Overview
This article provides a compassionate guide to writing BIRP notes, recognizing their vital role in behavioral health documentation. Have you ever felt overwhelmed by the administrative tasks that can distract from patient care? Structured BIRP notes—detailing Behavior, Intervention, Response, and Plan—are crucial for effective communication among healthcare providers. They enhance patient care by ensuring accurate record-keeping and informed treatment decisions.
By adopting structured BIRP notes, healthcare providers can alleviate some of the administrative burdens that often impede quality care. Imagine how streamlined documentation can lead to more time spent with patients, fostering stronger relationships and better outcomes. These notes not only serve as a communication tool but also empower providers to make informed decisions about patient treatment.
Ultimately, embracing the practice of writing BIRP notes can transform the way you approach documentation. It is a step towards enhancing your practice and supporting your patients more effectively. So, why not take the initiative today? Start incorporating BIRP notes into your routine and experience the benefits firsthand.
Introduction
Structured BIRP notes are more than just a formality in behavioral health; they serve as the cornerstone of effective client care. Every interaction deserves meticulous documentation and understanding. This guide invites you to explore the intricacies of BIRP note writing, offering a chance to enhance your documentation skills and, ultimately, improve patient outcomes. Yet, amidst the complexities of client interactions and the nuances of therapeutic techniques, how can you ensure your notes are both comprehensive and clear? It is essential to avoid common pitfalls that could compromise care.
As healthcare providers, you often face emotional challenges that can feel overwhelming. The administrative burdens can sometimes overshadow the core of patient care. However, by mastering the art of BIRP note writing, you can alleviate some of these pressures. Imagine the difference it could make in your practice and your patients’ lives.
Reflecting on your experiences, consider how improved documentation can lead to better communication and understanding in your therapeutic relationships. This guide is here to support you in navigating these challenges, providing you with the tools you need to succeed. Together, we can enhance the quality of care you provide.
Understand BIRP Notes: Definition and Purpose
Structured birp notes serve as a vital lifeline in behavioral health environments, designed to compassionately document client interactions and treatment plans. They represent a systematic approach encapsulated in the birp note, which stands for Behavior, Intervention, Response, and Plan. Each component plays a crucial role: capturing observable actions, detailing the interventions provided, recording the patient’s reactions, and outlining future treatment strategies. This structured method not only ensures accurate record-keeping but also enhances communication among healthcare providers using birp notes, fostering continuity of services and adherence to treatment protocols—especially in fragmented healthcare systems.
But why are progress records so essential? They go beyond mere documentation; birp notes are essential for clinicians striving to maintain a focus on the therapeutic process. By thoughtfully documenting all relevant aspects of individual management—such as discussions about treatment options, risks, and consent—these birp notes significantly enhance health outcomes and facilitate efficient treatment planning. Moreover, organized documentation, like birp notes, has been shown to elevate the quality of clinical files, leading to clearer and more concise entries that ultimately support better decision-making in healthcare.
In light of regulatory challenges like HIPAA, which can create barriers in communication between individuals and providers, the use of birp notes becomes indispensable. They help bridge communication gaps, addressing risks to patient safety and ensuring continuity of care amidst the complexities of fragmented healthcare systems. As Natalia Tague insightfully notes, 'With a structured birp note, you're conveying more of your understanding of their reaction,' which underscores the importance of capturing not just actions but also the nuanced dynamics of client interactions. Furthermore, common pitfalls in clinical records—such as overgeneralizing client behaviors or neglecting informed consent documentation—highlight the critical need for meticulous attention to detail in the birp note, which is an essential aspect of clinical practice.
In conclusion, let us embrace the power of structured notes. They are not just tools but essential resources that enhance our ability to provide compassionate care. How can we improve our documentation practices to better support our clients? Reflecting on this question can guide us toward more effective and empathetic healthcare delivery.
