Overview
The article highlights the emotional challenges that healthcare providers encounter when documenting SOAP notes for lower back pain. It presents a structured four-step process: Subjective, Objective, Assessment, and Plan. Each component is not just a box to check; they are vital for effective patient care. By ensuring thorough documentation, healthcare providers enhance communication and foster a collaborative environment.
Have you ever felt overwhelmed by administrative burdens? These can significantly impact patient care, making it difficult to focus on what truly matters—your patients. This structured approach to SOAP notes not only streamlines your documentation process but also ensures that treatment plans are built on comprehensive and precise information.
Imagine the benefits of improved patient outcomes as a result of clear and effective communication. By mastering the SOAP note documentation, you can alleviate some of the stress associated with patient care. This approach empowers you to provide the best possible support to your patients.
We encourage you to engage with this process and reflect on how it can transform your practice. Embrace the structured four-step process, and watch as it enhances your ability to care for your patients with confidence and compassion.
Introduction
Understanding the intricacies of clinical documentation can be a daunting challenge for healthcare professionals, especially when managing conditions like lower back pain. This task often weighs heavily, as effective communication is crucial in providing the best patient care. The SOAP note framework—comprising Subjective, Objective, Assessment, and Plan—serves as a vital tool in this regard. However, many practitioners encounter common pitfalls that can undermine the quality of their documentation.
How can healthcare providers navigate these complexities to enhance patient outcomes? The administrative burdens can sometimes feel overwhelming, impacting the quality of care delivered. Yet, mastering the SOAP note framework can lead to significant improvements in both documentation and patient interactions.
Imagine the benefits of streamlined practices that not only enhance your efficiency but also foster better relationships with your patients. By focusing on this essential skill, you can make a meaningful difference in your practice. Let’s explore how to overcome these challenges together and improve the quality of care for those who depend on us.
Understand the SOAP Note Framework
The SOAP note framework is not just a tool; it’s essential in clinical documentation, comprising four key components: Subjective, Objective, Assessment, and Plan. Each section plays a vital role in ensuring effective patient care, especially within fragmented healthcare systems where communication and coordination can feel overwhelming.
-
Subjective (S): This section captures the patient's personal experiences, feelings, and concerns regarding their condition. It contains direct quotations from the individual, offering insight into their symptoms and emotional state, which can be crucial for understanding their needs.
-
Objective (O): Here, clinicians document observable and measurable data, such as vital signs, physical examination findings, and results from diagnostic tests. This objective information is crucial for accurate assessments, paving the way for better care.
-
Assessment (A): This part synthesizes the subjective and objective data, leading to a diagnosis or differential diagnosis. It reflects the clinician's clinical reasoning and understanding of the patient's condition, providing a clearer picture of their health.
-
Plan (P): The final section outlines the proposed treatment plan, including further tests, medications, referrals, and follow-up appointments. This organized method guarantees continuity of care and clear communication among medical providers, which is essential in addressing the challenges posed by fragmented medical systems, including regulatory barriers like HIPAA that can obstruct effective communication.
In 2025, around 70% of healthcare providers employ this structured documentation framework, highlighting its significance in clinical practice. Successful applications of documentation have been recorded in various environments, showcasing enhanced communication and improved client outcomes. For instance, a study indicated that rearranging clinical notes to the APSO format improved usability and efficiency during chronic disease appointments, resulting in higher task success rates.
The efficiency of the structured format is broadly acknowledged, with medical professionals observing its function as a cognitive tool that arranges information for easy access, ultimately improving care for individuals. However, it is important to recognize that the framework has limitations, such as its inability to record changes over time, which can influence diagnosis and treatment. Understanding this structure is essential for developing thorough and impactful documentation that promotes clear communication among healthcare professionals and ultimately enhances care for individuals.

