Overview
In the demanding world of healthcare, writing effective SOAP notes can feel overwhelming. Have you ever found yourself struggling to document patient information clearly? You're not alone. Many healthcare providers face emotional challenges as they juggle administrative tasks alongside patient care.
Understanding the components of Subjective, Objective, Assessment, and Plan is essential. By mastering this format, you can enhance your clinical reasoning and improve patient care. Clarity and organization in your notes not only streamline your workflow but also ensure that your patients receive the best possible attention.
Here are some key benefits of effective SOAP notes:
- Improved communication with your healthcare team.
- Enhanced patient safety through accurate documentation.
- Increased efficiency in your daily tasks.
As you navigate the complexities of patient documentation, remember that mastering SOAP notes is a journey. Take the time to reflect on your current practices and consider how you can implement these strategies. Your commitment to improving your documentation skills will ultimately lead to better outcomes for your patients. Let's work together to make patient care a priority!
Introduction
Crafting a comprehensive SOAP note is vital for effective nursing practice. It serves as a foundational tool for clear communication and organized patient care. Yet, many nurses face emotional challenges in managing the complexities of documentation amidst their demanding schedules.
How often do you feel overwhelmed by the administrative tasks that take time away from patient care? By mastering the SOAP format—Subjective, Objective, Assessment, and Plan—healthcare professionals can enhance their clinical reasoning and ensure that critical information is conveyed accurately. However, the burden of documentation can feel heavy, impacting not just your workflow but also the quality of care you provide.
Imagine a world where you can streamline this process without sacrificing the quality of care. Here are some key solutions to consider:
- Utilize templates to save time.
- Prioritize documentation during quieter moments.
- Collaborate with your team to share the load.
By implementing these strategies, you can improve patient outcomes and reclaim valuable time for what truly matters—caring for your patients. Let’s explore how we can support each other in this journey toward better documentation and enhanced patient care.
Understand the SOAP Note Format
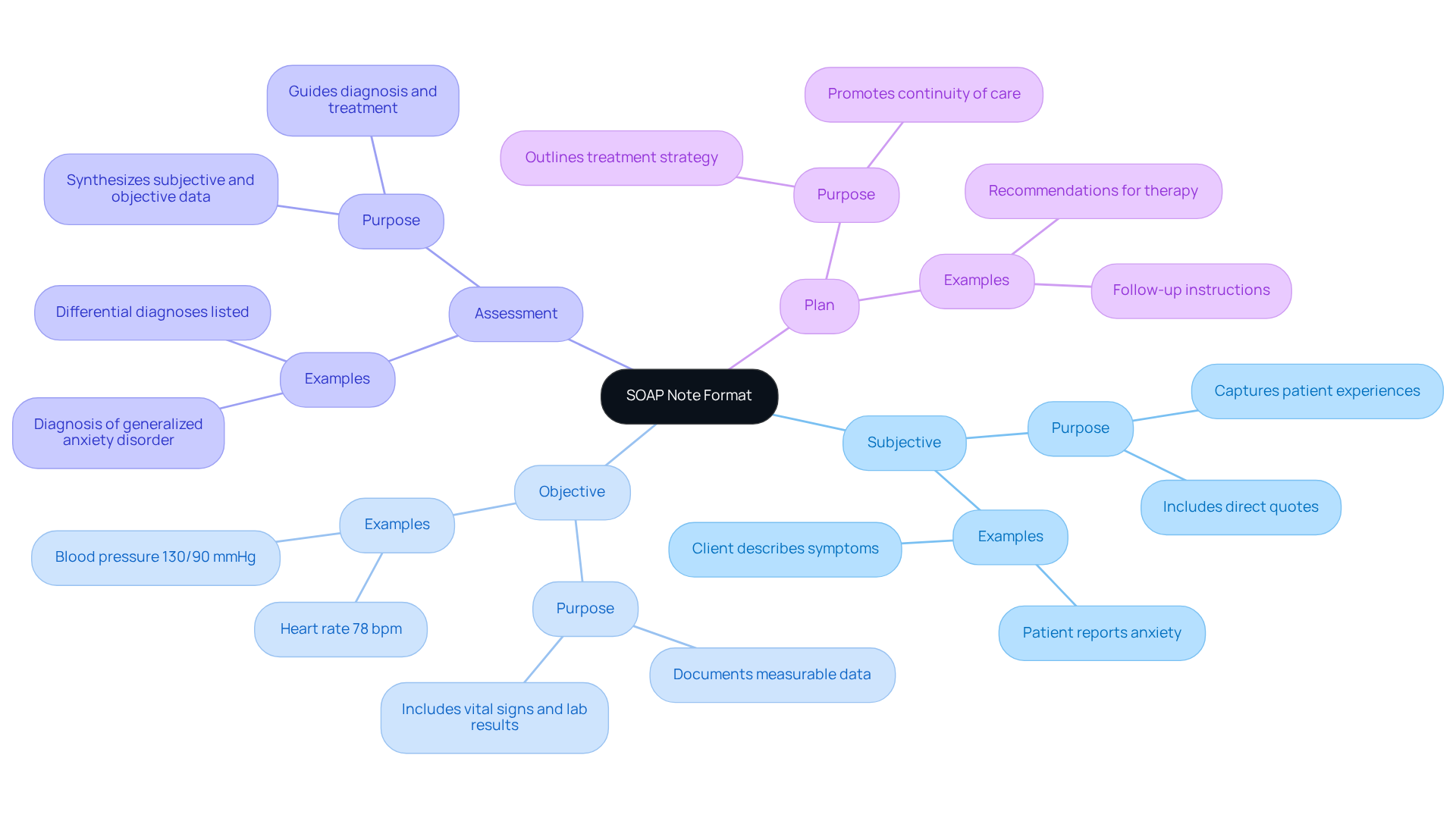
The documentation format is a cornerstone of organized medical records in healthcare, recognized for its clarity and effectiveness. SOAP stands for Subjective, Objective, Assessment, and Plan, with each component serving a distinct purpose:
