Overview
Healthcare providers often face emotional challenges in their demanding roles. The article offers a comprehensive step-by-step guide on presenting SOAP notes effectively, which can alleviate some of these burdens. By emphasizing the importance of each component—Subjective, Objective, Assessment, and Plan—it highlights how structured documentation can enhance communication and ultimately improve patient care outcomes.
Consider how administrative tasks can impact your ability to focus on patient care. This guide details how effective documentation not only reduces these burdens but also leads to more accurate diagnoses and treatment strategies. Imagine the relief of having a streamlined process that supports your work and benefits your patients.
This approach fosters a nurturing environment, encouraging healthcare providers to engage with the material. By understanding the significance of each SOAP note component, you can enhance your practice and make a meaningful difference in your patients' lives. We invite you to explore these strategies further and see how they can transform your documentation process.
Introduction
Mastering the art of SOAP note presentation is not just a skill; it’s a vital lifeline for healthcare providers navigating the often overwhelming complexities of patient documentation. This structured approach—comprising Subjective, Objective, Assessment, and Plan—ensures that critical information is communicated effectively, ultimately enhancing patient care and fostering collaboration among providers.
Yet, amidst increasing demands, one might wonder: how can we streamline this process without sacrificing the quality of care? By exploring the intricacies of each component, we not only uncover the transformative power of organized documentation but also address the pressing challenges that many face in today’s healthcare environment.
Together, we can find ways to ease these burdens and improve the experience for both providers and patients alike.
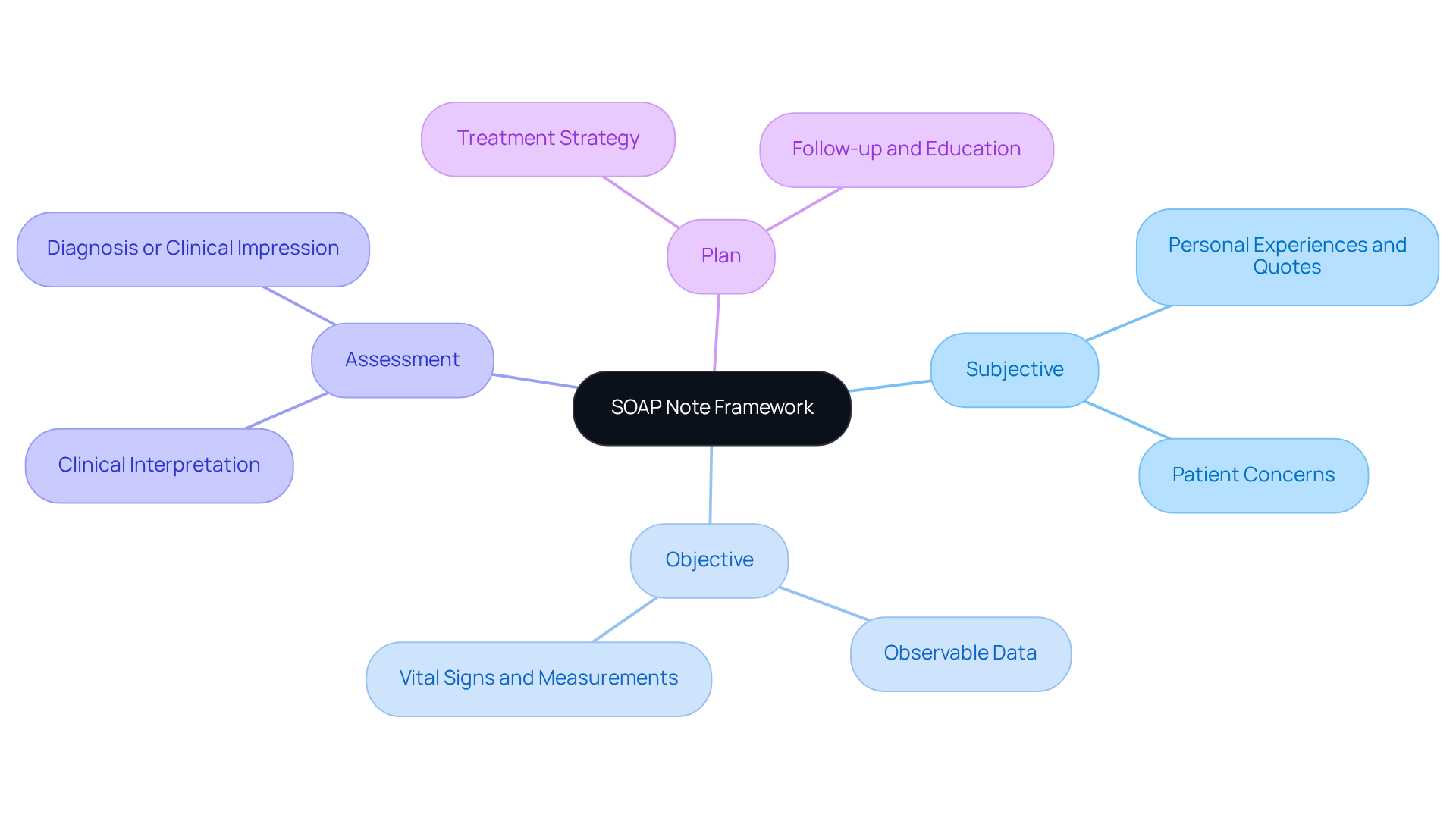
Understand the SOAP Note Framework
The soap note presentation provides a structured method of documentation consisting of four essential components: Subjective, Objective, Assessment, and Plan. Each section plays a vital role in individual care and communication among healthcare providers.
