Overview
In the demanding world of healthcare, providers often face emotional challenges that can impact their ability to deliver optimal care. The article highlights essential steps to help healthcare professionals master clinical notes, focusing on practical solutions that can ease administrative burdens and enhance patient interactions. By selecting appropriate frameworks like SOAP and SBAR, identifying key components such as patient identification and assessment, and implementing efficient note-taking strategies, providers can significantly improve their documentation practices.
Understanding the legal and ethical considerations surrounding clinical notes is crucial. The emphasis on confidentiality and accuracy not only protects patients but also fosters trust in the healthcare relationship. This comprehensive guide serves as a nurturing resource, offering insights that ultimately enhance patient care and compliance.
As you navigate these challenges, consider how these strategies can transform your documentation process. Reflect on the benefits of improved clinical notes—not just for compliance, but for the quality of care you provide. By taking these steps, you can create a more supportive environment for both yourself and your patients. Let’s embrace these practices together, ensuring that every note contributes to a better healthcare experience.
Introduction
Crafting effective clinical notes is not just a task; it’s a vital part of healthcare that can profoundly affect patient outcomes and communication among providers. Many healthcare professionals face the emotional challenge of balancing thorough documentation with the demands of their daily responsibilities. How often do you feel overwhelmed by paperwork while striving to provide the best care for your patients? By exploring various frameworks and essential components of clinical documentation, you can enhance your practice and streamline patient care.
However, the challenge remains: how can we ensure that our notes reflect the care we provide without adding to our already heavy workload? This article delves into essential steps for mastering clinical notes, offering strategies that improve efficiency and uphold legal and ethical standards in patient care. Together, we can navigate these challenges and foster a more supportive environment for both providers and patients.
