Overview
This article highlights the essential steps that healthcare providers must take to write effective progress notes, recognizing the emotional challenges they face in their demanding roles. Clear and concise documentation is not just a task; it is a vital component of patient care and communication that significantly enhances patient safety and ensures continuity of treatment. However, we understand that time constraints and inconsistent formats can create obstacles.
To address these common challenges, we offer supportive strategies, such as utilizing templates and AI tools, which can significantly enhance both efficiency and clarity in record-keeping. By adopting these practices, healthcare providers can alleviate some of the administrative burdens that impact their ability to focus on patient care.
We invite you to reflect on your current documentation practices and consider how these solutions can make a difference in your daily routine. Embracing these strategies not only benefits your workflow but also fosters a safer and more effective environment for your patients. Together, let’s enhance the quality of care through thoughtful and compassionate documentation.
Introduction
Progress notes are vital to providing compassionate patient care, capturing crucial details about a patient's clinical condition and the treatments administered during each interaction. Writing these notes is more than just a routine task; it is a critical skill that fosters communication among healthcare providers. This ensures continuity of care and adherence to legal requirements. Yet, as documentation demands become more complex, healthcare professionals may feel overwhelmed. How can they navigate the challenges of clarity, efficiency, and accuracy in their records?
This article explores essential steps for crafting effective progress notes, addressing common hurdles, and unveiling innovative solutions that can simplify the documentation process while enhancing patient outcomes. Together, we can tackle these challenges and improve the quality of care provided to our patients.
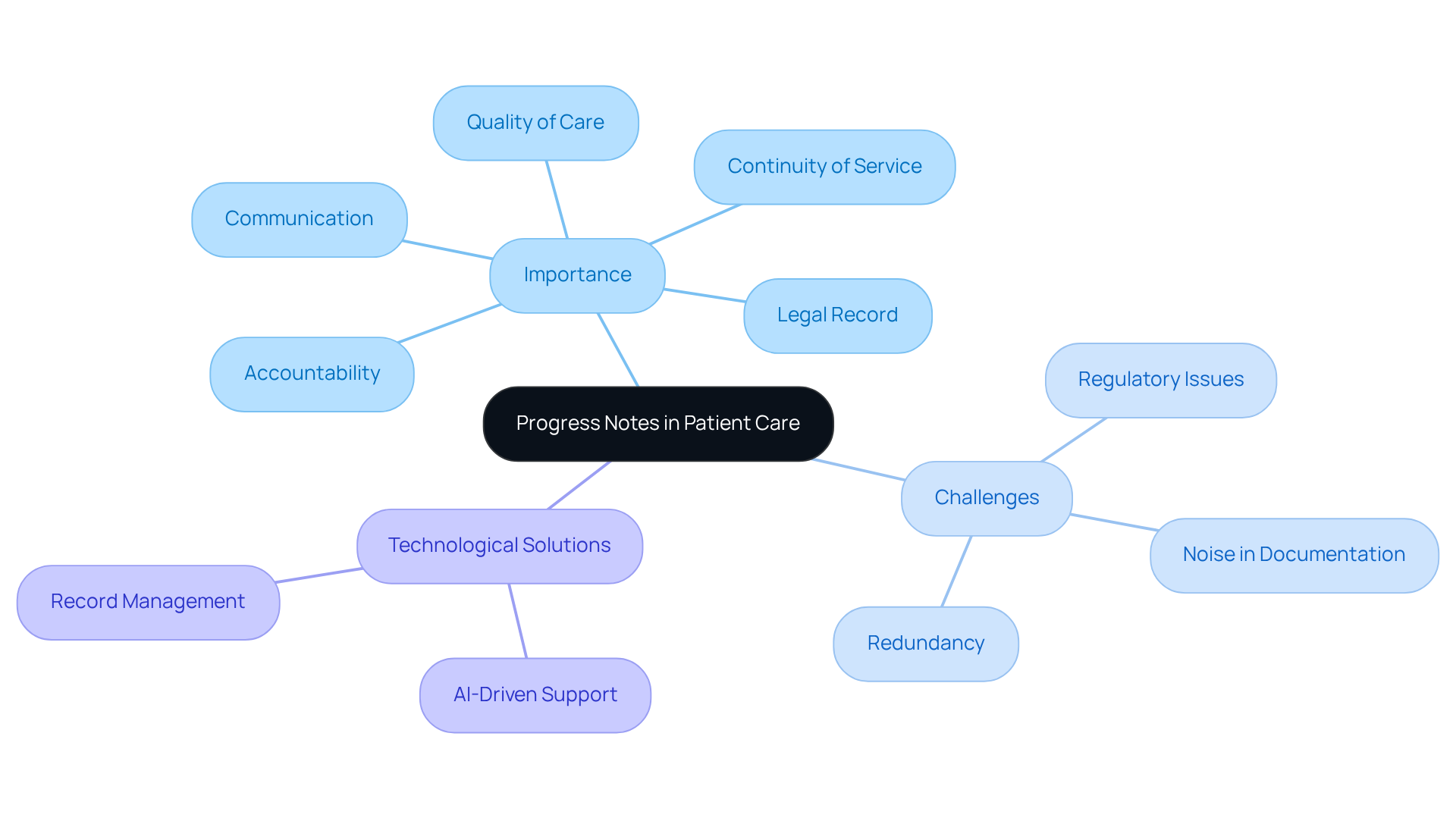
Define Progress Notes and Their Importance in Patient Care
