Overview
The article titled "7 SOAP Report EMS Examples to Enhance Your Documentation Skills" addresses a crucial concern in healthcare: the emotional and administrative challenges faced by providers. It highlights how structured SOAP notes can alleviate these burdens, ultimately leading to improved documentation practices. By streamlining the documentation process, these examples foster better communication and enhance patient care.
Have you ever felt overwhelmed by the administrative tasks that take time away from patient interactions? This article emphasizes that utilizing SOAP notes not only simplifies documentation but also significantly reduces the administrative load. This allows healthcare providers to dedicate more time to what truly matters—their patients and the outcomes of care.
Imagine a world where you can focus more on patient interactions rather than paperwork. The benefits of adopting these structured notes are profound, as they not only improve efficiency but also enhance the quality of care provided. We encourage you to explore these examples and consider how they can transform your documentation practices.
In the journey of healthcare, it's essential to acknowledge the common challenges we face. By embracing structured SOAP notes, you can take a significant step towards improving both your documentation skills and your overall patient care experience. Let’s work together to create a more compassionate and efficient healthcare environment.
Introduction
In the intricate world of healthcare, effective documentation is not merely a bureaucratic necessity; it serves as a cornerstone of quality patient care. As providers navigate the demands of clinical responsibilities alongside administrative tasks, the emotional strain can be overwhelming. The need for streamlined documentation practices is becoming increasingly evident, as it directly impacts the care patients receive.
This article explores the transformative power of SOAP notes, presenting seven compelling examples that not only enhance documentation skills but also significantly improve patient outcomes. These practices can alleviate some of the burdens that providers face, fostering a more supportive environment for both healthcare professionals and their patients.
However, with the ever-evolving challenges in healthcare and the integration of new technologies, how can providers ensure that their documentation remains relevant and effective? By reflecting on these questions, we can begin to identify strategies that not only address the current landscape but also promote a nurturing approach to patient care.
CosmaNeura: Streamline SOAP Report Documentation with AI Assistance
Healthcare providers often grapple with overwhelming administrative tasks that detract from their primary mission: caring for patients. CosmaNeura's AI platform is here to alleviate that burden, streamlining the documentation process for medical reports. Imagine being able to focus more on client care rather than paperwork. By integrating AI assistance, providers can ensure that their SOAP report EMS example notes are not only accurate but also completed in a fraction of the time, significantly enhancing efficiency in clinical settings.
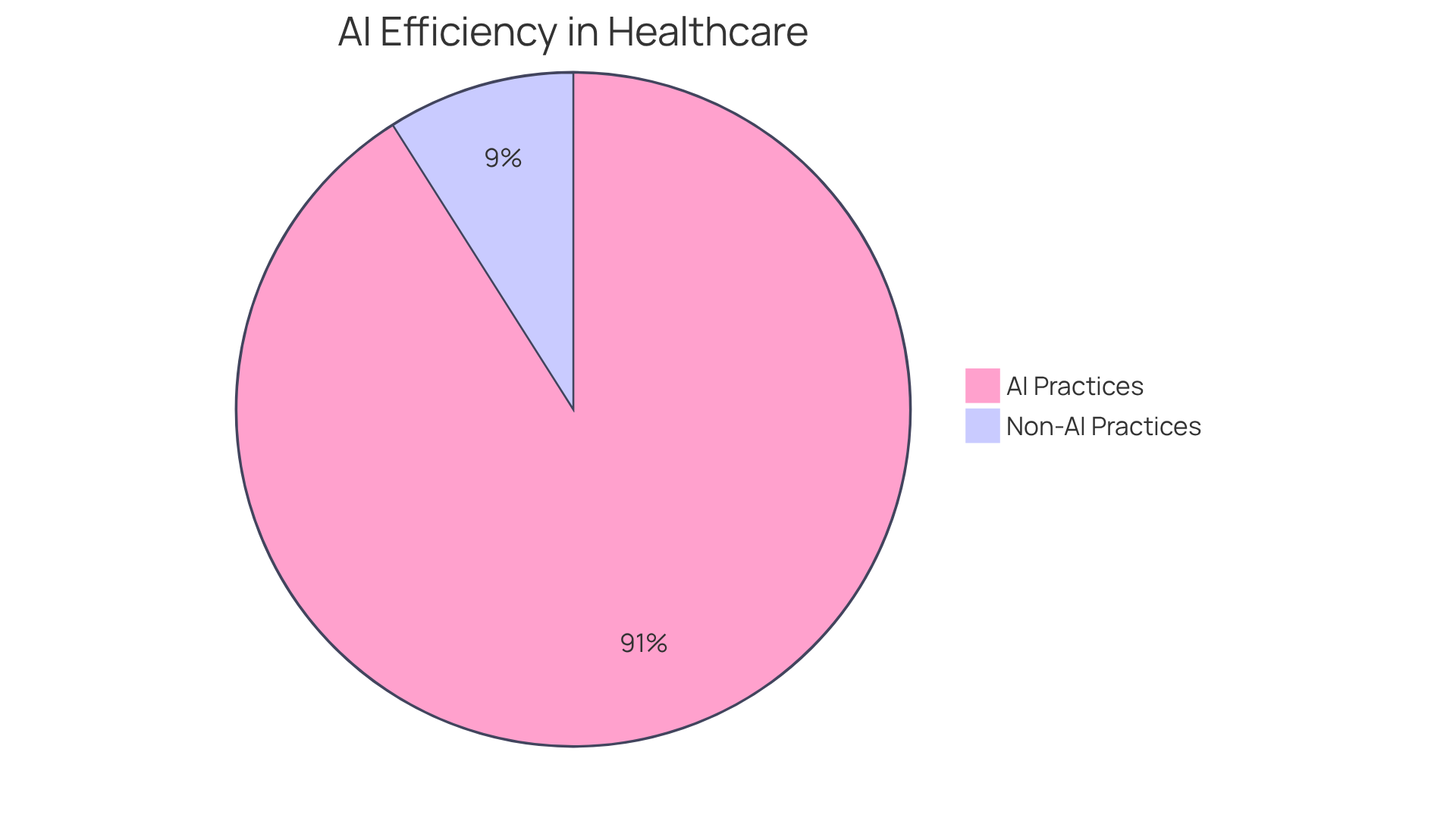
Consider this: practices utilizing AI have experienced a remarkable 91% reduction in document processing time. This technology not only streamlines workflows but also aligns with the mission of reducing administrative tasks while adhering to ethical guidelines. It ensures that the care for individuals remains the top priority. As we reflect on the transformative potential of AI, it's important to recognize that, as noted, "AI is transforming diagnostics, offering unprecedented accuracy and speed." This underscores the platform's role in enhancing the quality of documentation and care for individuals.