Select a Clinical Note Framework
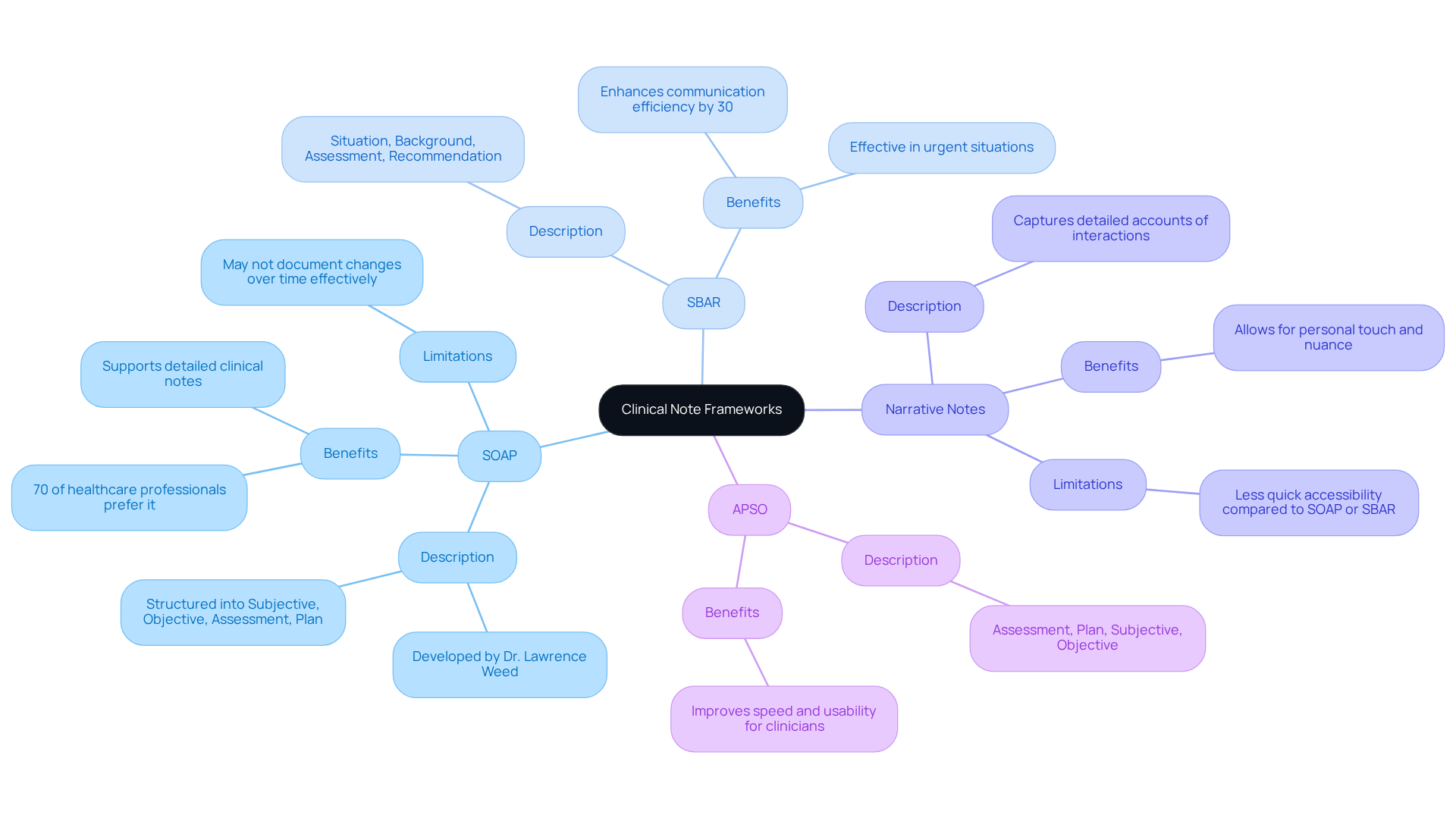
To begin, it's essential to choose a framework for clinical notes that resonates with your practice. Consider the emotional challenges you face daily and how the right framework can alleviate some of those burdens. Here are a few common frameworks that may suit your needs:
-
SOAP (Subjective, Objective, Assessment, Plan): Developed by Dr. Lawrence Weed in the 1960s, this widely adopted method organizes notes into four clear sections, making it straightforward to follow and review. Approximately 70% of healthcare professionals prefer SOAP formats due to their clarity and structure, which supports the creation of detailed clinical notes. However, it's important to note that some critiques highlight its limitations in clinical notes when documenting changes over time, potentially impacting effective clinical decision-making.
-
SBAR (Situation, Background, Assessment, Recommendation): This framework is particularly effective for concise communication, especially in urgent situations. SBAR facilitates quick information transfer, and research shows it can enhance communication efficiency by up to 30% in critical care settings. This makes it a preferred choice among healthcare professionals during handoffs or emergencies.
-
Narrative Notes: These notes are invaluable for capturing detailed accounts of interactions with individuals, allowing for a personal touch. They shine in contexts where nuance and detail are crucial, although they may not provide the quick accessibility found in SOAP or SBAR formats.
When selecting a framework, reflect on the specific needs of your practice and the preferences of your team as indicated in the clinical notes. Have you considered discussing your experiences with coworkers? Their insights could be instrumental in identifying a framework that enhances your clinical notes and the care you provide. Additionally, exploring the APSO format (Assessment, Plan, Subjective, Objective) may offer improved speed and usability for clinicians, further supporting effective documentation.
By thoughtfully considering these options, you can foster a more efficient and compassionate approach to clinical notes, ultimately benefiting both your practice and your patients.