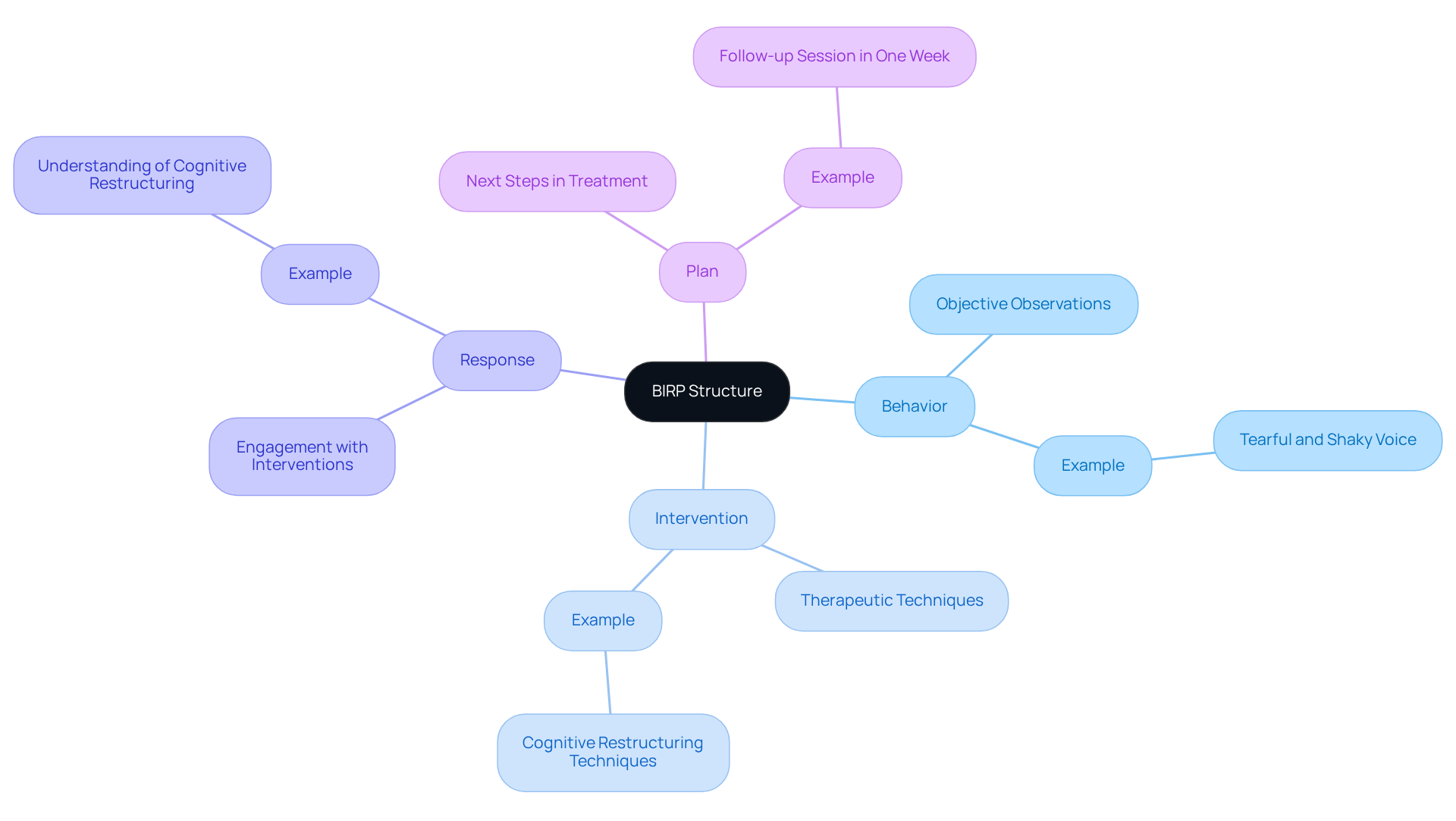
Break Down the BIRP Structure: Behavior, Intervention, Response, Plan
The BIRP note structure is composed of four essential components that support compassionate patient care:
-
Behavior: Observing the individual’s actions or statements during the session is crucial. This section should remain objective and specific, steering clear of subjective interpretations. For example, instead of saying 'the individual seemed upset,' a more precise observation would be 'the individual was tearful and spoke in a shaky voice.' Such clarity is vital for tracking client progress over time and understanding their emotional state.
