Overview
This article serves as a compassionate guide for healthcare providers navigating the complexities of writing SOAP notes in speech therapy. It recognizes the emotional challenges you may face and emphasizes the importance of a structured format—Subjective, Objective, Assessment, and Plan—as a vital tool for effective documentation. By detailing each component's purpose, the article not only provides clarity but also offers practical examples that resonate with your experiences.
Moreover, it highlights best practices that enhance communication among healthcare providers, ultimately leading to improved patient outcomes. Imagine the difference this structured approach can make in your daily interactions and the care you provide. As you explore these insights, consider how they may alleviate some of the administrative burdens that can impact patient care.
We encourage you to engage further with these strategies, reflecting on how they can transform your documentation process. Together, we can foster a more supportive environment for both providers and patients, ensuring that every note you write contributes positively to the care journey.
Introduction
Structured documentation is a cornerstone of effective healthcare, especially in fields like speech therapy where nuanced patient interactions are vital. The SOAP note framework—comprising Subjective, Objective, Assessment, and Plan—provides a systematic approach to capturing essential information. This enhances both communication and continuity of care, fostering a deeper connection with patients.
Yet, as the demands of clinical practice evolve, many practitioners may find themselves asking: how can traditional SOAP notes adapt to meet the dynamic needs of today's therapy environments? This guide explores the intricacies of writing SOAP notes in speech therapy. It offers insights and practical examples designed to elevate documentation standards and improve patient outcomes, ultimately supporting you in your vital role in patient care.
Understand the SOAP Note Framework
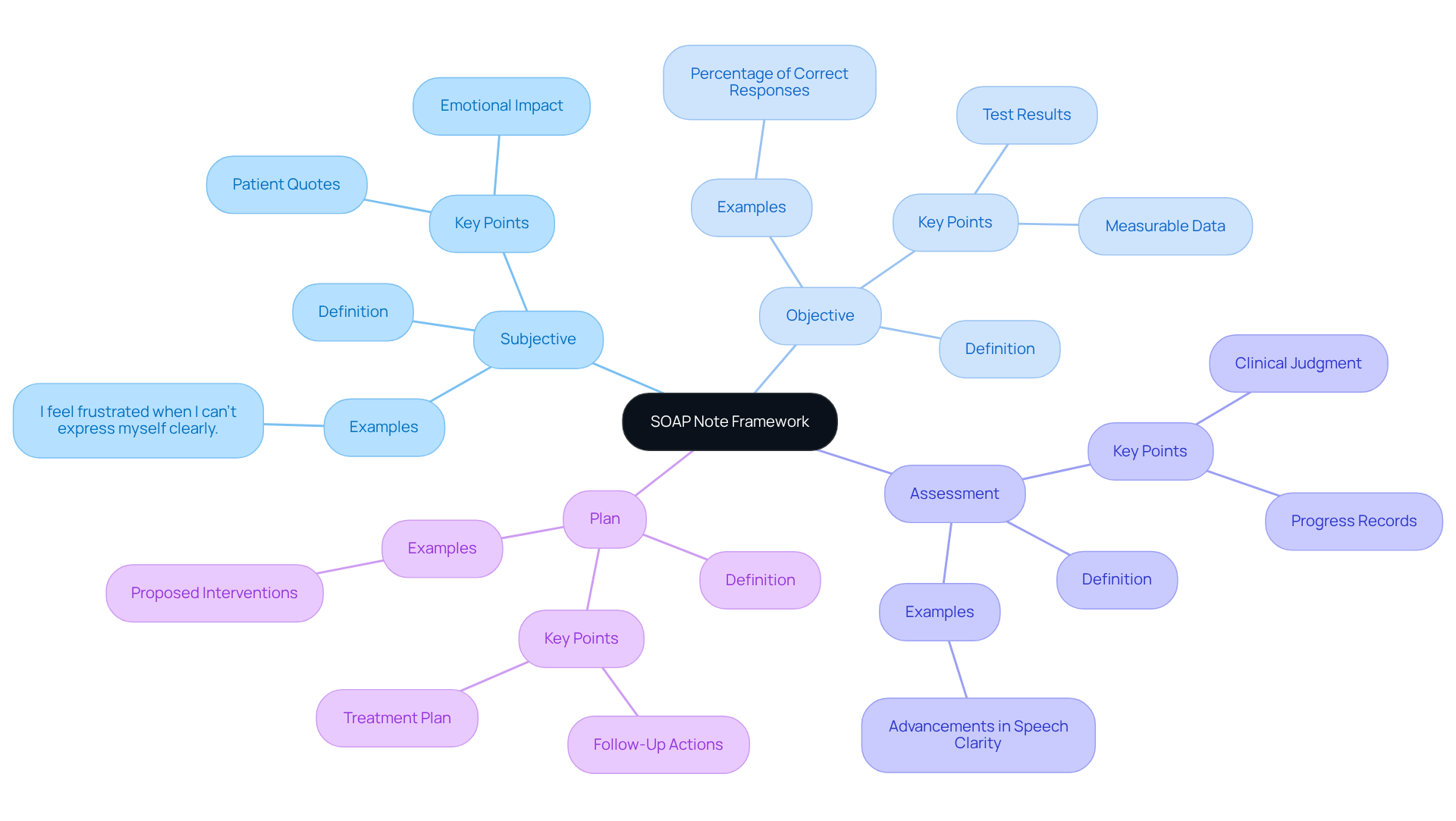
Structured notes provide a compassionate approach to documentation, serving as a vital tool for healthcare providers, including speech therapists, on to systematically log client interactions and treatment strategies. The acronym —highlights the importance of each section:
- Subjective: This section captures the patient's personal experiences and feelings regarding their condition. It often includes direct quotes, providing valuable insight into their perspective. For example, a speech therapist might note, "I feel frustrated when I can't express myself clearly," which underscores the emotional impact of their condition.