Progress summaries are vital, brief documents that capture a person's clinical condition and the support provided during each interaction. Have you ever considered how these summaries facilitate communication among healthcare providers? They ensure continuity of service and serve as a legal record of treatment. The significance of understanding how to write a progress note in healthcare cannot be overstated; it is essential for monitoring individual progress, guiding future treatment decisions, and enhancing accountability.
Accurate and timely records not only improve patient safety and care quality but also align with ethical standards and best practices. Recent studies reveal that the median length of outpatient progress records increased by 60.1% from 2009 to 2018. This trend underscores a growing emphasis on comprehensive documentation. However, this increase has also led to a 10.9 percentage point rise in redundant information, highlighting the need for clarity and precision in writing.
The presence of 'noise' in progress records, such as abbreviations and acronyms, can obscure clarity and hinder effective communication. Consider this: understanding how to write a progress note efficiently can significantly enhance outcomes for individuals by ensuring that all healthcare providers are informed and aligned in their treatment approach. This ultimately fosters a more cohesive healthcare experience. As Julie Taitsman, Chief Medical Officer for the US Department of Health and Human Services, aptly states, "Effective records enhance safety and quality of service for individuals."
Moreover, the challenges posed by fragmented healthcare systems and regulatory issues like HIPAA can complicate record-keeping practices. Thankfully, AI-driven solutions, such as those offered by CosmaNeura, can support healthcare providers in improving their record management. By upholding high standards in record-keeping, these solutions enhance communication and coordination, leading to better care.
How can we work together to ensure that our documentation practices serve our patients effectively?
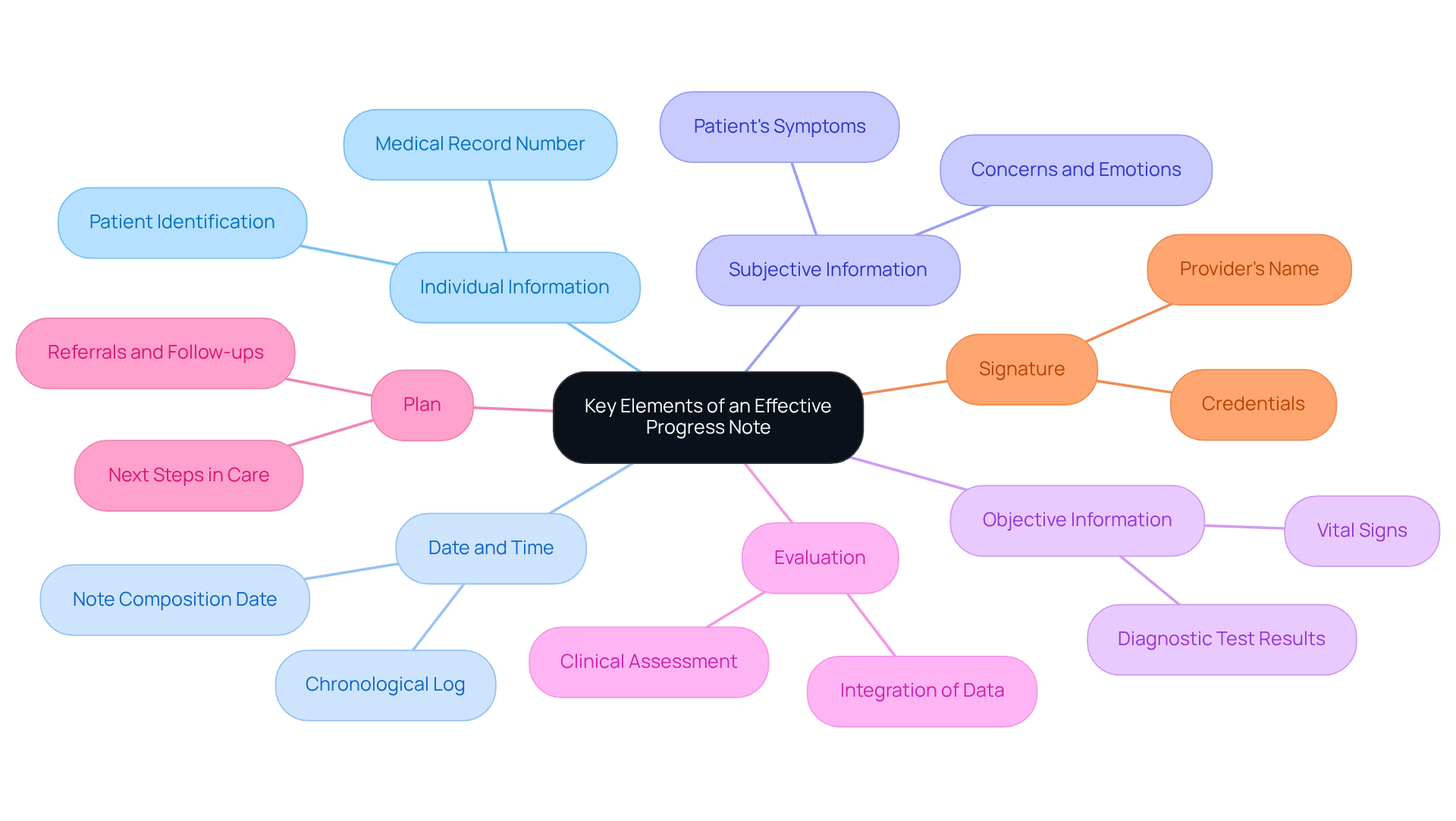
Identify Key Elements of an Effective Progress Note
Understanding how to write a progress note is vital for creating effective and comprehensive patient documentation, especially in a world increasingly shaped by generative AI. Healthcare providers often face emotional challenges due to administrative burdens that can detract from patient care. How can we ease this burden?