-
Intervention: Here, the clinician documents the specific interventions or therapeutic techniques applied during the session. This could encompass cognitive-behavioral strategies, motivational interviewing, or other relevant approaches. For instance, 'The clinician utilized cognitive restructuring techniques to challenge the individual's negative thought patterns.' This documentation aids in understanding the therapeutic process and fosters a sense of support for the individual.
-
Response: This section captures how the individual engaged with the interventions. It’s important to note whether their engagement was positive or negative. An example might be, 'The individual expressed understanding of the cognitive restructuring process and reported feeling less anxious.' Documenting these responses not only evaluates the effectiveness of the interventions but also acknowledges the individual’s journey. Incorporating direct quotes from clients can enhance understanding and provide deeper insights into their emotional states.
-
Plan: The final section outlines the next steps in the treatment process. This may include follow-up appointments, additional interventions, or referrals to other services. For example, 'The individual will return for a follow-up session in one week to continue exploring cognitive restructuring techniques.' This ensures consistency of support and establishes clear expectations for the individual, fostering a nurturing environment.
Documentation should ideally be finalized within 24-48 hours of the session to ensure precision and should vary from 100-300 words, depending on the session's complexity. By mastering each element of this documentation framework, clinicians can create thorough and impactful BIRP notes that significantly enhance patient care. Well-structured clinical documentation serves as valuable references for monitoring client progress and improving practice effectiveness, and can be tailored to different therapeutic environments.
Write Effective BIRP Notes: Step-by-Step Instructions
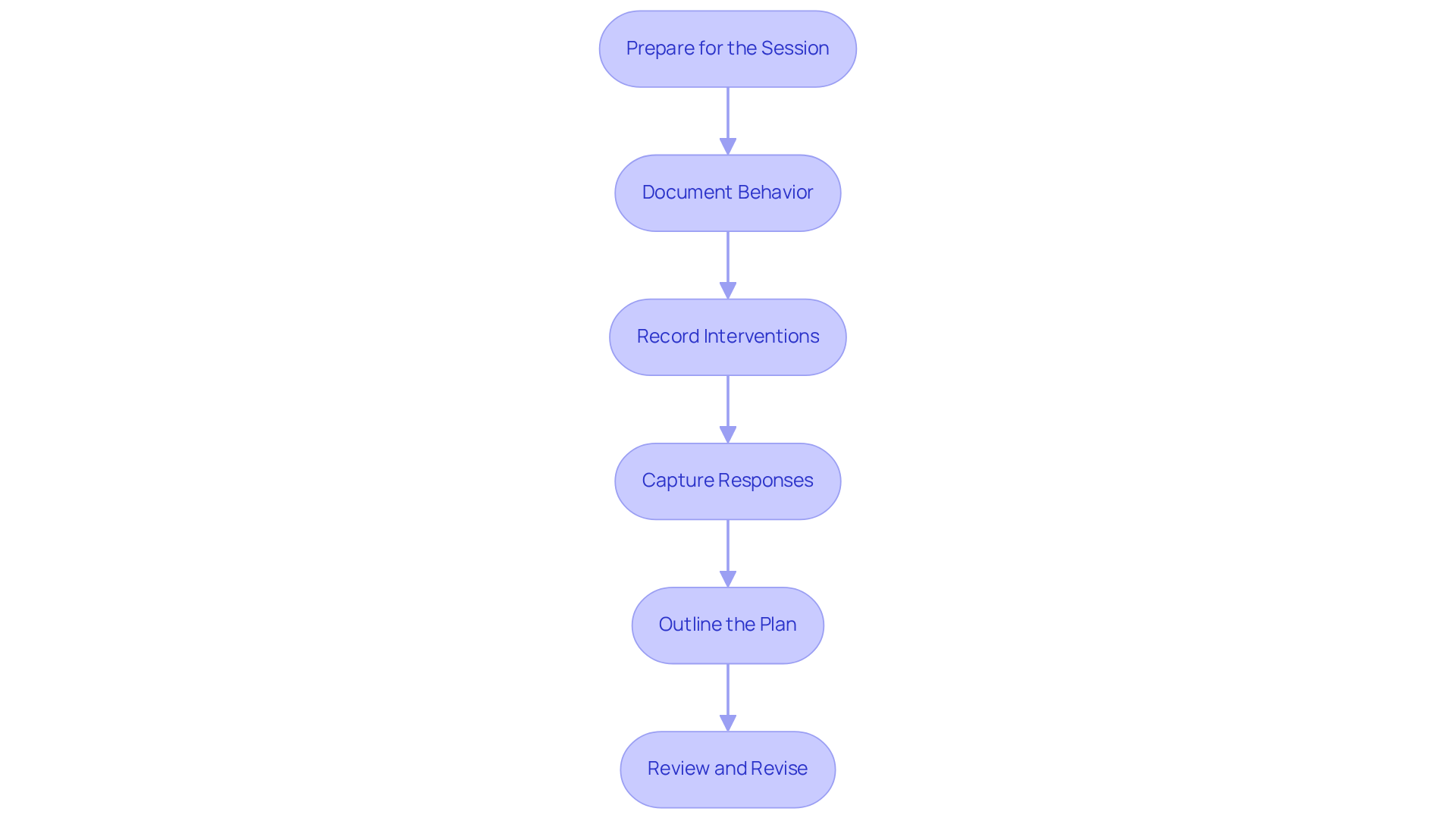
To write effective birp note, it's essential to approach the task with care and intention. Here’s a step-by-step guide to help you navigate this important process:
-
Prepare for the Session: Before meeting with the individual, take a moment to review any earlier records and treatment strategies. This preparation fosters continuity of care and can significantly enhance outcomes and satisfaction for those you serve. Have you considered how being well-prepared can transform your sessions?
-
Document Behavior: During the session, focus on taking detailed notes about the individual's observable behaviors. Use clear and objective language. For instance, you might note, 'The individual arrived punctually and seemed well-groomed but conveyed frustration about their current circumstances.' This precise documentation, particularly the birp note, is crucial for understanding the individual’s progress and challenges.
-
Record Interventions: After documenting behavior, it’s important to note the interventions you applied. Be specific about the techniques used and the rationale behind them. For example, 'The clinician introduced mindfulness exercises to help the individual manage anxiety.' This clarity aids in evaluating the effectiveness of interventions over time.
-
Capture Responses: Pay close attention to how the individual reacts to the interventions. Document both verbal and non-verbal cues. An example could be, 'The individual reported feeling calmer after the mindfulness exercise and was able to articulate their feelings more clearly.' Capturing these responses is vital for assessing progress and adjusting treatment plans accordingly.
-
Outline the Plan: Finally, summarize the next steps in the treatment process. Include any follow-up appointments or additional interventions. For instance, 'The individual will practice mindfulness techniques daily and return for a follow-up session in two weeks to assess progress.' A well-defined plan ensures that both you and the individual are aligned on treatment goals.
-
Review and Revise: After the session, take the time to examine your records for clarity and completeness. Ensure that all sections of the birp note are completed accurately and concisely. This final step is crucial, as thorough documentation can greatly reduce the risk of errors and enhance the overall quality of care.