- Objective: Here, clinicians document measurable data, such as test results and physical examinations. This could include metrics like the percentage of correct responses during therapy sessions, offering a clear picture of progress.
- Assessment: This section combines subjective and objective information to provide a clinical judgment about the individual's status. It may encompass diagnoses or progress records, such as advancements in speech clarity or areas needing further intervention.
- Plan: The final section outlines the proposed treatment plan, detailing interventions and follow-up actions. This clarity fosters a collaborative approach to care, ensuring both the clinician and the individual are aligned on next steps.
The significance of cannot be overstated. They enhance communication among providers, ensuring and improving outcomes. Studies indicate that about 75% of healthcare workers utilize structured formats for recording information, showcasing their acceptance and efficiency. In speech therapy, learning how to write a soap note speech therapy aids in and enhances , ultimately leading to improved therapeutic results.
However, it is essential to recognize the limitations of traditional formats, which may not fully address the evolving needs of healthcare records. The OODA model (Observe, Orient, Decide, Act) offers an alternative framework that emphasizes situational awareness and iterative learning in clinical environments. Integrating succinct documentation methods is also crucial, as written records should ideally consist of one brief paragraph per section to maintain clarity and focus.
Experts in the field acknowledge the from practical viewpoints. As one speech therapist noted, "Such records not only assist in tracking progress but also act as a communication resource among interdisciplinary teams, ensuring all are aligned regarding patient care." This highlights the cooperative nature of .
Ultimately, is vital for enhancing communication and ensuring continuity of care in speech therapy. It is equally important to consider the potential advantages of alternative models like OODA, fostering a nurturing environment for both providers and patients.
Detail the Components: Subjective, Objective, Assessment, and Plan
Understanding is essential, as each component of the SOAP note plays a crucial role in for both providers and patients.
