Overview
This article addresses the emotional challenges healthcare providers encounter when documenting back pain cases. It emphasizes the weight of administrative burdens and how they can detract from the quality of patient care. By focusing on mastering SOAP notes—Subjective, Objective, Assessment, and Plan—it offers a structured approach that not only enhances documentation accuracy but also alleviates some of the stress that contributes to clinician burnout.
Have you ever felt overwhelmed by the sheer volume of paperwork? You're not alone. Many healthcare professionals find themselves caught in a cycle of documentation that feels never-ending. This article highlights the pivotal role of generative AI tools, which can streamline the documentation process. Imagine being able to focus more on your patients rather than getting lost in administrative tasks.
By integrating these tools, we can improve patient care significantly. Enhanced documentation efficiency leads to more accurate assessments and tailored treatment plans, ultimately fostering a better healthcare experience for both providers and patients. This is not just about reducing burnout; it's about reclaiming the joy in patient interactions.
As you explore the insights shared here, consider how these strategies can be implemented in your practice. The journey to mastering SOAP notes is not just a professional obligation; it’s a step towards nurturing your well-being and enhancing the care you provide. Let's take this journey together, ensuring that we not only care for our patients but also for ourselves.
Introduction
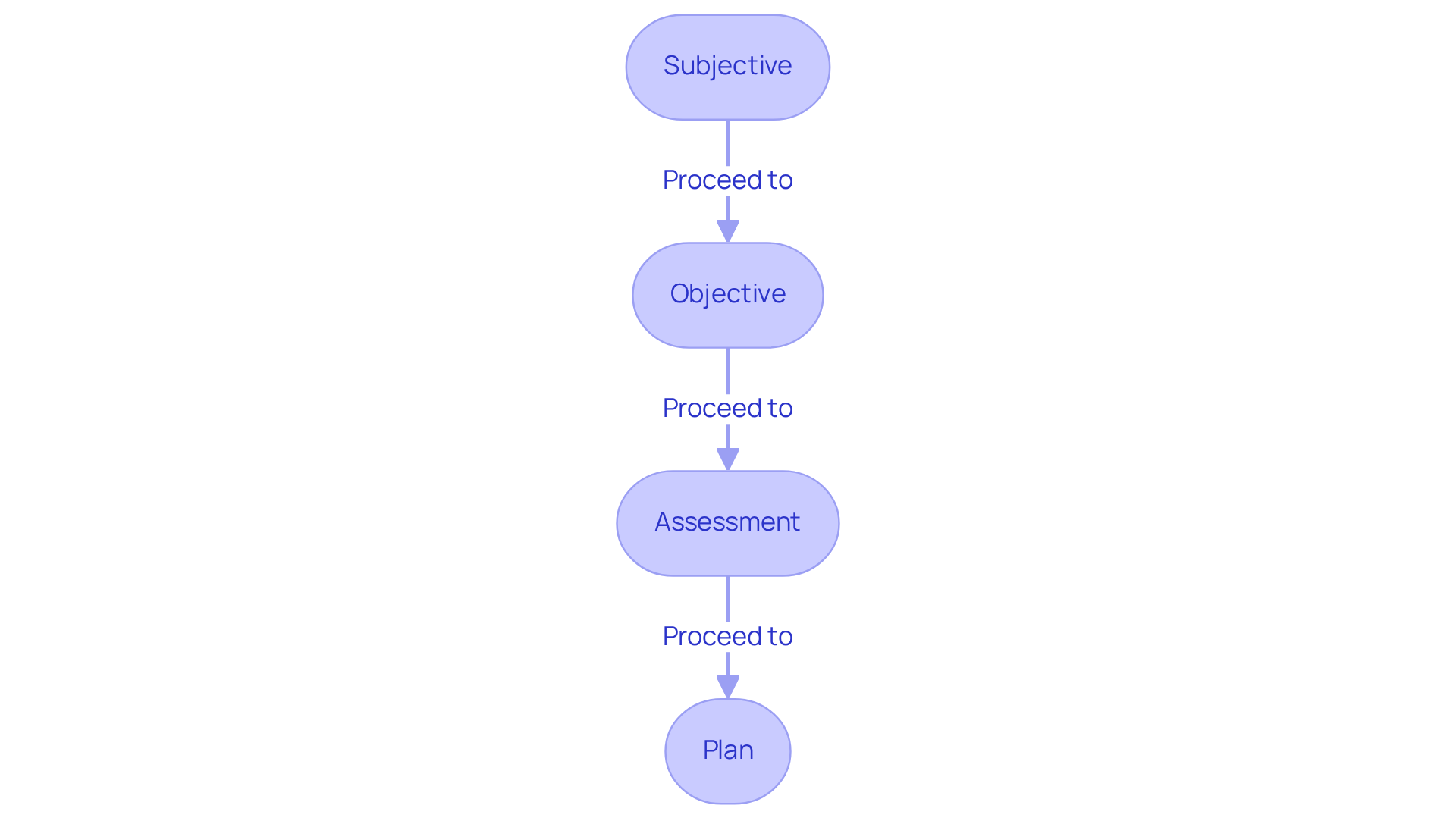
Mastering the SOAP note framework is essential for healthcare professionals dealing with back pain. It offers a structured approach to documenting patient care, which can feel overwhelming at times. By effectively capturing subjective experiences, objective findings, clinical assessments, and treatment plans, practitioners can significantly enhance patient outcomes and streamline communication. Yet, many healthcare providers face challenges in accurately documenting these crucial elements.