To begin, an effective progress note should encompass several key elements:
- Individual Information: Clearly state the individual's name, date of birth, and medical record number for accurate identification.
- Date and Time: Record when the note was composed as part of how to write a progress note, preserving a chronological log of medical attention.
- Subjective Information: Include the individual’s own expressions about their symptoms, concerns, and emotions regarding treatment, as this is crucial when considering how to write a progress note.
- Objective Information: Document measurable data such as vital signs and diagnostic test results, which is essential for clinical assessment and is an important aspect of how to write a progress note.
- Evaluation: Offer a clinical evaluation that includes guidance on how to write a progress note, integrating both subjective and objective information to assist in future treatment decisions.
- Plan: Outline how to write a progress note that details the next steps in the patient's care, including treatments, referrals, or follow-ups, ensuring a clear path forward.
- Signature: Including the provider's name and credentials to authenticate the document is essential when considering how to write a progress note, reinforcing accountability and professionalism.
Integrating generative AI into this documentation process can greatly enhance efficiency and effectiveness. In 2018, only 29.4% of outpatient progress documentation was directly typed, revealing a significant reliance on templated content. This highlights the importance of crafting personalized messages that reflect the unique aspects of each patient's treatment.
AI tools, such as natural language processing software, can automate repetitive tasks, allowing healthcare providers to focus on delivering personalized care. Consider this: the median length of outpatient progress records grew by 60.1% from 2009 to 2018, indicating increased complexity. It is crucial for healthcare professionals to prioritize clarity and brevity in their records to enhance communication and reduce redundancy. Lengthy and repetitive notes can obscure essential information, leading to potential diagnostic mistakes.
