Overview
Navigating the complexities of healthcare can be overwhelming, can't it? Many providers face emotional challenges as they juggle patient care with administrative tasks. This burden can often detract from the quality of care they wish to provide.
That’s where effective documentation comes in. The article offers a comprehensive step-by-step guide on filling out SOAP notes, focusing on the importance of each section: Subjective, Objective, Assessment, and Plan. By adopting best practices for documentation, such as using concise language and standardized terminology, healthcare providers can enhance clarity and accuracy.
Here are some key solutions to consider:
- Use real-time documentation to capture details accurately.
- Emphasize concise language to improve communication.
- Standardize terminology to ensure everyone is on the same page.
These practices not only streamline the documentation process but also significantly improve patient care. Imagine the peace of mind that comes from knowing your notes are clear and precise!
So, let’s take action together. By implementing these strategies, you can alleviate some of the administrative burdens and focus more on what truly matters—your patients. Remember, every step you take towards better documentation is a step towards better care.
Introduction
Structured documentation is vital in healthcare, yet many professionals feel overwhelmed by the complexities of capturing patient information. Have you ever found yourself struggling to keep track of vital details? The SOAP note framework—comprising Subjective, Objective, Assessment, and Plan—provides a streamlined approach to this intricate task, ensuring that essential information is recorded systematically.
As technology becomes more integrated into our practices, how can we effectively harness these tools to improve our documentation? This article aims to help you master the art of filling out SOAP notes. We’ll provide a step-by-step guide that clarifies each component while addressing common challenges and best practices.
By embracing this structured approach, you can enhance your documentation practices and ultimately elevate patient care. Let’s explore how you can make this process smoother and more efficient.
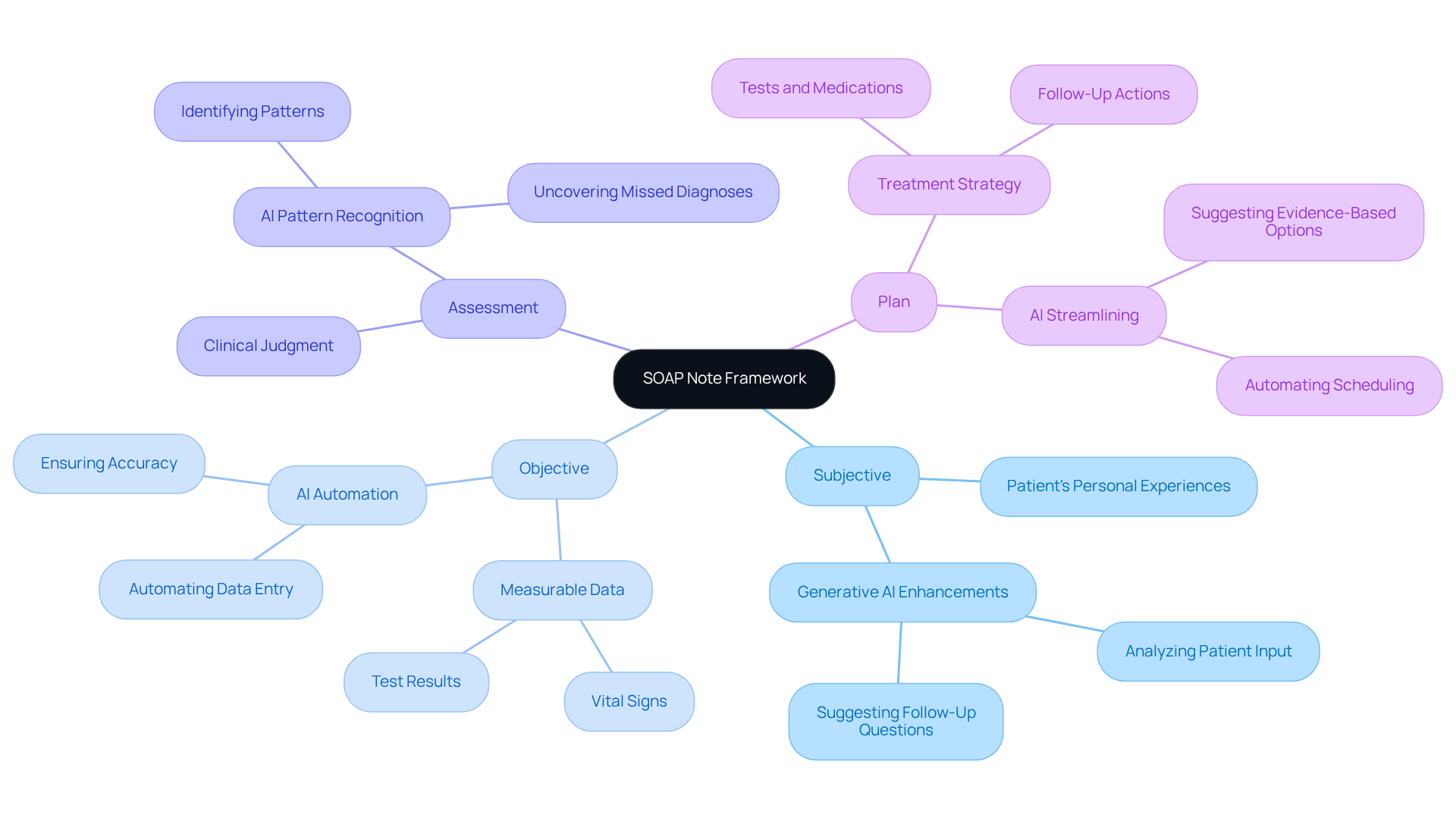
Understand the SOAP Note Framework
