Overview
This article addresses the emotional challenges that healthcare providers face in their daily practice. It offers effective samples and best practices for writing SOAP notes in healthcare documentation, recognizing how administrative burdens can detract from patient care. By emphasizing structured SOAP notes, we can enhance communication, improve the quality of patient care, and streamline administrative tasks. This ultimately allows healthcare providers to focus more on meaningful patient interactions rather than getting lost in paperwork.
Imagine the relief of having a clear and concise way to document patient information. Structured SOAP notes not only facilitate better communication among healthcare teams but also contribute to a more efficient workflow. When administrative tasks are simplified, healthcare providers can devote more time to what truly matters—caring for their patients.
We encourage you to explore these best practices and consider how implementing structured SOAP notes can transform your documentation process. By doing so, you can alleviate some of the stress associated with administrative duties and enhance the overall quality of care you provide. Together, let’s prioritize patient interactions and foster a more compassionate healthcare environment.
Introduction
Healthcare documentation can often feel like an uphill battle. Providers are frequently swamped by administrative tasks that hinder their primary mission: patient care. This overwhelming burden can lead to frustration and burnout, impacting not only the providers but also the patients they serve.
The emergence of AI-powered solutions, such as CosmaNeura, offers a promising way to revolutionize this landscape. By automating the creation of SOAP notes, these tools can free up valuable time for clinicians, allowing them to focus more on their patients. Imagine what it would feel like to have more time to connect with those in your care, to truly listen and respond to their needs.
However, as the reliance on technology grows, healthcare professionals may wonder: how can they ensure that their documentation remains precise, compliant, and truly beneficial to patient outcomes? This article aims to explore effective SOAP note samples, best practices, and the transformative role of technology in enhancing healthcare documentation.
Together, we can navigate these changes and embrace solutions that not only alleviate administrative burdens but also improve the overall quality of care. Let’s delve into the possibilities that lie ahead.
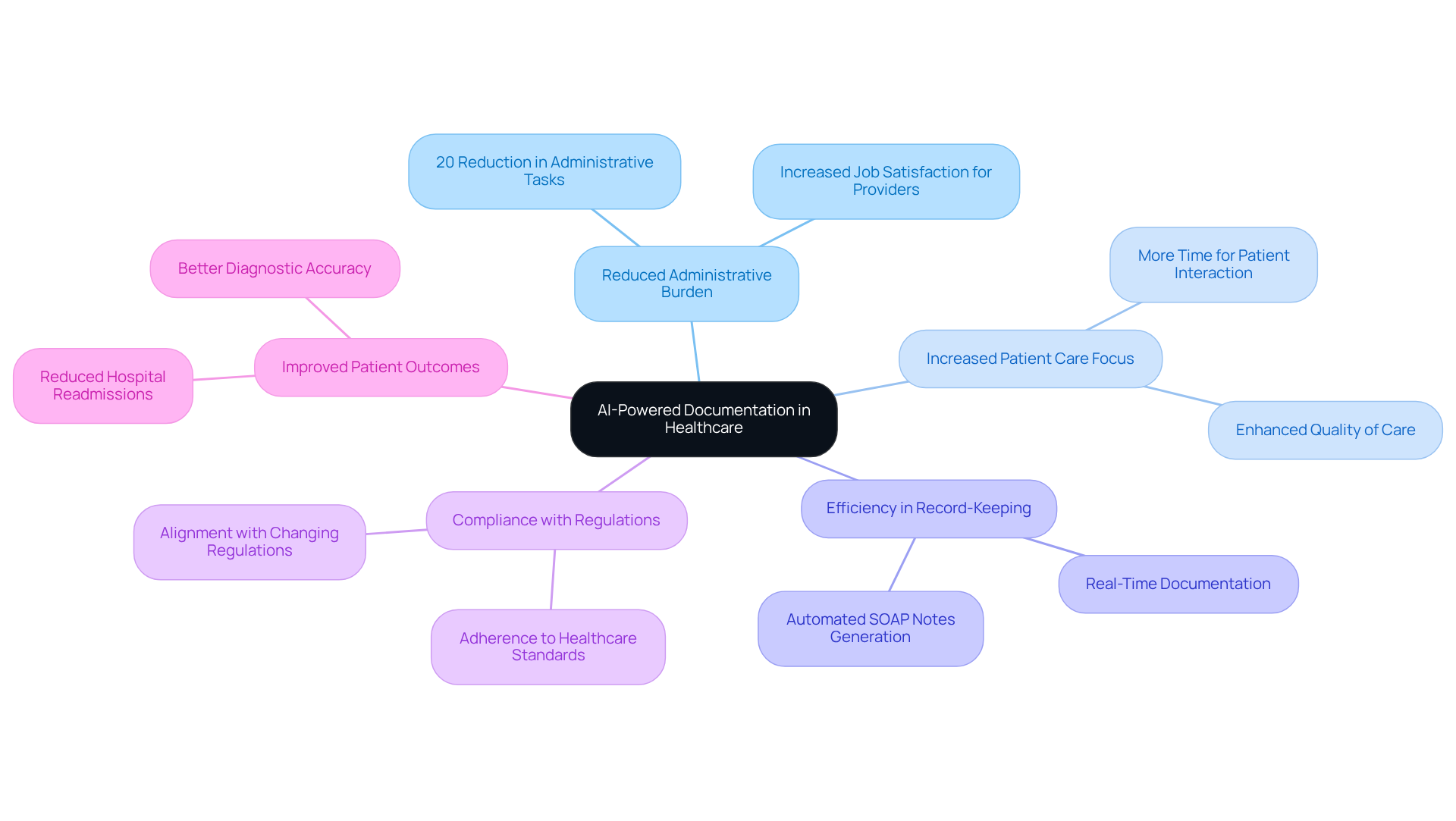
CosmaNeura: Streamline SOAP Notes with AI-Powered Documentation
Healthcare providers often face overwhelming administrative burdens that can detract from their primary focus: patient care. CosmaNeura understands these challenges and utilizes advanced AI technology to automate the generation of soap notes samples. By doing so, it significantly reduces the time spent on record-keeping, allowing clinicians to redirect their attention towards what truly matters—their patients.
Imagine reclaiming valuable hours each day. With AI handling approximately 20% of administrative tasks, healthcare professionals can enhance their ability to deliver quality care. This shift not only fosters efficiency but also ensures that documentation remains precise and compliant with healthcare standards. The result? Better outcomes for individuals who rely on their expertise.