By embracing such innovative solutions, healthcare providers can reclaim valuable time and focus on what truly matters: their patients. Are you ready to explore how AI can support your practice and improve patient care? Let's take this journey together, prioritizing compassion and efficiency in healthcare.
Heidi Health: Comprehensive SOAP Note Template with Practical Examples
Heidi Health provides a SOAP report EMS example that truly understands the needs of healthcare providers. This comprehensive tool not only provides a soap report ems example for each component—Subjective, Objective, Assessment, and Plan—but also addresses the emotional challenges providers face daily. Imagine the relief of having a structured approach that ensures all vital information is documented, enhancing communication and continuity of care.
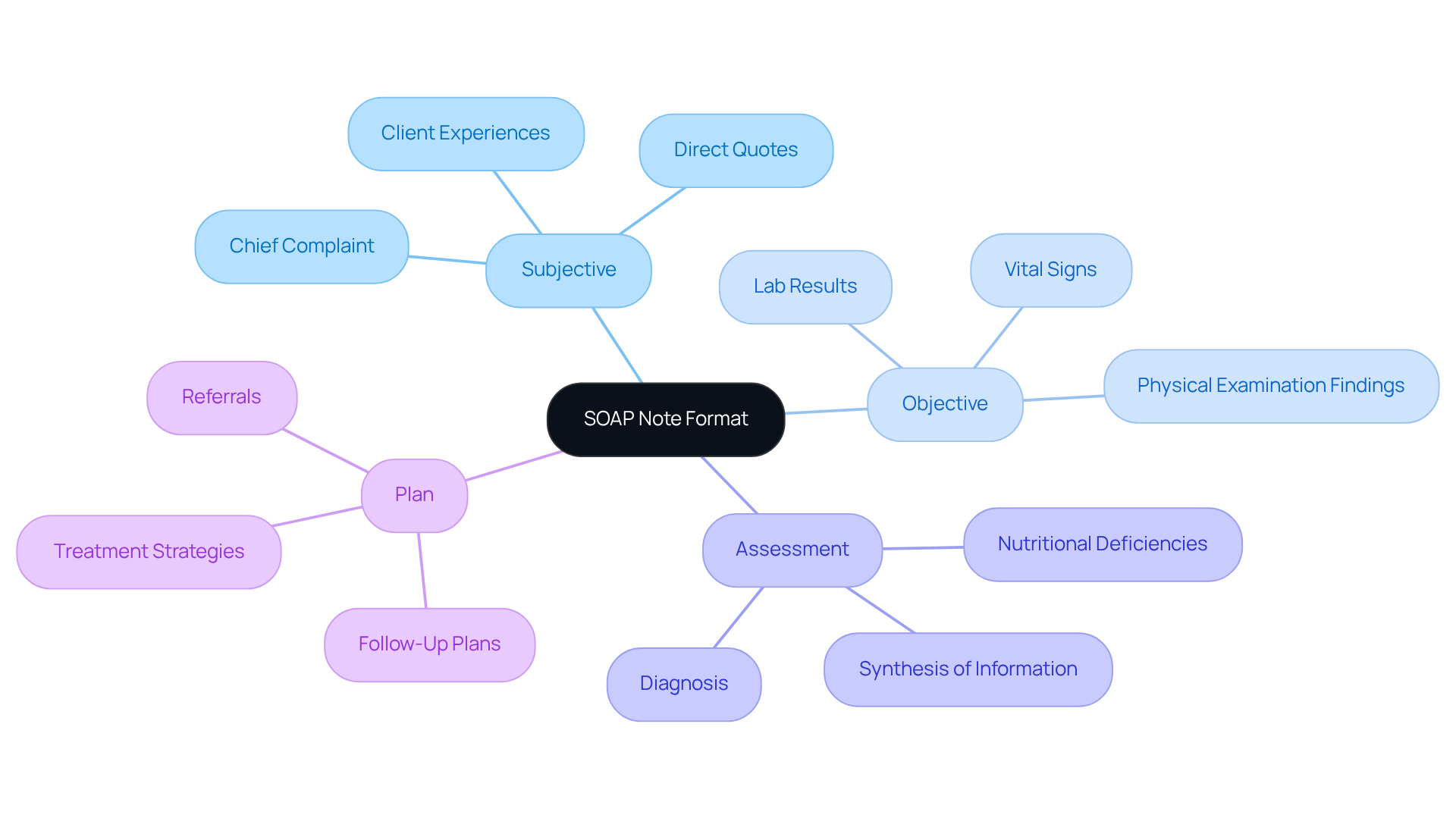
By adopting the soap report ems example format, providers can effectively capture detailed client experiences, clinical findings, and treatment plans, which are crucial for informed decision-making. The Subjective section allows practitioners to document the individual's chief complaint and relevant history, while the Objective section records quantifiable data such as vital signs and lab results. This clarity fosters a deeper connection with patients, ensuring they feel heard and understood.
The Assessment synthesizes this information, leading to a professional diagnosis, and the Plan outlines tailored treatment strategies. It's remarkable to note that the recording of vital signs increased from 80% to 98% after implementing organized formats, showcasing their significant impact on improving care results. By applying best practices—like using clear language and maintaining objectivity—medical documentation becomes more effective, ultimately enhancing care outcomes.
As Elaf Abdelrahman wisely noted, 'Precise and organized clinical records are vital for providing high-quality care to individuals.' Furthermore, tools such as the AI Charting Assistant empower professionals to create clinical documentation efficiently, enabling them to focus more on what truly matters: caring for individuals. By leveraging generative AI, healthcare providers can simplify the documentation process, reduce administrative burdens, and enrich the quality of interactions with patients.
Are you ready to embrace these solutions and enhance your practice? Together, we can foster a more compassionate and efficient healthcare environment.
NCBI: Understanding the Clinical Significance of SOAP Notes
In the demanding world of healthcare, clinical documentation serves a crucial role in recording interactions with individuals. This process not only ensures that vital information is communicated effectively among healthcare professionals but also addresses the emotional challenges faced by providers. Have you ever felt overwhelmed by the administrative burdens that can impact patient care? Organized clinical documents function as a legal record, and they are essential for clinical decision-making, treatment planning, and ensuring continuity of care.