Structured documentation notes offer a thoughtful way for healthcare professionals to record individual information systematically. Have you ever felt overwhelmed by the sheer volume of details to capture? The acronym SOAP—Subjective, Objective, Assessment, and Plan—provides a clear framework to ease this burden. Each section plays a vital role:
-
Subjective: This part captures the patient's personal experiences, feelings, and symptoms as they share them. It’s about listening to their voice and understanding their journey. Imagine how generative AI could enhance this by analyzing patient input and suggesting follow-up questions, ensuring no concern goes unaddressed.
-
Objective: Here, healthcare providers document measurable and observable data, like vital signs and test results. Wouldn’t it be great if AI tools could automate data entry? This would not only ensure accuracy but also free up providers to focus on what truly matters—interpreting the data and connecting with patients.
-
Assessment: This section merges subjective and objective information to form a clinical judgment about the individual’s condition. AI algorithms can help identify patterns, leading to more accurate assessments and potentially uncovering diagnoses that might have been missed.
-
Plan: Finally, this section outlines the proposed treatment strategy, including tests, medications, and follow-ups. Generative AI can streamline this process by suggesting evidence-based options and automating scheduling, ensuring everyone on the healthcare team is aligned and focused on the patient’s care.
Understanding how to fill out SOAP notes is crucial for effective communication among healthcare providers and for maintaining comprehensive client records. Research shows that efficient documentation can lead to accurate diagnoses and quicker treatments. As healthcare professionals learn how to fill out SOAP notes, they gain clarity and efficiency in record-keeping, ultimately enhancing patient care. As HealthOrbit AI states, 'structured documentation continues to be one of the most reliable formats in clinical medicine.' This highlights its enduring importance.
Moreover, well-crafted records serve as essential legal documents for audits, billing verifications, or legal assessments. This underscores the need for precision and thoroughness in record-keeping. By utilizing organized documentation templates, enhanced by AI features, healthcare providers can simplify the recording process, making it quicker and more efficient.
Are you ready to embrace these tools and improve your documentation practices? Together, we can enhance patient care and streamline your workflow.
