Overview
This article provides a compassionate, step-by-step approach to mastering patient chart notes. It recognizes the emotional challenges healthcare providers face and emphasizes the importance of effective documentation in delivering high-quality patient care and fostering communication among providers. By outlining the key components of effective chart notes, the article offers practical strategies to overcome common documentation challenges. This not only enhances the quality of patient records but also alleviates some of the administrative burdens that can impact patient care.
Have you ever felt overwhelmed by the demands of documentation? You're not alone. Many healthcare providers struggle with the intricacies of patient charting. This article aims to support you by breaking down the essential elements of effective chart notes, providing you with the tools you need to navigate these challenges with confidence.
Consider the benefits of mastering your charting skills: improved patient care, streamlined communication, and reduced stress. By implementing the strategies outlined, you can enhance the overall quality and efficiency of your patient records. Let's take this journey together towards more effective documentation, ensuring that every patient receives the care they deserve.
Key solutions include:
- Understanding the key components of effective chart notes
- Developing practical strategies to streamline documentation
- Enhancing communication among healthcare providers
As you read through, reflect on your experiences and challenges. Together, we can transform the way we approach patient charting, making it a more manageable and rewarding part of your practice.
Introduction
Patient chart notes are essential to effective healthcare, capturing a patient’s medical journey and enabling seamless communication among providers. As healthcare systems grow increasingly complex, mastering chart documentation is vital for ensuring quality care and legal protection. However, healthcare professionals often face emotional challenges, such as navigating inconsistent records and fragmented communication. How can we overcome these obstacles to create comprehensive notes that truly enhance patient outcomes?
The administrative burdens can weigh heavily on providers, impacting their ability to deliver the compassionate care patients deserve. It’s crucial to address these challenges head-on. By focusing on clear, effective documentation, we can improve not only our records but also the overall patient experience. Imagine a system where every note contributes meaningfully to a patient’s care.
Let’s explore practical solutions together. Consider implementing standardized templates to streamline documentation. Encourage open communication among team members to reduce misunderstandings. Regular training sessions can also empower providers to enhance their skills in charting. These strategies not only foster better documentation practices but also strengthen the bond between providers and patients.
Ultimately, the goal is to ensure that every patient receives the highest quality of care. By prioritizing effective chart notes, we can create a supportive environment that values both provider and patient experiences. Together, we can navigate these challenges and improve healthcare outcomes for everyone involved.
Understand the Purpose of Patient Chart Notes
Patient chart notes are vital in medicine, serving as a comprehensive account of an individual's medical history, treatment strategies, and development over time. These patient chart notes are crucial for ensuring continuity of care, enabling various medical providers to understand a person's journey and make informed decisions. Yet, many healthcare providers face emotional challenges due to the fragmentation of healthcare systems, which often leads to disjointed communication and coordination among providers.
Regulatory concerns, such as HIPAA, aim to protect individual privacy but can inadvertently create communication barriers that worsen this fragmentation. Consider this: research indicates that individuals with high continuity of care experience 12.49% fewer hospital admissions for ambulatory care-sensitive conditions compared to those with low continuity. This statistic highlights the tangible advantages of maintaining comprehensive records.
Moreover, well-documented patient chart notes provide legal protection for medical providers, illustrating compliance with care standards and shielding against potential malpractice claims. The importance of thorough patient chart notes cannot be overstated; they not only enhance communication among providers but also foster trust and understanding between individuals and their care teams.
The integration of electronic systems for documentation has proven to enhance the quality and efficiency of medical records, especially in managing patient chart notes, making it easier for professionals to maintain precise and comprehensive client information. Generative AI can also play a role in improving client interactions and alleviating provider burdens, addressing the challenges posed by fragmented medical systems.
By mastering effective chart documentation, healthcare professionals can significantly improve outcomes for individuals and streamline care processes. Together, let’s embrace these solutions and work towards a more connected and compassionate healthcare environment.

