Overview
This article offers a caring, step-by-step guide to mastering the SOAP narrative format in EMS, highlighting its crucial role in effective healthcare documentation.
Have you ever felt overwhelmed by the demands of documentation? This guide details each section—Subjective, Objective, Assessment, and Plan—showing how structured documentation not only alleviates administrative burdens but also enhances the quality of patient care.
By reducing errors, it fosters better communication and continuity of care, ultimately leading to improved outcomes for patients.
Embrace this opportunity to enhance your practice and support your patients more effectively.
Introduction
Mastering the SOAP note format is vital for emergency medical service (EMS) professionals. This format is not just a tool; it’s a cornerstone for effective documentation and patient care. By embracing the structured approach of Subjective, Objective, Assessment, and Plan, you can enhance the clarity and quality of medical records, which ultimately impacts patient outcomes positively. Yet, with the increasing complexity of patient interactions and the rise of technology, how can you ensure that all critical information is captured accurately and efficiently?
This guide delves into the intricacies of SOAP note writing. It offers step-by-step insights designed to elevate your documentation practices. Imagine the difference it could make in the quality of care you deliver. Let’s explore how these practices can alleviate some of the administrative burdens you face, allowing you to focus more on what truly matters—your patients.
Understand the SOAP Note Format
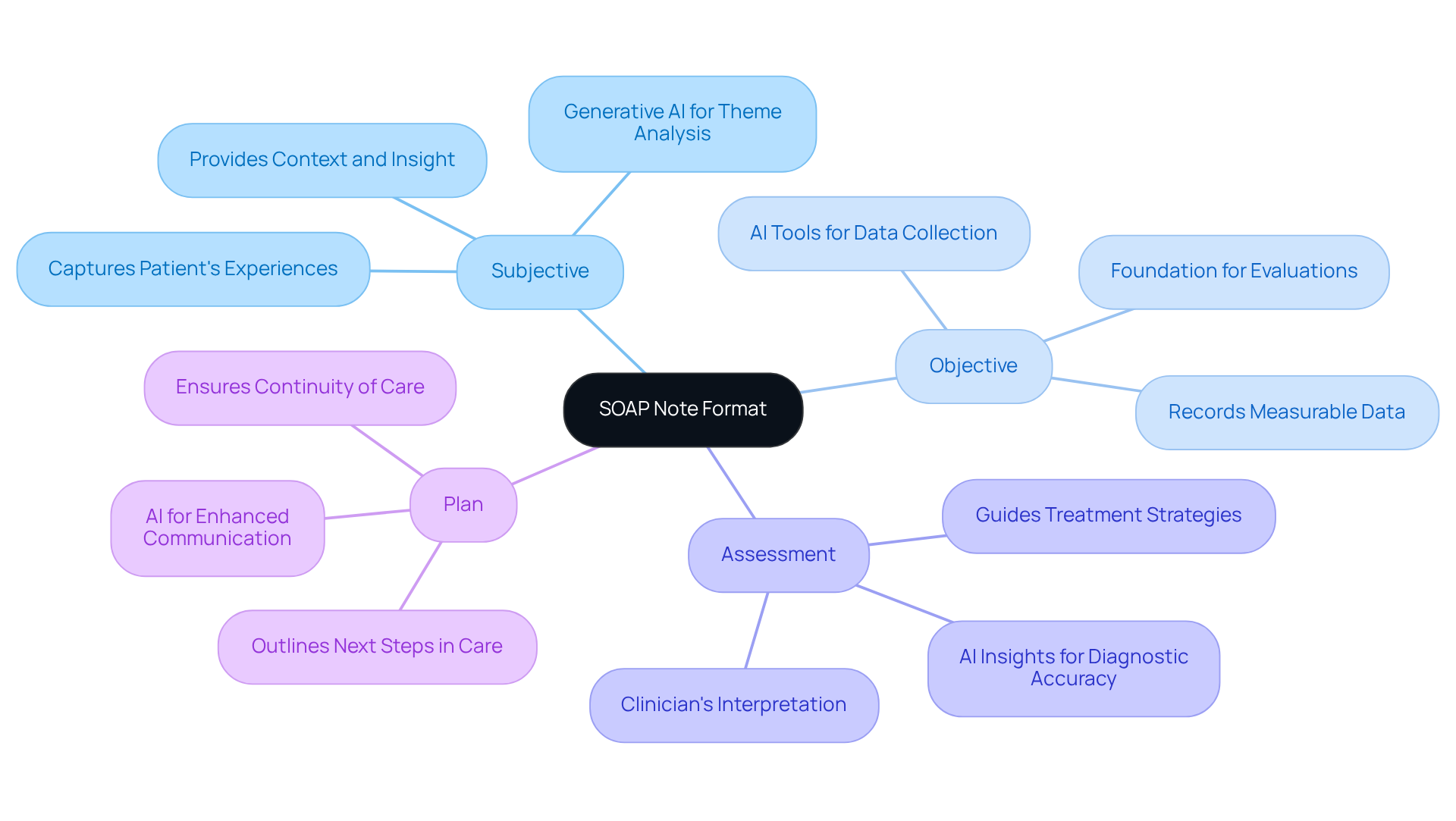
The format known as soap narrative ems, which stands for Subjective, Objective, Assessment, and Plan, is crucial for effective healthcare documentation. Each section plays a vital role in enhancing patient care and understanding.