- Subjective (S): This section captures the individual's personal experiences, feelings, and concerns regarding their health. It contains direct quotes from the individual, providing valuable insights into their perspective. For instance, an individual might express anxiety about their condition, stating, "I feel anxious daily and have trouble sleeping, especially after work hours."
- Objective (O): In this part, healthcare providers document observable and measurable data, such as vital signs, physical examination findings, and laboratory results. For example, an individual experiencing chest discomfort might have recorded vital signs of BP 140/90 and HR 96. This objective data is crucial for forming an accurate clinical picture.
- Assessment (A): This section involves the clinician's interpretation of the subjective and objective data, leading to a diagnosis or clinical impression. It reflects the provider's clinical reasoning and decision-making process, which is essential for effective management of individuals.
- Plan (P): The final section outlines the proposed treatment strategy, including interventions, follow-up appointments, and education for the individual. It serves as a roadmap for future care, ensuring that all team members are aligned on the patient's treatment strategy.
Understanding this framework is vital for in the soap note presentation among healthcare providers. Have you ever felt overwhelmed by the administrative tasks that can distract from patient care? Research has indicated that the regular utilization of soap note presentation leads to more precise diagnoses, quicker treatment, and reduced follow-up mistakes. Additionally, well-organized medical documentation functions as crucial legal records, enhancing adherence and legal safeguarding in healthcare. As Theodore Roosevelt aptly stated, "The individual receiving care is the most crucial member of the care team," emphasizing the necessity for a person-centered approach in record-keeping. By focusing on the structured framework, providers can enhance care records and ultimately improve health results.
Furthermore, the development of medical records over the last fifty years has resulted in greater length and complexity. This highlights the significance of organized records in contemporary healthcare practices. Together, let’s strive for clarity and compassion in our documentation, ensuring that every individual feels valued and understood.