Moreover, automating clinical documentation helps providers stay aligned with ever-changing healthcare regulations. This promotes a smoother workflow that benefits both professionals and the individuals they serve. If you're ready to embrace a solution that alleviates administrative pressures and enhances patient care, consider how CosmaNeura can support you in this vital journey.
SOAP Note Structure: Understanding Subjective, Objective, Assessment, and Plan
SOAP notes samples are organized into four essential components: Subjective, Objective, Assessment, and Plan. The Subjective section captures the individual's personal experiences, including their chief complaint and history of present illness, which is vital for understanding their perspective. Have you ever considered how these insights shape the care we provide? The Objective section presents measurable data, such as vital signs and lab results, providing a factual basis for clinical evaluation. The Assessment synthesizes both subjective and objective information to arrive at a diagnosis, while the Plan outlines the proposed treatment strategies and follow-up actions.
Mastering this structure is crucial for effective communication among healthcare providers, as it facilitates clarity and continuity of care. Research indicates that ineffective communication is a leading cause of sentinel events in healthcare. This underscores the need for precise documentation. By utilizing SOAP notes samples and following the structured format, clinicians can improve health outcomes, simplify communication, and guarantee that essential information is easily accessible. Additionally, the flexibility of medical documentation enables continuous revisions, which are crucial for monitoring patient development and making educated clinical choices.
Incorporating generative AI into the SOAP note process can further enhance these benefits. Imagine reducing the administrative burden on healthcare providers. AI tools can assist in automating the documentation process, allowing clinicians to concentrate more on client interactions and less on paperwork. This shift ultimately reduces burnout and enhances efficiency, creating a more nurturing environment for both providers and patients. Let’s embrace these advancements together for a better future in healthcare.

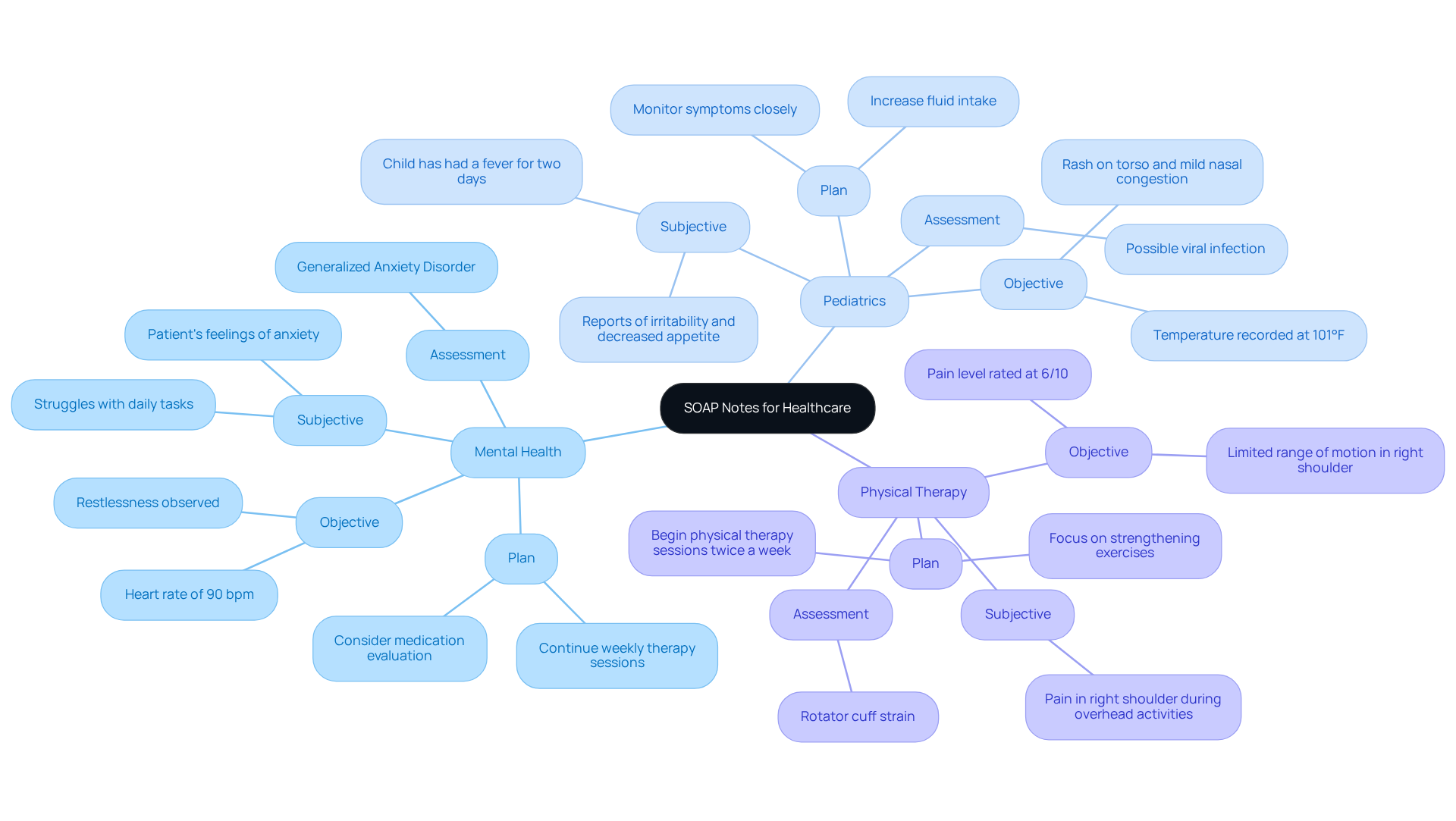
Sample SOAP Notes for Mental Health, Pediatrics, and Physical Therapy
-
Mental Health:
- Subjective: The patient shares feelings of anxiety and being overwhelmed, struggling to manage daily tasks.
- Objective: The patient appears restless, with a heart rate of 90 bpm and fidgeting during the session.
- Assessment: Generalized Anxiety Disorder, indicating a need for ongoing support.
- Plan: Continue weekly therapy sessions, consider a medication evaluation, and implement coping strategies.
-
Pediatrics:
- Subjective: The mother reports that her child has had a fever for two days, along with irritability and decreased appetite.
- Objective: The temperature is recorded at 101°F, with a rash on the torso and mild nasal congestion observed.
- Assessment: Possible viral infection, requiring close monitoring for symptom progression.
- Plan: Monitor symptoms closely, recommend increased fluid intake, and schedule a follow-up in 48 hours to reassess.
-
Physical Therapy:
- Subjective: The patient mentions pain in the right shoulder during overhead activities, impacting daily routines.