How can you leverage the SOAP note format to improve your documentation and ensure better care for your patients? This question is not just about efficiency; it’s about fostering deeper connections with those you serve. Recognizing the emotional challenges you encounter in your practice is the first step towards a more compassionate approach to patient care.
Administrative burdens can weigh heavily on your ability to provide the best care possible. However, by embracing the SOAP note framework, you can alleviate some of this pressure. It allows you to focus on what truly matters—your patients' well-being. Imagine the difference it could make if your documentation not only met requirements but also reflected the care and attention your patients deserve.
We encourage you to explore how the SOAP note format can transform your practice. Together, we can enhance communication, improve patient outcomes, and create a more nurturing environment for both providers and patients alike.
Understand the SOAP Note Framework
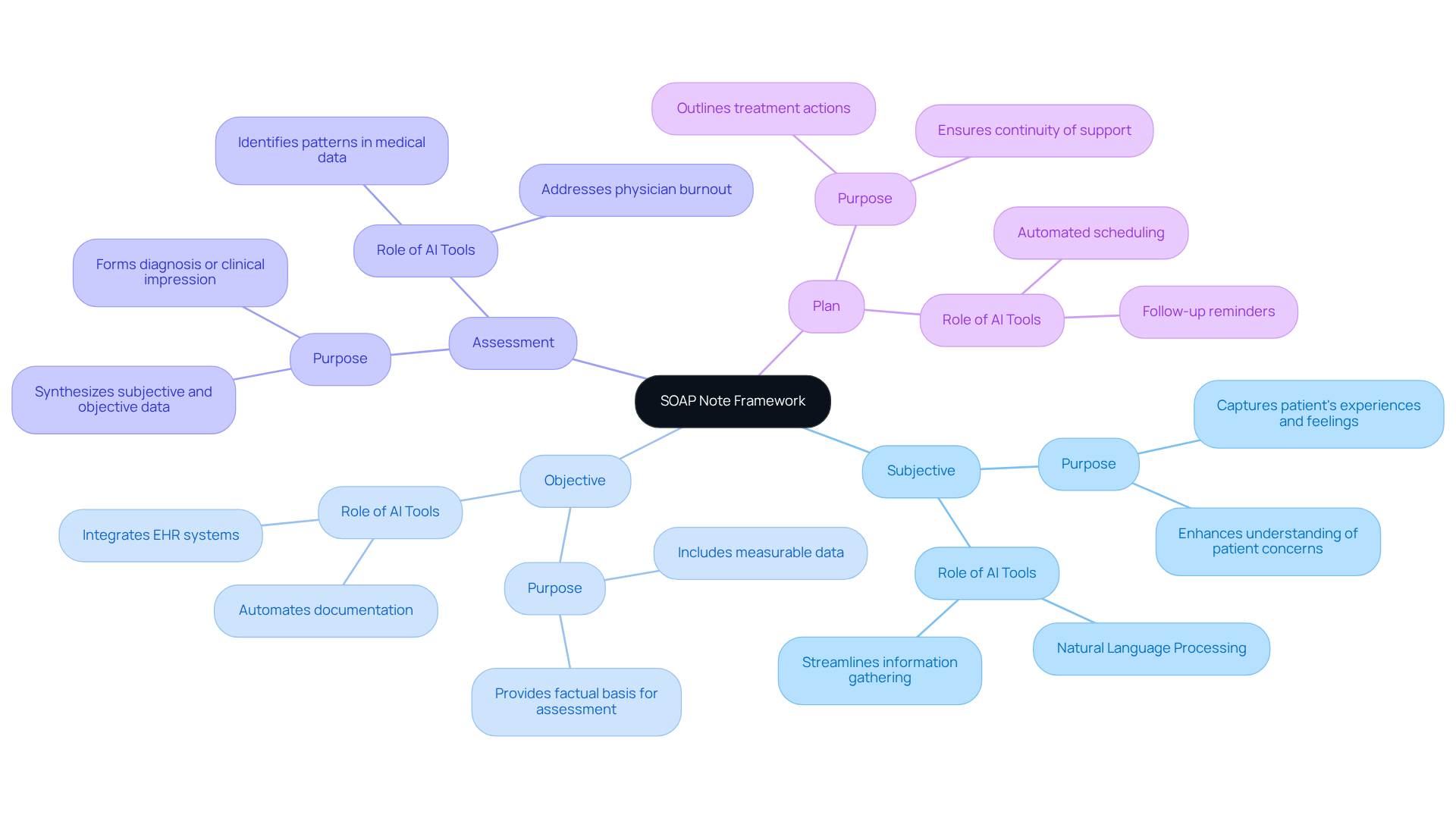
SOAP stands for Subjective, Objective, Assessment, and Plan. Each component serves a distinct purpose, essential for compassionate patient care.
-
Subjective (S): This section captures the patient's personal experiences, symptoms, and feelings regarding their condition. Understanding these narratives is crucial for grasping the individual's viewpoint and concerns. Generative AI tools, like natural language processing applications, can help streamline the gathering of subjective information. This ensures that patients’ stories are accurately captured and analyzed, enhancing their overall experience.
-
Objective (O): This part includes measurable data such as vital signs, physical examination findings, and diagnostic test results. It provides a factual basis for the clinician's assessment. AI tools can assist in automating the documentation of objective data, such as integrating electronic health records (EHR) systems. This reduction in administrative burden allows healthcare providers to focus more on the needs of their patients.
