Overview
This article serves as a compassionate guide for writing effective SOAP healthcare notes, underscoring the vital role of a structured format in enhancing patient care and fostering communication among healthcare providers.
Have you ever felt overwhelmed by the demands of documentation? You're not alone. The distinct components of SOAP notes—Subjective, Objective, Assessment, and Plan—are detailed here, along with step-by-step instructions for crafting them.
We also highlight common pitfalls to avoid, emphasizing the importance of precise documentation in improving clinical outcomes and ensuring continuity of care.
By mastering SOAP notes, you can alleviate some of the administrative burdens that impact your ability to provide the best care possible.
Let's work together to enhance our practices and support one another in this journey.
Introduction
Structured documentation is the backbone of effective healthcare communication, yet many professionals face emotional challenges in mastering its nuances. The SOAP note format—comprising Subjective, Objective, Assessment, and Plan—serves as a critical tool for clinicians to capture patient information accurately and comprehensively.
However, despite its significance, common pitfalls in SOAP note writing can lead to misunderstandings and compromised patient care.
How can healthcare providers refine their documentation skills to ensure clarity, enhance collaboration, and ultimately improve patient outcomes?
This guide delves into the intricacies of SOAP notes, offering a supportive, step-by-step approach to mastering this essential practice.
Understand the SOAP Note Format
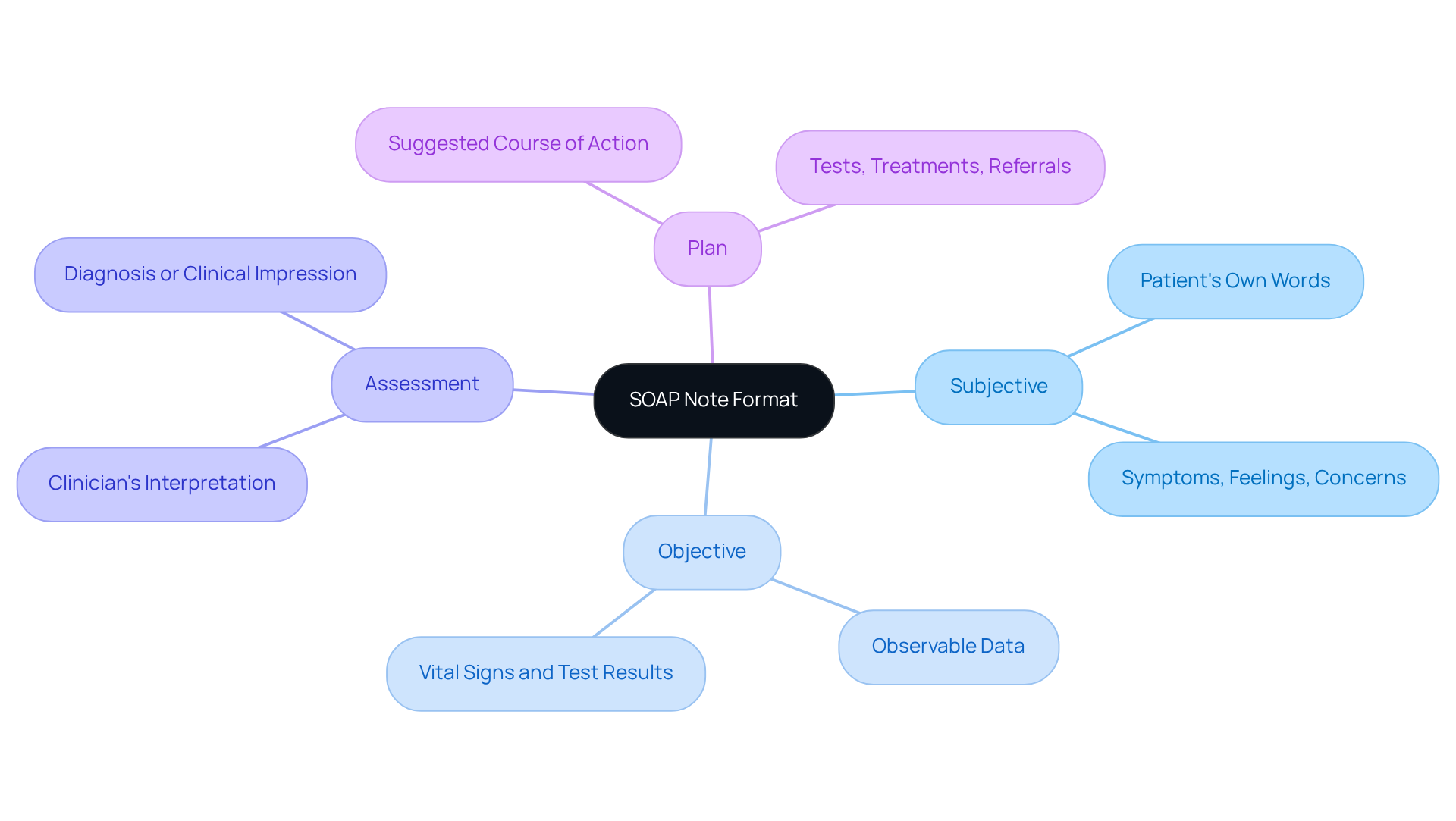
Structured notes play a vital role in nurturing effective communication during client interactions in soap healthcare. The SOAP acronym stands for:
- Subjective: This section captures the patient's own words, reflecting their symptoms, feelings, and concerns.