-
Subjective: This section captures the patient's personal experiences, feelings, and concerns. It often includes direct quotes that reflect their symptoms and emotional state. For example, an individual might say, "I’ve been feeling more anxious this week," which provides important context for their treatment.
-
Objective: Here, healthcare providers document measurable data, such as vital signs, physical examination findings, and laboratory results. For instance, noting a blood pressure of 130/90 mmHg or a heart rate of 78 bpm offers solid proof of the individual's physical state.
-
Assessment: This section synthesizes the subjective and objective information to arrive at a diagnosis or clinical impression. It’s essential for recognizing the primary issue and directing effective treatment choices, ensuring that assistance is tailored to the individual's needs.
-
Plan: The final component outlines the proposed treatment strategy, including medications, further tests, referrals, and education for the individual. A well-organized strategy not only promotes continuity of care but also enhances communication among healthcare providers, ensuring that everyone involved is aligned on the individual's treatment path.
The significance of organized documentation, like SOAP records, cannot be overstated. Have you ever felt overwhelmed by the administrative burdens that can distract from patient care? Research shows that effective documentation supports improved healthcare outcomes and enhances service delivery efficiency. By leveraging generative AI tools, healthcare professionals can automate data entry, integrate with electronic health records, and streamline the documentation process. For example, Dr. Shelagh Fraser reduced writing time from 2-2.5 hours to about 40 minutes with the use of AI, showcasing the effectiveness achieved through organized documentation. Additionally, AI-assisted documentation can cut daily documentation time by an average of 50%.
By understanding how to write a soap note nursing, healthcare professionals can enhance their clinical reasoning and ensure that essential information is conveyed clearly. This ultimately leads to improved quality of service. As one healthcare professional noted, "The documentation assists healthcare professionals in utilizing their clinical reasoning to evaluate, diagnose, and manage an individual based on the information given by them."
Moreover, incorporating AI into the documentation process can help tackle the challenges of disjointed healthcare systems. It makes all pertinent individual information readily available and exchanged among practitioners, improving coordination and continuity of treatment.