- Objective: Limited range of motion noted in the right shoulder, with a pain level rated at 6/10 during assessment.
- Assessment: Rotator cuff strain, necessitating targeted rehabilitation.
- Plan: Begin physical therapy sessions twice a week, focusing on strengthening exercises and pain management techniques.
By utilizing generative AI tools, healthcare providers can alleviate the burden of documentation, allowing more time to focus on patient care. This innovative approach not only enhances efficiency but also enriches the quality of interactions between doctors and individuals, ultimately leading to improved health outcomes. How might this transformative method change your daily practice?
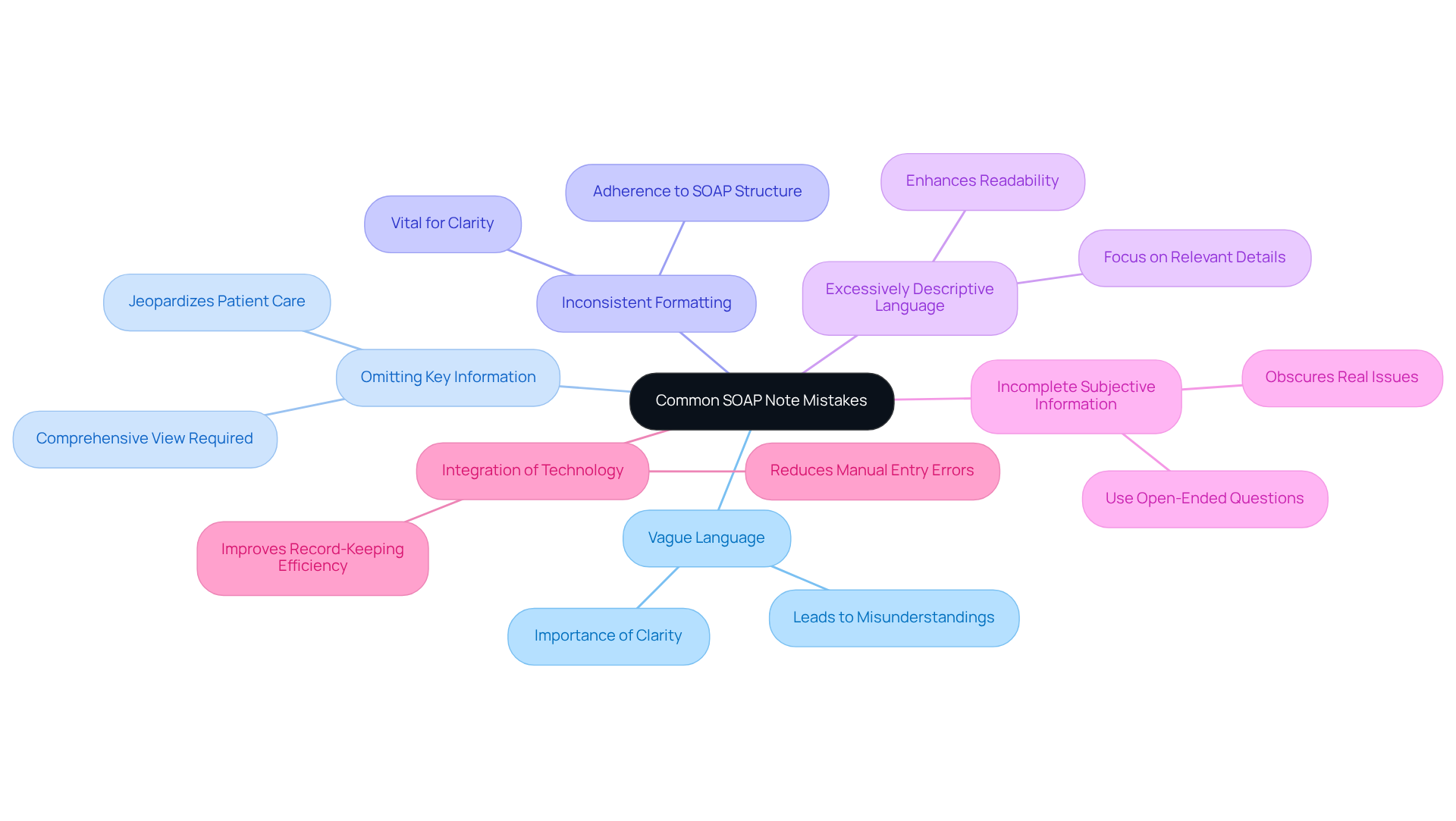
Common SOAP Note Mistakes to Avoid for Accurate Documentation
Common SOAP Note Mistakes to Avoid for Accurate Documentation include:
- Vague Language: Using non-specific terms can lead to misunderstandings and misinterpretations. It’s crucial to be exact in descriptions to ensure clarity and precision in medical records. Inconsistent documentation practices can create miscommunications and errors in care, highlighting the importance of clear language.
- Omitting Key Information: Neglecting to record crucial details can jeopardize care and lead to diagnostic mistakes. Always include relevant findings to provide a comprehensive view of the patient's condition, ensuring that no important aspect is overlooked.
- Inconsistent Formatting: Maintaining a consistent format is vital for clarity and ease of understanding. Using soap notes samples by adhering to the SOAP structure for all notes helps ensure that critical information is easily accessible. As Jess Barron states, "consistent documentation of interactions with your clients and their progress is a vital aspect of treatment."
- Excessively Descriptive Language: Avoid unnecessary details that do not contribute to the individual's care plan. Keeping notes concise and relevant enhances readability and allows for quicker reference during interactions with clients, fostering better communication.
- Incomplete Subjective Information: Omitting detailed subjective data can obscure the real cause of an individual's problem. Gathering comprehensive information through open-ended questions and direct quotes from individuals can significantly enhance diagnostic accuracy and treatment outcomes. Frequent evaluations by colleagues can assist in recognizing and rectifying discrepancies in record-keeping methods, thereby improving the quality of clinical summaries and ensuring the accuracy of soap notes samples.
- Integration of Technology: Employing technology, such as voice recognition software, can reduce manual entry mistakes and improve record-keeping efficiency. This enables healthcare providers to concentrate more on client care, ultimately enhancing the overall patient experience.