Identify Key Components of Effective Chart Notes
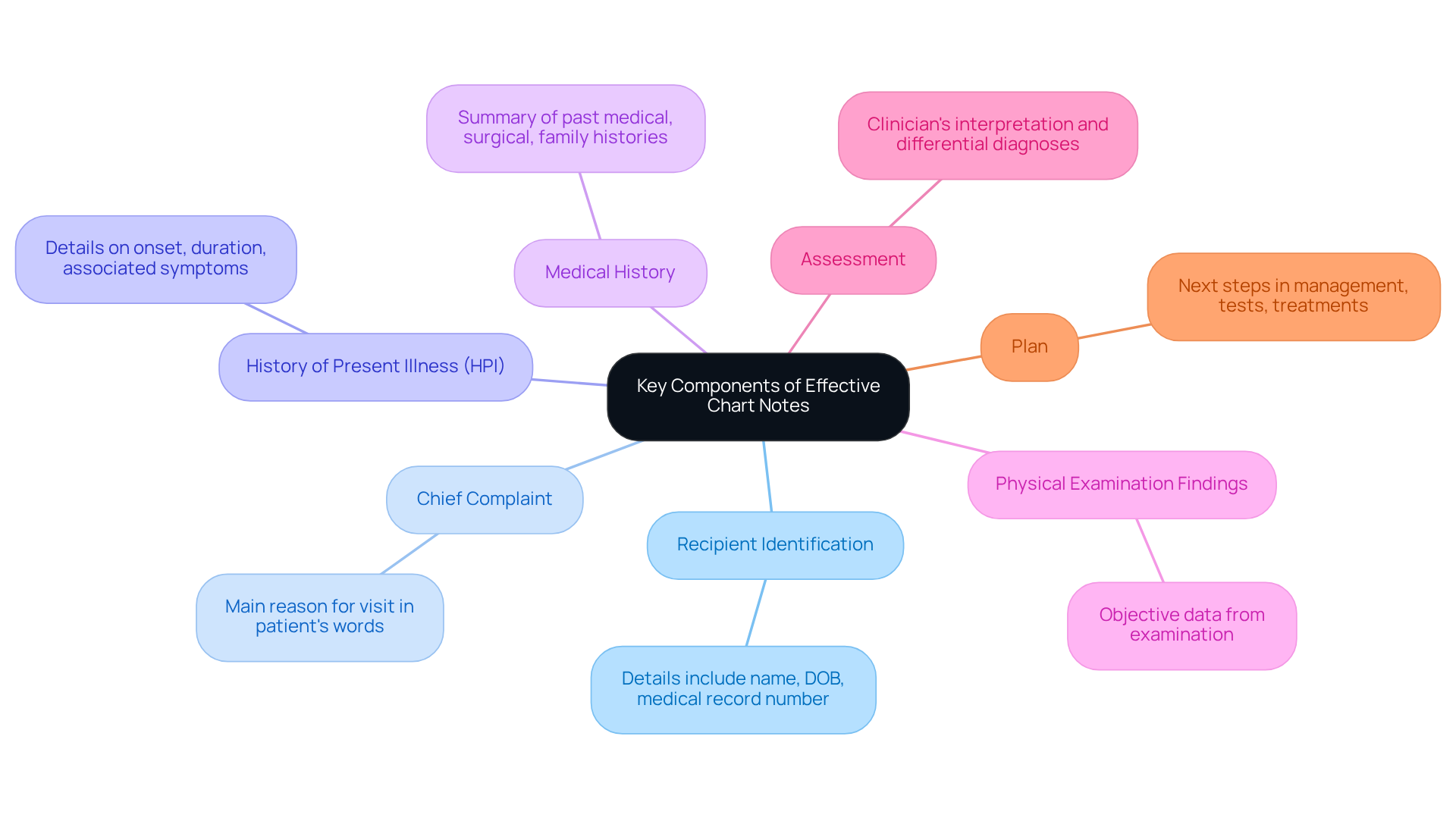
Effective chart notes are essential for quality patient care and should encompass several key components:
- Recipient Identification: Include essential details such as the individual's name, date of birth, and medical record number. This ensures precise tracking and reference, allowing for a more personalized approach to care.
- Chief Complaint: Document the main reason for the individual's visit, articulated in their own words. This captures their perspective and concerns, fostering a deeper understanding of their needs.
- History of Present Illness (HPI): Provide a comprehensive account of the individual's current condition, detailing the onset, duration, and any associated symptoms. This information is vital for informed clinical decision-making.
- Medical History: Summarize pertinent past medical, surgical, and family histories that may influence the individual's current health status and treatment options. Recognizing these factors can significantly impact care.
- Physical Examination Findings: Record objective data gathered during the examination. This serves as a foundation for clinical assessments and future care plans, reinforcing the importance of thorough documentation.
- Assessment: Offer the clinician's interpretation of the findings, including differential diagnoses. This guides further evaluation and management, ensuring a well-rounded approach to care.
