Overview
In the demanding world of speech therapy, mastering the SOAP note format—Subjective, Objective, Assessment, and Plan—is crucial for enhancing documentation and treatment outcomes. Have you ever felt overwhelmed by the administrative tasks that take time away from your patients? Each component of the SOAP note framework not only contributes to clearer communication but also allows for more effective tracking of client progress. This clarity can significantly improve the quality of care you provide.
Consider how the SOAP note format can alleviate some of the burdens you face. By organizing your thoughts and observations systematically, you can focus more on what truly matters: your clients. This structured approach fosters an environment where you can nurture your patients' growth and development, ultimately leading to better outcomes.
As you embrace this framework, think about the benefits it brings. Enhanced documentation leads to a more comprehensive understanding of each client's journey, making it easier to identify areas for improvement. When you have a clear plan in place, you can provide the compassionate care your clients deserve.
Let’s work together to refine our practices. By prioritizing the SOAP note format, we can not only streamline our documentation but also enhance the therapeutic experience for our clients. Are you ready to take this step toward better care?
Introduction
In the intricate landscape of speech therapy, effective documentation is essential for ensuring quality care and fostering communication among professionals. Have you ever felt overwhelmed by the demands of thorough documentation while striving to connect meaningfully with your clients? The SOAP note format—comprising Subjective, Objective, Assessment, and Plan—emerges as a powerful tool to streamline this process. It allows clinicians to track client progress and tailor interventions with precision, ultimately enhancing the care provided.
Yet, the challenge remains: how can speech therapists balance these administrative burdens with the need for genuine client interaction? This article delves into mastering the art of SOAP notes, offering a step-by-step approach designed to enhance both efficiency and effectiveness in clinical practice. Together, we can navigate these challenges and improve our impact on the lives of those we serve.
Understand the SOAP Note Format in Speech Therapy
In the demanding world of speech therapy, the speech therapy soap note—standing for Subjective, Objective, Assessment, and Plan—serves as a vital framework for documenting client development and treatment. Each component plays a crucial role in fostering clarity and consistency in clinical notes, which directly influences the quality of care and communication among healthcare professionals.
Have you ever felt overwhelmed by the administrative tasks that can detract from patient interaction? By standardizing documentation, the SOAP format not only simplifies the recording process but also significantly improves the ability to track progress over time.
Consider this: a client produced 8 out of 10 /s/ sounds correctly during articulation drills, showcasing the effectiveness of this structured approach. This systematic method allows healthcare providers to make informed adjustments to care strategies as needed, ultimately leading to better outcomes for individuals. Effective documentation practices, as highlighted by the American Speech-Language-Hearing Association, affirm that speech therapy soap notes are essential for justifying the client’s need for speech-language therapy while conveying case history and treatment trajectory.
It is also beneficial to note that SOAP notes typically range between 100-300 words, striking a balance between thoroughness and brevity. Have you documented your SOAP notes right after sessions? This practice is essential for maintaining accuracy, ensuring that vital details are captured without omission. By embracing this comprehensive approach, we can truly appreciate the importance of standardized documentation in healthcare, fostering a supportive environment for both providers and clients.