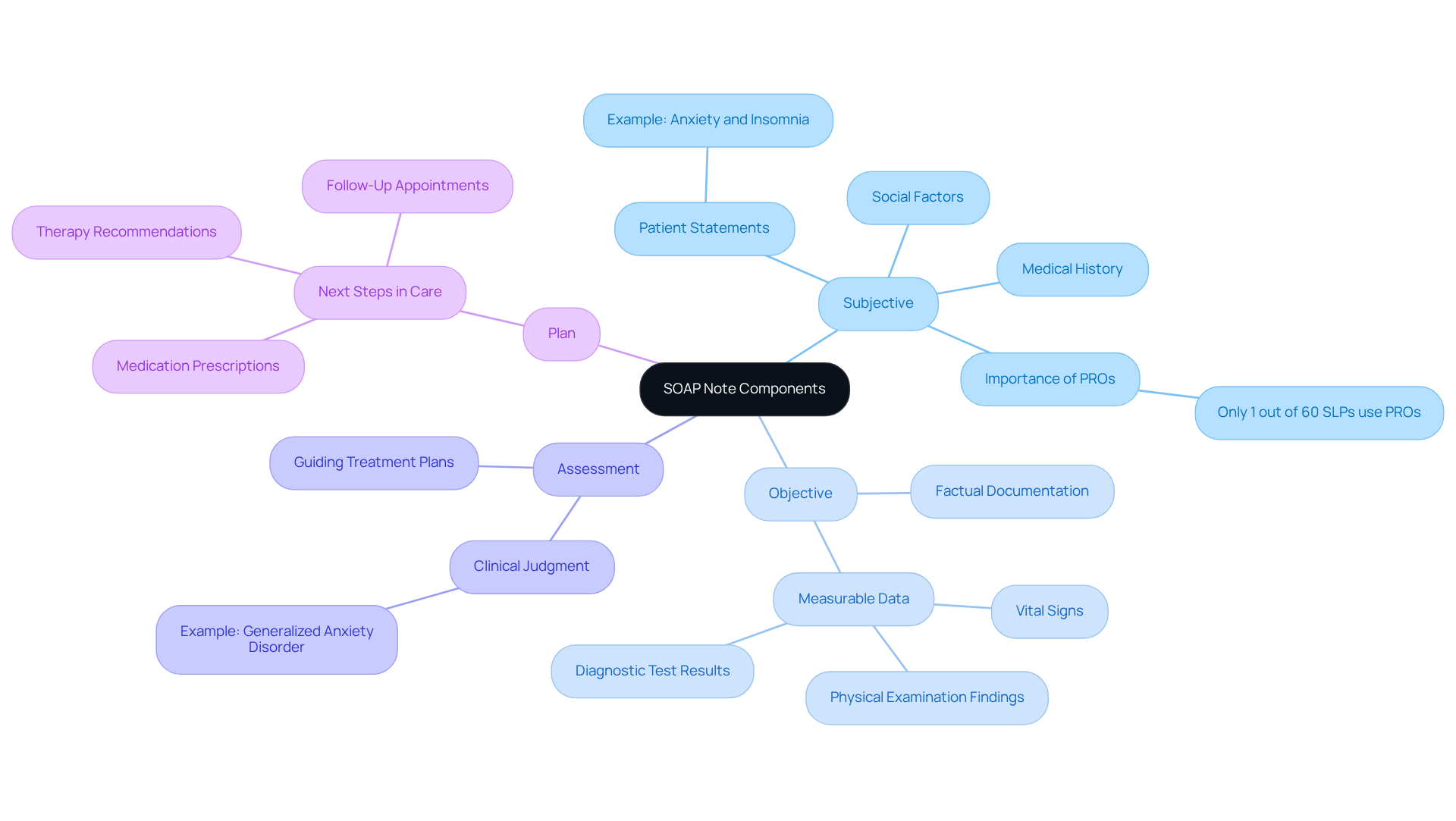
Explore the Components: Subjective, Objective, Assessment, and Plan
Each component of the soap note presentation plays a vital role in patient documentation, and understanding this can significantly ease the burden on healthcare providers.
- Subjective: Gathering information directly from the patient is essential. For instance, if someone shares, "I've been feeling anxious and can't sleep at night," it's crucial to document this statement verbatim. This section should also include the individual's medical history and any relevant social factors. It's concerning that only 1 out of more than 60 speech-language pathologists reported regularly utilizing a Patient-Reported Outcome (PRO). This highlights the importance of capturing individual perspectives in documentation, as it can lead to more personalized care.
- Objective: Documenting measurable data such as vital signs (e.g., blood pressure, heart rate), physical examination findings (e.g., "individual appears well-nourished, in no distress"), and results from diagnostic tests (e.g., lab results) is paramount. This data should be factual and free from interpretation, as accurate objective measurements are crucial for clinical assessments and decision-making.
- Assessment: Analyzing the information collected in the subjective and objective sections is where clinical judgment comes into play. If the individual presents with anxiety and insomnia, the assessment might read, "Generalized Anxiety Disorder, moderate severity." This section is critical for and ensuring that care is tailored to the individual's needs.
- Plan: Outlining the next steps in the individual's care is essential. This could include prescribing medication, recommending therapy, or scheduling follow-up appointments. For example, 'Initiate the individual on SSRIs, refer to counseling, and follow up in four weeks.'
By thoroughly examining each element, providers can ensure that their documentation, particularly in the soap note presentation, is comprehensive and effective. Furthermore, leveraging CosmaNeura's AI-driven transcription and summarization services can aid in precise documentation, aligning with the mission to improve care through technology. This approach not only enhances the quality of care but also alleviates some of the administrative burdens that can impact patient-provider relationships.