In summary, embracing organized documentation and AI tools can significantly alleviate the pressures faced by healthcare providers, allowing them to focus more on what truly matters—their patients.
Explore the Components: Subjective, Objective, Assessment, and Plan
Each component of the SOAP note plays a critical role in patient documentation:
-
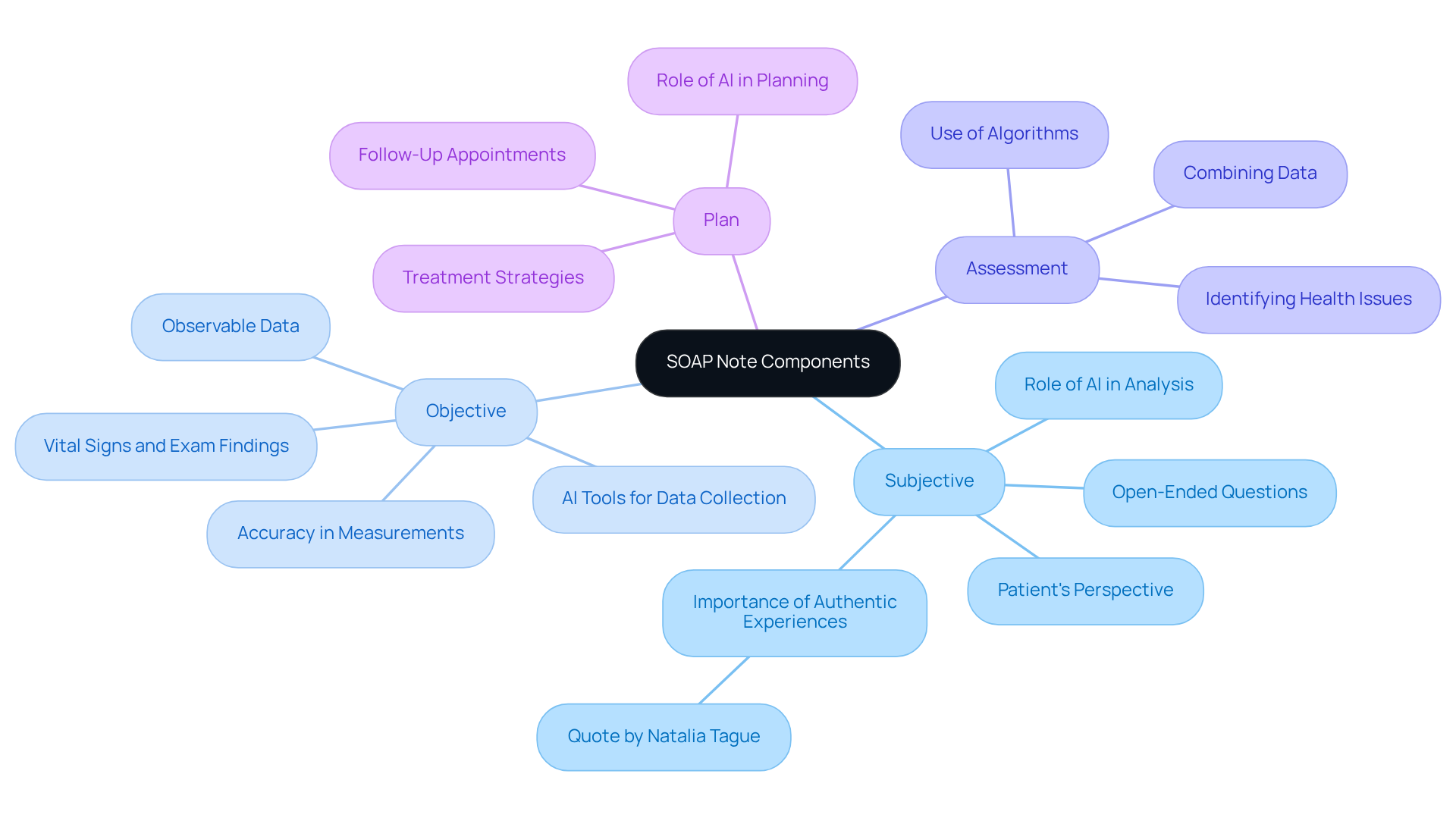
Subjective: Focus on the patient's perspective. Ask open-ended questions to gather detailed information about their symptoms and concerns. For example, instead of asking, 'Are you in pain?' you might ask, 'Can you describe how you feel?' As Natalia Tague, a licensed counselor, emphasizes, the subjective section captures authentic client experiences, which is essential for personalized care. Utilizing generative AI can further improve this process by analyzing responses and identifying key themes, allowing for a more nuanced understanding of individual needs.