-
Subjective (S): Here, we capture the patient's personal experiences, symptoms, and feelings about their condition. Recording the individual's own words is essential, as it provides context and insight into their care, enriching the clinician's understanding of their perspective. Have you considered how generative AI can analyze user input to identify key themes, ensuring that no critical information is overlooked?
-
Objective (O): This section records measurable data such as vital signs, physical examination findings, and diagnostic test results. This information lays a factual foundation for understanding the individual's condition, enabling precise evaluations and informed clinical decisions. Imagine the relief AI tools can bring by automating data collection and analysis, reducing the administrative burden on healthcare providers.
-
Assessment (A): In this part, the clinician interprets the subjective and objective data, including the diagnosis or clinical impression derived from the gathered information. This interpretation is vital for guiding treatment strategies. How might AI algorithms support clinicians by providing insights based on historical data and trends, enhancing diagnostic accuracy and efficiency?
-
Plan (P): Finally, the plan outlines the next steps in the individual's care, including treatments, referrals, and follow-up appointments. This section is crucial for ensuring continuity of care and aligning treatment objectives with the individual's needs. By incorporating AI into this process, healthcare providers can enhance communication and coordination, ultimately improving outcomes for those receiving care.
Mastering the soap narrative ems structured format is essential for healthcare professionals, as it provides an organized framework for documenting encounters with individuals. Studies have shown significant improvements in documentation quality following training in SOAP note writing, with total scores rising from 21.9 to 61.8 after intervention (P<0.001). This structured method not only improves the quality of care but also promotes better outcomes by ensuring that all relevant information is captured and utilized effectively. As Don Berwick stated, "Truly listening to individuals and incorporating their feedback is fundamental to enhancing the experience of those receiving care." Moreover, educating healthcare practitioners in uniform medical recording methods is vital, as 70% of medical records contain at least one mistake made by doctors. This underscores the importance of using SOAP narrative EMS format in reducing recording difficulties and enhancing patient care.