Moreover, over 77% of healthcare professionals feel they complete work later than preferred due to excessive record-keeping. This statistic underscores the impact of administrative burdens on providers. By embracing these essential elements and optimal methods, and utilizing AI tools, healthcare providers can significantly improve how to write a progress note. Together, we can enhance service delivery and foster a more compassionate healthcare environment.
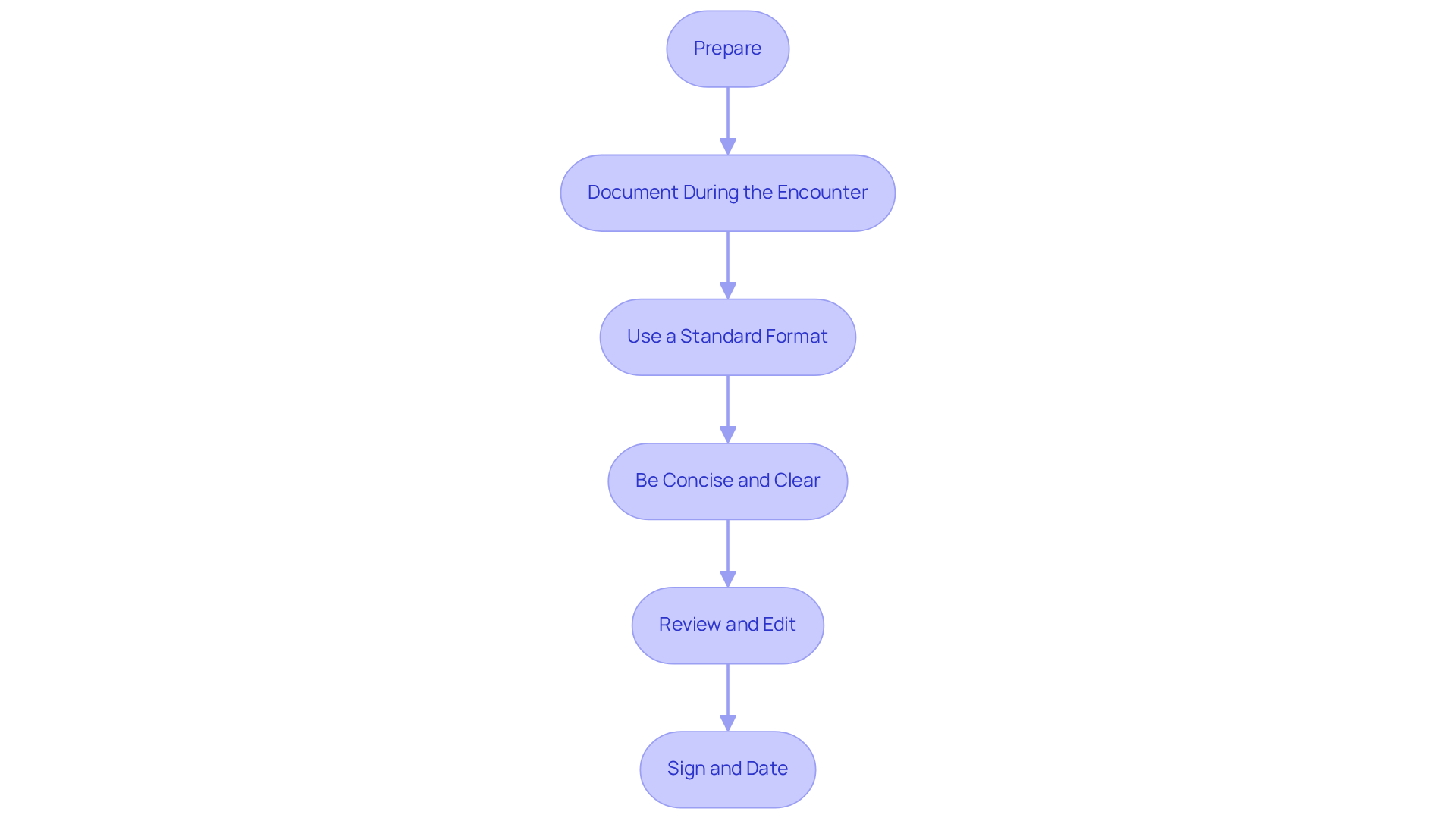
Follow a Step-by-Step Process to Write Progress Notes
Understanding how to write a progress note effectively can feel overwhelming, especially when balancing patient care with administrative tasks. However, by following these essential steps on how to write a progress note, you can ease this burden and enhance the quality of your documentation, ultimately benefiting your patients.