- Plan: Clearly outline the next steps in management, specifying tests, treatments, and follow-up appointments. Integrating AI-powered solutions, such as automated scheduling and record-keeping systems, can simplify this process, improving efficiency and precision in records.
Integrating these elements into patient chart notes not only enhances the quality of documentation but also promotes better health outcomes by enabling effective communication among healthcare professionals. Have you considered how thorough chart records can lead to enhanced care for individuals? A case study from CosmaNeura illustrates that meticulous documentation of patient chart notes results in improved care for patients and increased efficiency for providers, highlighting the real-world impact of effective record-keeping. Together, let’s work towards a future where compassionate care is at the forefront of healthcare.
Follow a Step-by-Step Process for Writing Chart Notes
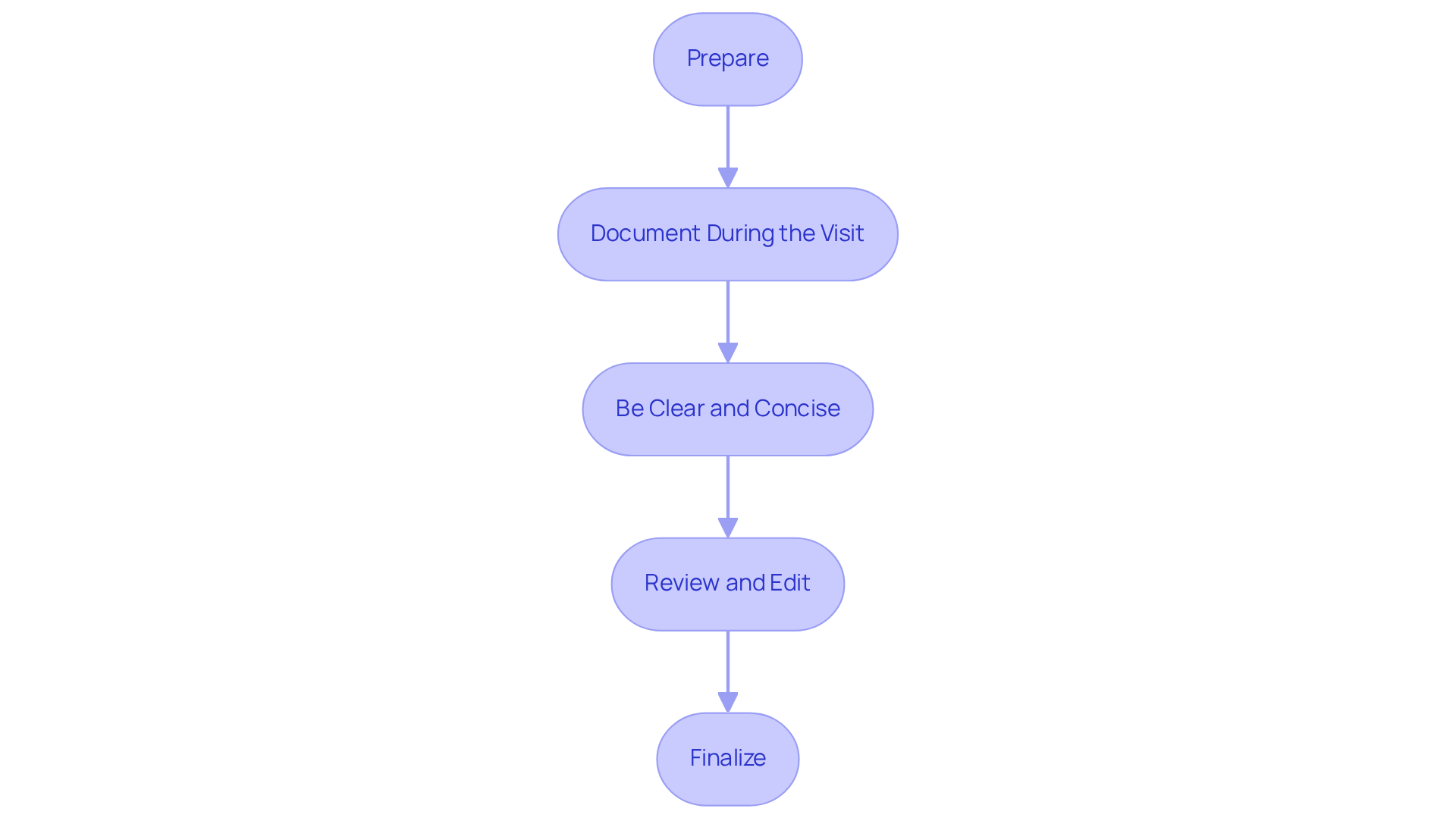
Writing effective patient chart notes can feel overwhelming, especially with the demands of patient care. To ease this burden, consider these structured steps that not only enhance your documentation but also support your role as a caregiver.