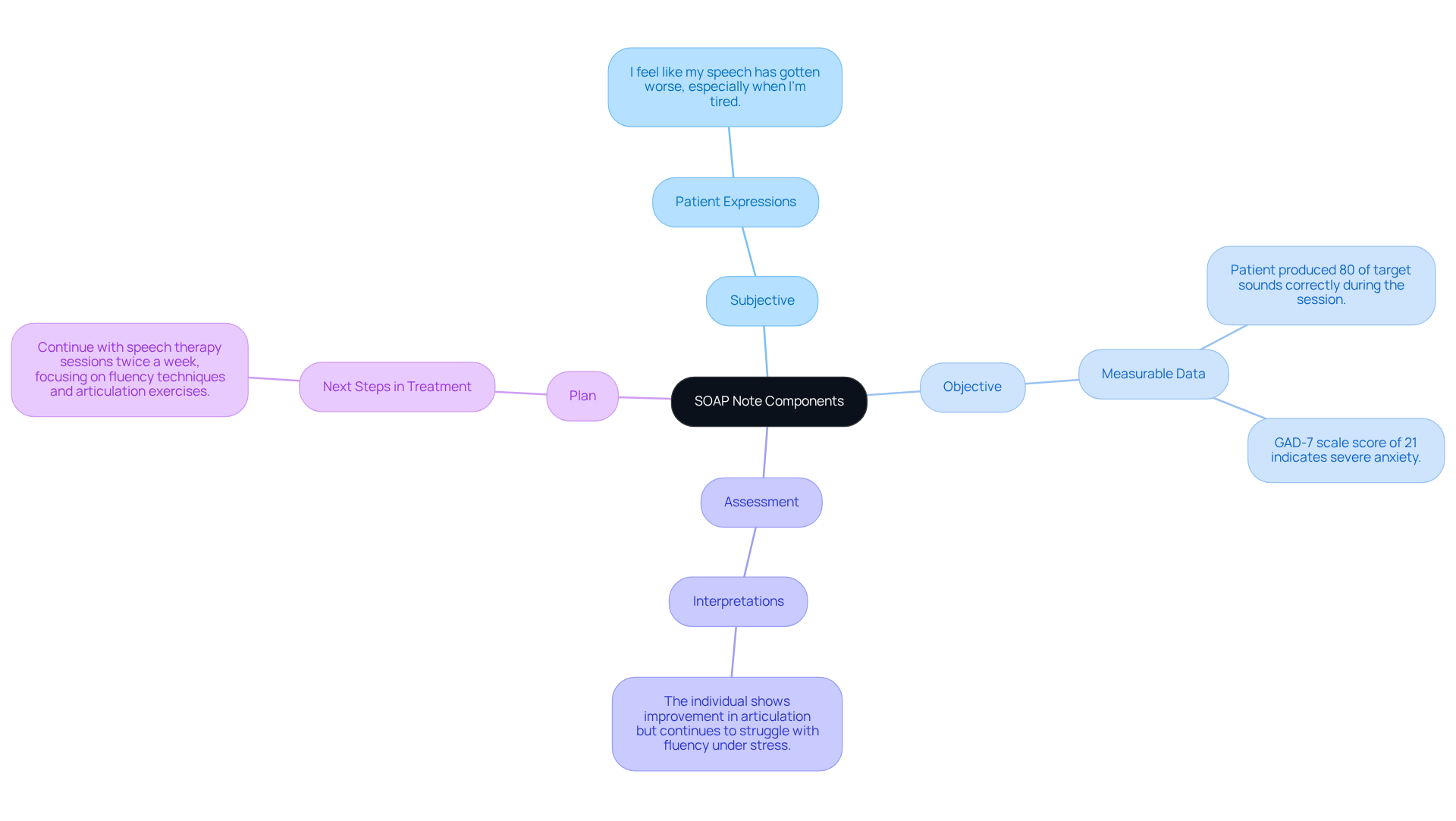
- Subjective: This section should include the patient's own words about their condition. For instance, an individual might express, "I feel like my speech has gotten worse, especially when I’m tired." This offers context and understanding of the individual's experience, allowing to connect with their feelings.
- Objective: Document or observations made during therapy. For example, "Patient produced 80% of target sounds correctly during the session." Additionally, evaluations like the Generalized Anxiety Disorder 7 (GAD-7) scale can be recorded, with a score of 21 indicating severe anxiety. This information is vital for comprehending the individual's condition and tailoring care appropriately.