-
Prepare: Before your encounter, take a moment to review prior documentation and relevant medical history. This preparation not only guides your evaluation but also ensures continuity of care, which is vital for your patients’ well-being.
-
Document During the Encounter: Capture key points in real-time during the patient visit. This practice enhances accuracy and helps avoid the common pitfalls of relying solely on memory. How often have you left a session wishing you had written down more?
-
Use a Standard Format: Adopting a consistent structure—such as SOAP (Subjective, Objective, Assessment, Plan), DAP (Data, Assessment, Plan), or BIRP (Behavior, Intervention, Response, Plan)—can significantly organize your records. Research suggests that utilizing organized templates can greatly decrease paperwork time and enhance clarity, with studies demonstrating that optimizing physician record templates saved an average of 2.6 hours daily.
-
Be Concise and Clear: Utilize straightforward language and avoid jargon. This ensures that your observations are easily understood by other healthcare providers, fostering effective communication and continuity of care. Have you considered how clarity in your notes can impact patient outcomes?
-
Review and Edit: After the encounter, take the time to examine your records for completeness and clarity. Make necessary edits to ensure that all relevant information is accurately captured before finalizing the document. Remember, clinicians have a legal and ethical responsibility to document each treatment episode as part of the client’s official medical record.
-
Sign and Date: Always sign and date your notes to authenticate them. This maintains a legal record that complies with documentation standards and regulations, ensuring accountability.
By following these steps, you will understand how to write a progress note that improves the quality of your progress records. This not only serves as an effective tool for tracking patient advancement but also facilitates communication among care teams. As Innocent Turner observed, composing compliant messages can be challenging. Yet, by adhering to these best practices, you can streamline the process and focus more on what truly matters—your patients.
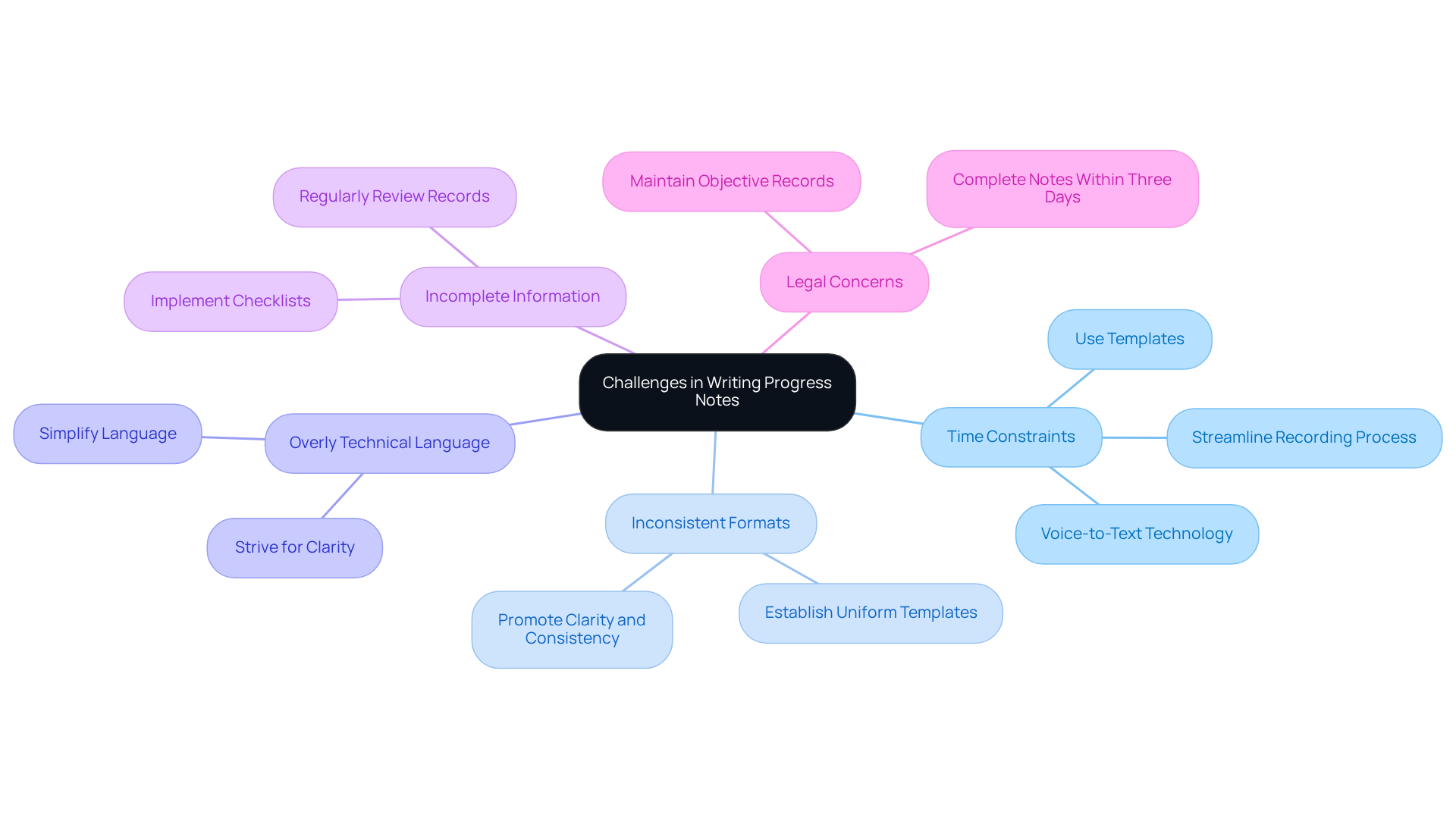
Address Common Challenges in Writing Progress Notes
Healthcare providers often face significant challenges regarding how to write a progress note. These obstacles can weigh heavily on their daily responsibilities, impacting not only their workflow but also patient care. Here, we explore some common hurdles and compassionate strategies to overcome them:
-
Time Constraints: Many providers feel a pressing urgency during patient interactions, often spending too much time on record-keeping. To alleviate this stress, consider using templates or voice-to-text technology. These tools can streamline the recording process, allowing for quicker and more effective note-taking. Research shows that clinicians can reclaim several hours each day that were previously consumed by routine administrative tasks, showcasing the potential for enhanced efficiency.
-