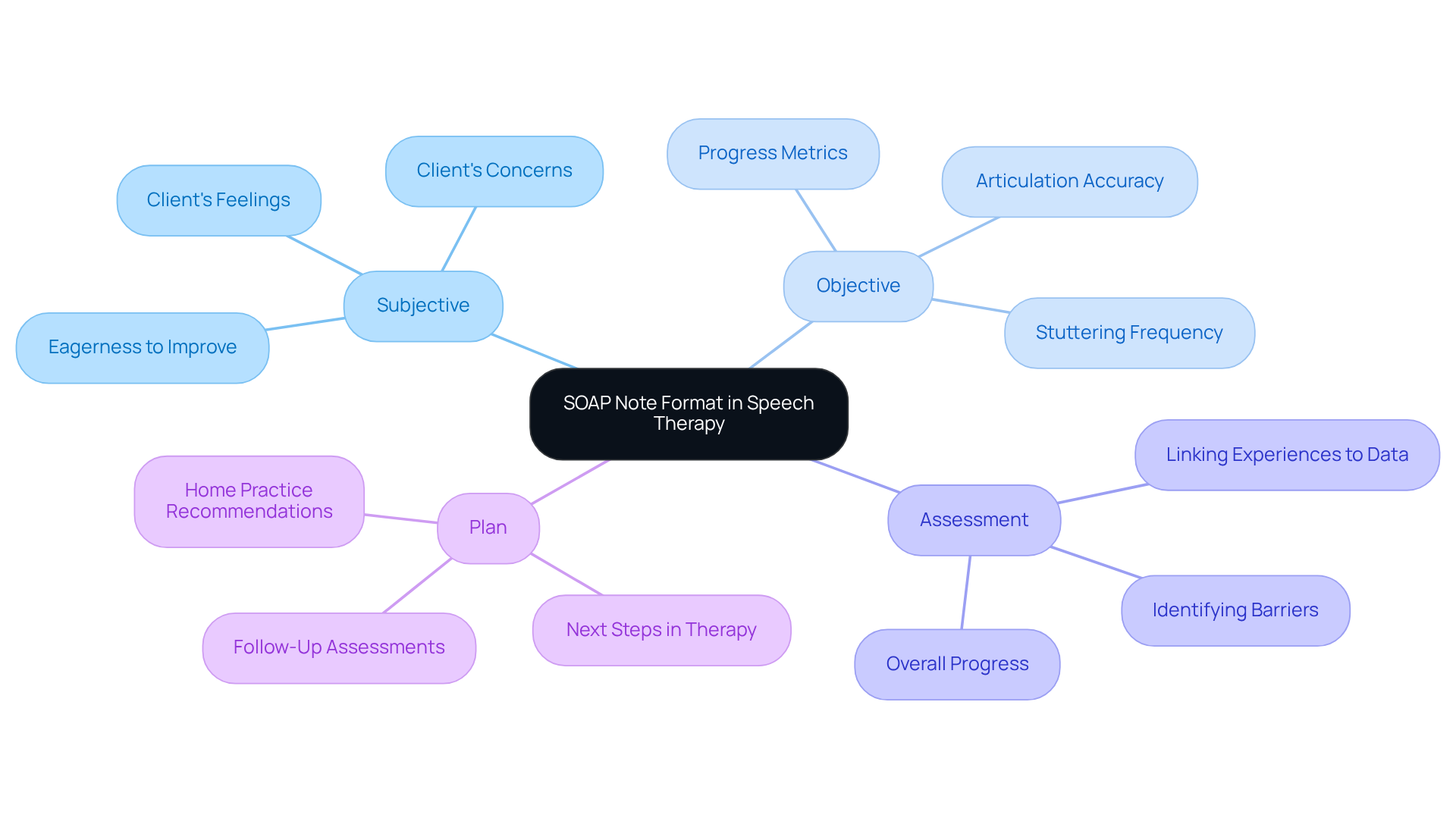
Break Down the Components: Subjective, Objective, Assessment, and Plan
-
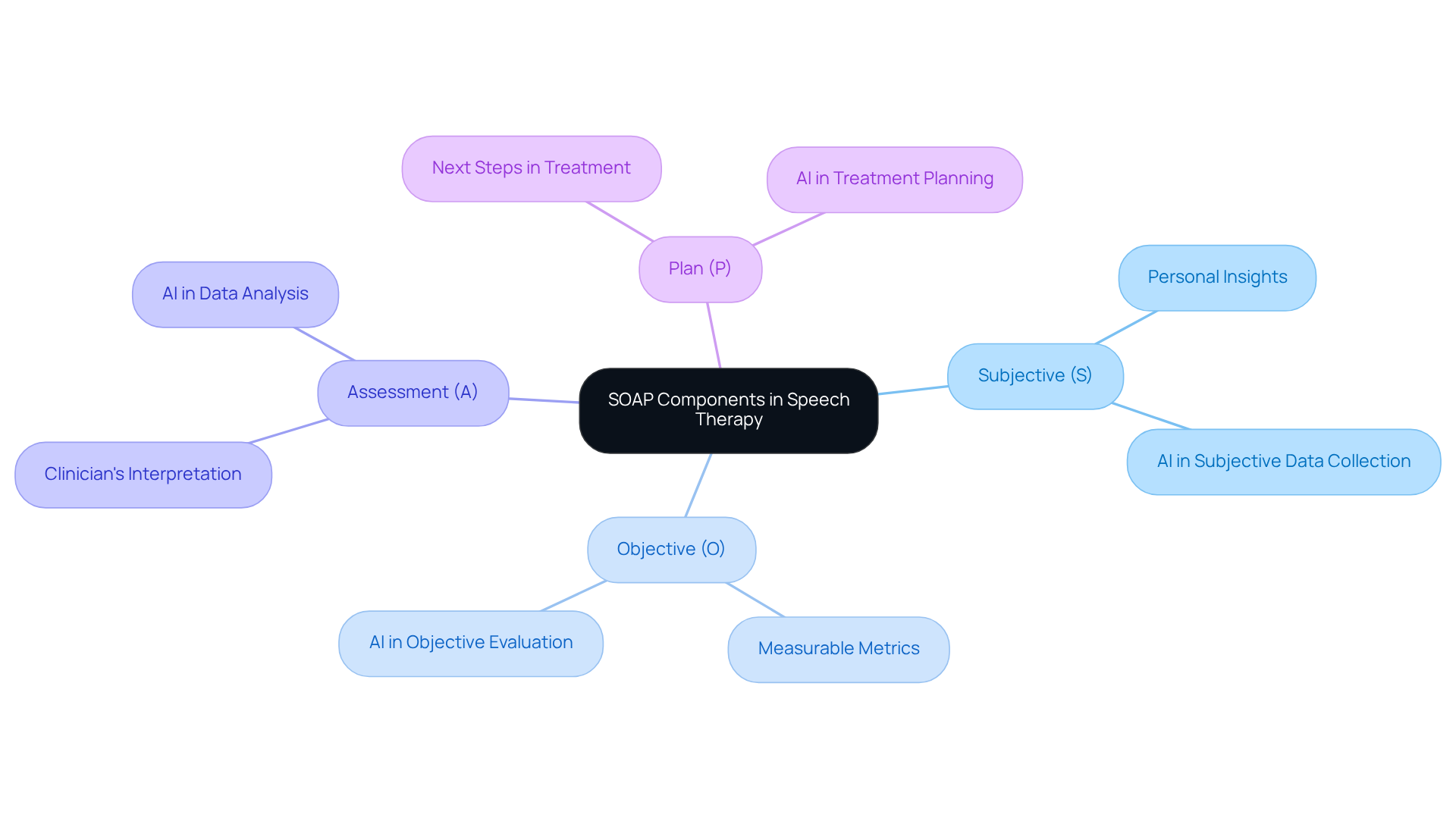
Subjective (S): This segment captures the individual's expressions regarding their feelings, symptoms, and concerns. For instance, an individual might share, "I feel more confident speaking in front of others." Such personal insights are essential as they provide valuable perspectives on the individual's emotional state, significantly impacting treatment outcomes. By utilizing smart engagement tools driven by generative AI, clinicians can enhance the collection of subjective information for the speech therapy soap note, ensuring that individual voices are accurately represented and understood.
-
Objective (O): In this part, the clinician records measurable data and observations from the session. This may include outcomes from standardized evaluations, the individual's performance on specific tasks, or observable behaviors. For example, one might note, "The patient correctly articulated 80% of target words during the session," providing a clear metric for evaluating progress. AI can assist in evaluating these metrics more effectively, allowing for timely adjustments to care strategies based on real-time information documented in the speech therapy soap note.
-
Assessment (A): This section involves the clinician's interpretation of both subjective and objective data. It encompasses examining the individual's progress and evaluating the effectiveness of the treatment strategy. An example could be, "The individual shows improvement in articulation but continues to struggle with fluency," which aids in customizing future interventions. Generative AI can offer insights by recognizing patterns in individual data, enhancing the clinician's ability to make informed assessments while alleviating some of the administrative burdens linked to data analysis, much like a speech therapy soap note simplifies documentation.
-
Plan (P): The plan outlines the next steps in the treatment process. This may involve setting specific goals for the upcoming session, modifying the therapy approach, or recommending home practice strategies. For instance, one might state, "Continue with articulation exercises and introduce fluency techniques in the next session," ensuring a structured path forward in therapy. By incorporating AI tools, like telemedicine platforms, clinicians can optimize the planning process in their speech therapy soap note, ensuring that each individual's unique needs are addressed efficiently.
Including the perspectives of individuals is crucial, as studies have demonstrated a connection between language impairment and mental health challenges, such as anxiety and depression. As highlighted by a notable expert in the field, "Confidence is not in perfect speech, but in the courage to speak," emphasizing the importance of fostering a supportive atmosphere for individuals. Additionally, the collaborative nature of therapy can be illustrated through case studies like the "Client-Therapist Partnership," which highlights the mutual effort required for success.