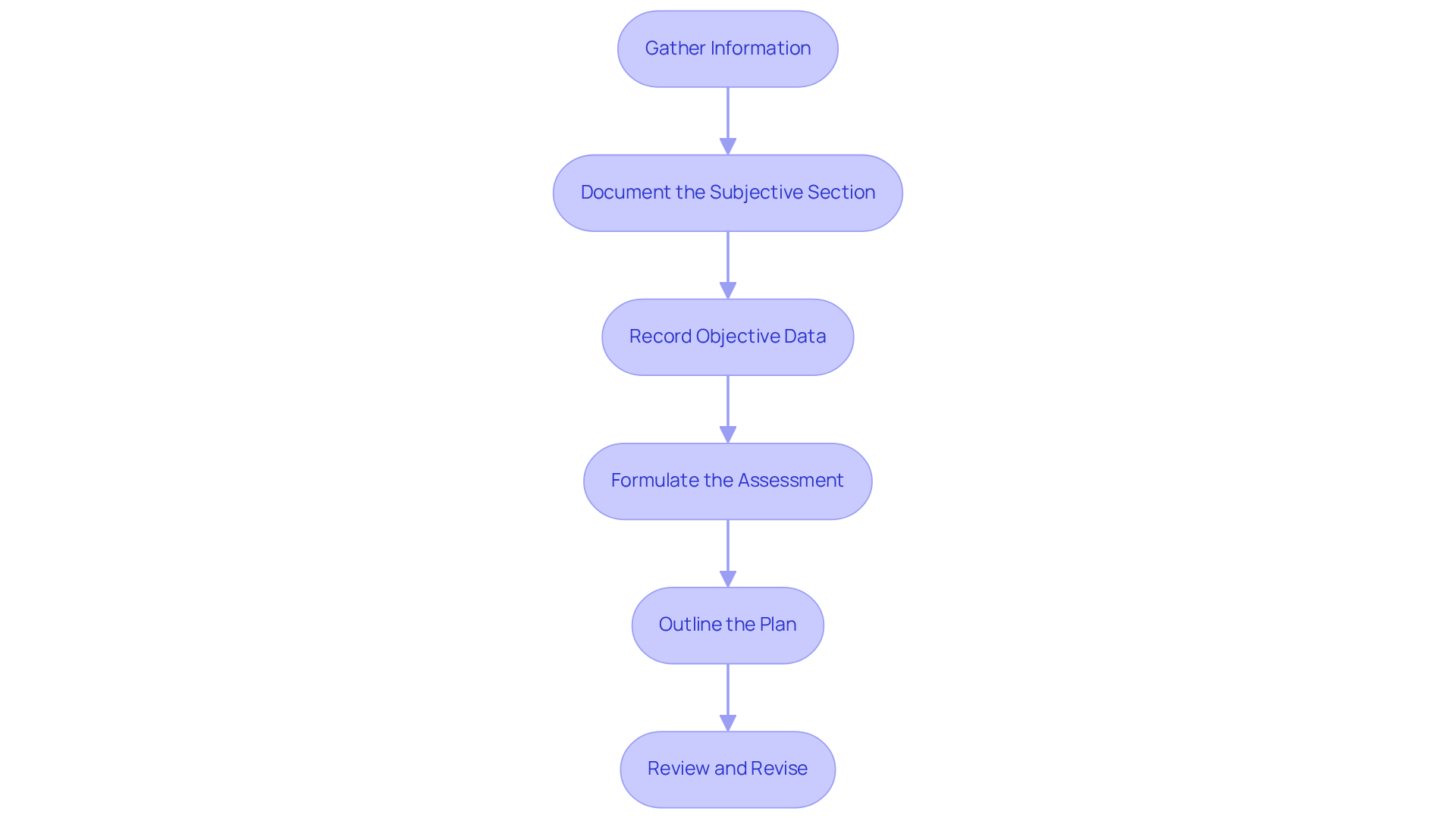
Craft Your SOAP Note: Step-by-Step Instructions
Creating an effective SOAP note can feel overwhelming, especially amidst the many responsibilities healthcare providers face. However, by following these essential steps, you can simplify the process and improve patient care.
- Gather Information: Begin by collecting all relevant details from the individual during the consultation. Use to encourage them to express their concerns fully. This approach not only fosters a trusting environment but also ensures comprehensive data collection.
- Document the Subjective Section: Accurately record the individual's statements verbatim. Include their chief complaint, relevant history, and any other pertinent details. For instance, you might note, "Patient reports a headache for the past three days, rated 7/10 in severity." This segment reflects the individual's viewpoint, which is essential for effective treatment planning.