Including direct quotations from individuals can further enrich these records, providing deeper insights into their experiences and nurturing a stronger therapeutic bond. For example, an individual might express, 'I feel a bit more relaxed now,' illustrating the effectiveness of the interventions used. Moreover, it’s important to recognize that these records can alleviate mental stress for professionals by maintaining a curated account of clients' clinical histories. By adhering to these procedures, clinicians can create effective documentation that enhances care for individuals and fosters communication among healthcare professionals.
Troubleshoot Common Issues in BIRP Note Writing
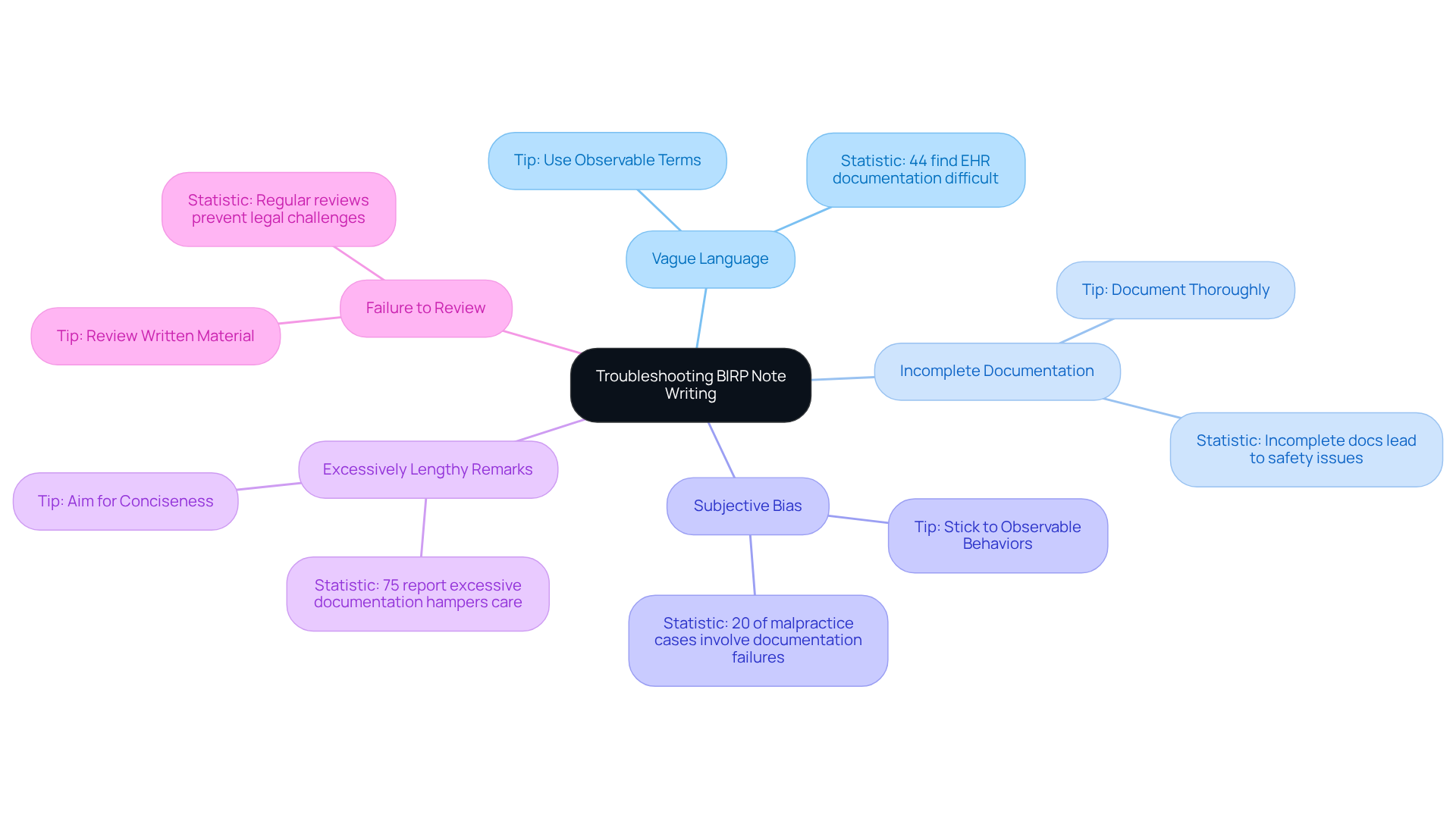
When writing a birp note, clinicians often face emotional challenges that can feel overwhelming. It’s important to recognize these hurdles and address them with compassion. Here are some supportive troubleshooting tips to help you navigate these common issues:
-
Vague Language: It’s easy to fall into the trap of ambiguous terms that may lead to misinterpretation. Instead of stating 'the individual appeared improved,' clarify what 'improved' means in observable terms, such as 'the individual reported a reduction in anxiety symptoms.' Statistics show that over 44% of healthcare professionals find it difficult to document patient treatment accurately in electronic health records (EHR), emphasizing the need for clarity in your notes.