- Objective: Here, we record observable and measurable data from the examination, including vital signs and test results.
- Assessment: This part conveys the clinician's interpretation of both subjective and objective data, leading to a diagnosis or clinical impression.
- Plan: The suggested course of action is outlined, detailing necessary tests, treatments, or referrals for the individual's care.
The impact of the SOAP note structure on patient records is profound, especially in primary care settings. Have you ever considered how effective record-keeping can enhance continuity of care and mitigate risks associated with malpractice claims? Research indicates that comprehensive records can significantly reduce the likelihood of successful claims, serving as an invaluable resource for clinicians in legal situations.
Standardized records, such as SOAP notes, foster collaboration among healthcare providers, ensuring that every team member has access to clear and concise patient information. This is particularly important, given that health professionals trained in record-keeping are 4.2 times more likely to maintain accurate entries. Additionally, electronic record-keeping systems have been shown to improve recording accuracy by 2.2 times compared to manual methods.
Experts emphasize the importance of soap healthcare notes in enhancing patient care. As healthcare leaders have noted, effective record-keeping practices account for 95% of ensuring appropriate reimbursement, underscoring the financial implications of diligent record management. Looking ahead to 2025, the emphasis on standardized records will only grow, driven by the need for quality assessment and compliance with regulatory standards. Therefore, mastering this structured format is essential for healthcare professionals aiming to refine their documentation skills and ultimately improve client outcomes in soap healthcare.
Explore the Components of SOAP Notes
Each component of a SOAP note serves a distinct and vital purpose in patient care, reflecting the compassionate approach that soap healthcare providers strive to embody.
-
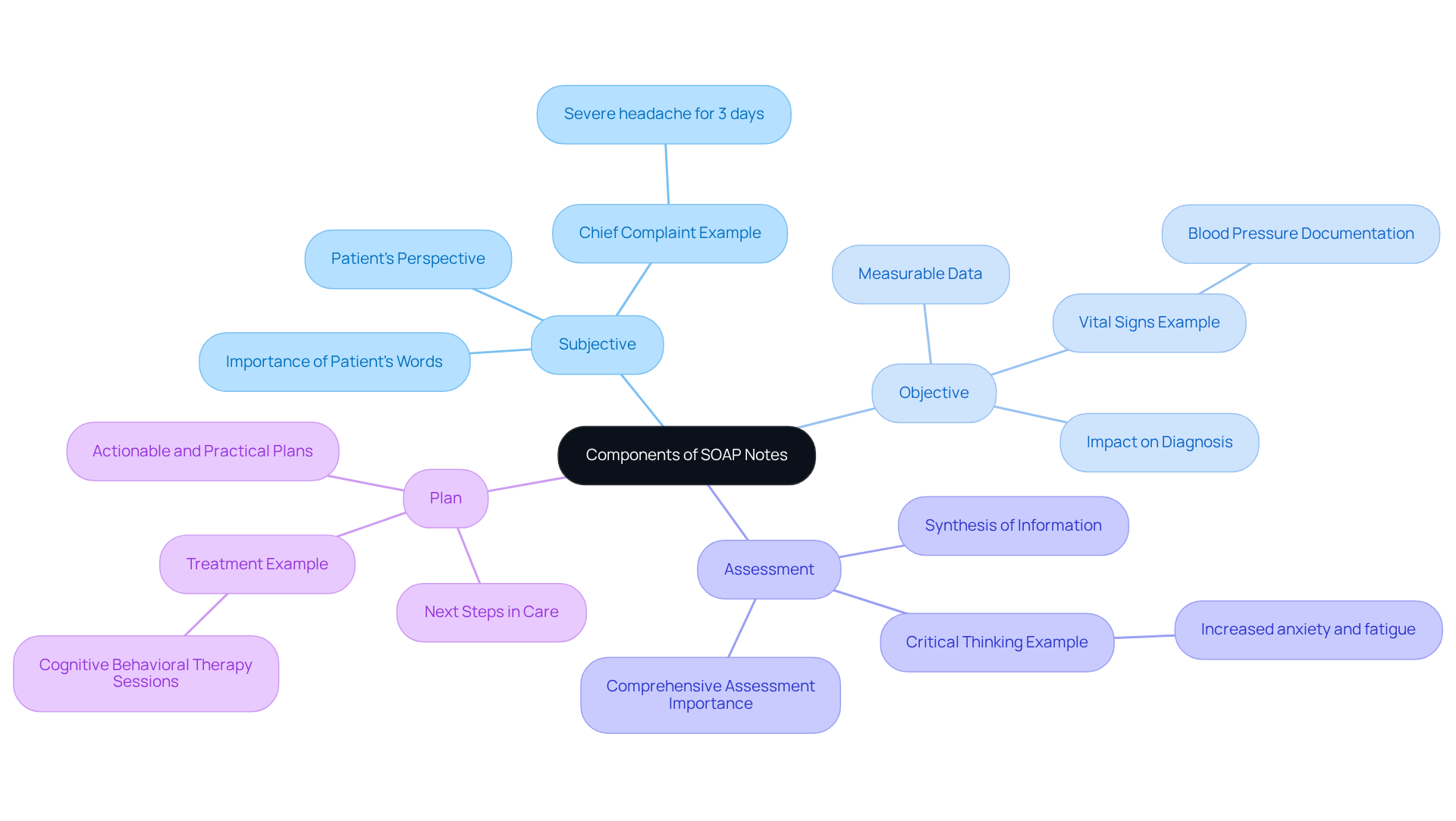
Subjective: This section captures the patient's perspective, including their chief complaint, history of present illness, and any relevant medical history. Recording the individual’s own words is essential for precisely conveying their concerns. For instance, an individual might report, "I have had a severe headache for three days," which directly informs the clinician's understanding of the issue. How often do we find that a patient's words hold the key to their care?