- Record Objective Data: Measure and document observable data, such as vital signs, physical exam findings, and lab results. For example, you could write, "Blood pressure: 120/80 mmHg; temperature: 98.6°F." This objective information provides a factual basis for your assessment and treatment decisions.
- Formulate the Assessment: Analyze the subjective and objective data to arrive at a clinical impression. Clearly state your diagnosis or differential diagnoses. For example, you might conclude, "Assessment: Tension-type headache." This step is vital for guiding the treatment plan and ensuring continuity of care.
- Outline the Plan: Specify the treatment plan, including medications, referrals, and follow-up instructions. For instance, you could state, "Plan: Advise over-the-counter analgesics, recommend stress management techniques, and schedule a follow-up in one week." A well-defined plan enhances patient understanding and compliance.
- Review and Revise: After drafting the SOAP document, take a moment to review it for clarity and completeness. Ensure that all pertinent information is included and that the message is concise yet comprehensive. Research indicates that adopting specific strategies can help decrease record-keeping time while maintaining high-quality standards.
By following these steps, you can create effective SOAP notes that not only simplify record-keeping but also significantly improve care and communication. On average, over 78% of healthcare providers commit more than 10 hours weekly to record-keeping; thus, mastering this process can lead to significant time savings and enhanced job satisfaction. As Dr. Lawrence Weed noted, "Weed’s system sought to make records easier to read, more comprehensive, and ultimately more useful in patient care." Furthermore, AI-based transcription tools can enhance record-keeping, making it quicker and more precise. Employing organized templates can also improve the quality of records by 36.6%.
Utilize Best Practices and Resources for Effective SOAP Notes
To enhance your SOAP note documentation, consider these best practices that can truly make a difference:
- Be Concise and Specific: Clarity is paramount in your notes. How often do we find ourselves lost in jargon? Aim to avoid unnecessary complexity and ensure that each statement is direct and relevant to the patient's care. This approach not only improves readability but also minimizes the risk of misinterpretation, allowing you to focus on what truly matters. Implement standardized templates for SOAP note presentation to simplify the recording process. These templates ensure that all necessary components are included, saving you valuable time and reducing the likelihood of errors. Many healthcare practitioners have reported considerable enhancements in record-keeping efficiency by utilizing such templates. For instance, over 225,000 healthcare professionals across the country use SimplePractice, which provides complimentary 30-day trials to help you get started with efficient record-keeping.
- Review Regularly: Periodically evaluate your documentation for accuracy and completeness. This practice not only aids in recognizing areas for enhancement but also ensures compliance with record-keeping standards, ultimately improving patient safety and care quality. Reflect on your notes—what can be improved? Seek feedback by collaborating with colleagues to review each other's SOAP note presentations. Constructive feedback can provide valuable insights into enhancing record-keeping practices, fostering a culture of continuous improvement within your practice. As industry leaders have noted, peer review is crucial for enhancing writing skills and supporting each other in this journey.
- Stay Informed: Keep abreast of the latest guidelines and best practices for SOAP note recording. Engaging with resources such as professional organizations, workshops, and online courses can provide you with valuable information that enhances your writing skills. Interacting with these resources can lead to improved outcomes for individuals, as demonstrated by case studies highlighting the effectiveness of structured documentation.
By implementing these best practices and utilizing available resources, you can significantly enhance the quality of your SOAP notes, leading to improved patient care outcomes. Remember, every step you take contributes to a more compassionate and effective healthcare environment.

Conclusion
Mastering the SOAP note presentation is vital for healthcare providers who wish to deliver effective and compassionate care. By fully grasping the framework—Subjective, Objective, Assessment, and Plan—providers can significantly enhance their documentation practices. This ensures that every patient’s voice is not only heard but also accurately represented in their medical records.
Each component of the SOAP note plays a crucial role. The subjective section captures the patient's perspective, while the objective section provides measurable data essential for diagnosis. The assessment synthesizes these elements into a clinical impression, and the plan outlines the next steps for treatment. Best practices, such as maintaining conciseness, regularly reviewing notes, and staying informed about guidelines, can greatly elevate the quality of documentation.
Refining SOAP note practices not only raises the standard of patient care but also nurtures a more efficient healthcare environment. Embracing structured documentation leads to better health outcomes, reduced administrative burdens, and a more person-centered approach to healthcare. As providers implement these strategies, they contribute to a system where every individual feels valued and understood, reinforcing the critical role of effective communication in medical practice.