-
Objective: Understand how to write a soap note nursing by recording observable and measurable data. This includes vital signs (e.g., blood pressure, heart rate), physical exam findings (e.g., swelling, redness), and results from diagnostic tests. Ensure accuracy and clarity in your measurements, as these provide a factual basis for clinical decisions. For example, an individual's blood pressure reading can signify underlying health concerns, directing further evaluation and intervention. AI tools can assist in automating the collection and analysis of this data, improving efficiency and accuracy in documentation.
-
Assessment: Combine the subjective and objective data to understand how to write a soap note nursing for formulating a clinical judgment. This may involve identifying the individual's primary health issues and any potential complications. For instance, if an individual reports increased pain (subjective) and exhibits elevated blood pressure (objective), the assessment may highlight the need for immediate intervention. Advanced algorithms can assist physicians in making these evaluations by identifying patterns in medical data that may not be readily apparent.
-
Plan: Create a detailed strategy that includes how to write a soap note nursing to address the individual's needs. This should include treatment options, follow-up appointments, and any necessary referrals. Be specific about the interventions and the rationale behind them. For instance, if an individual is experiencing anxiety, the plan might include cognitive behavioral therapy sessions and a referral to a psychiatrist for medication evaluation. By incorporating AI into the planning process, healthcare providers can ensure that their strategies are informed by the latest evidence and customized to individual circumstances, while also addressing the administrative burdens that often complicate care delivery.
Including both subjective and objective data not only improves the quality of evaluations but also conforms to best practices in healthcare documentation. Efficient communication via structured documentation enhances greater involvement of individuals, ultimately resulting in better health results. The client engagement solution market is anticipated to exceed $21.6 billion by 2030, emphasizing the increasing significance of efficient documentation in improving client involvement and care delivery.