Identify Key Components of SOAP Notes
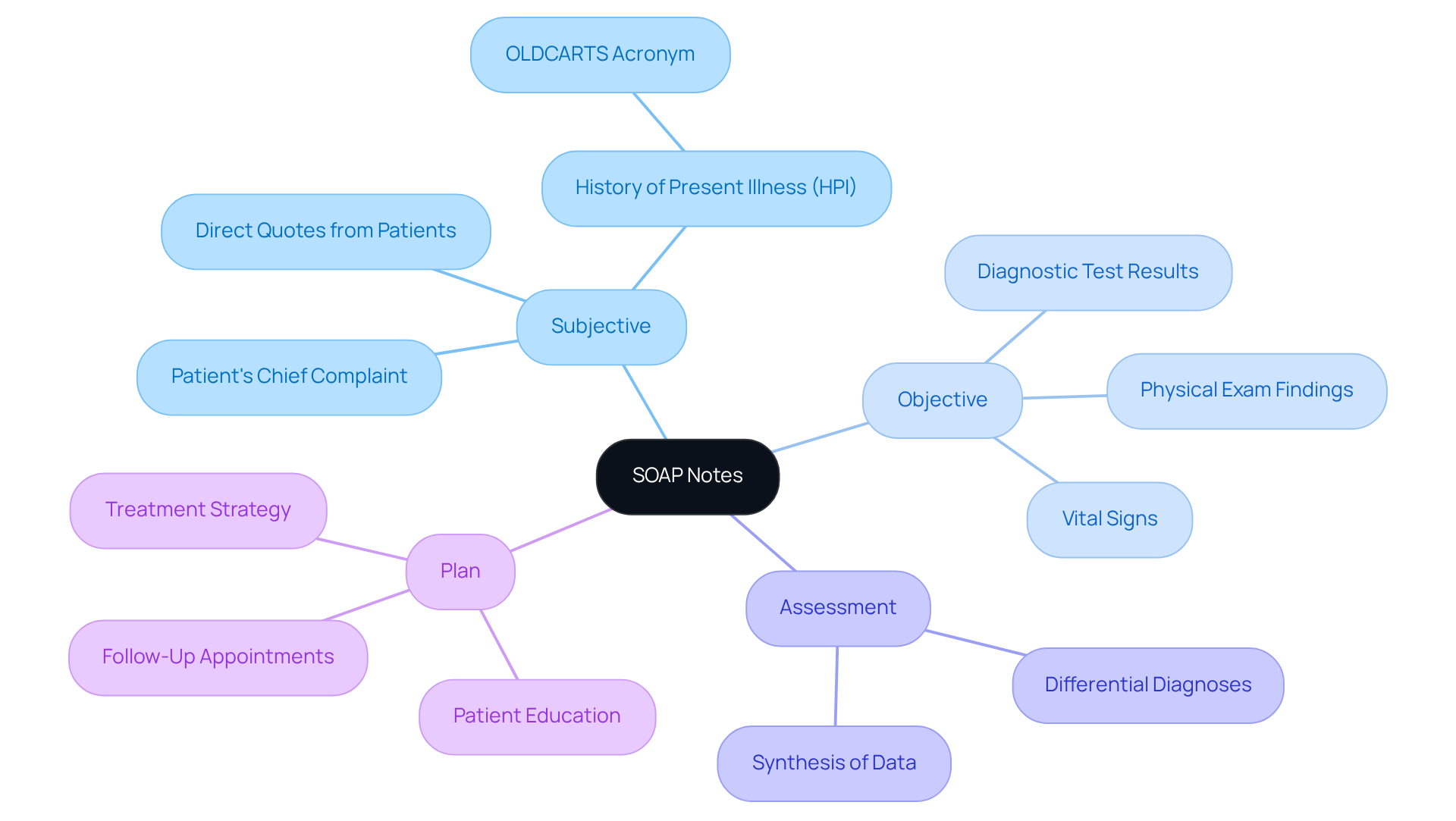
Each component of the SOAP note is essential for effective patient documentation:
-
Subjective: This section captures the patient's chief complaint, history of present illness, and relevant medical history. Direct quotes from individuals can significantly enhance the accuracy of documentation, reflecting their personal experiences and concerns. For instance, when a patient shares, 'I couldn't walk more than a block without pain, but now I can manage three blocks before discomfort begins,' it provides invaluable insights for tailoring care.
-
Objective: Documenting observable data is crucial. This includes vital signs like blood pressure and heart rate, physical exam findings such as tenderness or swelling, and results from diagnostic tests, including lab results and imaging. Accurate objective data supports clinical assessments and informs treatment decisions.
-
Assessment: This section synthesizes the subjective and objective data to provide a clear diagnosis or clinical impression. Including differential diagnoses is essential for guiding further evaluation and treatment.
-
Plan: The treatment strategy should be detailed, outlining medications, referrals, follow-up appointments, and education for the individual. Specificity in this section ensures clarity in patient care and helps in tracking progress over time.
By concentrating on these essential elements, EMS providers can develop thorough SOAP narrative EMS notes that enhance record-keeping and improve communication and continuity of care. The incorporation of AI automation can further simplify the record-keeping process, alleviating the administrative load on healthcare providers. For instance, AI can assist in automating data entry, decreasing record-keeping time and enhancing precision. This enables providers to devote more time to client interactions and care, ultimately transforming outcomes for those receiving treatment.
However, frequent errors in clinical record keeping, such as unclear entries or insufficient detail, can lead to misunderstandings and impact health outcomes. AI can aid in recognizing these errors, ensuring that both subjective and objective information are accurately recorded for effective evaluations. Moreover, recording clinical observations right after interactions with individuals, as highlighted by Blake Bauer, strengthens optimal methods in record-keeping.