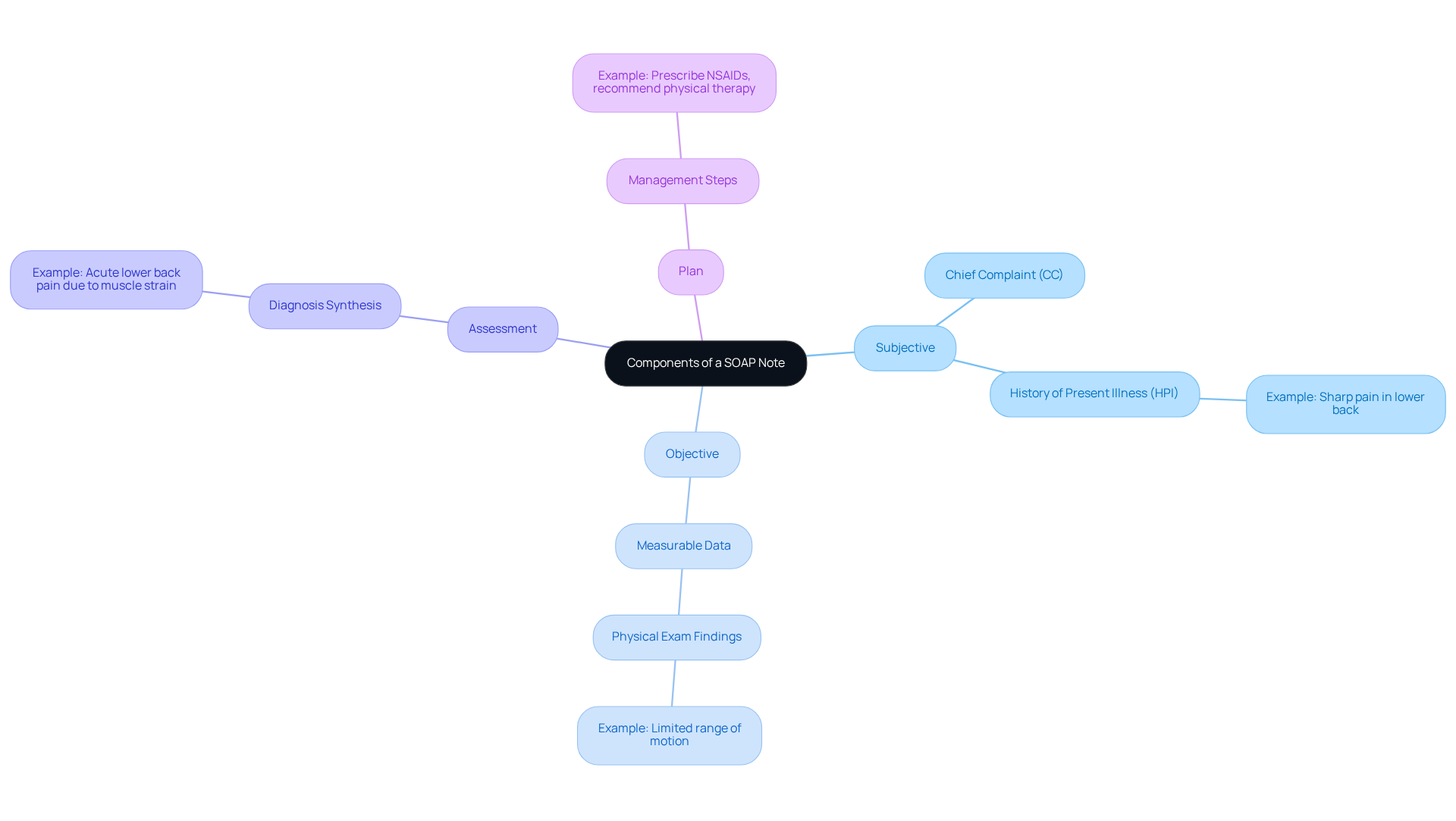
Explore the Components of a SOAP Note
Each component of the lower back pain soap note plays a vital role in effective patient documentation and care management, which can often feel overwhelming for healthcare providers.
-
Subjective: This section captures the patient's chief complaint (CC) and history of present illness (HPI). For instance, an individual might express, "I have a sharp pain in my lower back that started three days ago." This statement provides critical context for the clinician, helping to understand the patient's experience.
-
Objective: Here, measurable data is documented, including physical exam findings. An example could be, "Individual exhibits limited range of motion in the lumbar region and tenderness upon palpation." This information aids in evaluating the physical condition of the individual, fostering a clearer understanding of their needs.
-
Assessment: This part synthesizes the subjective and objective data to form a diagnosis. For example, one might conclude, "Acute lower back pain soap note likely due to muscle strain." This synthesis is crucial as it guides the treatment approach, ensuring that care is tailored to the individual.
-
Plan: The plan outlines the next steps in management. An effective plan might state, "Prescribe NSAIDs for pain relief, recommend physical therapy, and schedule a follow-up in two weeks." This structured approach to care is essential for fostering recovery and support.
