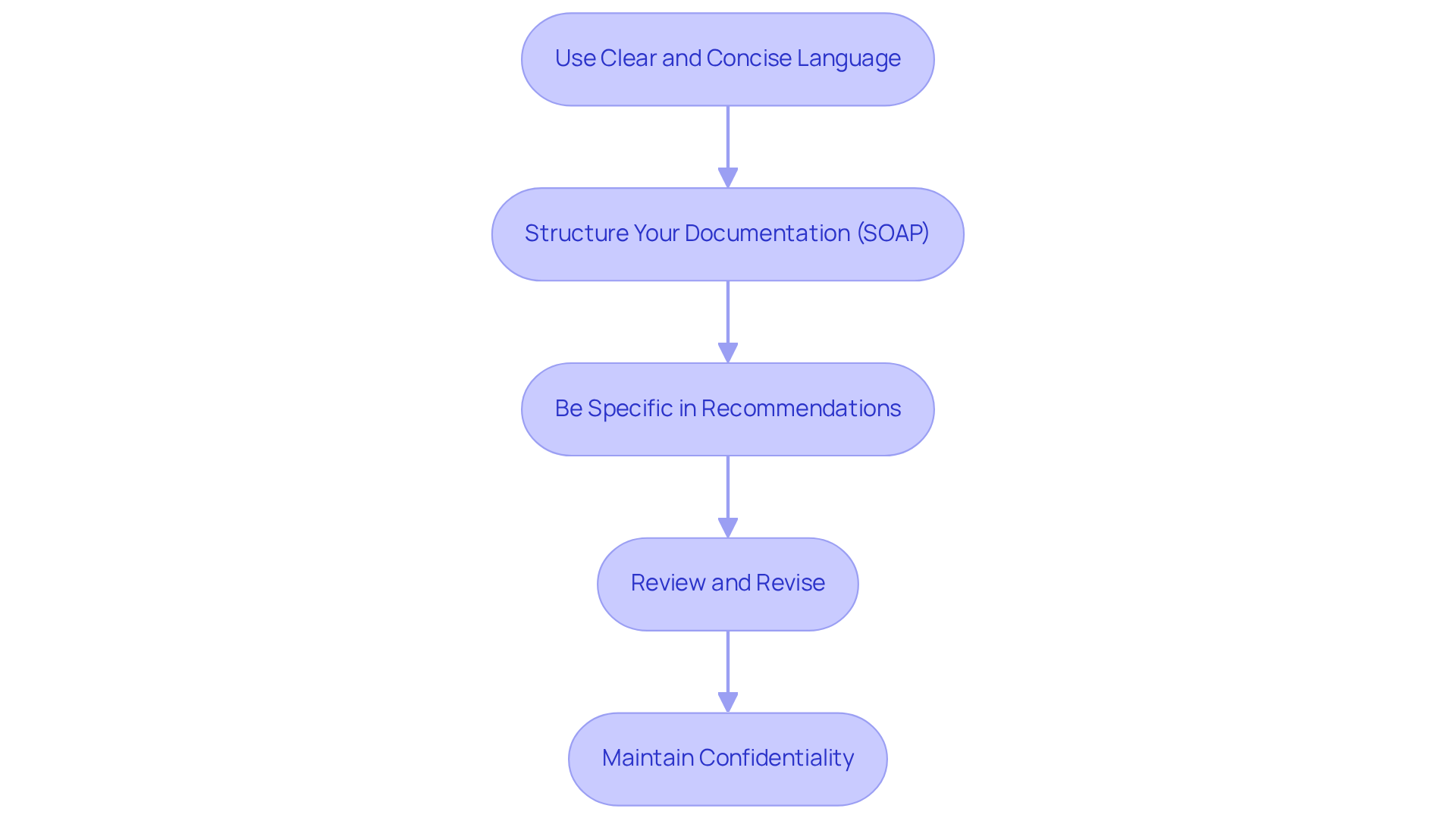
To document your findings and recommendations clearly, it's essential to follow these compassionate guidelines:
-
Use Clear and Concise Language: Avoid jargon to ensure your documentation is understandable to all healthcare providers. For example, instead of stating 'the individual exhibits abdominal discomfort,' you should include an abdominal pain soap note that specifies 'the individual reports sharp pain in the right lower quadrant.' This precision not only enhances communication but also reduces the risk of misinterpretation, fostering a better understanding among colleagues.