Lastly, while upholding client confidentiality and adherence to regulations like HIPAA is vital, it is important to incorporate these practices smoothly into the documentation process to improve overall efficiency.
Write Each Section of the SOAP Note
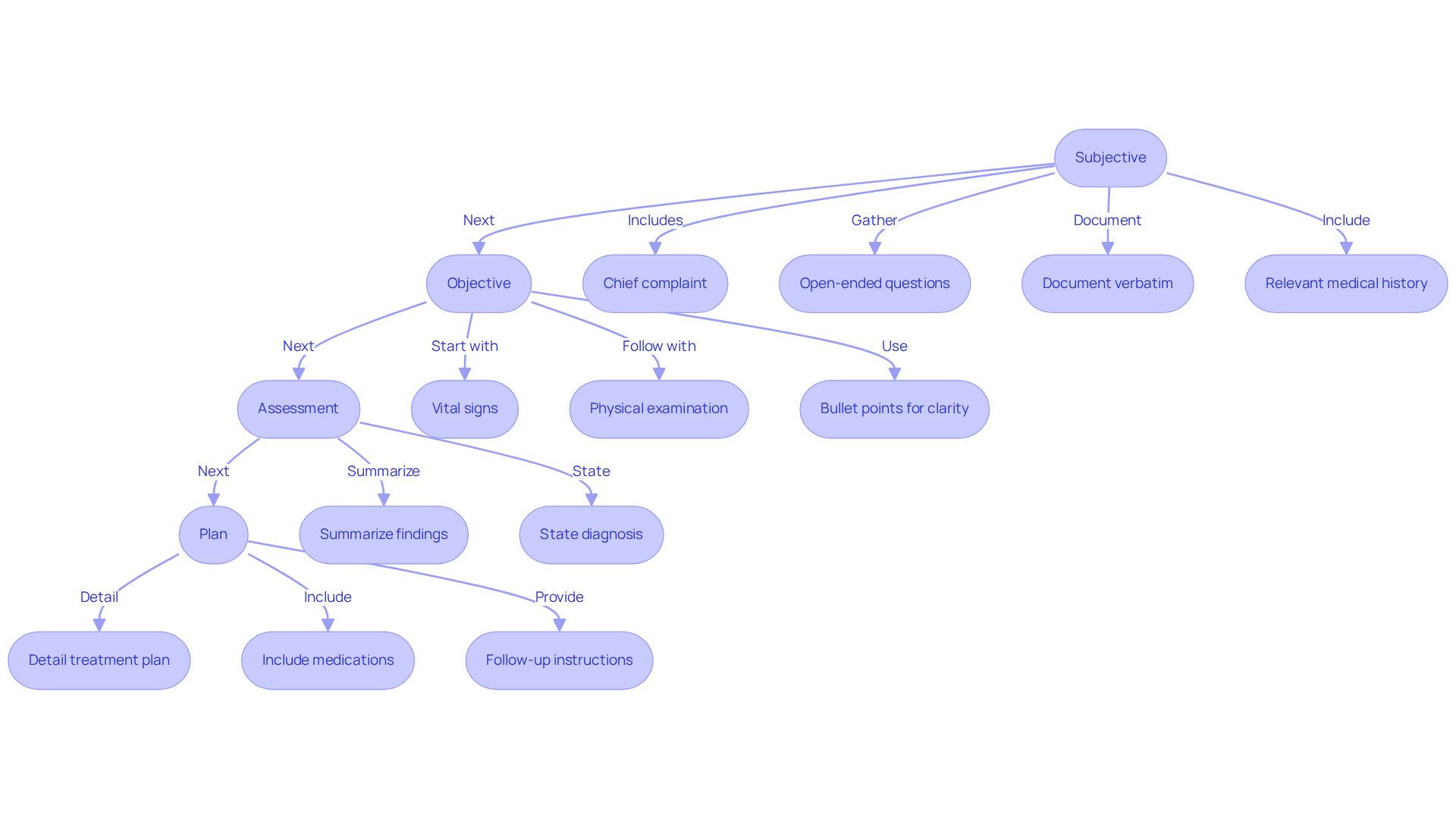
To effectively write each section of the SOAP note, it’s important to approach this task with care and empathy. Start with the patient’s chief complaint in the Subjective section. Use open-ended questions to gather detailed information. For instance, ask, "Can you describe your symptoms?" Documenting the individual’s responses verbatim, when possible, enhances diagnostic value. Additionally, include relevant medical history that may impact their current condition. Recording client statements as quotes is essential for precision and clarity, ensuring their voice is heard.