Identify Essential Components of Clinical Notes
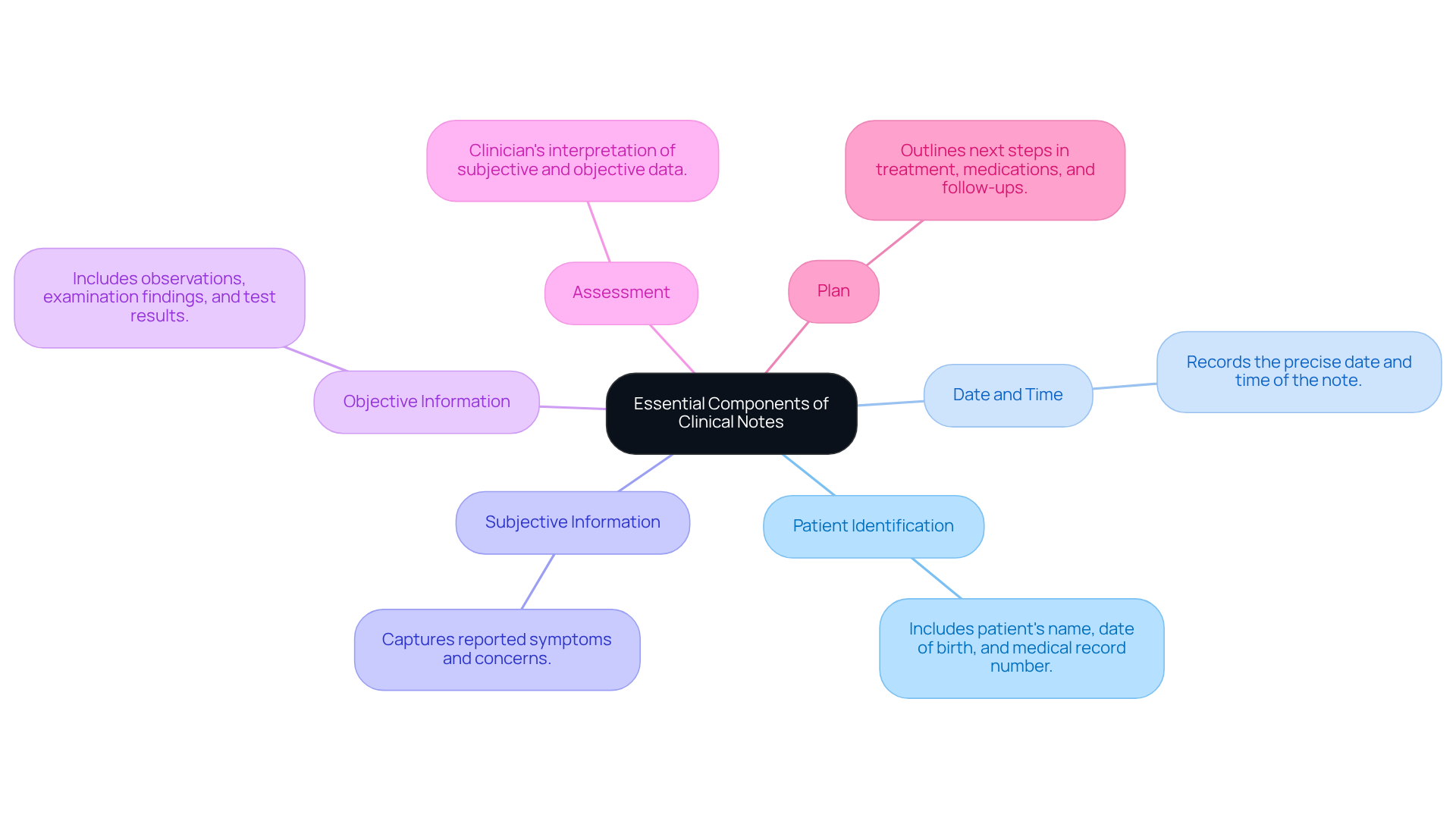
Crucial elements of clinical notes are vital for ensuring comprehensive care and fostering effective communication among healthcare professionals. These components include:
- Patient Identification: Clearly documenting the patient's name, date of birth, and medical record number is essential for accurate identification and continuity of care.
- Date and Time: Recording the precise date and time when the note is made is crucial for monitoring progress and treatment schedules.
- Subjective Information: Capturing the individual's reported symptoms and concerns provides insight into their experience and perspective on their health.
- Objective Information: Including observations, physical examination findings, and test results presents a factual basis for clinical decisions.
- Assessment: This section offers the clinician's interpretation of the subjective and objective data, synthesizing information to create a clear understanding of the individual's condition.
- Plan: Outlining the next steps in treatment, detailing medications, referrals, and follow-up appointments ensures a structured approach to care.