Follow a Step-by-Step Process to Write a SOAP Note
Writing an effective SOAP note and learning how to write a soap note nursing can feel overwhelming, especially when you're juggling numerous responsibilities. But don’t worry; following these steps can make the process smoother and more manageable:
-
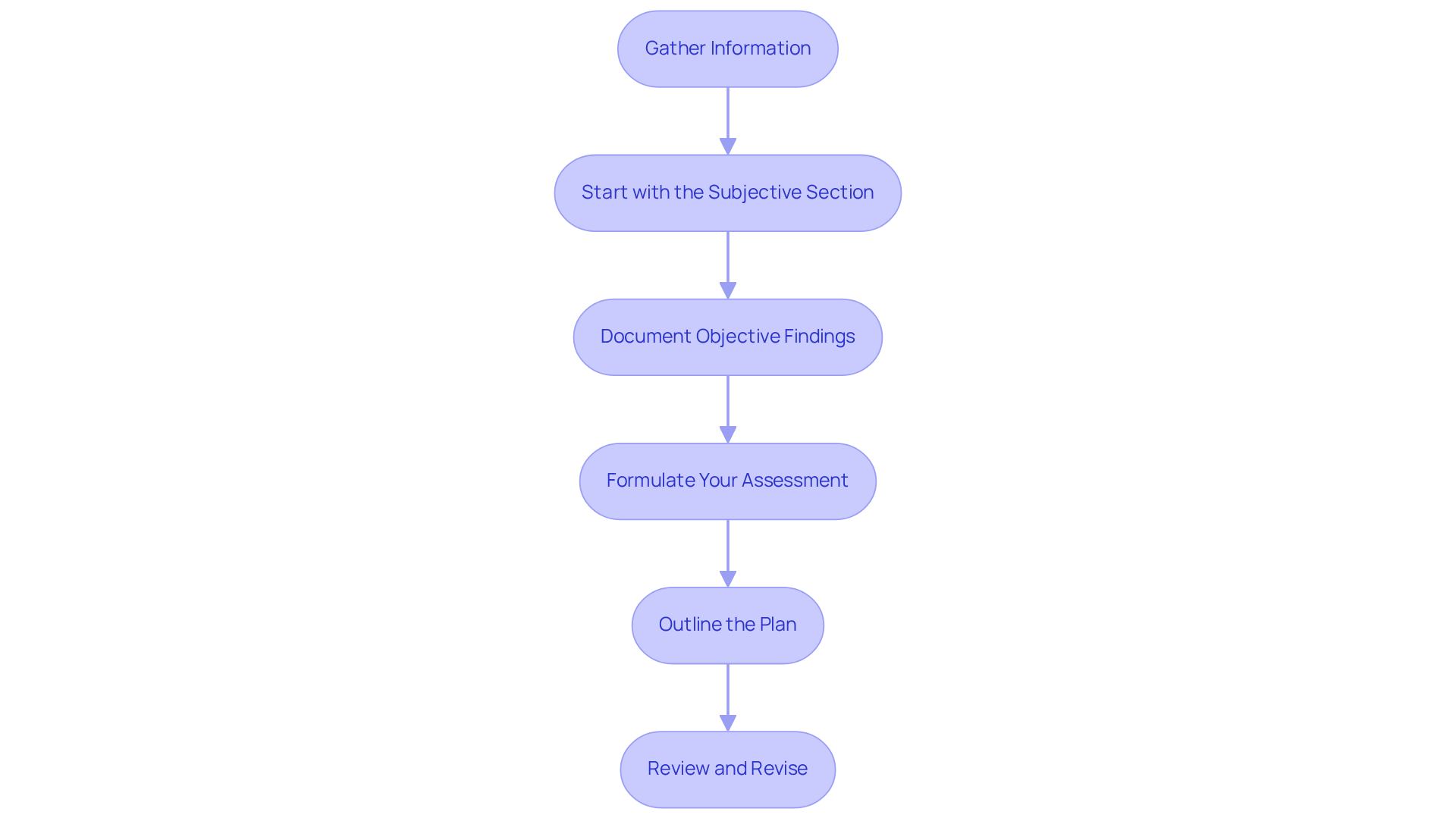
Gather Information: Start by collecting all relevant individual information, including medical history, current medications, and any previous notes. This foundational step ensures you have a comprehensive understanding of how to write a soap note nursing, which is crucial for effective care.
-
Start with the Subjective Section: Document the individual's statements in their own words. Use quotes where appropriate to accurately capture their feelings and concerns. This section should reflect their narrative, including their chief complaint and history of present illness. How often do we overlook the importance of truly listening to our patients?
-
Document Objective Findings: Record measurable data from your examination and tests, such as vital signs and lab results. Make sure this information is clear and concise, distinguishing between subjective symptoms and objective signs. Clarity in how to write a soap note nursing can significantly impact patient outcomes.
-
Formulate Your Assessment: Analyze the subjective and objective data to arrive at a diagnosis or clinical impression. Justify your assessment based on the information provided by demonstrating how to write a soap note nursing, synthesizing all relevant details to support your clinical reasoning. This step is where your expertise shines through.
-
Outline the Plan: Clearly state the next steps in the individual's care, including treatments, referrals, and follow-up actions. Ensure the plan is patient-centered, incorporating how to write a soap note nursing that aligns with their values and preferences. Including necessary testing and rationale can make all the difference in their journey to recovery.