-
Objective: This part includes measurable data such as vital signs, physical examination findings, and results from diagnostic tests. Objective data provides a factual basis for the clinician's assessment. For example, documenting an individual’s blood pressure or lab results can significantly affect the diagnosis and treatment strategy. Research indicates that proper documentation of objective measurements can enhance clinical evaluations and improve outcomes for individuals. Isn’t it reassuring to know that thorough documentation can lead to better care?
-
Assessment: In this section, the clinician synthesizes the subjective and objective information to formulate a diagnosis or clinical impression. This requires critical thinking and clinical reasoning. For example, if an individual presents with increased anxiety and reports fatigue, the clinician must consider both the subjective complaints and objective findings, such as vital signs, to arrive at a comprehensive assessment. This thoughtful integration is what truly makes a difference in patient care.
-
Plan: The plan outlines the next steps in care for individuals, including treatments, referrals, follow-up appointments, and the integration of soap healthcare. It ought to be evident and practical, directing the healthcare team in overseeing the individual’s care. For instance, a plan may suggest cognitive behavioral therapy sessions twice a week for a duration of 180 days, ensuring that the individual receives structured support. How can we ensure that our plans are both actionable and compassionate?
Including both subjective and objective information in clinical documentation not only improves clarity and structure but also promotes better communication in soap healthcare, ultimately resulting in enhanced care for individuals. As Kunal Sindhu, MD, highlights, "Mastering clinical documentation requires effort, but they are a vital resource for recording and sharing patient information." Furthermore, efficient documentation of patient encounters can improve the educational experience for medical trainees, emphasizing its wider significance in healthcare. Let us continue to strive for excellence in our documentation practices, knowing that it leads to better care for all.