-
Structure Your Documentation: Adhering to the SOAP format can help maintain consistency and clarity:
- Subjective: Summarize the patient's reported symptoms.
- Objective: Detail your physical examination findings and any relevant test results.
- Assessment: Clearly state your clinical impression and any differential diagnoses.
- Plan: Outline the next steps, including any tests, treatments, or referrals. For instance, "Order an abdominal pain soap note to assess for appendicitis." Organized records significantly enhance the quality of clinical notes, with studies showing a mean quality score of 87 for electronic health records (EHR) compared to 44 for prior handwritten documentation, highlighting the effectiveness of structured methods.
-
Be Specific in Recommendations: When outlining your plan, provide specific recommendations. Rather than saying 'monitor the individual,' specify 'reassess in 2 hours and consider surgical consultation if symptoms worsen.' This level of detail ensures actionable steps are clear, which is crucial for effective patient management and demonstrates your commitment to their care.
-
Review and Revise: Before finalizing your written materials, take a moment to review for clarity and completeness. Ensure that all relevant information is included and that your recommendations are actionable. Regular chart reviews have been shown to improve record-keeping practices and clinician awareness of essential information. Health experts trained in standard practice recording were found to be 4.2 times more likely to document their practices, underscoring the importance of training in enhancing the quality of records.
-
Maintain Confidentiality: Always ensure that all records comply with HIPAA regulations, preserving individual confidentiality. This is not only a legal necessity but also crucial for establishing trust with your clients, reinforcing the compassionate care you provide.
By adhering to these guidelines, you will produce clear and effective materials that improve communication and aid in high-quality patient care. Remember, efficient record-keeping methods can lead to increased reimbursement rates and reduced claims denials, as effective practices are linked to higher reimbursement rates for medical facilities. Proper documentation is essential for nearly every aspect of the healthcare industry, as emphasized by experts like Kamran Shafii. Your dedication to clear communication not only benefits your practice but also profoundly impacts the lives of your patients.
Conclusion
Mastering the abdominal pain SOAP note is crucial for healthcare professionals dedicated to delivering high-quality patient care. The structured framework of SOAP—Subjective, Objective, Assessment, and Plan—supports thorough documentation, ensuring that both clinicians and patients enjoy clear communication and continuity of care. This approach not only improves the accuracy of clinical impressions but also nurtures a more compassionate healthcare environment.
Have you ever felt overwhelmed by the administrative tasks that take time away from patient interactions? Throughout this article, we’ve explored the importance of each component of the SOAP note. From effectively gathering patient information to analyzing data and documenting findings, every step is vital in forming a comprehensive understanding of the patient's condition. Utilizing generative AI tools can further ease this burden, allowing clinicians to devote more attention to patient care rather than paperwork. Additionally, the positive reception of the APSO format highlights the ongoing evolution of documentation practices in healthcare.
Ultimately, embracing the SOAP note framework and its variations is essential for enhancing patient outcomes and improving the overall healthcare experience. By prioritizing clear communication and effective documentation, healthcare providers can not only fulfill regulatory requirements but also build trust and rapport with their patients. The journey to mastering the abdominal pain SOAP note transcends mere documentation; it is about cultivating a culture of care that acknowledges the unique needs of every individual seeking assistance.
Reflect on how adopting this framework can transform your practice. Are you ready to embrace this journey toward compassionate care?