-
Prepare: Before your consultation, take a moment to review earlier records and relevant medical backgrounds. This preparation helps you understand the context of the visit, making your interactions more informed and compassionate. AI tools like history summarizers can assist in quickly sifting through important information, boosting your efficiency and confidence.
-
Document During the Visit: Capture real-time information by taking notes throughout your patient interactions. Using a structured format such as SOAP (Subjective, Objective, Assessment, Plan) can enhance the clarity and organization of patient chart notes. AI-driven record-keeping tools can suggest relevant phrases, ensuring that essential information is captured, thus optimizing your documentation process.
-
Be Clear and Concise: It's important to use straightforward language that avoids jargon. This approach ensures your notes are legible and focused on the crucial aspects of the visit. AI can provide templates and examples to help you create clear records efficiently, allowing you to communicate effectively without added complexity.
-
Review and Edit: After your visit, take the time to meticulously review your records for accuracy and completeness. Making necessary edits to clarify observations and plans ensures that all relevant information is captured. Prompt documentation is vital; finalizing your patient chart notes soon after the encounter reduces the risk of omitting key details. AI tools can flag inconsistencies or suggest enhancements based on best practices, making your review process smoother.
-
Finalize: Ensure that all necessary components are included, and that your documentation is dated and signed. This final step is crucial for meeting legal and professional standards, protecting both you and your patients. Specialists note that reducing paperwork time with AI can significantly lessen administrative burdens, leading to improved job satisfaction among healthcare professionals.
By following this structured approach and integrating AI tools, you can enhance the quality of your documentation. This not only improves patient care but also helps you stay compliant with legal requirements. Remember, you are not alone in this journey; embracing these practices can lead to a more fulfilling and effective caregiving experience.
Troubleshoot Common Issues in Chart Note Writing
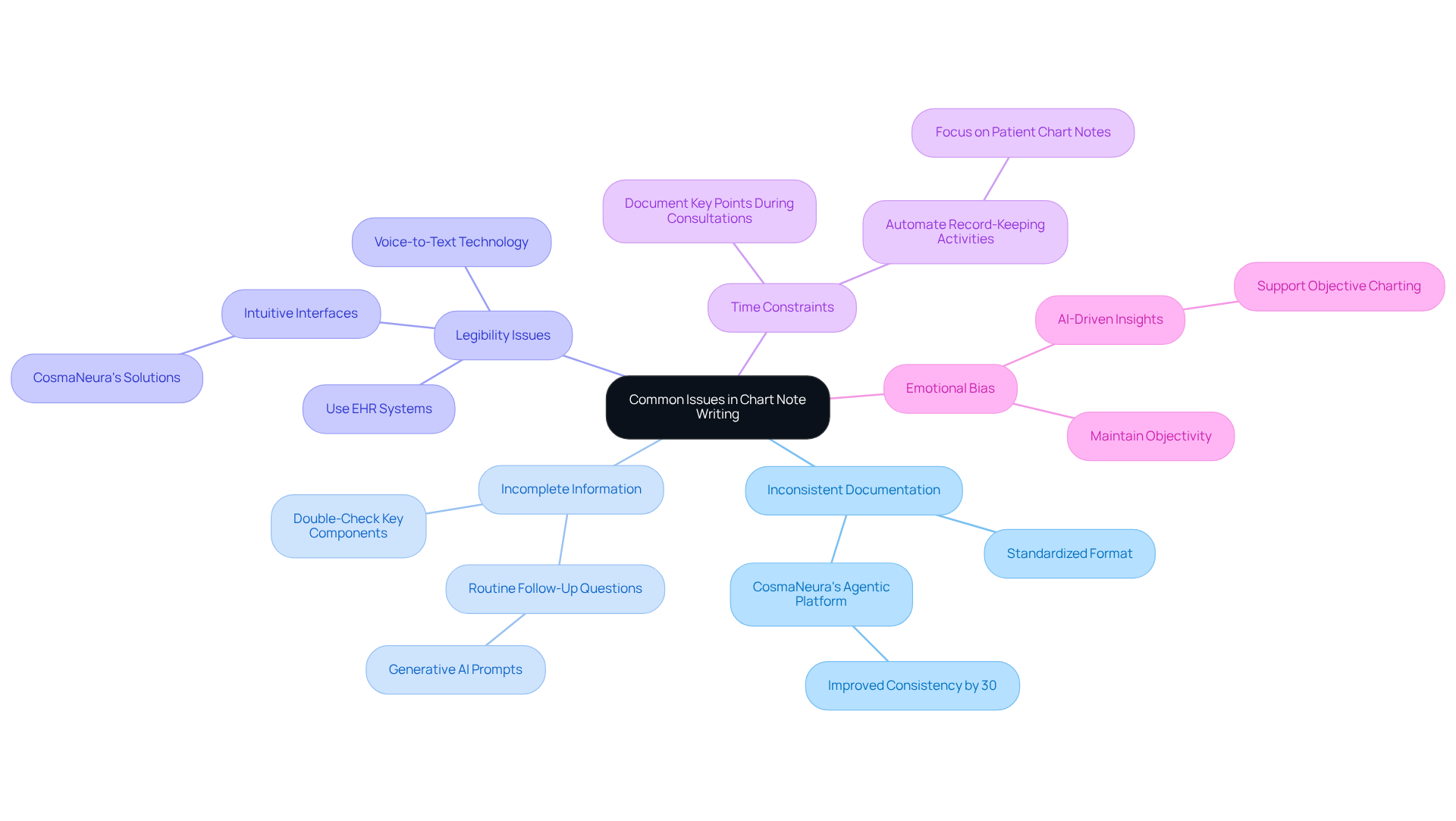
Common issues in writing patient chart notes documentation can feel overwhelming for healthcare providers. Inconsistent Documentation is a common hurdle. It's essential to follow a standardized format for all patient chart notes to maintain consistency. CosmaNeura's Agentic Platform can simplify this process, ensuring uniformity across records. For example, a healthcare provider improved their documentation consistency by 30% after implementing the platform.
Another challenge is Incomplete Information. Always double-check that all key components are included in your notes. If you notice gaps, consider developing a routine of asking follow-up questions during interactions. The platform's generative AI capabilities can prompt necessary questions, helping you gather comprehensive information.