Follow Step-by-Step Instructions for Writing SOAP Notes
Writing effective SOAP notes can feel overwhelming at times, but following these steps can make the process smoother and more manageable.
-
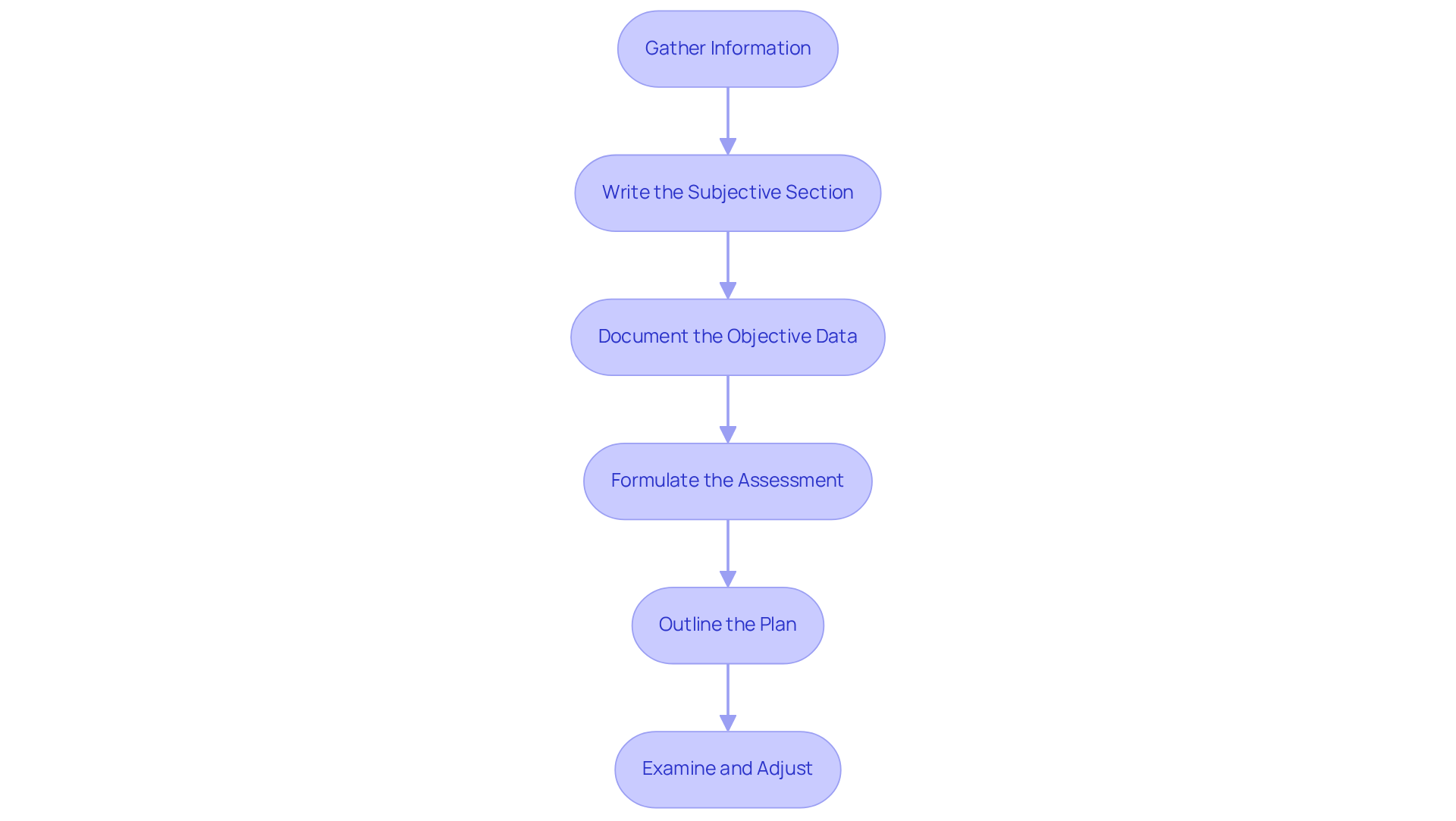
Gather Information: Begin by collecting all relevant individual information, including medical history, current medications, and previous notes. This foundational step is crucial for comprehensive documentation and sets the stage for understanding the individual’s needs.