By fostering transparent communication, clinical documentation plays a vital role in enhancing healthcare outcomes and improving service provision. Imagine how much smoother collaboration among clinicians can be when information is clearly organized. This clarity encourages effective teamwork, ultimately leading to enhanced care for individuals.
As healthcare providers, it’s essential to recognize the importance of these documents. They not only streamline processes but also support the compassionate care that every patient deserves. Let’s continue to prioritize effective clinical documentation, ensuring that we provide the best possible care for those we serve.

Sondermind: Step-by-Step Guide to Writing Effective SOAP Notes
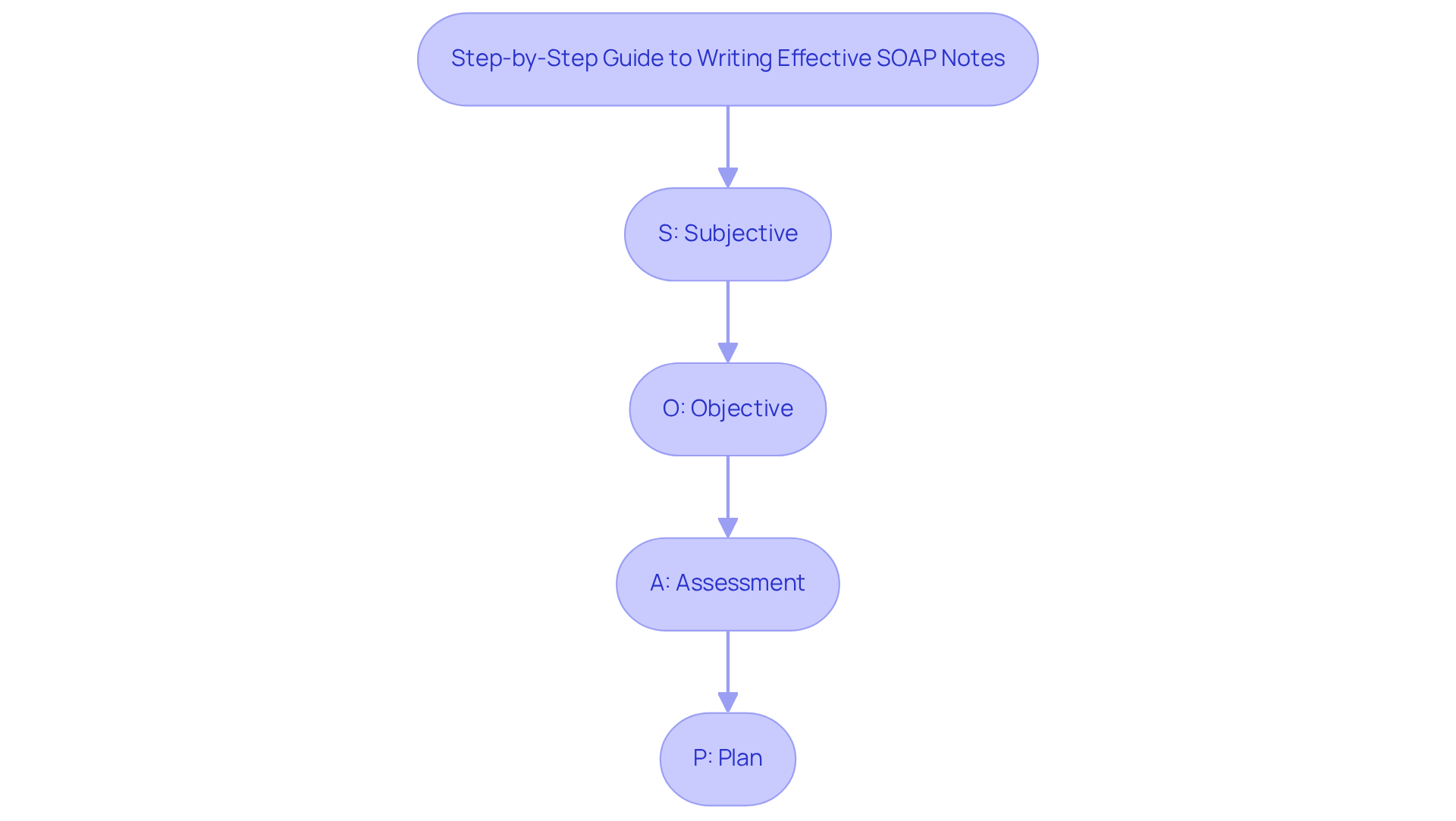
At Sondermind, we understand the emotional challenges that healthcare providers face in their daily practice. Creating effective documentation can often feel overwhelming, especially when administrative burdens detract from patient care. Our extensive, detailed guide offers a compassionate approach to enhancing your documentation skills, carefully outlining each element to improve comprehension.
Clarity and conciseness in medical records are not just best practices; they are essential for fostering better patient care. By focusing on relevant details that directly impact care, you can significantly enhance your clinical summaries. Imagine how much more effective your communication could be with clear and actionable documentation.
By following these organized steps, healthcare professionals can greatly improve their record-keeping abilities. This not only ensures that your documentation is informative but also actionable, ultimately leading to better communication among providers and reducing the risk of errors. Remember, clear and concise documentation is key to elevating the quality of patient care. We encourage you to engage with our guide and take the next step towards improving your documentation practices.