Break Down the Components: Subjective, Objective, Assessment, and Plan
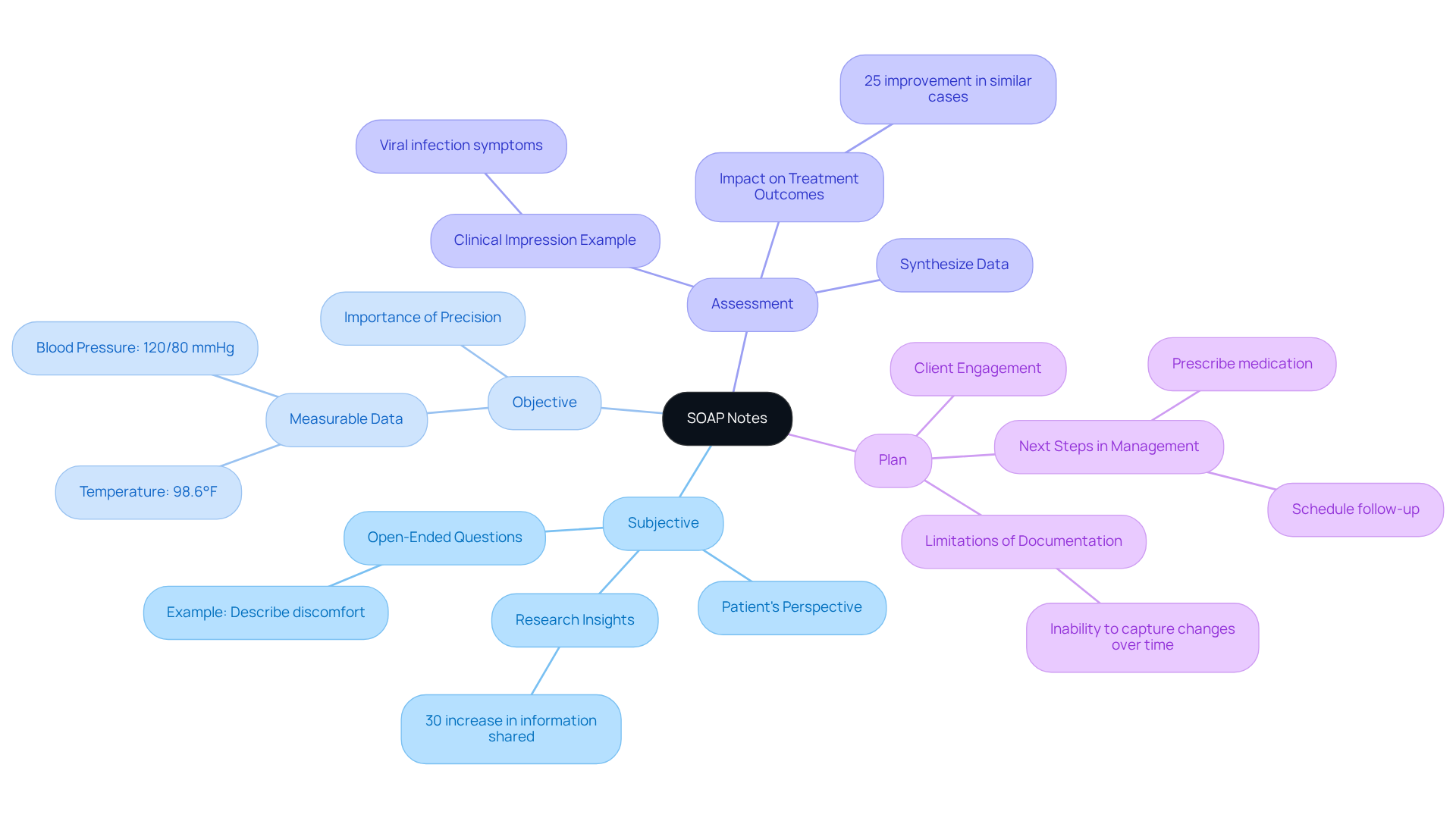
Completing SOAP notes effectively can be a challenge for healthcare providers, and understanding each component is crucial to alleviating some of that burden:
-
Subjective: It’s important to capture the patient’s perspective using their own words. Open-ended questions can encourage them to share more. Instead of asking, ‘Are you in pain?’, try, ‘Can you describe any discomfort you are feeling?’ Research shows that this approach can lead to a 30% increase in the amount of information shared. This not only helps you understand the individual’s experience better but also aligns with effective interviewing practices.
-
Objective: It is essential to understand how to fill out SOAP notes to document measurable data with precision. Include specific metrics like blood pressure readings, temperature, and lab test results. For example, ‘Blood pressure: 120/80 mmHg; Temperature: 98.6°F.’ This objective data is vital for forming a clear clinical picture and supports your assessment process. Healthcare professionals agree that precise documentation is key for effective management and treatment planning.
-
Assessment: Here, you synthesize the subjective and objective data to create a cohesive clinical impression, which is essential for understanding how to fill out SOAP notes. For instance, ‘Patient presents with symptoms consistent with a viral infection, as evidenced by elevated temperature and reported fatigue.’ This section is crucial for guiding treatment decisions and ensuring continuity of care. A case study highlighted that comprehensive evaluations led to a 25% improvement in treatment outcomes for similar cases.
-
Plan: Clearly outline how to fill out SOAP notes as the next steps in managing the individual. This could involve prescribing medication, scheduling follow-up appointments, or recommending lifestyle changes. For example, ‘Prescribe antiviral medication; follow up in one week to reassess symptoms.’ A well-defined plan not only enhances client engagement but also sets clear expectations for ongoing care. However, it’s important to recognize that the documentation format has limitations, such as its inability to capture changes over time, which can hinder monitoring client progress.