Comprehending these elements enables medical practitioners to develop thorough and efficient clinical notes, ultimately improving outcomes for individuals. Have you considered how clarity in documentation can enhance your communication with healthcare teams? As noted by medical professionals, the quality of documentation is crucial for tracking individual progress and ensuring effective collaboration among care providers.
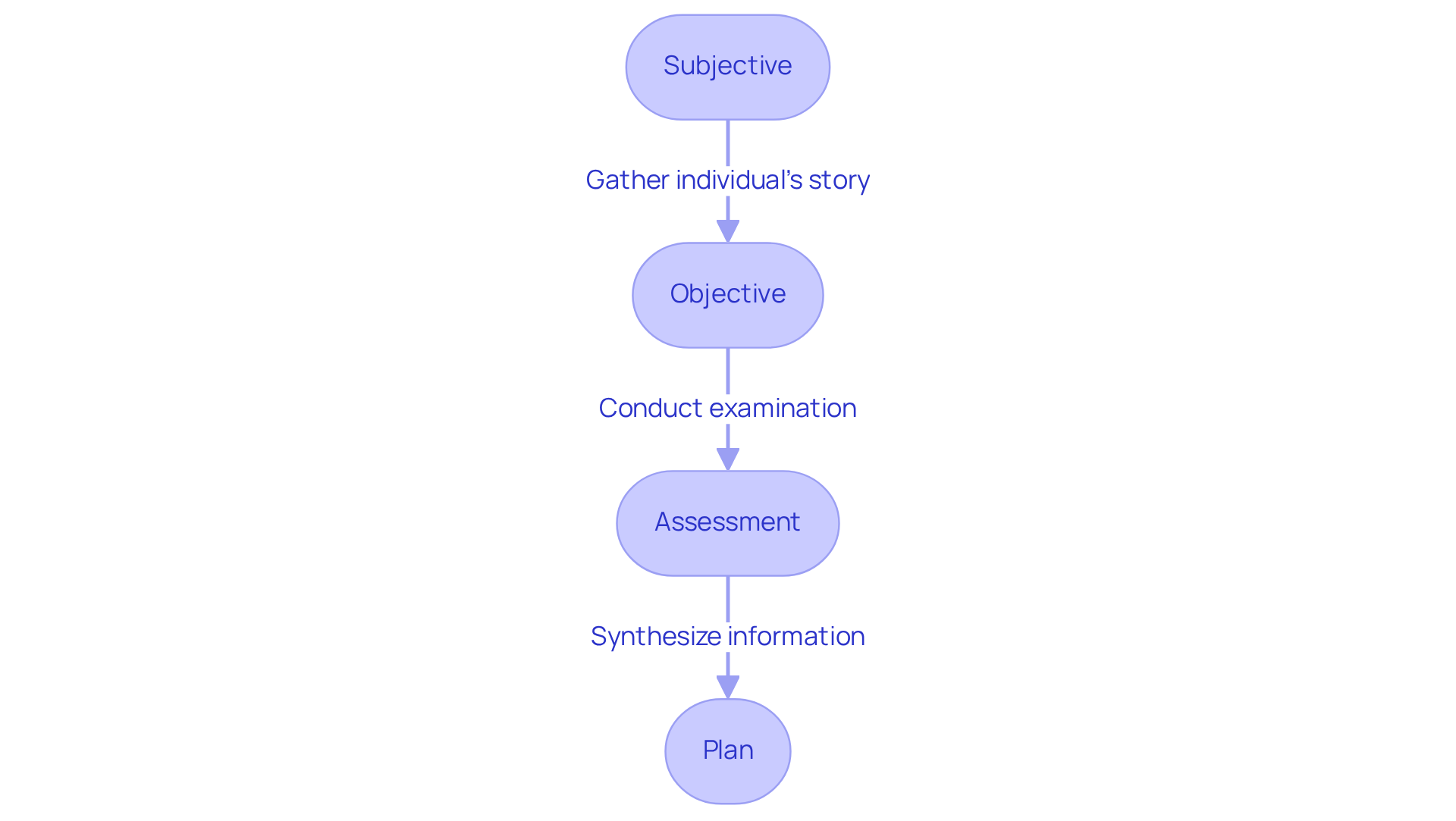
Document Lower Back Pain: Step-by-Step Instructions
To effectively document lower back pain using the SOAP format, it’s important to follow these structured steps with compassion and care:
-
Subjective: Start by gathering the individual’s story. Essential questions to consider include:
- "Can you describe the pain?"
- "When did it begin?"
- "What activities make the pain worse?"