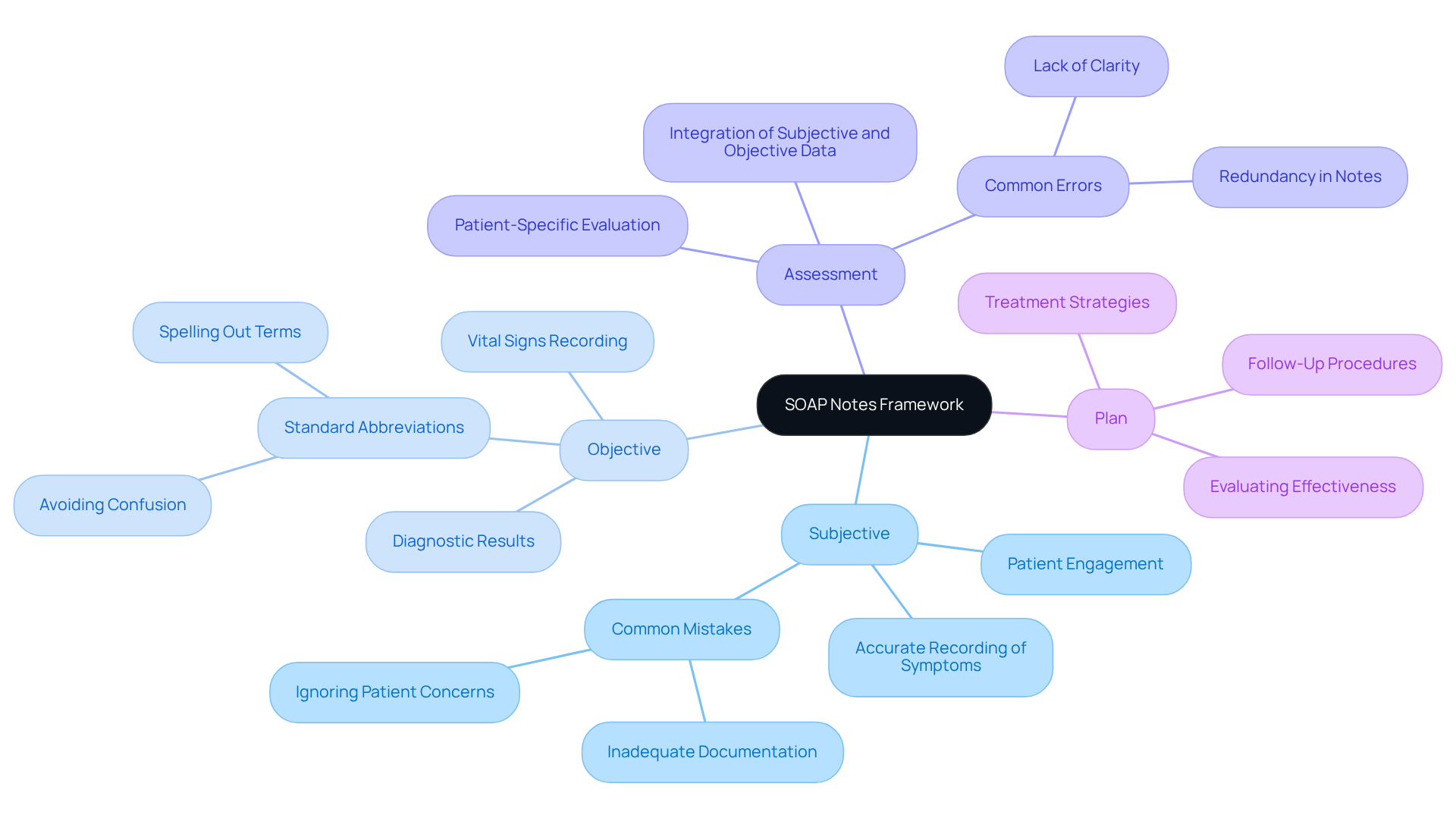
Wolters Kluwer: Expert Insights on SOAP Note Components
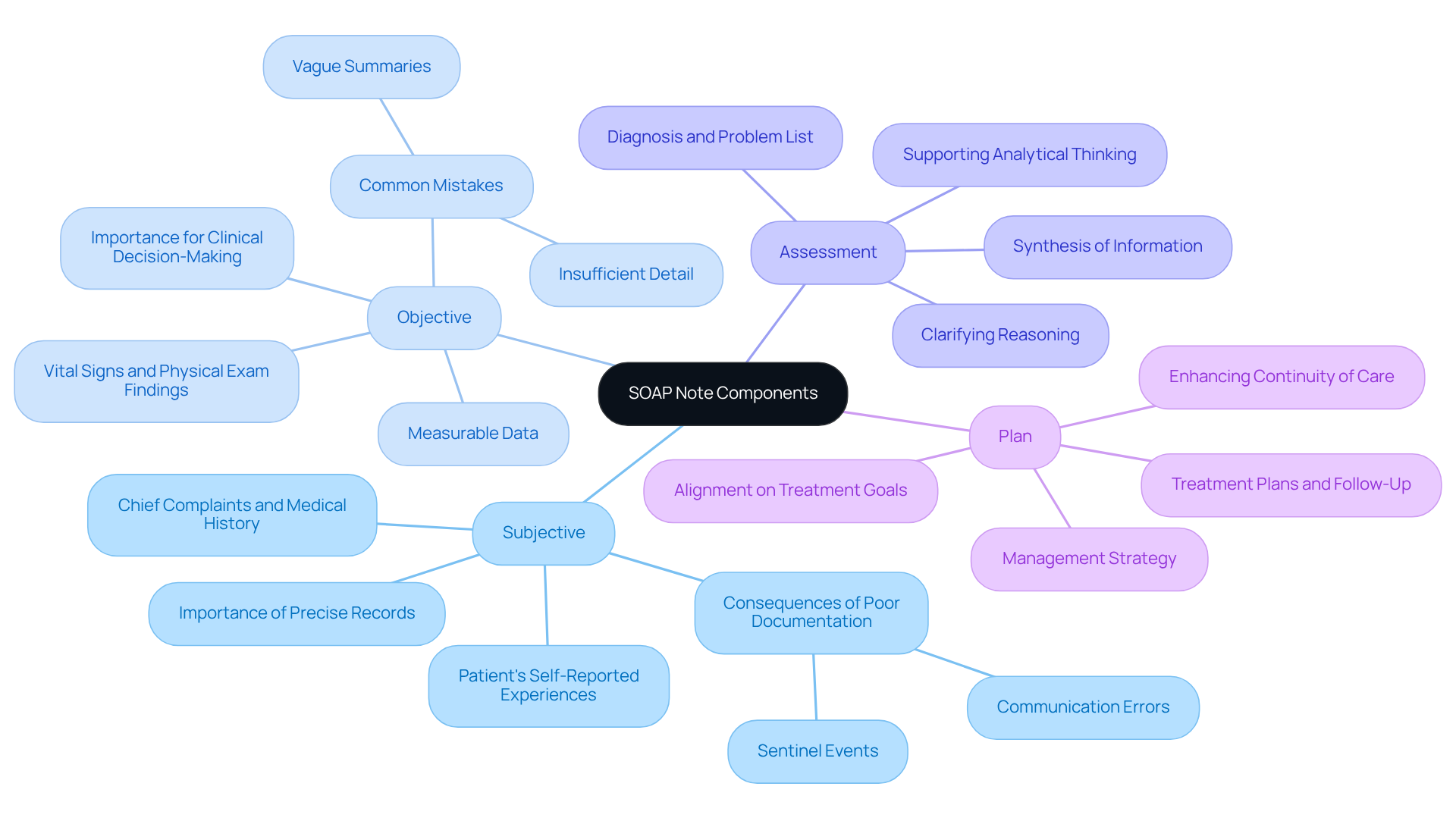
Wolters Kluwer recognizes the emotional challenges that healthcare providers face in delivering high-quality care. Understanding the elements of structured documentation—Subjective, Objective, Assessment, and Plan—is essential for enhancing communication and collaboration within the care team, particularly in a soap report ems example. By grasping the purpose of each element, healthcare professionals can not only improve their record-keeping but also foster a nurturing environment for individuals in their care.