By carefully dissecting these elements and incorporating empirical evidence, you can create detailed notes that are not only thorough but also essential in promoting effective care for individuals. Remember, you’re not alone in this; acknowledging these challenges is the first step towards improving your practice.
Fill Out Each Section: Step-by-Step Instructions
Here’s how to fill out each section of a SOAP note:
-
Subjective:
- Begin by warmly greeting the patient and establishing a connection.
- Ask open-ended questions to gather detailed insights about their symptoms and concerns.
- When possible, record the individual’s responses verbatim, using quotation marks for direct quotes.
- For example, the patient might say, “I have been feeling very tired and have a persistent cough.”
-
Objective:
- Conduct a thorough physical examination and gather vital signs.
- Document any observable findings, such as skin color, swelling, or range of motion.
- Include results from any diagnostic tests performed.
- An example could be: Physical exam reveals mild wheezing; chest X-ray shows no abnormalities.
-
Assessment:
- Analyze the subjective and objective data to formulate a clinical impression.
- Consider possible diagnoses and document your reasoning clearly.
- For instance, the assessment might indicate acute bronchitis based on the individual’s history and examination findings.
-
Plan:
- Clearly outline the treatment plan in a concise manner.
- Specify any medications, referrals, or follow-up actions needed.
- An example could be: The plan includes prescribing a bronchodilator and scheduling a follow-up appointment in two weeks.
By learning how to fill out soap notes, healthcare professionals can create effective documentation that not only enhances patient care but also fosters better communication. Remember, each note is a step towards understanding and supporting your patients more effectively.
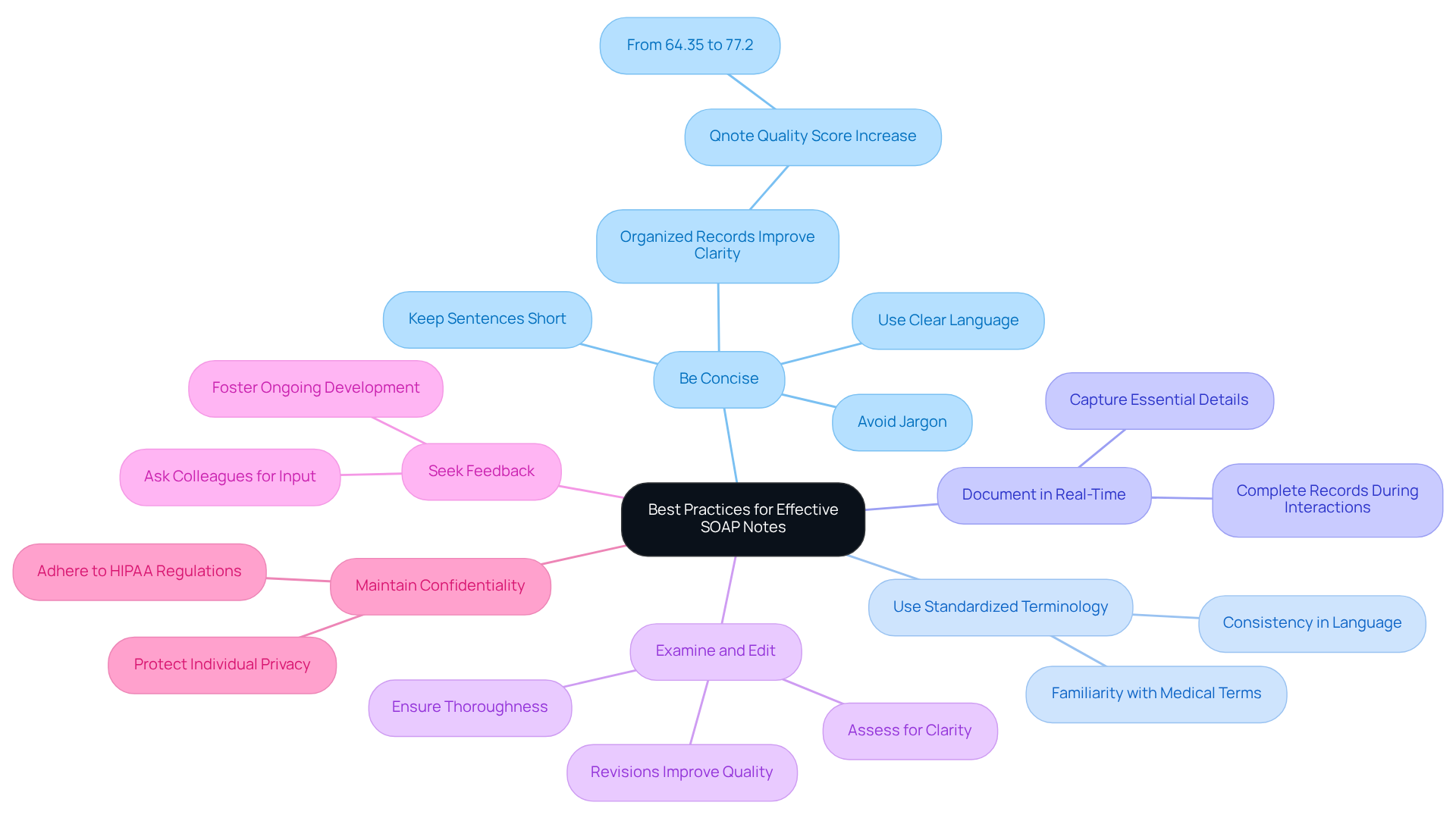
Implement Best Practices for Effective SOAP Notes
To ensure your SOAP notes are effective, consider these best practices:
- Be Concise: Use clear and straightforward language. Avoid unnecessary jargon and keep sentences short to enhance readability. Research shows that organized records can boost clarity, with quality ratings significantly improving when brief entries are used. For example, organized records raised the Qnote quality score from 64.35 to 77.2, a notable increase of 12.8 points (p < 0.001).
- Use Standardized Terminology: Consistency in language helps avoid confusion. Familiarize yourself with common medical terms and abbreviations; this standardization is crucial for effective communication among healthcare providers.
- Document in Real-Time: Complete clinical records during or right after interactions with clients to ensure precision and thoroughness. This practice captures essential details and aligns with findings that highlight the importance of prompt record-keeping in enhancing care for individuals.
- Examine and Edit: After finalizing your documentation, take a moment to assess it for clarity and thoroughness. Revisions are vital to ensure that the record accurately reflects the patient encounter. Comprehensive reporting reduces risks and improves the quality of care. As employment lawyer Stuart Rudner notes, "Documentation is critical. Cases will be decided based upon the evidence, and not necessarily the truth."