-
Write the Subjective Section: Document the individual's chief complaint in their own words, along with relevant history and symptoms they report. This section should capture direct quotes to avoid vague language, enhancing the clarity of the individual's perspective. Have you ever found yourself overgeneralizing symptoms in this section? It’s a common mistake that can lead to misinterpretation of the individual's condition.
-
Document the Objective Data: Record measurable data such as vital signs, physical examination findings, and test results. Precision is key; ensure that all observations are factual and devoid of subjective interpretations. Remember, statements without supporting data can compromise the quality of your documentation.
-
Formulate the Assessment: Analyze the subjective and objective data to arrive at a clinical impression or diagnosis. This synthesis should reflect your clinical reasoning, based on both the individual's reported experiences and observable data. Many clinicians summarize instead of analyzing, which can weaken the assessment. How can you ensure your analysis is thorough and insightful?
-
Outline the Plan: Clearly state the next steps in the patient's care, including treatments, referrals, or follow-up appointments. The plan should be actionable and specific, detailing immediate next steps to ensure continuity of care. Focus on immediate actions rather than rewriting the entire treatment plan; clarity here is essential.
-
Examine and Adjust: After composing the documentation, take a moment to assess it for clarity, accuracy, and completeness. Consistently reviewing your materials helps uphold high documentation standards and ensures all pertinent information is recorded efficiently. It’s important to recognize that clinical documentation has constraints, including its inability to record changes over time, which can impact continuous care for individuals.
By incorporating these steps, you can enhance the quality of your documentation, leading to better patient care and improved communication among healthcare professionals. Remember, you’re not alone in this journey; every small improvement contributes to a more compassionate and effective healthcare environment.
Identify Common Mistakes in SOAP Note Writing
Common mistakes in SOAP healthcare note writing can create significant challenges for healthcare providers.
-
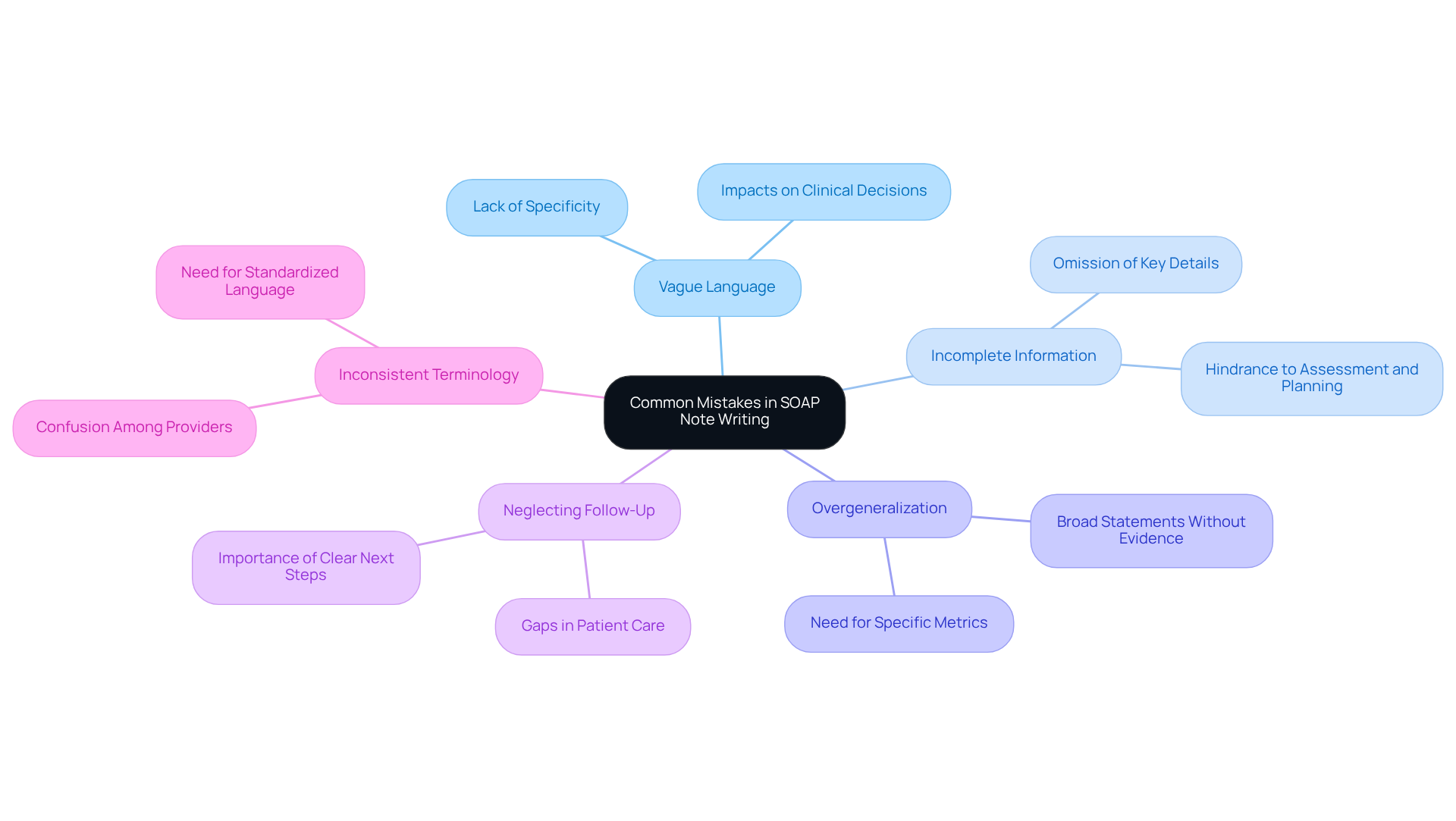
Vague Language: Using general terms instead of specific details can lead to misunderstandings and misinterpretations. For instance, phrases like 'patient feels fine' lack the necessary detail to inform clinical decisions. Aim for clarity and precision in your descriptions to ensure effective communication among healthcare providers. As Jess Barron notes, vague assessments can undermine clinical clarity. Have you considered how this might impact patient care?
-
Incomplete Information: Omitting key details, particularly in the subjective or objective sections, can significantly hinder the assessment and planning process. In SOAP healthcare, comprehensive documentation is essential for maintaining continuity of care and ensuring that all relevant information is captured. The objective section should include specific interventions and client responses to enhance clarity. Think about the implications of missing information on patient outcomes.