Each section of the soap report ems example serves a distinct purpose, contributing to effective communication. Let’s explore how these elements can impact patient care:
-
Subjective: This section captures the patient's self-reported experiences, including their chief complaints and relevant medical history. Precise records here are vital, as they provide context for the clinician's evaluation and inform treatment choices. Poor documentation in this area can lead to communication errors, which are among the most common causes of sentinel events in healthcare.
-
Objective: The Objective section includes measurable data such as vital signs and physical exam findings. This factual basis is crucial for clinical decision-making, ensuring that assessments are grounded in objective evidence. Common mistakes in this section consist of vague summaries and insufficient detail, which can hinder effective management of individuals.
-
Assessment: In this section, clinicians synthesize information from the Subjective and Objective sections to arrive at a diagnosis. A well-crafted evaluation not only summarizes the individual's condition but also includes a problem list and differential diagnoses, guiding further management. It is essential for clinicians to clarify their reasoning and support analytical thinking in problem-solving.
-
Plan: The Plan outlines the management strategy for each identified medical issue, detailing treatment plans and follow-up considerations. A clear plan enhances continuity of care and ensures that all team members are aligned on the individual's treatment goals.
By mastering the soap report ems example structured format, healthcare providers can significantly enhance their record-keeping practices. This leads to improved outcomes for individuals receiving care and fosters better communication within the healthcare team. Embracing the standard format encourages familiarity and supports structured documentation, which is crucial for maintaining high standards of care. Let’s work together to improve our practices and the care we provide.
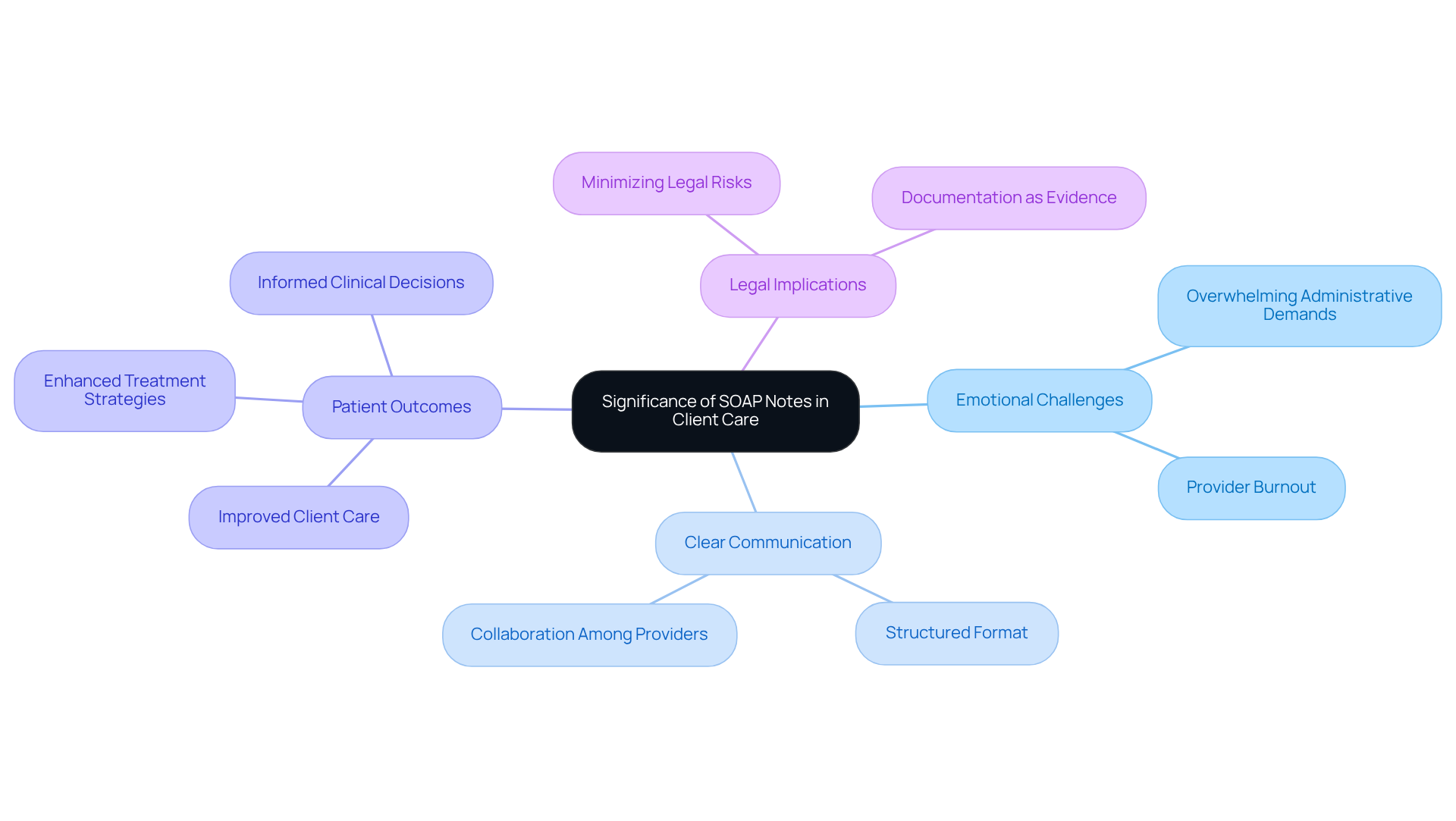
Zanda Health: The Purpose and Significance of SOAP Notes in Client Care
At Zanda Health, we recognize the emotional challenges healthcare providers face in delivering exceptional client care. Structured documentation, exemplified by a soap report ems example, plays a vital role in alleviating these burdens, serving as an essential tool for recording client interactions and treatment strategies. How often do we feel overwhelmed by the administrative demands that can detract from our focus on patients? By prioritizing effective clinical note documentation, we can enhance the quality of care and improve client outcomes.