-
Assessment (A): In this section, clinicians synthesize subjective and objective information to formulate a diagnosis or clinical impression. This reflects the clinician's clinical reasoning. Generative AI can help identify patterns in medical data, potentially leading to more precise evaluations and tailored treatment plans. This approach addresses the pressing issues of physician burnout and labor shortages.
-
Plan (P): This outlines the subsequent actions in the individual's treatment, including therapy options, referrals, and follow-up strategies. It is crucial for ensuring continuity of support. By utilizing AI-driven tools, such as automated scheduling and follow-up reminders, physicians can enhance their planning processes, ensuring that follow-up actions are communicated and executed efficiently.
Understanding this framework is vital for effective documentation and enhances communication among healthcare providers. By incorporating generative AI into clinical documentation, healthcare professionals can ease administrative demands, reduce burnout, and ultimately enhance care for individuals. How can you leverage these tools to support your practice and your patients' well-being?
Explore the Components of a SOAP Note
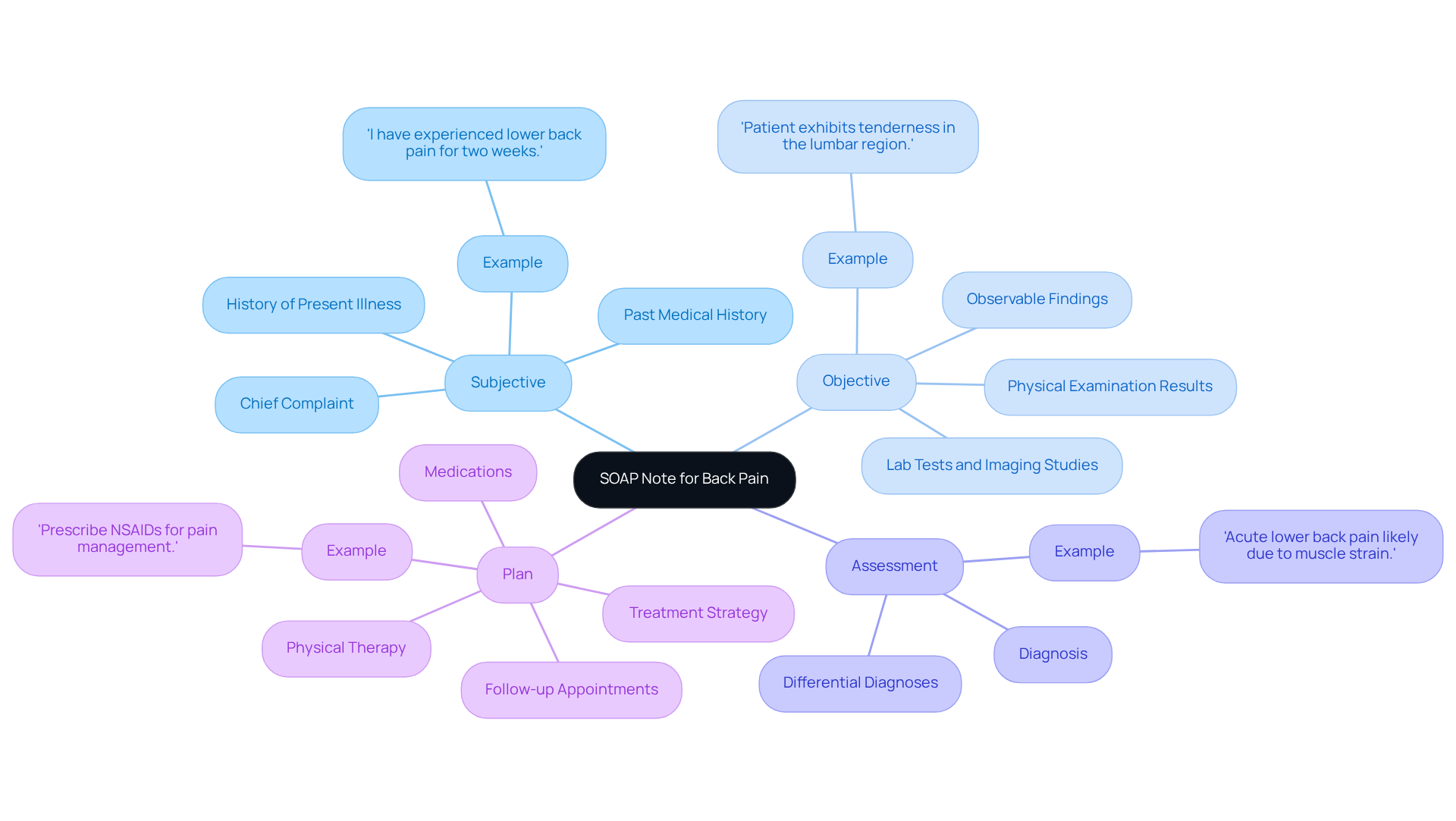
Each component of the soap note for back pain is crucial for effective patient documentation.
Subjective: This section captures the patient's chief complaint, history of present illness, and pertinent past medical history. For instance, an individual might express, 'I have experienced lower back pain for two weeks, and it intensifies when I bend over.' This personal narrative is vital for understanding the individual's experience and guiding clinical assessment.
Objective: Here, observable findings are documented, including physical examination results, lab tests, and imaging studies. An example might state, 'Patient exhibits tenderness in the lumbar region and has a range of motion of 30 degrees.' This section is essential for recording measurable data that validates the patient's reported symptoms and supports the clinician's assessment.