Inconsistent Formats: Variability in note-taking practices can create confusion among team members. By establishing a uniform template for all providers within a practice, you can ensure consistency and clarity in how to write a progress note. This promotes better communication and continuity of care, fostering a supportive environment.
-
Overly Technical Language: The use of medical jargon can create barriers to understanding among team members. Strive for clarity and simplicity in your language to ensure that all staff can grasp the messages being conveyed. This is crucial for effective collaboration and optimal patient care.
-
Incomplete Information: Missing essential elements in progress notes can diminish their effectiveness. Implementing a checklist or template can help guarantee that all necessary components are included when considering how to write a progress note. Regularly reviewing records for completeness can further enhance the quality of documentation.
-
Legal Concerns: Documentation carries significant legal implications. It's vital to maintain factual, objective records that are free from personal opinions to safeguard against liability. Ideally, completing notes within three days of the session can aid memory retention, as delays may challenge accuracy in legal contexts.
By addressing these prevalent challenges with thoughtful solutions, healthcare providers can significantly improve their documentation practices. This not only enhances patient care but also contributes to professional satisfaction. Let's work together to create a more supportive and efficient environment for all.
Conclusion
Understanding how to write a progress note is essential for healthcare providers who genuinely care about enhancing patient care and communication. These concise documents not only track a patient's clinical condition but also ensure that all healthcare professionals involved in a patient's treatment are informed and aligned. The importance of mastering this skill cannot be overstated, as it directly impacts the quality of care and accountability within healthcare systems.
Have you ever felt overwhelmed by the administrative burdens that come with documentation? This article has outlined the essential elements of an effective progress note, including the significance of clear and concise documentation and the role of technology, such as AI-driven solutions, in streamlining the record-keeping process. By following a structured approach and addressing common challenges, healthcare providers can significantly improve their documentation practices. Key strategies include:
- Adopting standardized formats
- Utilizing technology for efficiency
- Ensuring that notes are both comprehensive and easy to understand
Ultimately, the quality of progress notes reflects a deep commitment to patient safety and care. By prioritizing clarity, consistency, and thoroughness in documentation, healthcare providers not only enhance their own workflow but also contribute to better patient outcomes. Embracing these best practices is essential for fostering a collaborative and effective healthcare environment, where every interaction is documented with the utmost care and professionalism. How will you take the next step in improving your documentation practices today?