In the Objective section, begin with vital signs, followed by a systematic physical examination. Using bullet points can enhance clarity and organization. For example:
- Blood Pressure: 120/80 mmHg
- Heart Rate: 72 bpm
- Respiratory Rate: 16 breaths/min
- Findings: No distress, normal lung sounds.
Moving on to the Assessment, summarize the findings from both the subjective and objective sections. Clearly state the diagnosis or clinical impression, such as, "Assessment: Acute bronchitis." This provides a clear understanding of the patient’s condition.
Lastly, in the Plan section, detail the treatment plan, including medications, referrals, and follow-up instructions. Be specific about dosages and timelines. For example, "Plan: Prescribe albuterol inhaler, 90 mcg, 2 puffs every 4-6 hours as needed. Follow up in one week." This clarity is crucial for effective patient care.
By following these steps, EMS providers can create clear and effective SOAP narrative EMS notes that facilitate communication and enhance care for individuals. It’s also important to recognize the challenges faced by healthcare providers in managing administrative burdens that can impact patient care. Continued training and encouragement are vital for enhancing record-keeping practices, and employing electronic systems can greatly improve efficiency in this area. Inadequate records can lead to legal risks and negative outcomes for individuals, underscoring the significance of precision and comprehensiveness in medical files. Incorporating specific instances of effective treatment strategies recorded in progress reports can further demonstrate best practices, fostering a culture of care and understanding.
Ensure Compliance and Best Practices in Documentation
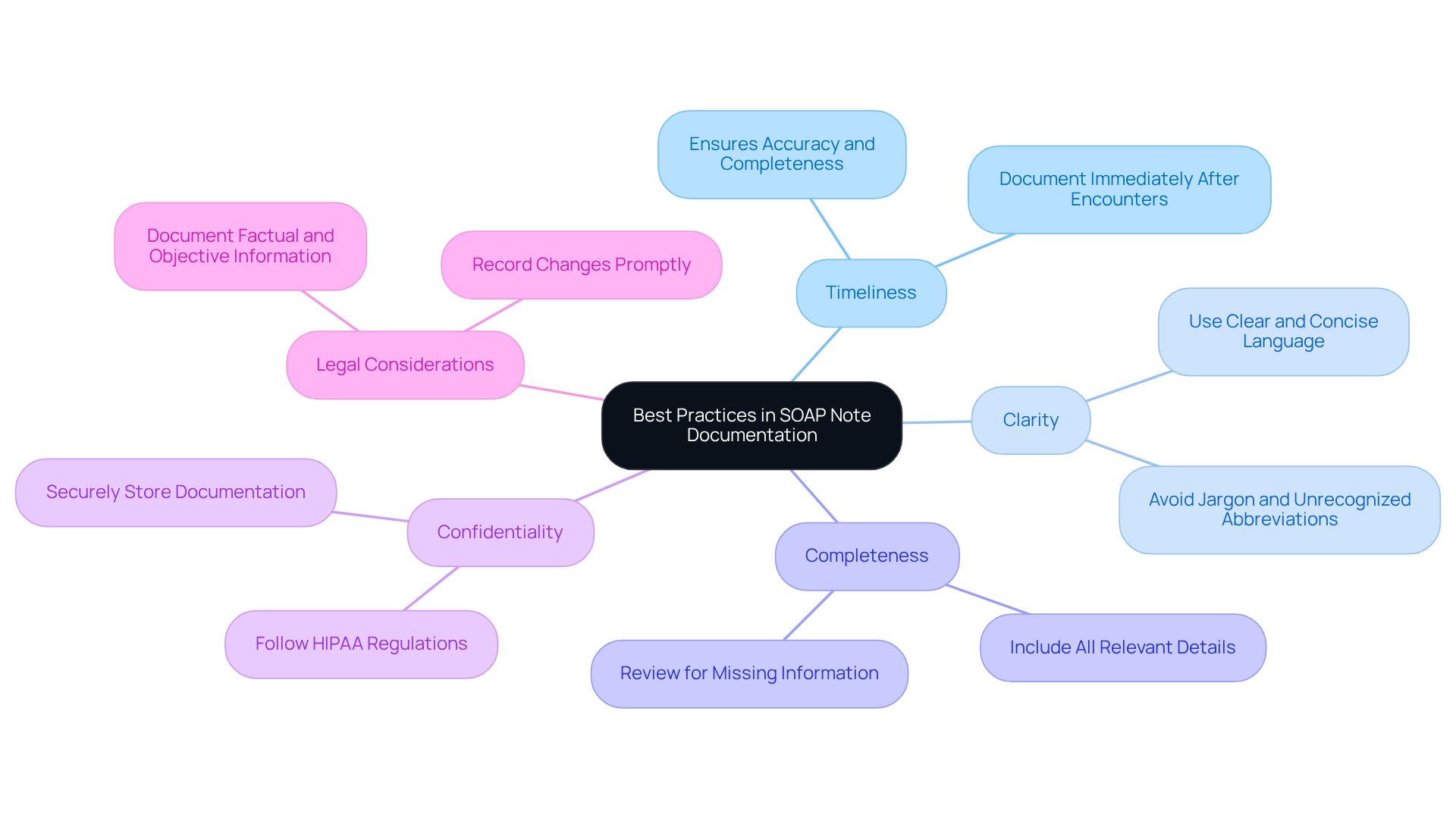
To ensure compliance and uphold best practices in SOAP note documentation, it’s essential to embrace the following guidelines with care and understanding:
- Timeliness: We understand that your time is valuable. Documenting patient encounters immediately after each interaction not only guarantees accuracy but also ensures completeness. Prompt documentation is crucial for maintaining a reliable medical record, allowing you to focus on what truly matters—your patients.
- Clarity: Clear and concise language is vital. By avoiding jargon and ensuring that all abbreviations are widely recognized within the EMS community, we can facilitate understanding among all healthcare providers, fostering a collaborative environment.
- Completeness: Each section of the SOAP document should include all relevant details. Before finalizing, take a moment to examine the document for any missing information, ensuring a comprehensive and supportive record that reflects the care you provide.