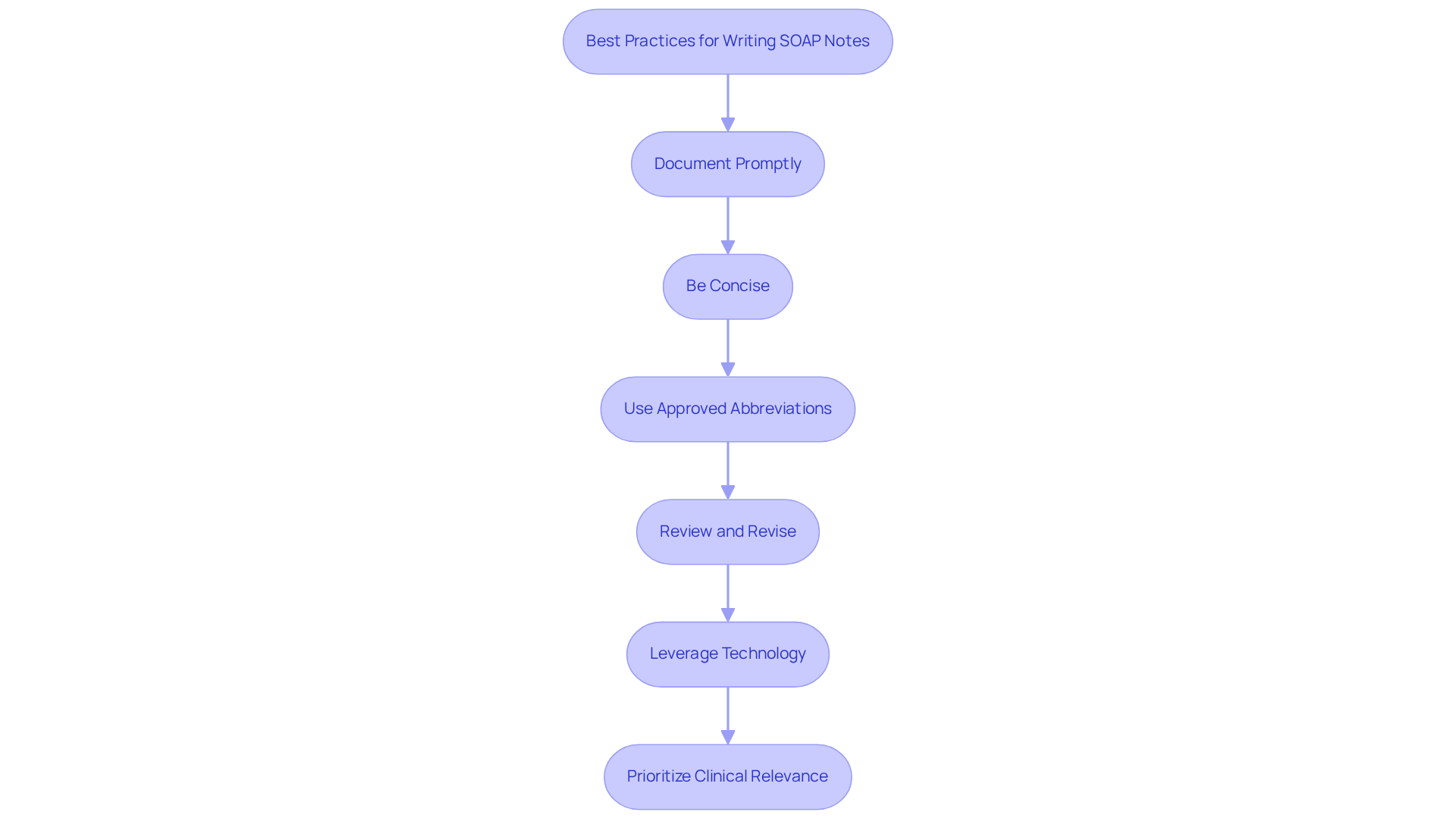
Best Practices for Writing Effective SOAP Notes
Writing effective soap notes samples can feel overwhelming at times, but by following a few best practices, you can ease this burden and enhance patient care.
-
Document Promptly: Capture critical details immediately after your patient encounters. Timely record-keeping is essential; neglecting this can lead to overlooked details that compromise patient safety and the quality of care. Consider utilizing AI tools for reminders and templates that facilitate swift documentation.
-
Be Concise: Use clear and straightforward language to convey information. Aim for brevity; a typical SOAP note should ideally be two to four paragraphs long, depending on the complexity of the client's condition. AI-driven summarization tools can effectively condense your notes.
-
Use Approved Abbreviations: Familiarize yourself with commonly accepted abbreviations to save time while ensuring clarity. This practice simplifies record-keeping and enhances communication among healthcare professionals. AI can suggest relevant abbreviations based on the context of your notes.
-
Review and Revise: Before finalizing your notes, always review them for completeness and accuracy. AI tools can help by flagging inconsistencies or missing information, significantly reducing the risk of medical errors, especially in medication administration and treatment.
-
Leverage Technology: Embrace AI-driven tools and voice recognition software to streamline the documentation process. These technologies enhance precision and allow you to focus more on patient care rather than paperwork. By automating repetitive tasks, AI can free up your time, enabling you to see more patients and improve overall care delivery.
Incorporate structured templates, as utilizing organized templates can enhance the quality of your soap notes samples by 36.6% while reducing preparation time by 42%. AI can assist in developing and personalizing these templates, promoting consistency in clinical records and facilitating better communication of care information.
- Prioritize Clinical Relevance: Focus on quality over quantity in your clinical records to ensure thorough reporting without overwhelming the reader. Each element of a SOAP note—Subjective, Objective, Assessment, and Plan—plays a vital role in effective patient management. With over 78% of providers spending more than 10 hours weekly on documentation, adopting efficient practices is crucial. AI can provide insights into the most relevant information to include based on individual histories and treatment plans.
By implementing these strategies, you can alleviate some of the administrative burdens that often accompany patient care and ultimately enhance the quality of service you provide. Remember, you are not alone in this journey; support is available to help you thrive.