The structured format of SOAP notes, as demonstrated in the soap report ems example, which includes Subjective, Objective, Assessment, and Plan, facilitates clear communication among healthcare providers. This seamless sharing of information fosters collaboration, ensuring that everyone involved in a client's care is informed and aligned. It promotes a thorough understanding of each individual's unique needs, empowering healthcare teams to make informed choices that positively influence health outcomes.
As specialists in the field highlight, careful record-keeping is a fundamental aspect of efficient healthcare delivery, as demonstrated in a soap report ems example, and not merely a procedural requirement. This practice can significantly enhance patient experiences and outcomes. In fact, research has shown that the evaluation component of clinical documentation can improve results by as much as 50%.
Furthermore, clear and prompt documentation practices are essential for maintaining high standards of care and minimizing legal risks associated with inadequate record-keeping. As Lawrence Weed, the innovator of the structured format, wisely stated, 'The format was created to guarantee that clinicians record their observations in a manner that’s simple to document and revisit.' This underscores the importance of structured documentation in clinical practice.
Let us embrace the power of organized documentation, fostering a nurturing environment where both providers and patients thrive.
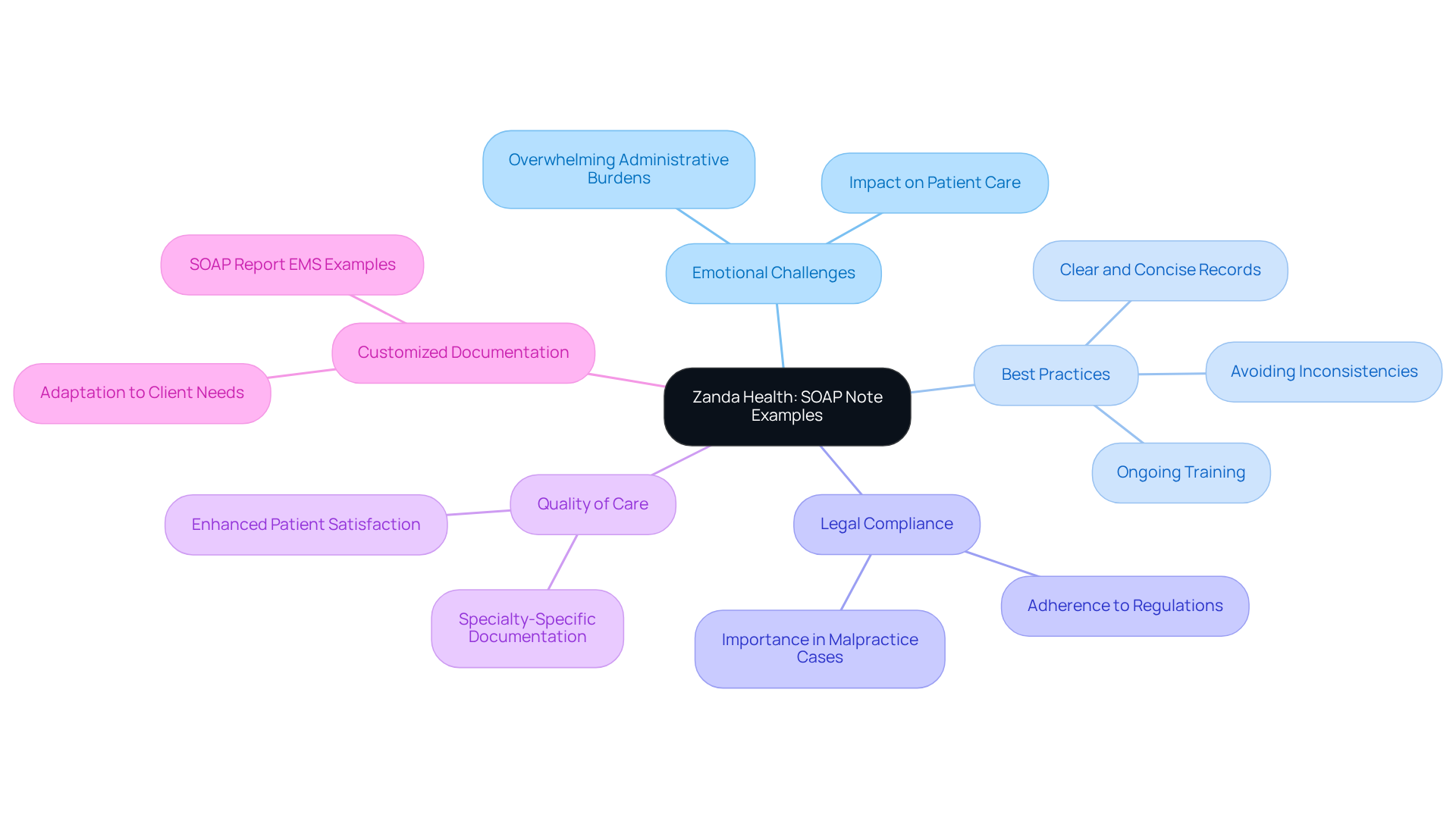
Zanda Health: SOAP Note Examples Across Different Specialties
At Zanda Health, we understand the emotional challenges healthcare providers face when it comes to record-keeping. It can often feel overwhelming, especially with the administrative burdens that can detract from patient care. Our range of customized sample records, including a SOAP report EMS example, tailored for various specialties, offers a compassionate solution to these challenges.
These SOAP report EMS examples are not just tools; they serve as vital resources that empower healthcare professionals to adapt their documentation to meet the unique needs of their clients. By examining these specialized instances, providers can enhance their record-keeping skills, ensuring their notes are both comprehensive and relevant to each individual’s condition and treatment plan.
Current best practices underscore the importance of clear, concise, and organized records. These elements are essential for fostering effective communication among healthcare professionals and maintaining high standards of care. Have you considered how streamlined records could improve your practice?
Moreover, it is crucial for clinical records to comply with laws and regulations regarding client files. This adherence not only protects your practice but also helps you understand the legal implications of record-keeping. Statistics reveal that healthcare providers who embrace specialty-specific documentation practices can significantly boost the quality of care, leading to better outcomes and enhanced patient satisfaction.
Avoiding inconsistencies in charting is equally important, as it can prevent negative repercussions in malpractice cases. Ultimately, mastering the art of customized documentation is a vital step toward providing exceptional healthcare. We invite you to explore these resources further and see how they can transform your approach to patient care.