Comprehensive clinical notes are not only a regulatory necessity; they significantly impact patient outcomes. As healthcare experts remind us, 'Ninety-five percent of securing suitable reimbursement is simply effective record-keeping that most clinicians are aware of.' This underscores the importance of careful record-keeping. Insufficient records can lead to claims denials and reduced productivity, which no one wants to face. Moreover, efficient documentation methods such as clinical notes can lead to increased reimbursement rates and decreased legal liability, ultimately improving the quality of care delivered to individuals. By adhering to these crucial elements, healthcare providers can cultivate trust, enhance safety for individuals, and ensure compliance with evolving healthcare standards.
Have you considered how these practices can transform your approach to patient care? Embracing thorough documentation not only supports your professional responsibilities but also nurtures the relationships you build with your patients. Let's work together to foster a healthcare environment where every detail matters.
Implement Strategies for Efficient Note-Taking
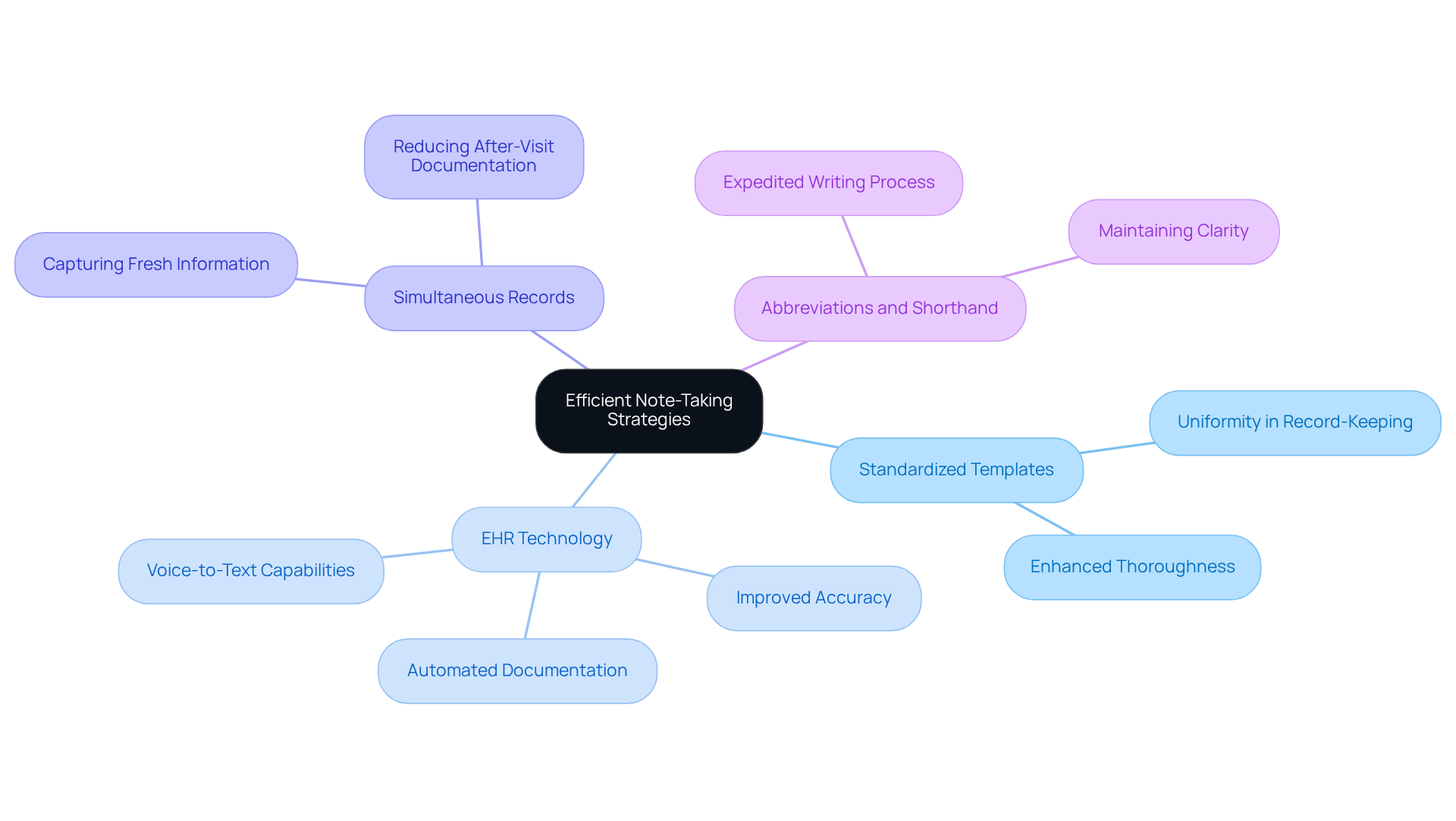
To enhance your note-taking efficiency and alleviate some of the burdens you face, consider implementing the following strategies:
- Utilize Standardized Templates: Developing and using standardized templates tailored for various types of patient visits can simplify your record-keeping process. This approach not only ensures uniformity but also enhances thoroughness in your clinical notes.