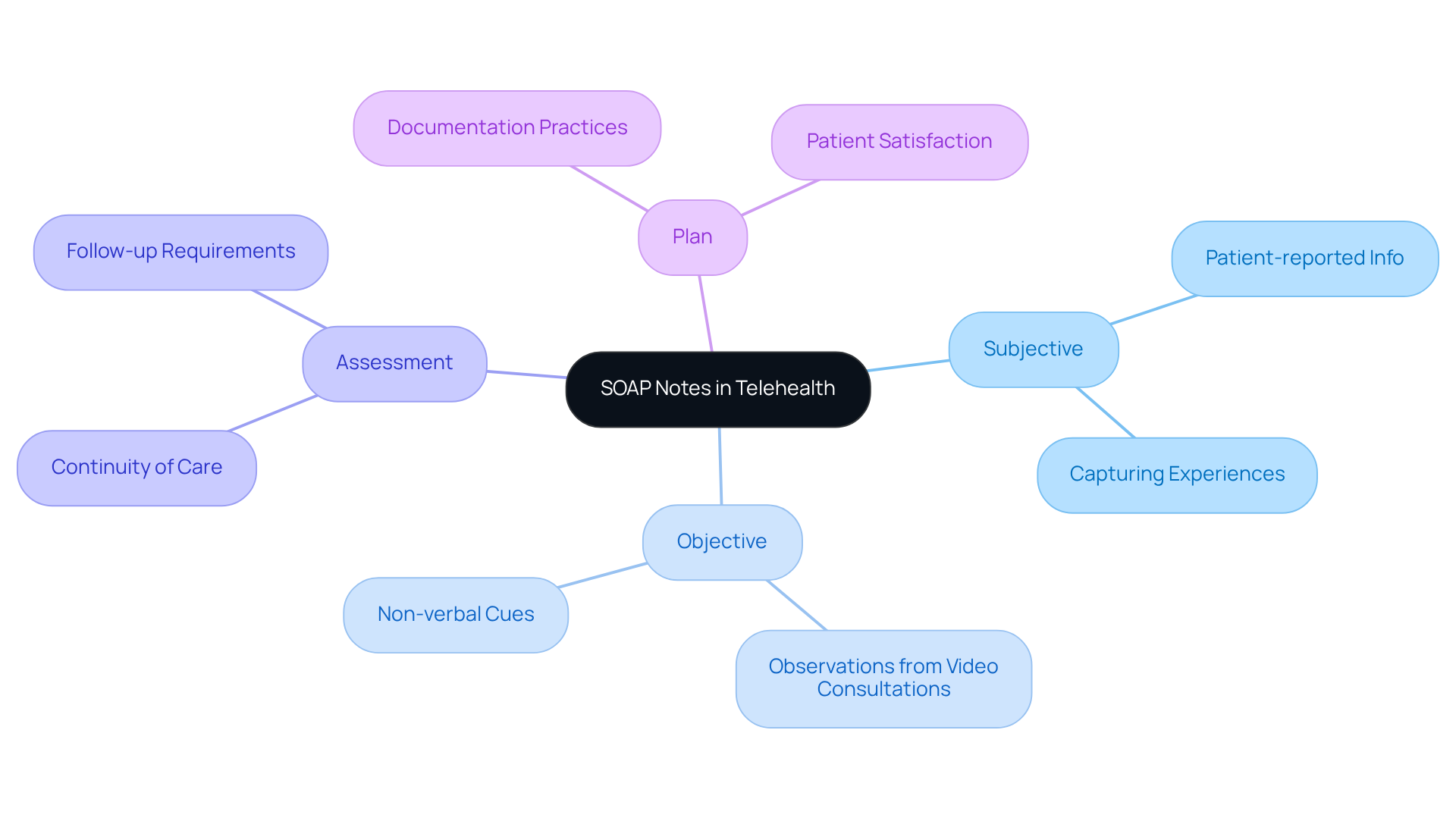
The Role of SOAP Notes in Telehealth: Ensuring Quality Care from a Distance
In the realm of telehealth, using soap notes samples plays a vital role in documenting client encounters, particularly when physical examinations are limited. Have you ever considered how this shift impacts the way we understand our patients? The Subjective section increasingly relies on patient-reported information, allowing their experiences and concerns to be captured effectively. At the same time, the Objective section can include observations from video consultations, such as non-verbal cues and environmental factors that may affect patient health.
Accurate records are essential for ensuring continuity of care and fulfilling follow-up requirements. Did you know that telehealth usage surged from under 20% before 2020 to over 50% by mid-2020? This rapid growth highlights the need for providers to adapt their documentation practices, utilizing soap notes samples to reflect the unique aspects of telehealth interactions. By doing so, we not only enhance the quality of care but also align with the growing emphasis on meticulous record-keeping in telehealth environments, where more than 80% of individuals express satisfaction with virtual care.
As we navigate this evolving landscape, the role of structured documentation remains crucial in maintaining high standards of care and fostering effective communication. Let’s embrace these changes together, ensuring that all relevant information is captured compassionately and thoroughly. How can we continue to improve our practices to better serve our patients in this new era of healthcare?
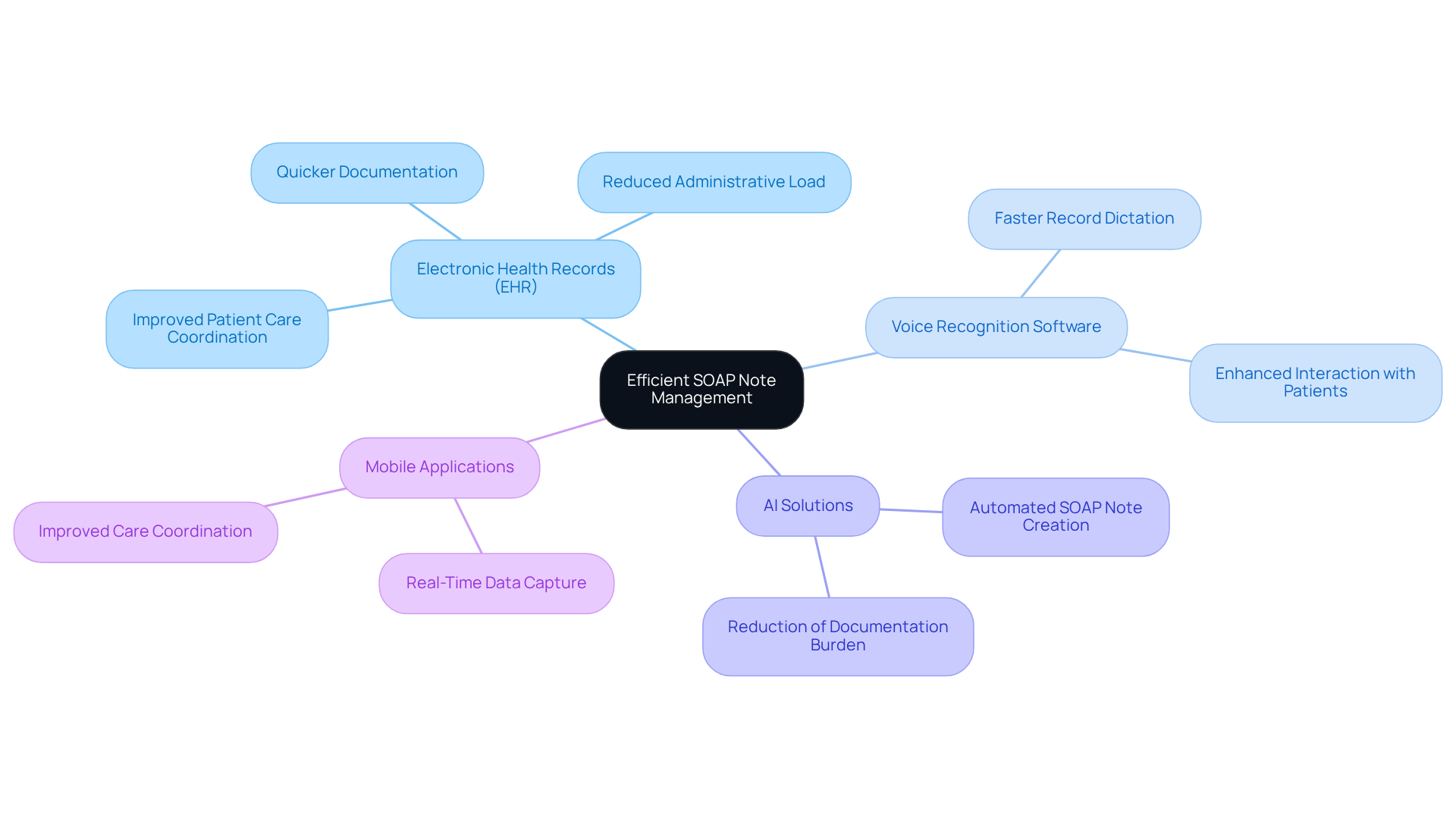
Leveraging Technology for Efficient SOAP Note Management
Healthcare providers often face overwhelming emotional challenges, particularly related to the administrative burdens that can detract from patient care. To alleviate these pressures, a variety of technologies can enhance the management of soap notes samples, leading to improved outcomes for both providers and patients.
- Electronic Health Records (EHR): EHR systems typically feature built-in templates for SOAP notes, facilitating quicker documentation of patient encounters and improving overall efficiency. These systems assist in alleviating the administrative load of managing client records and scheduling.
- Voice Recognition Software: This technology allows providers to dictate records, greatly speeding up the recording process and enabling more prompt interaction with individuals receiving care. By reducing the time spent on manual entry, clinicians can concentrate more on care for individuals.
Advanced AI solutions can automate the creation of soap notes samples based on client interactions, effectively reducing the administrative burden on clinicians, such as documentation and scheduling tasks. This enables healthcare professionals to regain valuable time, ultimately enhancing outcomes for those receiving care. As indicated by Bester Chimbo, "The electronic health record (EHR) system is often referenced as an essential component of health information technology to enhance the quality of care." - Mobile Applications: Numerous healthcare apps enable providers to record observations in real-time while on the go, ensuring that essential information is captured swiftly and precisely. A case study at Dr. George Mukhari Academic Hospital emphasized how mobile recording tools enhanced the effectiveness of healthcare providers, facilitating improved care coordination.