-
Review and Revise: After drafting the SOAP document, take a moment to review it for clarity and completeness. Ensure that all sections are correctly completed and that the message thoroughly represents the individual's circumstances. Quick proofreading is essential to ensure the accuracy of names, medications, dosages, and observations.
Integrating organized documentation methods, including how to write a soap note nursing, not only boosts communication among healthcare professionals but also enhances outcomes for those receiving treatment. Understanding how to write a soap note nursing is essential for efficient documentation, which preserves precise medical records and guarantees continuity of care.
Common Challenges: Healthcare professionals often face typical difficulties in understanding how to write a soap note nursing, such as time limitations and the necessity for clarity. To help with this, consider using tools like the OLDCARTS and HEADSS acronyms to arrange patient information efficiently.
By embracing these practices, you can alleviate some of the administrative burdens that impact patient care. Remember, your role is vital, and every note you write contributes to a larger picture of health and healing.
Apply Best Practices and Avoid Common Mistakes
To enhance your SOAP note writing, it’s important to consider some best practices that can truly make a difference:
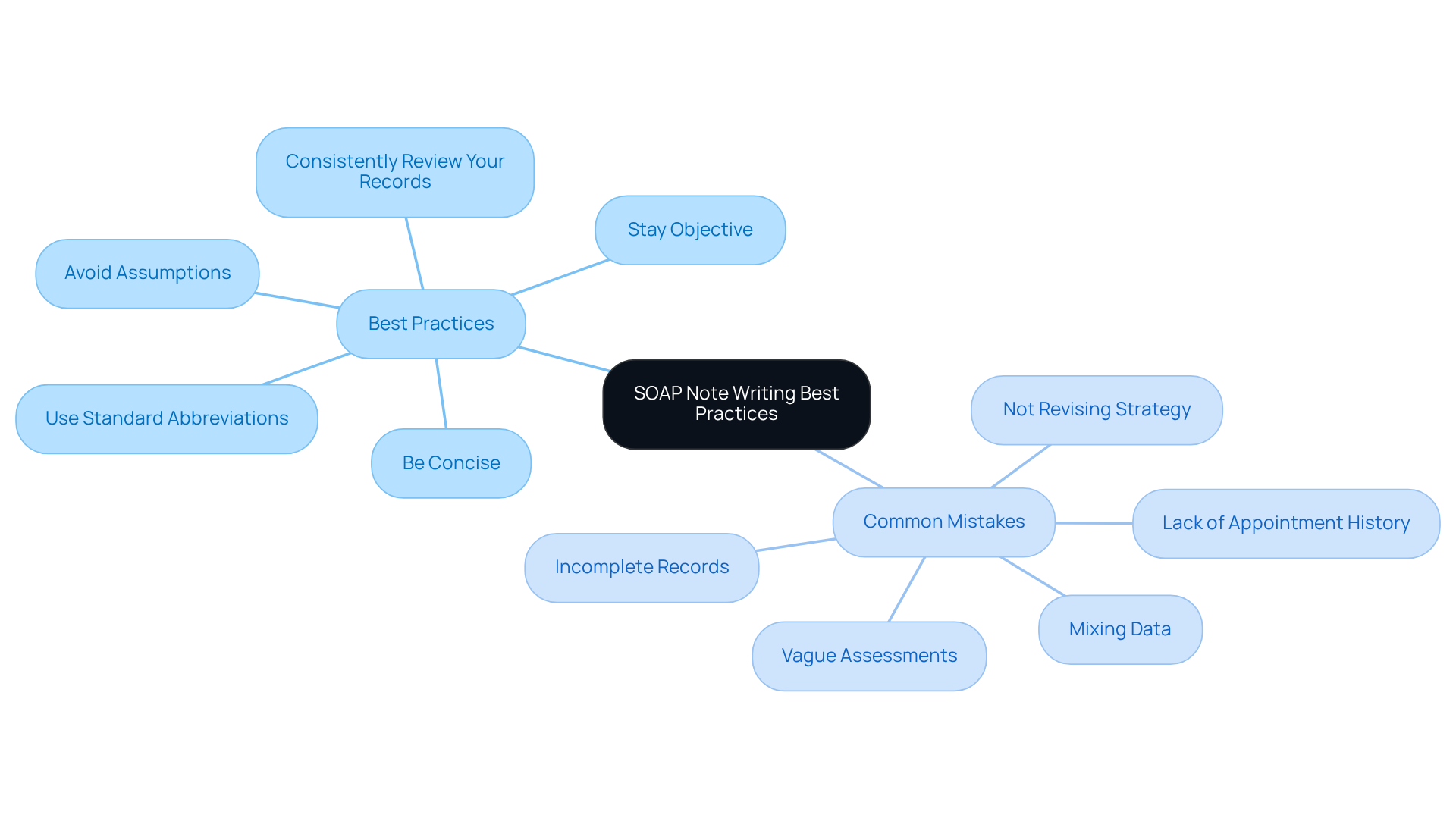
- Be Concise: Clear and straightforward language is key. SOAP notes should be brief, focused, informative, and always written in the past tense. Avoid unnecessary jargon that might confuse readers.