Legibility Issues can also arise. If handwriting is a concern, think about using electronic health record (EHR) systems or voice-to-text technology to enhance clarity. CosmaNeura's solutions support this by offering intuitive interfaces that foster clear records.
Time constraints can be daunting, but there are strategies to manage them effectively. Document key points during consultations and finalize your notes afterward. Prioritize essential information to avoid feeling overwhelmed. The Agentic Platform can automate standard record-keeping activities, enabling medical professionals to focus more on patient chart notes.
Lastly, Emotional Bias is something to be mindful of. Personal biases can affect your documentation, so strive to remain objective and focus on factual information. By leveraging AI-driven insights, CosmaNeura helps maintain objectivity in charting.
It's important to acknowledge that some medical providers may hesitate to adopt these innovative solutions due to concerns about altering established practices. However, by addressing these common issues with supportive solutions, healthcare providers can enhance their chart note writing skills and significantly improve patient care.
Reflect on these challenges and consider how embracing these tools can transform your documentation process, leading to better patient outcomes.
Conclusion
Mastering patient chart notes is more than just an essential skill for healthcare professionals; it is a vital part of providing compassionate care. These notes form the backbone of effective patient interactions, and by understanding their purpose, providers can enhance communication, ensure legal protection, and maintain continuity of care. This article has presented a thoughtful approach to writing effective chart notes, emphasizing clarity, thoroughness, and the integration of modern tools to simplify the process.
Key components of effective chart notes include:
- Precise patient identification
- Detailed accounts of the chief complaint and medical history
- Clear plans for future care
By following a structured, step-by-step process for writing these notes, healthcare professionals can address common challenges such as inconsistent documentation and incomplete information. The integration of AI tools further supports this effort, improving both the quality of care and the efficiency of documentation.
Reflecting on these insights, it becomes clear that investing time in mastering patient chart notes transcends mere administrative duty; it is a crucial aspect of delivering high-quality healthcare. By embracing these practices and tools, healthcare providers can create a more connected and compassionate environment, ultimately leading to better patient outcomes. The journey toward effective documentation begins with a commitment to continuous improvement—an essential step for all dedicated healthcare professionals.
How can you take the first step today to enhance your documentation skills and, in turn, your patient care?