Write Each Section: Tips for Subjective, Objective, Assessment, and Plan
-
Subjective: When possible, use direct quotes from the individual to truly capture their feelings. For instance, a client might express, "Talking about my childhood made me realize how much it still impacts me today." This approach not only validates their experiences but also aligns seamlessly with the objectives outlined in the speech therapy soap note. Keep the language concise, relevant, and easily understandable, avoiding jargon.
-
Objective: Be specific and utilize measurable terms. Incorporate numerical information where appropriate, such as percentages or scores from assessments. For example, noting that an individual improved their speech clarity by 20% after specific exercises should be documented in the speech therapy soap note, providing a solid foundation for your evaluation. Observational studies have revealed risk differences ranging from 1.2% to 1.8%, closely matching randomized trial estimates of 1.7%.
-
Assessment: Synthesize both subjective and objective data to deliver a clear analysis. Employ clinical reasoning to articulate the individual’s progress or challenges. Rather than vague statements, focus on specific areas of improvement or concern in the speech therapy soap note, such as changes in speech rate or articulation accuracy. For instance, when evaluating velopharyngeal function, effective assessment recorded in a speech therapy soap note can lead to targeted interventions that significantly enhance speech quality.
-
Plan: Clearly outline the next steps in treatment. Use bullet points for clarity, detailing specific goals and timelines. For example, establishing a goal for the individual to achieve a 30% enhancement in speech fluency within the next month is crucial and should be documented in the speech therapy soap note to underscore the importance of tailored care and quantifiable results.
Review Examples of Effective Speech Therapy SOAP Notes
-
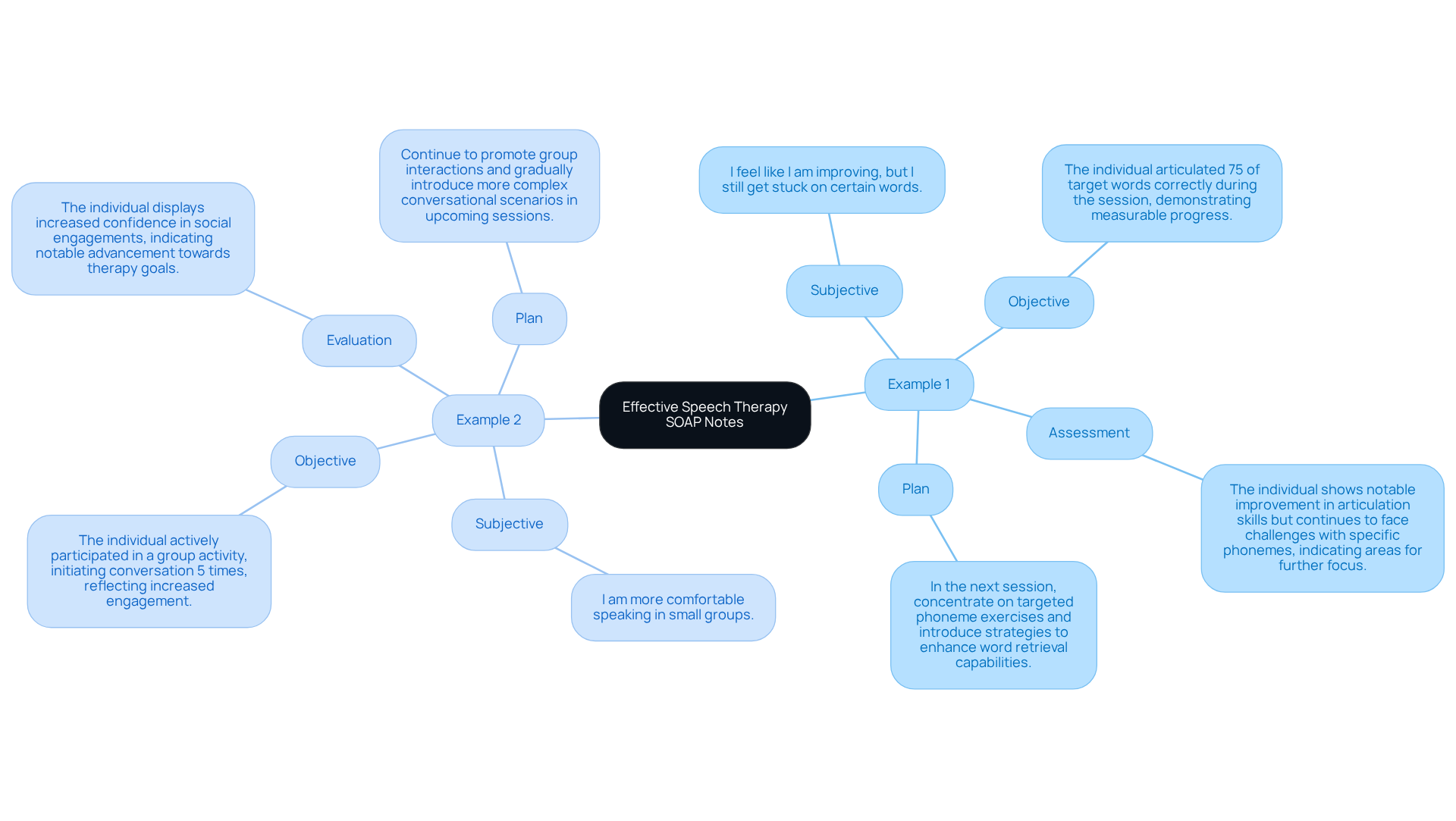
Example 1:
- Subjective: "I feel like I am improving, but I still get stuck on certain words."
- Objective: "The individual articulated 75% of target words correctly during the session, demonstrating measurable progress."
- Assessment: "The individual shows notable improvement in articulation skills but continues to face challenges with specific phonemes, indicating areas for further focus."
- Plan: "In the next session, concentrate on targeted phoneme exercises and introduce strategies to enhance word retrieval capabilities."
-
Example 2:
- Subjective: "I am more comfortable speaking in small groups."
- Objective: "The individual actively participated in a group activity, initiating conversation 5 times, reflecting increased engagement."
- Evaluation: "The individual displays increased confidence in social engagements, indicating notable advancement towards therapy goals."
- Plan: "Continue to promote group interactions and gradually introduce more complex conversational scenarios in upcoming sessions."