By incorporating these technologies, healthcare professionals can greatly improve the efficiency and quality of documentation management. This not only results in better outcomes for individuals but also helps reduce the pressures that can lead to physician burnout. How might these solutions transform your practice and enhance your connection with patients?
Legal and Ethical Considerations in SOAP Note Documentation
SOAP notes samples play a vital role not only in clinical documentation but also as essential legal records. It's crucial for healthcare providers to adhere strictly to various legal and ethical standards. Here are some key considerations that can help you navigate these challenges with care:
- Confidentiality Maintenance: Safeguarding patient information is paramount. Aligning with HIPAA regulations, you must protect Protected Health Information (PHI). Did you know that in 2022, 68% of healthcare data breaches were due to lost devices? This statistic highlights the urgent need for robust confidentiality measures. In 2023, over 93 million healthcare records were exposed in breaches, underscoring the importance of vigilance in protecting patient data.
- Accuracy Prioritization: Precise records are vital. Inaccuracies can lead to significant legal repercussions, including malpractice claims. It's concerning that 53% of healthcare data breaches stem from employee carelessness, often due to inadequate record-keeping methods. This statistic emphasizes the critical need for you to prioritize accuracy in your documentation processes.
- Adherence to Ethical Standards: Your documentation must reflect ethical guidelines, demonstrating your commitment to client care and safety. Ethical factors in clinical documentation include ensuring informed consent and honoring individual autonomy. How can you ensure these principles are upheld in your practice?
- The legal implications require that SOAP notes samples must comply with legal standards. Failure to do so can result in civil penalties ranging from $100 to $1.5 million per violation. The evolving legal landscape in 2025 emphasizes the need for you to stay informed about regulations and the potential consequences of non-compliance.
- Importance of Confidentiality: Upholding confidentiality is not just a legal obligation; it's a fundamental element of trust between you and your patients. Unauthorized disclosures can lead to a loss of trust and significant reputational damage. How do you foster that trust in your practice?
- Expert Opinions on HIPAA Compliance: Experts emphasize that regular training and awareness programs are essential for healthcare organizations to mitigate risks associated with HIPAA violations. A survey indicated that 24% of healthcare employees did not receive adequate security awareness training. This highlights a critical area for improvement in your organization.
- Statistics on HIPAA Compliance: The number of healthcare data breaches evaluated by the HHS Office for Civil Rights doubled from 2018 to 2023, with unauthorized disclosure of PHI being the most common violation. This statistic reinforces the necessity for you to implement stringent compliance measures in your documentation practices.
By focusing on these considerations, you can enhance the quality of care you provide while ensuring that your documentation practices are both ethical and legally sound. Let's work together to create a safer healthcare environment for everyone.