-
Incomplete Documentation: Remember that thorough documentation is key to continuity of care. Make sure that the birp note is filled out completely in all sections. For instance, if an intervention was applied, document it thoroughly, including the individual's response. Incomplete documentation can lead to decreased safety of individuals and inadequate reimbursement for services, which can add to your stress.
-
Subjective Bias: Striving for objectivity in your observations is crucial. Avoid inserting personal opinions or assumptions about the individual's feelings. Stick to observable behaviors and factual statements. Documentation errors, particularly in high-risk specialties, can significantly impact legal outcomes, with 20% of malpractice cases involving documentation failures. Keeping your observations factual can help safeguard your practice.
-
Excessively Lengthy Remarks: While detail is important, excessively lengthy remarks can obscure key information. Aim for conciseness while ensuring that all relevant details are included. Nearly 75% of healthcare professionals report that excessive documentation hampers patient care, emphasizing the need for efficiency. Consider using bullet points to enhance readability and maintain focus on essential information.
-
Failure to Review: Always take a moment to examine your written material after composing it. This helps catch any errors or omissions and ensures that the documentation is clear and accurate. Consider having a colleague review your records for additional feedback. Regular reviews can prevent documentation errors that may lead to legal challenges, such as missing or incorrect signatures.
By being aware of these common issues and implementing these supportive troubleshooting tips, you can enhance the quality of your birp note. This ultimately enhances patient care and reduces the risk of documentation-related legal issues, allowing you to focus on what truly matters—caring for your patients.
Conclusion
Mastering the art of BIRP note writing is essential for providing effective and compassionate care in behavioral health settings. These structured notes serve not only as documentation but also as a vital communication tool that enhances the therapeutic process and supports continuity of care. By focusing on the components of Behavior, Intervention, Response, and Plan, clinicians can create comprehensive records that reflect the nuances of client interactions and treatment strategies.
Throughout the article, we explored key insights, including:
- The importance of objective observations
- The need for clarity in documenting interventions
- The significance of capturing client responses
Each step in the BIRP note writing process—from preparation to review—was outlined to ensure that clinicians can navigate this critical task with confidence and precision. Addressing common pitfalls such as vague language and incomplete documentation further emphasizes the necessity for meticulous attention to detail in clinical practice.
Reflecting on the significance of BIRP notes, it becomes clear that effective documentation is a cornerstone of quality patient care. By embracing these best practices, clinicians can not only improve their documentation skills but also enhance the overall therapeutic experience for their clients. A commitment to mastering BIRP notes ultimately translates into better health outcomes and a more empathetic approach to mental health care.
How can each clinician take these insights and apply them to elevate their practice? The answer lies in continuous reflection and a dedication to compassionate care.