- Stay Objective: While the subjective section captures the individual’s feelings, ensure that the objective section is based solely on measurable data. Document observable client behavior, interventions used, and measurable outcomes, steering clear of general statements without supporting data.
- Use Standard Abbreviations: Familiarizing yourself with commonly accepted medical abbreviations can save time and maintain clarity in your notes.
- Avoid Assumptions: Record only what you witness or what the individual communicates. It’s crucial to avoid making assumptions about the individual’s condition and ensure that the subjective section doesn’t include unsourced opinions.
- Consistently Review Your Records: Periodically revisiting your documentation can help identify areas for improvement. Documenting SOAP notes right after interactions with clients enhances precision and decreases the likelihood of overlooking significant details.
Common mistakes to avoid include:
- Failing to include all relevant information in each section, which can lead to incomplete records.
- Mixing subjective and objective data, resulting in confusion and misinterpretation.
- Writing vague assessments that lack clear clinical insights, hindering effective treatment planning.
- Failing to revise the strategy according to the individual’s progress or changes in their condition, which can undermine the quality of support.
- Not maintaining a record of the patient’s appointment history, which can provide valuable insights into their engagement with care.
By keeping these practices in mind, you can improve how to write a soap note nursing and ultimately enhance the care you provide to your clients.
Conclusion
Mastering the art of writing SOAP notes is vital for nursing professionals who genuinely care about delivering high-quality patient care. Have you ever felt overwhelmed by the administrative tasks that take time away from your patients? By understanding and effectively utilizing the SOAP format—Subjective, Objective, Assessment, and Plan—you can communicate essential information clearly and concisely. This structured approach not only enhances your documentation but also contributes to improved healthcare outcomes through better coordination and continuity of care.
Each component of the SOAP note plays a significant role in patient care. The subjective section captures the patient's voice, allowing you to understand their concerns. The objective section provides measurable data, giving you a clear picture of their condition. The assessment synthesizes these elements into a clinical impression, while the plan outlines the necessary steps for treatment. Moreover, integrating AI tools can streamline your documentation processes, enabling you to focus more on meaningful patient interactions rather than getting bogged down by paperwork.
So, how can you adopt best practices for SOAP note writing? By avoiding common pitfalls and embracing a systematic approach, you can enhance your clinical reasoning and documentation skills. This commitment not only benefits your individual patients but also elevates the overall quality of healthcare delivery. As the demand for effective documentation continues to grow, investing time and effort into mastering SOAP notes will undoubtedly pay dividends in your pursuit of excellence in nursing practice.
Key Solutions for Effective SOAP Note Writing:
- Embrace the structured format to enhance clarity.
- Utilize AI tools to reduce administrative burdens.
- Focus on the patient’s voice in the subjective section.
- Ensure measurable data is captured in the objective section.
Remember, your dedication to mastering SOAP notes is a step towards not just improving your practice but also enriching the lives of those you care for. Let's continue to strive for excellence together!