- Utilize EHR Technology: Embrace electronic health record (EHR) systems equipped with voice-to-text capabilities or automated documentation generation features. These tools can significantly decrease the time you spend on record-keeping while improving accuracy, allowing you to focus more on patient care.
- Practice Simultaneous Records: Engage in simultaneous records by jotting down observations during patient interactions. This method enables you to capture information while it is fresh, reducing the need for extensive after-visit records and enhancing the quality of your clinical notes.
- Incorporate Abbreviations and Shorthand: Consider creating a list of commonly used abbreviations and shorthand notations to expedite your writing process. This strategy can help maintain clarity while speeding up your record-keeping efforts.
By adopting these strategies, you can significantly reduce the time dedicated to clinical notes. This not only allows for more meaningful interactions with individuals but also improves overall efficiency in your practice, ultimately benefiting both you and your patients.
Understand Legal and Ethical Considerations
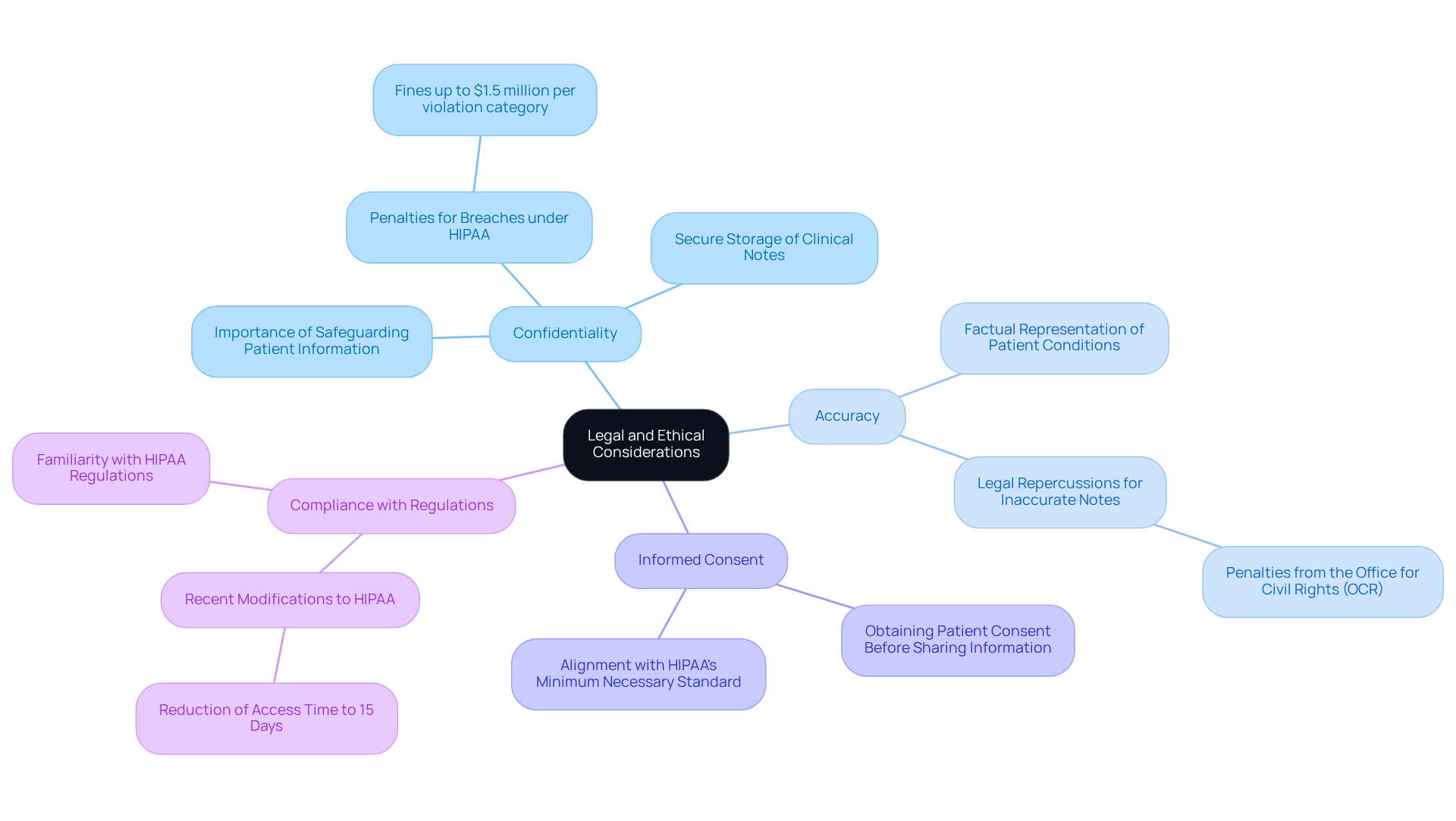
When documenting clinical notes, it’s essential to consider important legal and ethical principles that can significantly impact your practice and the well-being of your patients.
-
Confidentiality: Safeguarding patient information is paramount. How secure are your notes? Ensuring that all clinical notes are stored securely helps prevent unauthorized access, as breaches can lead to serious penalties under HIPAA, with fines reaching up to $1.5 million per violation category annually.
-
Accuracy: Are your entries truly reflective of your patients' conditions? All clinical notes must be factual and accurately represent the individual's treatment. Inaccurate clinical notes can lead to legal repercussions, including penalties from the Office for Civil Rights (OCR), which has imposed over 50 penalties under the HIPAA Right of Access enforcement initiative.
-
Informed Consent: Have you obtained consent from your patients before sharing their information? Always acquire consent before sharing information with third parties. This practice not only honors individual autonomy but also aligns with HIPAA's minimum necessary standard, which requires that only essential information is shared.
-