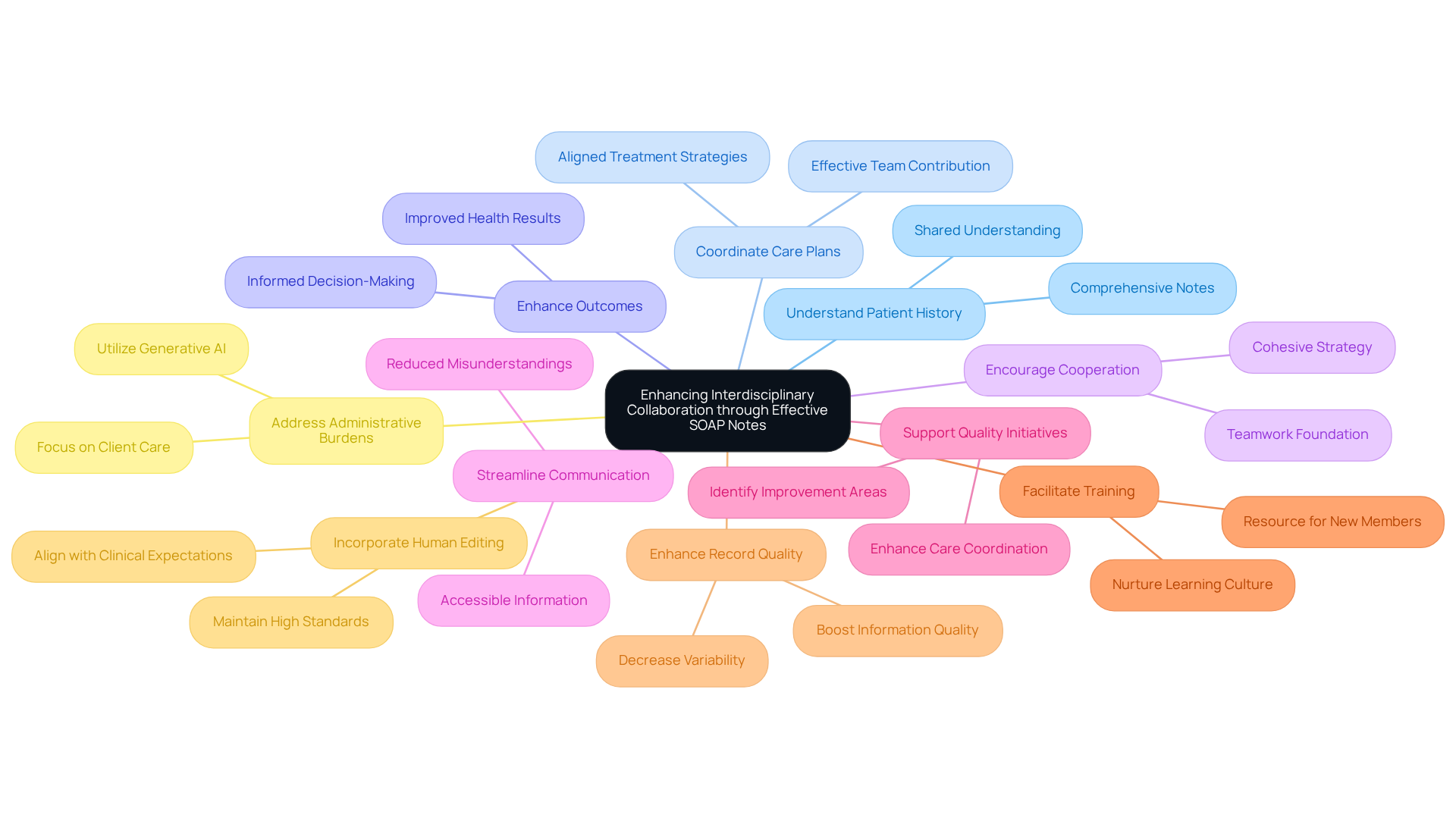
Enhancing Interdisciplinary Collaboration through Effective SOAP Notes
Effective documentation plays a crucial role in fostering interdisciplinary cooperation by providing a clear and structured account of healthcare interactions. Imagine how much easier it would be for all team members to access soap notes samples that are well-documented. This accessibility can truly transform patient care.
- Understand Patient History: Comprehensive notes empower providers to swiftly grasp a patient's background and treatment history, nurturing a shared understanding among the care team. How often do we find ourselves wishing for a clearer picture of our patients?
- Coordinate Care Plans: Clear documentation facilitates discussions about treatment strategies, ensuring that all team members are aligned in their approach and can contribute effectively to care. This alignment is vital for delivering the best outcomes.
- Enhance Outcomes for Individuals: By sharing precise and prompt information, healthcare teams can make informed decisions that lead to improved care, ultimately enhancing overall health results. Isn’t that the goal we all strive for?
- Encourage Interprofessional Cooperation: Efficient documentation serves as a foundation for teamwork, enabling various healthcare specialists to collaborate seamlessly, addressing individual care requirements through a cohesive strategy.
- Streamline Communication: Well-organized records reduce misunderstandings and miscommunications, ensuring that essential information is readily accessible to all team members, which is crucial for coordinated care.
- Support Quality Enhancement Initiatives: By examining clinical records, healthcare teams can pinpoint areas for improvement in record-keeping practices, leading to better care coordination and safety for individuals.
- Facilitate Training and Education: Clinical records can serve as valuable resources for new team members, demonstrating optimal practices in record-keeping and care coordination, thus nurturing a culture of ongoing learning within the team.
- Enhance Record Quality: Organized records have been shown to boost information quality by 20%, decreasing variability among providers and ensuring uniformity in client records.
- Incorporate Human Editing: The inclusion of human supervision in evaluating AI-generated clinical summaries is essential for maintaining high-quality standards and ensuring alignment with clinical expectations.
- Address Administrative Burdens: By utilizing generative AI to automate and simplify the record-keeping process, healthcare providers can alleviate the administrative burdens linked to conventional note-taking. This allows them to focus more on client care, ultimately improving the overall effectiveness of healthcare delivery.
Let’s embrace these solutions together, fostering a supportive environment that prioritizes patient care and teamwork.