- Assessment: Here, you interpret the subjective and objective data. An example might be, "The individual shows improvement in articulation but continues to struggle with fluency under stress." This assessment helps in understanding the patient's journey.
- Plan: Outline the next steps in treatment. For example, "Continue with twice a week, focusing on fluency techniques and ." This clear plan can provide reassurance to both the patient and the provider.
By describing each element, professionals can ensure their documentation on how to write a soap note speech therapy is thorough and beneficial for the continuous care of individuals. It is also crucial to follow HIPAA standards when recording clinical observations to safeguard individual information. The , has become a standard in . With over 225,000 clinicians nationwide utilizing platforms like SimplePractice for practice management, the significance of for individuals cannot be overstated.
Reflect on how these components can enhance your practice and the care you provide. Together, we can foster a nurturing environment that prioritizes the well-being of every individual.
Explore Practical Examples of SOAP Notes in Speech Therapy
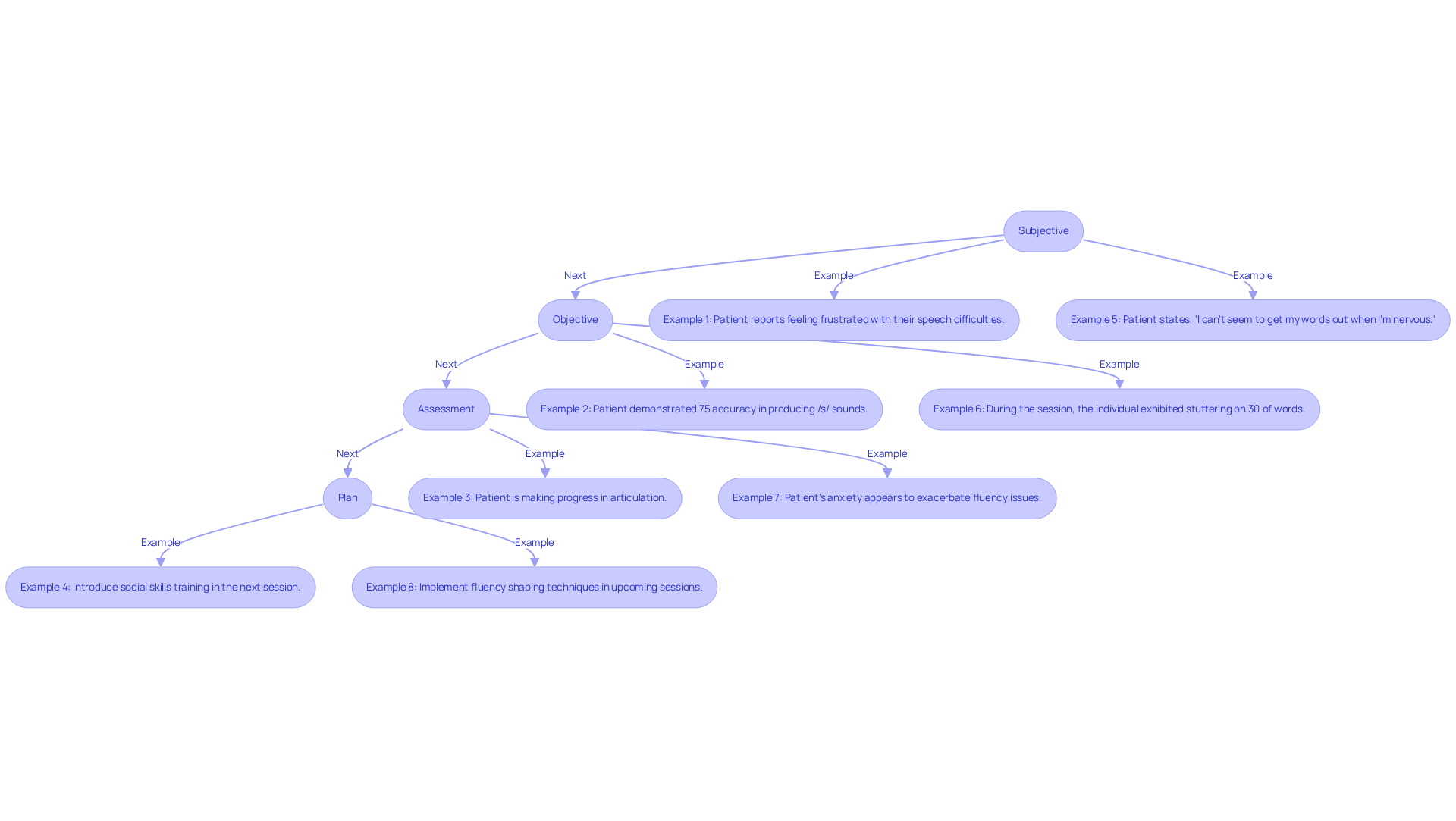
In speech therapy, is crucial, and practical examples of into this process:
-
Example 1:
- Subjective: "Patient reports feeling frustrated with their , especially in social situations."