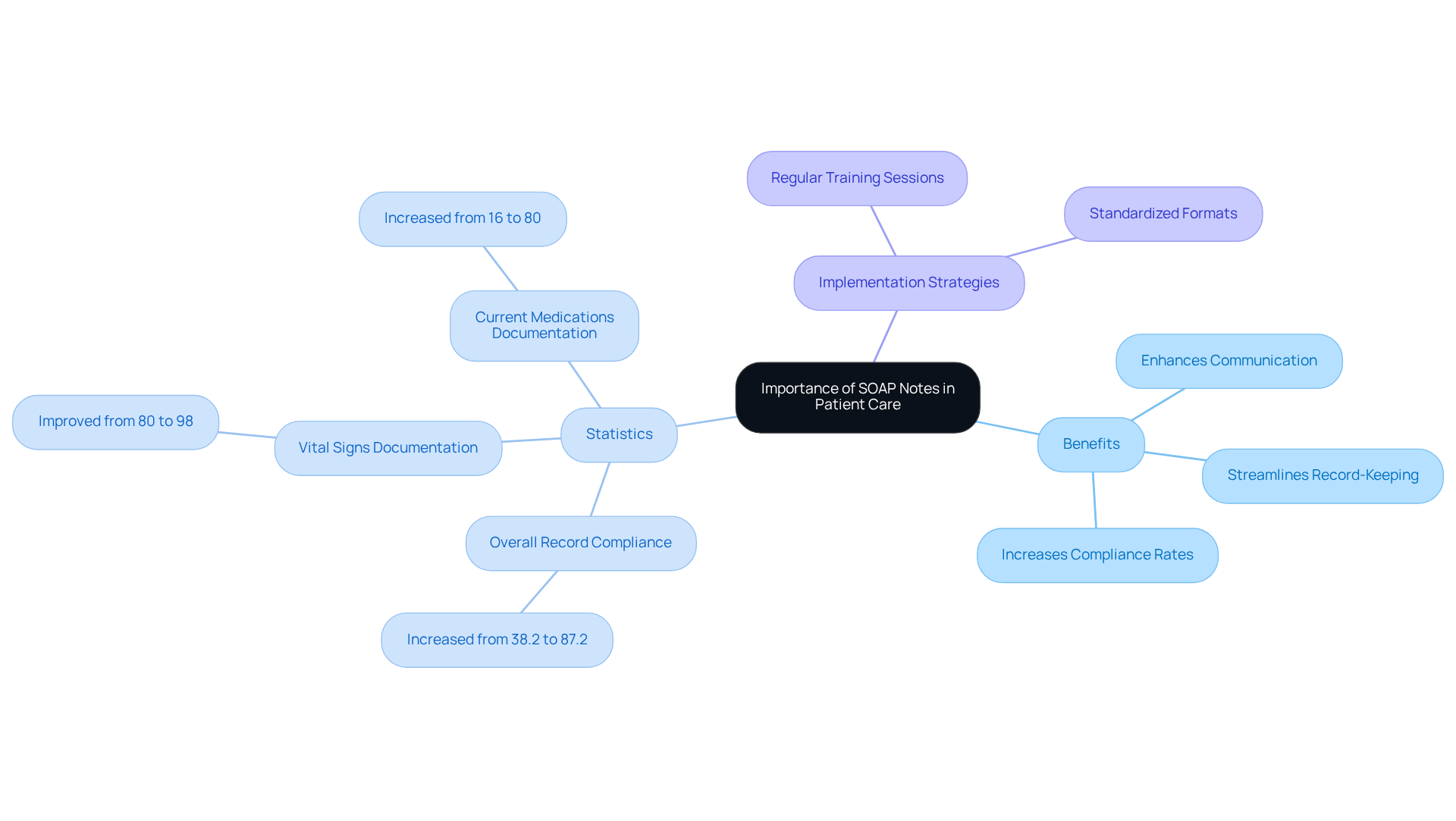
Heidi Health: Importance of a Good SOAP Note Template for Patient Care
Heidi Health emphasizes the importance of a quality SOAP report EMS example in enhancing care delivery, particularly within fragmented healthcare systems. Have you ever felt overwhelmed by the administrative demands of your role? A well-structured soap report ems example can save you time while ensuring that all critical information is captured accurately, fostering better communication and coordination among various providers.
By utilizing a quality soap report ems example, healthcare providers can simplify their record-keeping process. This allows you to focus more on meaningful interactions with clients and less on paperwork, ultimately elevating the quality of care you deliver. Research shows that adopting organized record-keeping practices can lead to a remarkable increase in compliance rates; for instance, overall record compliance rose from 38.2% to 87.2% after introducing standardized templates and focused training. Additionally, the recording of vital signs improved from 80% to 98%, while the documentation of current medications increased from 16% to 80%. These statistics highlight the crucial role structured templates play in accurately capturing essential individual information.
Imagine how generative AI could further streamline this process by automating records and enhancing interactions with individuals, thereby alleviating provider burdens. As Rajeev Rajagopal aptly states, "By ensuring precise, consistent, and prompt clinical record keeping, medical transcription services enhance patient outcomes and improve overall healthcare practice management."
To effectively implement structured templates, consider:
- Regular training sessions
- The use of standardized formats tailored to your specific needs
Together, we can address the challenges posed by fragmented systems and improve the overall quality of care.
StatPearls: Foundational Overview of SOAP Notes for Healthcare Providers
StatPearls provides a compassionate overview of clinical notes, shedding light on their structure and purpose in healthcare records. This guidance is particularly beneficial for new healthcare providers who might feel overwhelmed by the documentation format. By understanding the fundamentals, providers can ensure their documentation is not only effective but also contributes positively to patient care.
The acronym for Subjective, Objective, Assessment, and Plan serves as a structured framework for recording encounters with individuals. This format fosters effective communication among healthcare professionals, enhancing the quality of care by ensuring that all crucial information is captured systematically. Additionally, utilizing standard medical abbreviations and avoiding unnecessary details are vital components of efficient clinical notes. Clear communication in records supports healthcare and increases the likelihood of successful medical reimbursement.
Understanding this framework is essential for creating comprehensive records that meet both clinical and legal standards. Training programs focused on note documentation can significantly bolster providers' skills, empowering them to accurately record individual interactions and treatment plans. For example, workshops that highlight the importance of engaging with patients during consultations can assist clinicians in capturing subjective experiences, which is often overlooked.
However, it's important to acknowledge the limitations of this model, such as its inability to document changes over time, which can impact diagnosis and treatment. Furthermore, the APSO format (Assessment, Plan, Subjective, Objective) has been shown to improve speed, accuracy, and usability for chronic disease visits, offering an alternative approach to record-keeping.