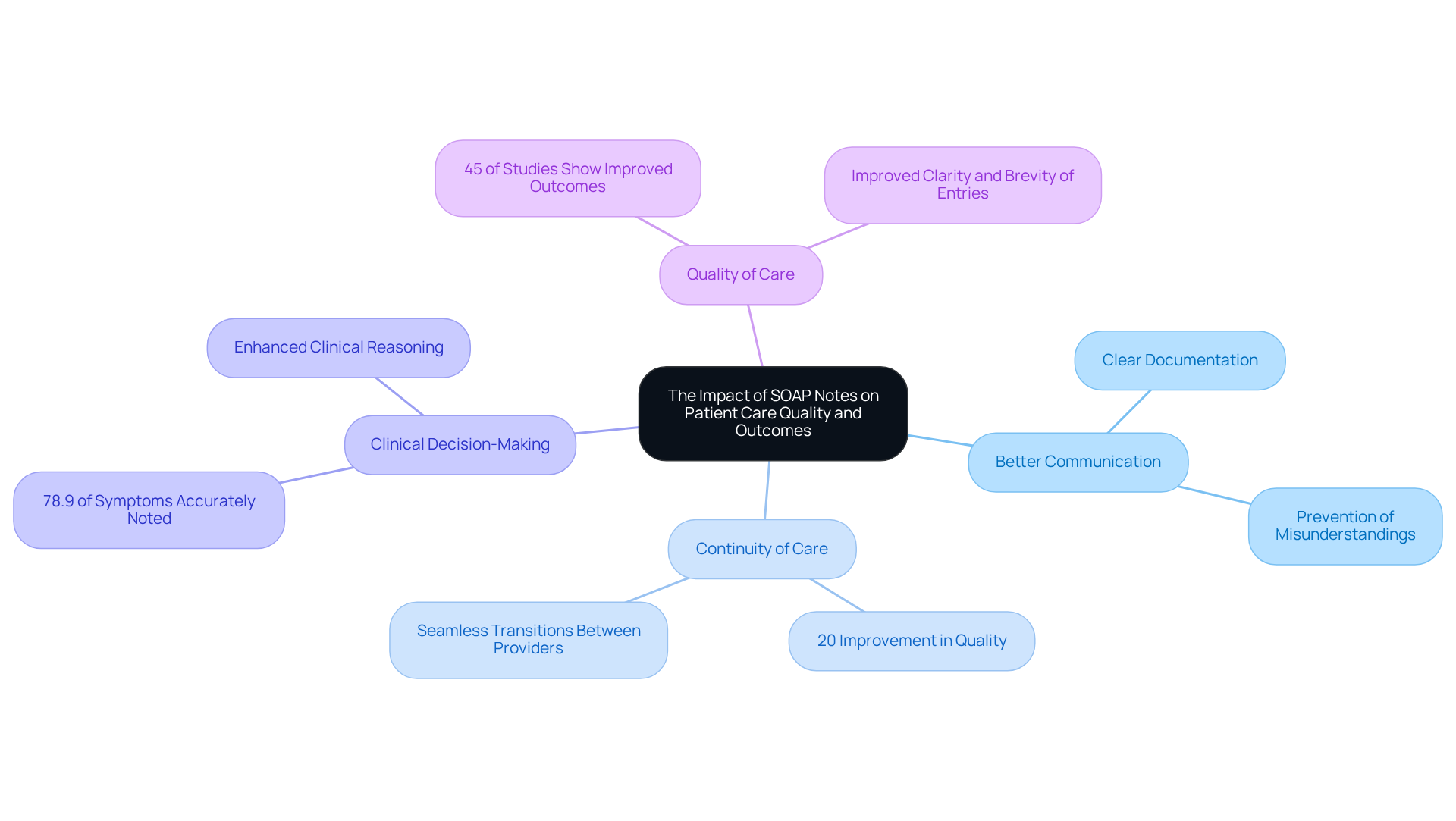
The Impact of SOAP Notes on Patient Care Quality and Outcomes
The caliber of clinical documentation is crucial in influencing healthcare results, particularly when addressing the emotional and practical challenges faced by healthcare providers. Creative AI solutions, like CosmaNeura's Agentic Platform, can significantly alleviate administrative burdens, allowing providers to focus more on patient care. By simplifying record-keeping tasks, these innovations enhance the quality of soap notes samples, resulting in better outcomes for everyone involved.
- Facilitate Better Communication: Have you ever felt the strain of miscommunication in patient care? Clear documentation ensures that all healthcare providers involved in a patient's care are informed and can collaborate effectively. This clarity is vital in preventing misunderstandings that could lead to negative outcomes for individuals.
- Enhance Continuity of Care: Accurate records enable seamless transitions between different care providers, significantly reducing the risk of errors. Research has shown that organized records can lead to a 20% improvement in quality, directly correlating with enhanced patient safety and care continuity.
- Support Clinical Decision-Making: SOAP notes samples provide comprehensive information essential for providers to make informed treatment decisions. Studies indicate that only 78.9% of symptoms are accurately noted, underscoring the need for thorough documentation to enhance clinical reasoning and ultimately improve health outcomes for individuals.
- Impact on Patient Care Quality: Case studies reveal that organized records not only improve the clarity and brevity of entries but also elevate the overall quality of care. For instance, a multicenter study found that adopting organized record-keeping significantly improved clinical notes, leading to better management and outcomes for patients. Additionally, 45% of studies highlighted a statistically significant connection between necessary nursing records and improved patient outcomes, emphasizing the importance of comprehensive record-keeping practices.
- Expert Commentary: Specialists remind us that incomplete or erroneous records can adversely affect patient care, highlighting the necessity for healthcare providers to develop strong record-keeping skills. HyeRin Roh pointed out that deficiencies in record-keeping could lead to legal repercussions, stressing the urgent need for training in this area. Integrating structured documentation models into training programs is essential for nurturing these skills among medical professionals.
In summary, the effective use of soap notes samples, enhanced by innovative AI solutions, is integral to improving communication, continuity of care, and clinical decision-making. These elements are essential for enhancing patient care quality and outcomes. Let’s embrace these tools and practices to foster a more supportive healthcare environment.
Conclusion
The significance of effective SOAP notes in healthcare documentation is profound. Healthcare providers often face emotional challenges, grappling with the weight of administrative tasks that can detract from patient care. By leveraging structured templates and innovative technologies, such as CosmaNeura's AI-powered solutions, these burdens can be alleviated. This allows clinicians to dedicate more time to their patients, nurturing those vital relationships that are at the heart of healthcare.
Throughout this article, we have explored key insights on the structure and best practices for writing SOAP notes, focusing on the essential components of Subjective, Objective, Assessment, and Plan. Effective communication and precise documentation are not just technical requirements; they are foundational for fostering interdisciplinary collaboration, enhancing continuity of care, and ultimately improving healthcare outcomes. We also discussed common pitfalls to avoid and the transformative role of technology in streamlining the documentation process.
As the healthcare landscape evolves, embracing these practices and technologies is crucial for delivering high-quality care. By prioritizing accurate and efficient SOAP note documentation, healthcare professionals can enhance their workflows and contribute to better health outcomes for their patients. It is essential for providers to stay informed and adapt to these advancements, ensuring that patient care remains at the forefront of their efforts.
In summary, consider these key steps:
- Embrace structured templates for clarity.
- Utilize technology to reduce administrative burdens.
- Focus on effective communication for better collaboration.
By taking these actions, you can not only improve your documentation practices but also enrich the care you provide. Let us continue to prioritize the emotional and physical well-being of our patients, ensuring they receive the compassionate care they deserve.