Assessment: This section synthesizes the subjective and objective data to arrive at a diagnosis or differential diagnoses. For example, one might conclude in a soap note for back pain, 'Acute lower back pain likely due to muscle strain.' This analysis is crucial for guiding treatment choices and ensuring continuity of care.
Plan: The treatment strategy outlines the next steps for individual support, including medications, physical therapy, and follow-up appointments. An example could be, 'Prescribe NSAIDs for pain management and refer to physical therapy for strengthening exercises.' This roadmap is essential for guiding future healthcare providers in ensuring comprehensive patient care, which includes the proper documentation of a soap note for back pain.
Research indicates that effective documentation should balance subjective and objective information. Studies show that subjective data often comprises about 60% of the note, while objective data accounts for 40%. This balance is crucial for creating a well-rounded clinical picture. The structured approach of SOAP notes enhances clarity and communication among healthcare providers. As healthcare experts emphasize, clear and concise documentation improves care decisions and adheres to legal requirements. Moreover, considering the APSO format (Assessment, Plan, Subjective, Objective) may enhance usability and speed during client visits. By mastering these components, healthcare providers can create thorough and effective clinical notes that significantly improve outcomes for individuals.
Apply the SOAP Note Format to Back Pain Cases
When documenting a case of back pain with a soap note for back pain, it's essential to approach this task with care and empathy. Many healthcare providers face emotional challenges when managing patient discomfort, and structured documentation can alleviate some of that burden.