Moreover, promptly revising clinical notes after interactions with individuals is crucial for maintaining accurate medical records, and compliance with HIPAA regulations is essential for protecting personal information. Regular training on compliance issues is necessary to ensure that healthcare providers stay informed about best practices in documentation. As specialists emphasize, mastering the structured format is an invaluable tool for healthcare providers, enhancing their ability to communicate essential patient information effectively.
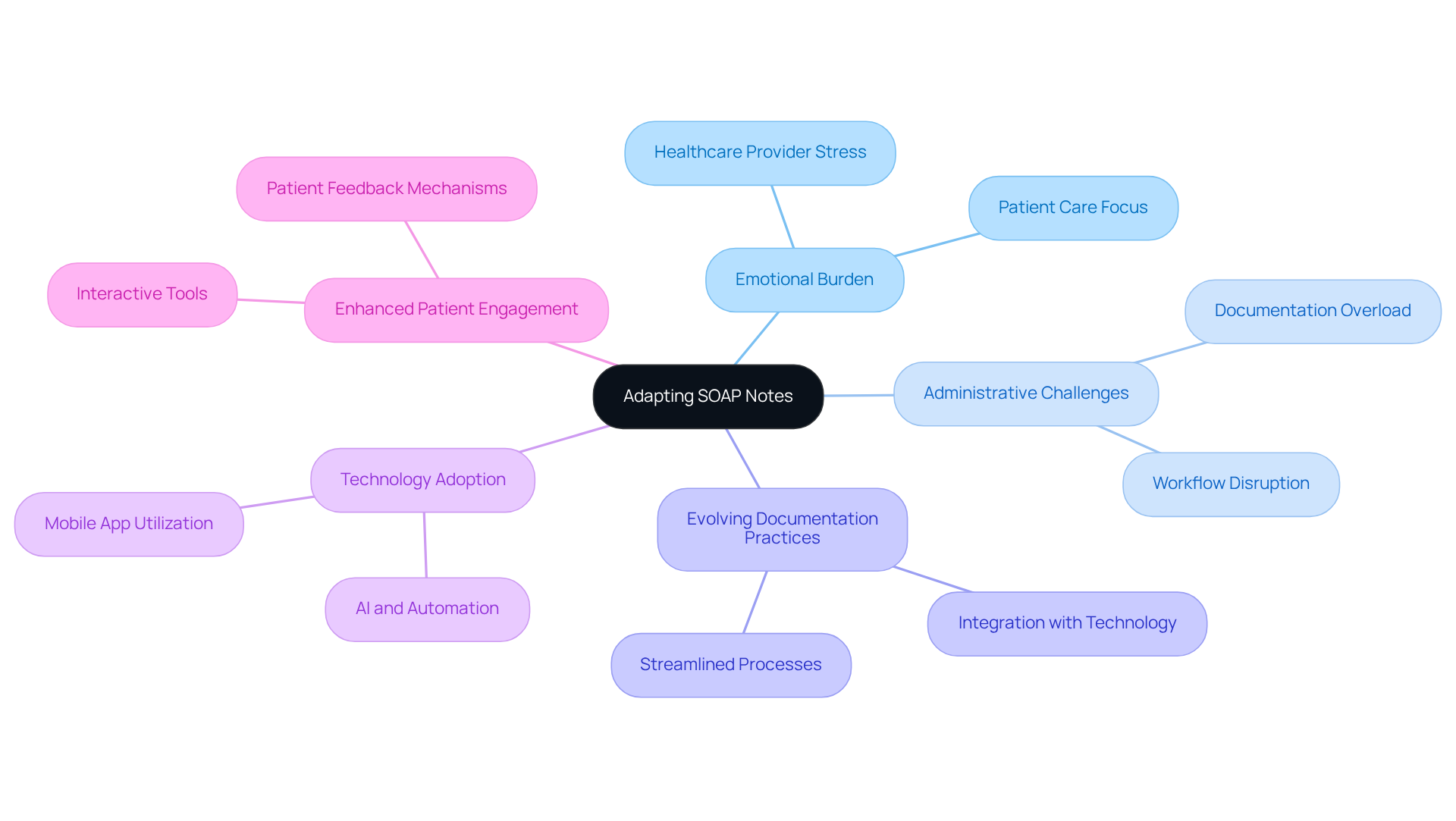
Zanda Health: Adapting SOAP Notes to Modern Healthcare Challenges
At Zanda Health, we understand the emotional weight that healthcare providers carry as they navigate the complexities of modern healthcare. The challenges of telehealth and collaborative care can feel overwhelming, and the administrative burdens often distract from what truly matters—patient care. By modifying documentation practices to meet these evolving needs, we can alleviate some of that pressure.
As the healthcare landscape transforms, it’s essential for documentation practices to evolve as well. Embracing new technologies and methodologies allows healthcare providers to maintain the relevance and effectiveness of their SOAP report EMS example. This not only enhances the quality of care but also fosters greater patient engagement, creating a more supportive environment for everyone involved.
Imagine a world where your documentation seamlessly integrates with your workflow, allowing you to focus more on your patients and less on paperwork. By adopting these innovative approaches, you can transform your practice and improve patient outcomes. We encourage you to explore these solutions further and join us in this journey towards more compassionate care.
Conclusion
Integrating SOAP notes into healthcare documentation goes beyond mere procedure; it represents a transformative practice that can profoundly enhance patient care and provider efficiency. By embracing the structured format of Subjective, Objective, Assessment, and Plan, healthcare professionals can document vital information clearly and effectively. This fosters improved communication and collaboration within care teams, addressing the emotional challenges that many providers face.
Throughout this article, we've explored various examples and tools that illustrate how organizations like CosmaNeura and Heidi Health are leading the charge for better documentation practices. From AI-assisted reporting that significantly reduces processing time to comprehensive templates that enhance clarity and compliance, the advantages of structured SOAP notes are clear. The focus on training and adapting these practices to meet modern healthcare challenges further underscores a commitment to upholding high standards of care.
The importance of effective SOAP documentation cannot be overstated. As healthcare providers adopt these innovative solutions and best practices, they not only ease administrative burdens but also prioritize the compassionate care that patients truly deserve. The journey toward enhanced documentation is a collective endeavor that can lead to improved health outcomes and a more supportive environment for both providers and patients. Now is the time to take proactive steps in refining documentation skills and leveraging available resources to ensure that quality care remains at the forefront of healthcare delivery.