Compliance with Regulations: Are you familiar with the latest HIPAA regulations? Understanding HIPAA and other relevant laws is crucial for maintaining accurate clinical notes. Recent modifications stress compliance, with a suggested rule change reducing the time to grant access to protected health information (PHI) from 30 days to just 15 days, emphasizing the need for prompt and precise clinical notes.
By adhering to these principles, healthcare providers can uphold ethical standards in their documentation practices. This commitment not only ensures patient confidentiality but also reinforces compliance with legal requirements, fostering a trusting relationship with those in your care.
Conclusion
Selecting the right framework for clinical notes is a crucial step for healthcare providers striving to enhance their documentation practices. Have you ever felt overwhelmed by the demands of note-taking? By understanding and utilizing structured approaches such as SOAP, SBAR, or Narrative Notes, professionals can streamline their processes, ultimately improving the quality of care delivered to patients. This choice of framework not only influences the clarity and efficiency of clinical documentation but also significantly impacts communication among healthcare teams and patient outcomes.
Key components of effective clinical notes—ranging from patient identification to assessment and plan—are essential for comprehensive care. These elements help ensure that healthcare providers maintain accurate records, which are vital for regulatory compliance and optimal patient management. Imagine how implementing strategies like standardized templates and EHR technology can reduce the time spent on documentation, allowing for more meaningful patient interactions.
Ultimately, the significance of clinical notes extends beyond mere record-keeping; they are foundational to building trust and ensuring safety in healthcare. By prioritizing meticulous documentation practices and adhering to legal and ethical standards, healthcare providers can foster a more accountable and patient-centered environment. Embracing these principles not only enhances professional responsibilities but also strengthens relationships with those in care, leading to improved health outcomes and a more efficient healthcare system. Together, we can create a supportive atmosphere that values both care and clarity.