-
Subjective: Begin by gathering the individual's account of their discomfort. For instance, you might encounter a patient like a 35-year-old male who reports a sharp discomfort in the lower back that began after lifting heavy boxes. He rates his discomfort as 7 out of 10 on the Visual Analog Scale (VAS) and notes that it worsens with movement. How might this pain be impacting his daily life?
-
Objective: Next, document measurable findings from the physical examination. For example, a physical examination may reveal limited lumbar flexion to 40 degrees (normal range is 60-80 degrees) and tenderness upon palpation of the lower lumbar region. Vital signs are stable, with a blood pressure of 120/80 mmHg. These objective findings are crucial in understanding the patient's condition.
-
Assessment: Then, synthesize the subjective and objective data to formulate a diagnosis. You might conclude, "The patient probably has acute lumbar strain, possibly worsened by recent physical activity, as indicated by the reported discomfort and physical examination findings." This assessment can guide your treatment plan.
-
Plan: Finally, outline a comprehensive treatment strategy. For instance, you could suggest rest, the use of ice for 20 minutes each hour, and over-the-counter analgesics like ibuprofen. It’s also wise to arrange a follow-up appointment in one week to evaluate discomfort levels and functional mobility. What steps can we take to ensure the patient feels supported during their recovery?
Utilizing this soap note for back pain not only enhances the clarity and organization of client information but also aids in effective treatment planning. Research indicates that structured documentation practices can improve client outcomes by 20-30%. This makes it essential for healthcare providers to prioritize thorough and accurate notes.
As one clinician aptly noted, "Thorough documentation protects practitioners legally and ensures consistent communication among healthcare providers" (StatPearls). Additionally, considering alternative formats like APSO (Assessment, Plan, Subjective, Objective) may enhance usability and speed in clinical settings. It’s important to recognize that the clinical model has limitations, such as its inability to record changes over time, which can be crucial in evolving medical situations.
By implementing these best practices, healthcare professionals can significantly enhance the quality of care documented in the soap note for back pain. Together, we can navigate these challenges and provide the compassionate care that our patients deserve.
Avoid Common Mistakes in SOAP Note Documentation
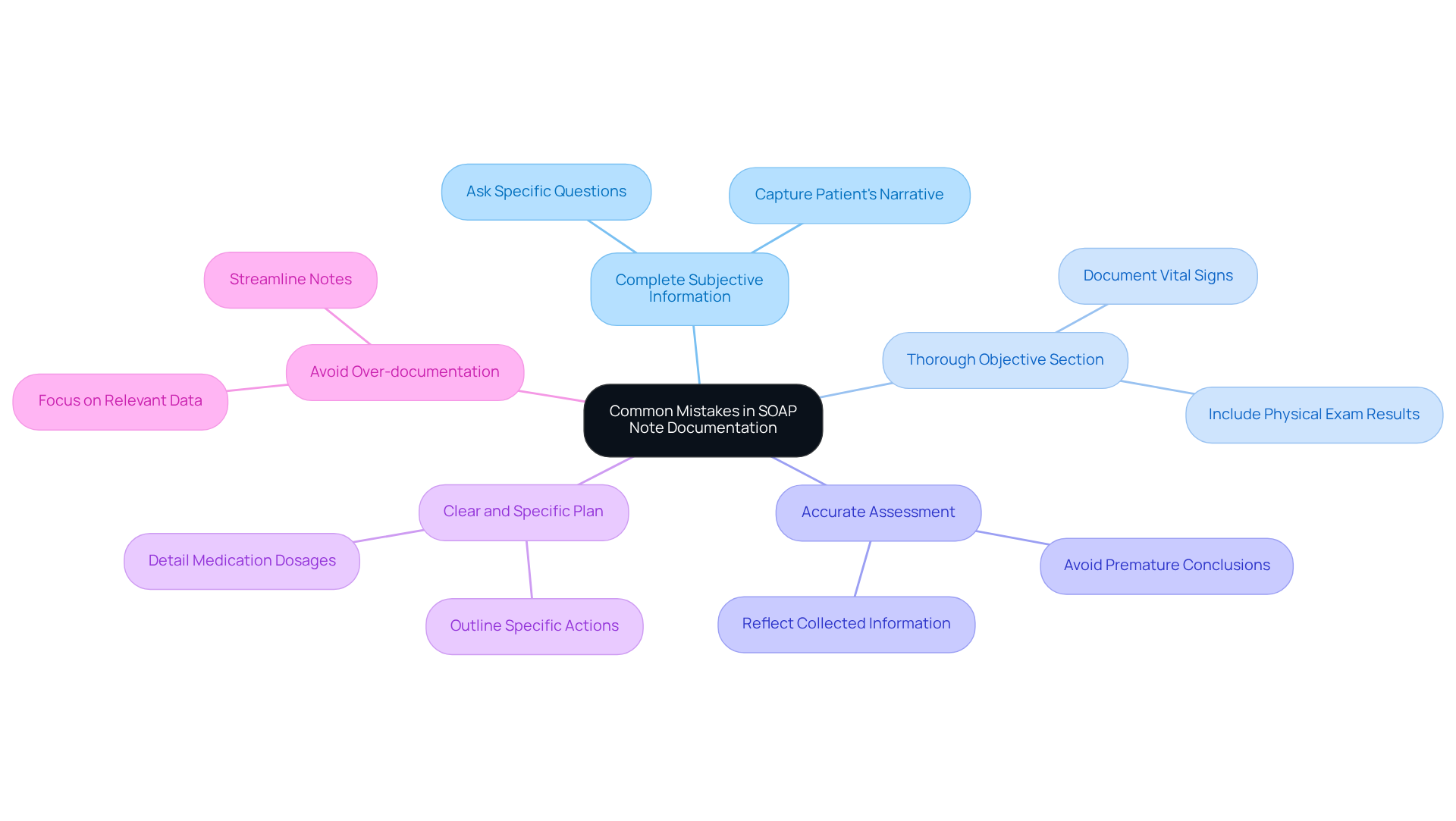
To enhance the quality of SOAP note documentation and avoid common pitfalls, consider these compassionate guidelines:
-
Capture Complete Subjective Information: It’s essential to gather the full narrative of the individual. Instead of vague remarks like "the individual feels bad," ask specific questions that elicit detailed responses reflecting their true experience. For instance, when Connor reported significant improvements in mood, capturing his specific feelings and experiences was crucial in informing his treatment plan.