- It’s crucial to document the individual’s responses verbatim whenever possible, as this enhances the accuracy of the record and shows that their voice matters.
-
Objective: Conduct a thorough physical examination and record your findings with attention to detail. Key elements to include are:
- Vital signs (e.g., blood pressure, heart rate)
- Observations (e.g., posture, gait)
- Specific tests (e.g., straight leg raise test)
- Note any abnormalities or limitations in movement, as these details are vital for a comprehensive assessment and show the individual that you are attentive to their needs.
-
Assessment: Synthesize the subjective and objective data to formulate a diagnosis. For example:
- "The patient presents with acute lower back pain likely due to muscle strain, with no neurological deficits noted. Our mission is simple: get you out of pain so you can get back to being you, only better." This analysis should reflect clinical reasoning while considering the individual’s overall condition, recognizing the emotional weight of their experience.
-
Plan: Develop a detailed treatment plan based on your assessment, ensuring it is supportive and clear. This should encompass:
- Medications (e.g., NSAIDs for pain relief)
- Referrals (e.g., physical therapy for rehabilitation)
- Follow-up appointments to monitor progress
- Patient education on their condition and activity modifications to prevent exacerbation of symptoms, empowering them to take charge of their health.
By following these steps, healthcare professionals can create thorough clinical documentation, such as a lower back pain soap note, that accurately reflects the individual’s condition and outlines a clear care plan. It’s important to remember that organized documentation methods can improve record quality by 36.6% and decrease documentation time by 42%, allowing providers to focus more on care rather than paperwork. This approach not only enhances efficiency but also fosters a nurturing environment for both providers and patients.
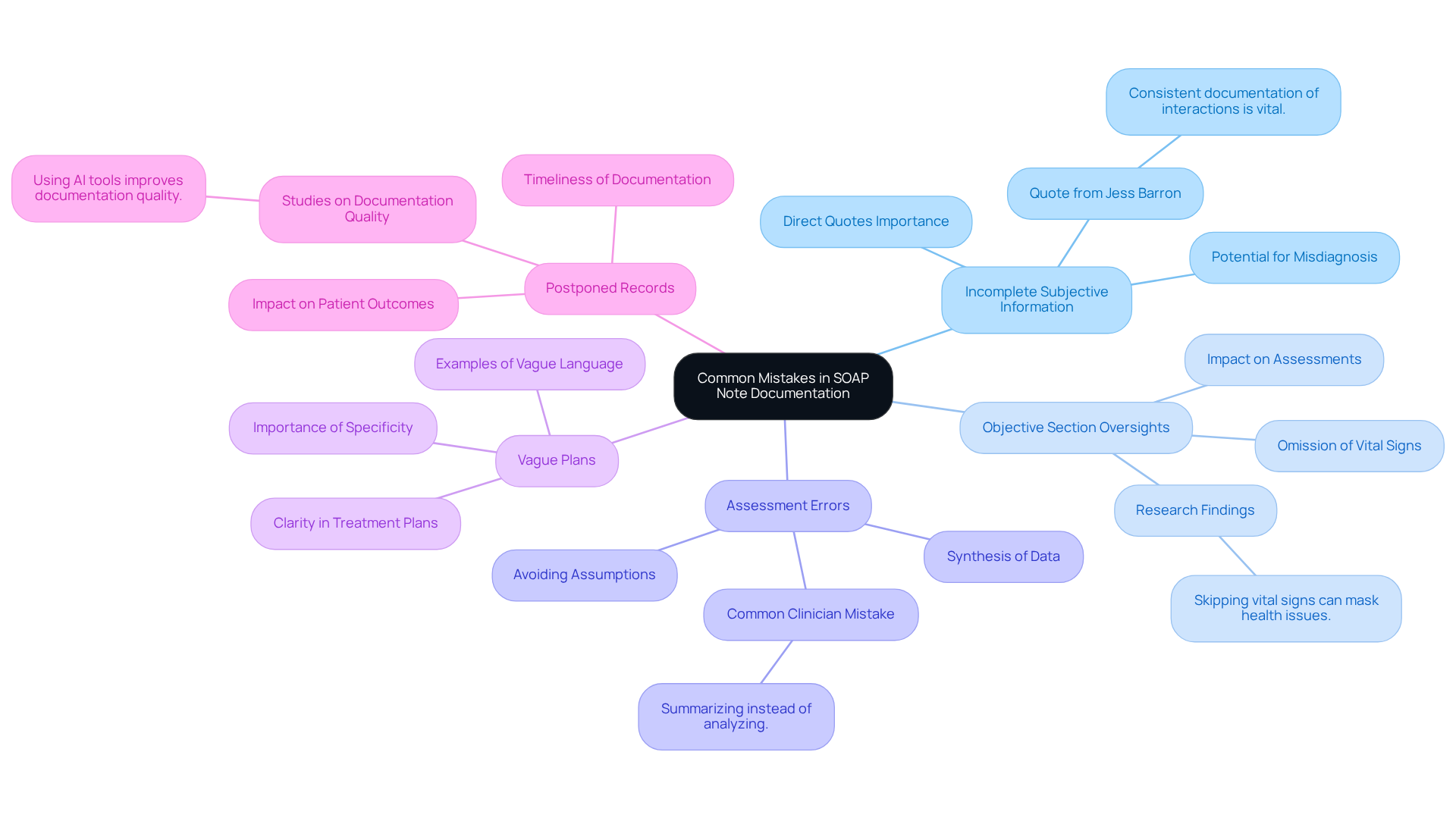
Avoid Common Mistakes in SOAP Note Documentation
Enhancing the quality of your SOAP notes is crucial, and being mindful of common mistakes can make a significant difference. Here are some key areas to focus on:
-
Incomplete Subjective Information: It's essential to capture the complete narrative of the individual by documenting direct quotes and specific symptoms. Summarizing or paraphrasing can lead to the omission of crucial details, potentially compromising diagnosis and treatment. As Jess Barron, Editor-in-Chief at SimplePractice, emphasizes, "Consistent documentation of interactions with your clients and their progress is a vital aspect of treatment."
-
Objective Section Oversights: Ensure that all relevant findings from the physical examination are documented. Omitting vital signs or specific test results can result in incomplete assessments, leading to misdiagnosis or ineffective treatment plans. Research indicates that skipping vital signs can mask underlying health issues, underscoring the importance of thorough documentation.
-