-
Overgeneralization: Avoid making broad statements without supporting evidence. Each assessment should be grounded in specific data derived from the subjective and objective sections. Instead of saying 'the individual is improving,' specify the metrics or observations that support this conclusion. A study shows that occupational therapists frequently make SOAP note errors due to poor note-taking abilities, hectic schedules, or lack of training. How can we improve our practices to avoid such pitfalls?
-
Neglecting Follow-Up: Failing to outline a clear plan for follow-up can create gaps in care for individuals. It is crucial to specify the next steps in the patient's management, ensuring that all team members are aligned on the treatment plan. Reflect on how clear follow-up plans can enhance patient outcomes.
-
Inconsistent Terminology: Using different terms for the same condition can lead to confusion and miscommunication. Consistency in language throughout the SOAP healthcare note is vital for clarity and effective collaboration among healthcare professionals. Consistent training and compliance with standardized formats can help alleviate these issues, improving the overall quality of records. Utilizing structured tools like ICANotes or HealthOrbit AI can also prevent omissions and improve documentation accuracy. Have you explored these tools to enhance your documentation process?
Conclusion
Mastering the SOAP note format is crucial for healthcare professionals who strive to enhance their documentation skills and improve patient outcomes. Have you ever felt overwhelmed by the demands of documentation? By understanding and utilizing the structured approach of Subjective, Objective, Assessment, and Plan, clinicians can foster better communication and collaboration within healthcare teams. This systematic method not only aids in accurate record-keeping but also plays a critical role in ensuring continuity of care and minimizing risks associated with malpractice claims.
Throughout this guide, we have explored the key components of SOAP notes in detail. Each section serves a specific purpose, from capturing the patient's perspective to documenting measurable data, synthesizing information for a diagnosis, and outlining actionable plans for care. It’s essential to avoid common pitfalls, such as vague language and incomplete information, as precision and consistency in clinical documentation are vital.
Ultimately, committing to mastering SOAP notes is a commitment to delivering high-quality healthcare. As the emphasis on standardized records continues to grow, healthcare professionals are encouraged to refine their documentation practices. By doing so, you not only enhance your own effectiveness but also contribute to a more compassionate and efficient healthcare environment. Embracing this structured format is not merely about compliance; it is a pathway to better patient care and improved health outcomes for all. Are you ready to take this important step toward excellence in your practice?