-
Thorough Objective Section: Document all relevant findings with care. Omitting vital signs or physical examination results can lead to incomplete assessments, impacting the quality of care. As seen in various case studies, lacking essential information can hinder a clinician's understanding of the individual's condition.
-
Accurate Assessment: Your assessment should truly reflect the information collected. Avoid jumping to conclusions without sufficient evidence, as this can misguide treatment decisions. Alex Bendersky highlights that mistakes in SOAP notes can lead to misunderstandings, ultimately affecting outcomes for individuals.
-
Clear and Specific Plan: Articulate a well-defined treatment plan. Rather than stating, "the individual will feel better," outline specific actions, such as medication dosages and follow-up appointments, to ensure clarity in the treatment pathway. This specificity is vital for effective management of individuals receiving care.
-
Avoid Over-documentation: While thoroughness is important, excessive detail can clutter notes and obscure critical information. Focus on relevant data that supports clinical decision-making and enhances clarity. For example, including only the most pertinent observations can streamline the note while maintaining its effectiveness.
By being mindful of these common mistakes, healthcare providers can significantly improve the effectiveness and clarity of their SOAP notes, ultimately enhancing patient care. Remember, every improvement in documentation is a step towards better support for those you care for.
Conclusion
Mastering the SOAP note framework is not just a technical skill; it’s a vital component in the compassionate management of back pain. Understanding and applying the elements of Subjective, Objective, Assessment, and Plan allows healthcare providers to deliver organized care that resonates with patients’ needs. How often do you find that effective communication enhances patient outcomes? By creating comprehensive documentation, practitioners can bridge gaps in understanding and foster a supportive environment.
This guide has highlighted the significance of each SOAP component, illustrating the power of weaving subjective narratives with objective findings into a coherent assessment and actionable plan. Imagine leveraging generative AI tools while adhering to best practices—this approach can alleviate administrative burdens and reduce errors. The balance between subjective and objective data is crucial, as it paints a well-rounded clinical picture that truly reflects patient experiences.
The journey toward effective SOAP note documentation is ongoing, requiring attention to detail and a commitment to improvement. As healthcare providers, how can we strive to enhance our documentation practices? The ultimate goal remains clear: to provide compassionate, patient-centered care that addresses the unique challenges faced by individuals with back pain. Embracing these practices not only leads to better clinical outcomes but also nurtures a supportive environment for both patients and providers alike.