Assessment Errors: Your assessment should synthesize both subjective and objective data. Avoid making assumptions without supporting evidence, as this can weaken clinical interpretation and hinder effective treatment planning. Many clinicians summarize instead of analyzing, which can dilute the quality of the assessment section.
-
Vague Plans: Be explicit in your treatment plan. Rather than using unclear instructions such as 'Follow up as needed,' define the timeframe and criteria for follow-up. This supports accountability and clarity in care, as vague language can undermine clinical clarity and lead to confusion in treatment protocols.
-
Postponed Records: Compose your clinical observations swiftly following the client interaction to guarantee precision and thoroughness. Delaying documentation can result in overlooked details and inaccuracies, negatively impacting outcomes. Studies show that using an ambient AI tool led to higher documentation quality scores, highlighting the benefits of timely and accurate note-taking.
By steering clear of these frequent traps, medical providers can greatly enhance their documentation practices. This ultimately improves care and communication for individuals. Accurate lower back pain SOAP notes have been shown to lead to better patient outcomes, as they facilitate clear communication among healthcare providers and ensure that treatment plans are based on comprehensive and precise information. Reflect on these points, and consider how you can implement these improvements in your practice.
Conclusion
Mastering the SOAP note framework is essential for effective clinical documentation, especially when addressing the emotional and physical challenges of lower back pain. This structured approach not only enhances communication among healthcare providers but also ensures that patient care is thorough and compassionate. By understanding and applying the components of Subjective, Objective, Assessment, and Plan, healthcare professionals can create detailed records that genuinely reflect the individual needs of their patients.
Each section of the SOAP note plays a crucial role. How can capturing the patient's voice, documenting measurable data, synthesizing information for accurate assessments, and outlining clear treatment plans truly contribute to improved patient outcomes? It’s vital to recognize that these elements are interconnected and foundational to quality care. However, common pitfalls in SOAP note documentation, such as incomplete subjective information and vague treatment plans, can hinder this process. Practitioners are encouraged to adopt best practices for accuracy and clarity, ensuring that each note is a true representation of the patient's experience.
Ultimately, effective SOAP note documentation transcends bureaucratic necessity; it is a vital part of delivering quality healthcare. By committing to meticulous documentation, healthcare providers can foster better communication, enhance patient care, and lead to more successful treatment outcomes. Embracing these practices not only benefits individual patients but also strengthens the healthcare system as a whole. It is imperative for all practitioners to refine their documentation skills, recognizing that every note is an opportunity to make a difference in a patient’s journey toward healing.