These examples highlight the essential role of effective documentation, including the speech therapy soap note, in monitoring patient development and customizing treatment plans. By doing so, we can ultimately achieve better outcomes as documented in the speech therapy soap note.
Have you ever felt overwhelmed by administrative tasks? It’s a common challenge that many healthcare providers face, often leading to burnout and limiting the time available for patient-centered care.
Imagine a world where generative AI streamlines the documentation process, reducing these burdens. This technology allows healthcare providers to focus more on their patients, fostering a nurturing environment. As noted by Piera Willner, MS, CCC-SLP, "Every client is different and has different needs, so you’ll need to adapt the content of your note based on what happens in your individual sessions." This adaptability is enhanced by generative AI, ensuring timely and accurate speech therapy soap note documentation.
Ultimately, these advancements reinforce the importance of measurable data in assessing client progress and tailoring interventions. Let’s embrace these solutions together to improve not just our documentation, but the overall quality of care we provide.
Conclusion
Mastering speech therapy SOAP notes is truly significant, as they serve as a crucial tool for documenting client progress and treatment strategies. By following the structured framework of Subjective, Objective, Assessment, and Plan, speech therapists can improve communication among healthcare professionals and ensure that each client's unique needs are met with care.
Each component of the SOAP notes plays an essential role:
- Subjective insights offer a personal glimpse into the client's emotional state.
- Objective data provides measurable outcomes that reflect their progress.
- The Assessment section combines this information to evaluate treatment effectiveness.
- The Plan outlines actionable steps for future sessions.
Together, these elements create a comprehensive picture of client development, ensuring that therapy remains tailored and responsive.
Incorporating standardized documentation practices not only streamlines administrative tasks but also enhances the quality of care provided to clients. As the field of speech therapy evolves, embracing innovative tools like generative AI can further improve the efficiency and accuracy of SOAP note documentation. By prioritizing effective communication and meticulous record-keeping, speech therapists can foster a supportive environment that empowers clients to achieve their goals.
How can we better support our clients through effective documentation? By recognizing the emotional challenges faced by healthcare providers and addressing the administrative burdens that impact patient care, we can create a more nurturing atmosphere. Let's continue to engage with one another, share best practices, and embrace solutions that enhance our ability to serve our clients compassionately.