- Objective: "Patient demonstrated 75% accuracy in producing /s/ sounds during structured tasks."
- Assessment: "Patient is making progress in articulation but requires additional support in social communication contexts."
- Plan: "Introduce social skills training in the next session to address communication in social settings."
-
Example 2:
- Subjective: "Patient states, 'I can’t seem to get my words out when I’m nervous.'"
- Objective: "During the session, the individual exhibited stuttering on 30% of words during spontaneous speech."
- Assessment: "Patient's anxiety appears to exacerbate fluency issues."
- Plan: " and relaxation strategies in upcoming sessions."
These examples illustrate , emphasizing the in capturing client interactions. With approximately 2.5 million individuals in the UK facing , and 30% of stroke survivors dealing with ongoing speech and language issues, is essential. , particularly how to write a soap note speech therapy, not only helps in adhering to healthcare regulations but also enhances communication among providers, ultimately leading to improved patient outcomes. As Piera Willner, MS, CCC-SLP, emphasizes, "Most importantly, SLPs must document medical necessity and skilled intervention."
Composing effective clinical documentation requires clarity, conciseness, and precision. This approach ensures that all pertinent information is captured for future reference, fostering a supportive environment for both patients and healthcare providers.
Implement Best Practices for Effective SOAP Note Writing
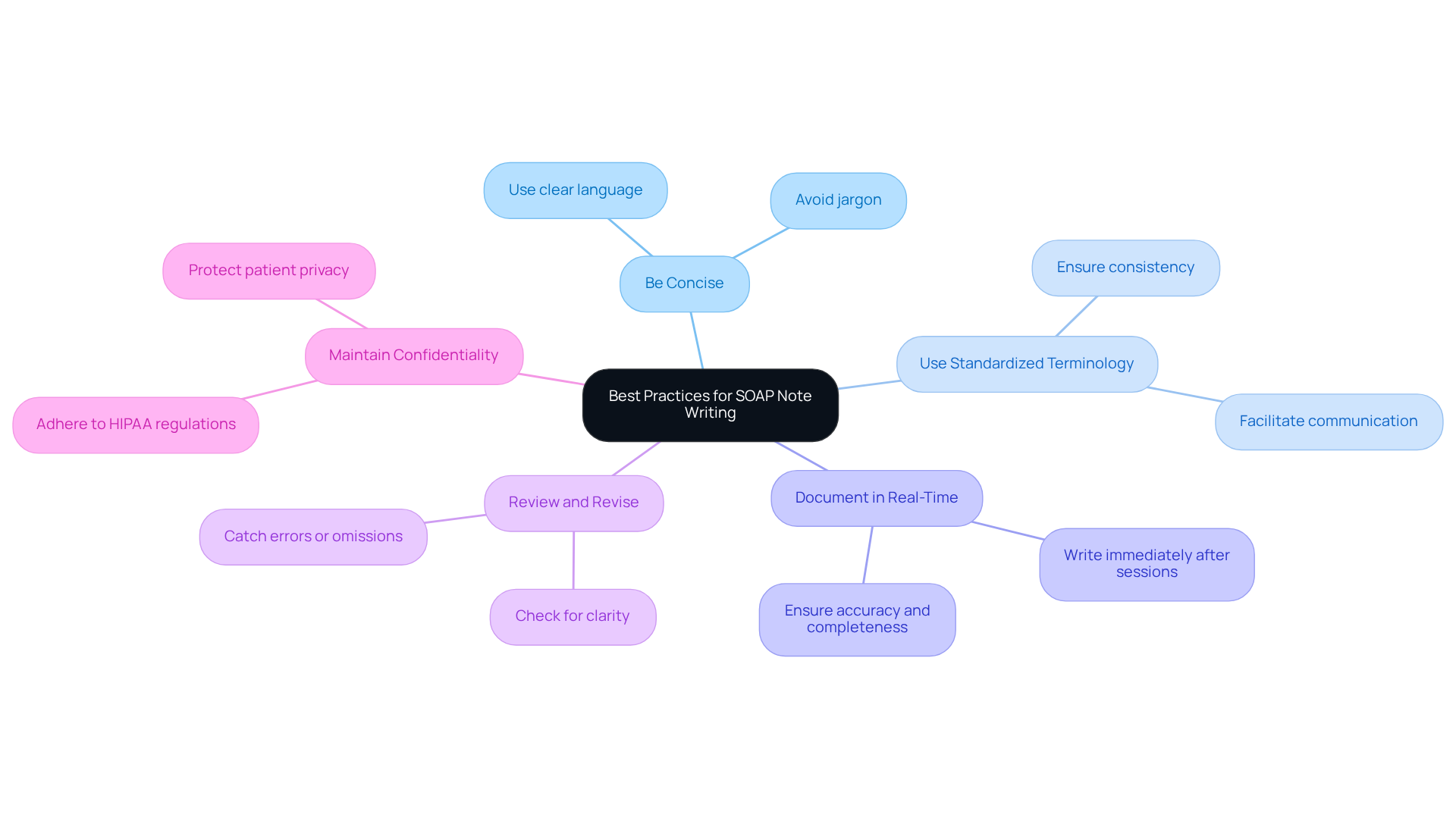
To write effective , it's essential to consider some that can make a significant difference in your documentation process:
- Be Concise: Use clear and straightforward language. This helps avoid unnecessary jargon that may confuse readers and ensures your message is understood.
- Use : Consistency in language aids in ensuring that all comprehend the documentation, facilitating better communication among the team.
- : Whenever possible, immediately after the session. This practice ensures accuracy and completeness of information, which is vital for quality care.