- Seek Feedback: Regularly ask colleagues for feedback on your SOAP notes. Constructive feedback can help you enhance your writing skills over time, fostering a culture of ongoing development in clinical practices.
- Maintain Confidentiality: Always ensure that individual information is kept confidential and secure, adhering to HIPAA regulations. Proper records not only protect individual privacy but also uphold legal and ethical principles in healthcare. Keith Carlson, RN, encourages new nurses to write as though their entries could be examined in court.
By applying these best practices, healthcare providers can learn how to fill out SOAP notes effectively, which will improve the quality of their documentation, leading to better care for individuals and enhanced communication within the healthcare team. Effective documentation isn't just a regulatory requirement; it's a cornerstone of high-quality patient care.
How can you implement these practices in your daily routine? Reflect on your current documentation habits and consider how these strategies might ease your administrative burdens, allowing you to focus more on what truly matters—your patients.
Conclusion
Mastering the art of filling out SOAP notes is crucial for healthcare professionals who want to improve patient care and simplify their documentation processes. Have you ever felt overwhelmed by the administrative tasks that take time away from your patients? By understanding and applying the SOAP framework—Subjective, Objective, Assessment, and Plan—you can create structured and effective records that enhance communication and ensure comprehensive client care.
Throughout this guide, we’ve shared key insights on capturing patient experiences, documenting measurable data, synthesizing information for clinical judgments, and outlining clear treatment plans. Best practices like real-time documentation, using standardized terminology, and seeking feedback can significantly elevate the quality of your SOAP notes. This ultimately leads to better patient outcomes and a more efficient healthcare environment.
As the healthcare landscape evolves, incorporating advanced tools and methodologies into your documentation practices is more vital than ever. Embracing these strategies not only promotes accuracy and clarity but also fosters a culture of continuous improvement in patient care. Reflect on your current documentation habits: how can these practices be integrated into your daily routines to ensure that patient needs remain at the forefront of healthcare delivery?
Key Solutions to Enhance Your SOAP Notes:
- Real-time documentation to capture insights as they happen.
- Standardized terminology for consistency and clarity.
- Regular feedback to refine your approach.
It’s time to take action. By reflecting on your documentation practices and embracing these strategies, you can make a meaningful impact on your patients’ care. Let’s work together to ensure that every patient feels valued and understood.