- Confidentiality: Upholding patient confidentiality is paramount. By strictly following HIPAA regulations and securely storing documentation, you ensure that access remains restricted to authorized individuals only, safeguarding your patients’ trust.
- Legal Considerations: Remember, SOAP notes are legal documents that must be factual, objective, and free of personal opinions. As Keith Carlson wisely states, "Recording clearly and honestly meets legal obligations in care records." Documenting any changes in a patient's condition or treatment plan promptly is essential for maintaining an accurate legal record.
The format introduced by Lawrence Weed in the 1950s has evolved into a standard in healthcare records, underscoring the importance of organized entries. Utilizing practice management software like SimplePractice, which provides templates for SOAP notes, can greatly enhance your record-keeping process, allowing you to focus more on patient care.
By embracing these compliance and best practice guidelines, EMS providers can significantly enhance the quality of their documentation. This not only ensures that it serves as a reliable resource for patient care but also provides the legal protection that is so vital in our profession. Together, let’s commit to nurturing our documentation practices for the benefit of our patients and ourselves.
Conclusion
Mastering the SOAP narrative format is not just a skill; it’s a vital tool for EMS professionals that can significantly ease the documentation process and elevate the quality of patient care. Have you ever felt overwhelmed by the demands of documenting patient experiences? By grasping and applying the Subjective, Objective, Assessment, and Plan structure, healthcare providers can ensure that every patient's journey is accurately captured and addressed, paving the way for improved clinical outcomes.
Throughout this article, we delved into the essential components of the SOAP note. The importance of capturing patient perspectives in the Subjective section cannot be overstated. Similarly, documenting measurable data in the Objective section, synthesizing information in the Assessment, and outlining clear treatment strategies in the Plan are crucial steps. Moreover, the potential of AI tools to assist in these processes was highlighted, showcasing how technology can lighten administrative burdens and enhance documentation accuracy.
In conclusion, embracing the SOAP narrative format is more than a compliance measure; it fosters a culture of thoroughness and empathy in patient care. As healthcare providers, striving for excellence in documentation is a journey worth undertaking. By committing to continuous improvement and adhering to best practices, we can significantly enhance the quality of care delivered. Let us prioritize effective communication and meticulous record-keeping, ensuring that every patient receives the attentive and informed care they truly deserve.