- Review and Revise: Take a moment to review your notes for clarity and completeness before finalizing them. This simple step can help catch any errors or omissions that might otherwise impact .
- Maintain Confidentiality: Always ensure that individual information is kept confidential and secure, adhering to to protect your patients' privacy.
By implementing these best practices, you can enhance how to write a soap note . This ultimately benefits not only your practice but also the care you provide to your patients, fostering better communication and understanding.
Conclusion
Writing a SOAP note in speech therapy is not just a task; it’s a vital part of ensuring effective clinical documentation and patient care. By embracing the structured framework of Subjective, Objective, Assessment, and Plan, speech therapists can create thorough records that enhance communication among healthcare providers and ensure continuity of care. This systematic approach not only tracks patient progress but also nurtures a collaborative environment where both clinicians and patients are united on treatment goals.
Each component of the SOAP note holds significant importance, and practical examples illustrate how to document client interactions effectively. Consider the impact of using concise language, standardized terminology, and real-time documentation. These practices maintain clarity and accuracy, essential for fostering trust and understanding in therapeutic relationships. Moreover, reviewing notes and safeguarding patient confidentiality are best practices that further elevate the quality of clinical records.
Ultimately, mastering the SOAP note writing process is essential for speech therapists who aspire to enhance patient outcomes and streamline communication within interdisciplinary teams. By prioritizing effective documentation, therapists create a supportive environment that champions the well-being of every individual they serve. Embracing this structured approach not only improves clinical practice but also reinforces the profound value of thorough and compassionate patient care in the field of speech therapy.




