Overview
This article addresses the emotional challenges that healthcare providers face daily. It provides essential examples of SOAP notes, highlighting their significance in effectively documenting patient care. Have you ever felt overwhelmed by the administrative tasks that take time away from your patients? Structured SOAP notes can alleviate some of that burden.
By illustrating how these notes enhance communication among healthcare professionals, we can see how they improve treatment outcomes. Imagine a world where you can focus more on patient care rather than paperwork. The benefits of using structured SOAP notes are clear: they not only streamline documentation but also foster collaboration among providers.
Ultimately, we encourage you to consider integrating structured SOAP notes into your practice. By doing so, you can enhance your ability to provide compassionate care while reducing the stress of administrative tasks. Let’s work together towards a more efficient and patient-centered approach to healthcare.
Introduction
In the intricate landscape of healthcare, the administrative demands placed on providers can often overshadow the core mission of patient care. This reality can be overwhelming, as the pressure to document effectively mounts. The implementation of effective SOAP notes is not merely a procedural formality; it serves as a vital tool in enhancing communication, ensuring compliance, and ultimately improving treatment outcomes. However, many healthcare professionals grapple with common pitfalls that can compromise the quality of their records.
How can providers navigate these challenges to create precise, compassionate, and efficient documentation that supports both their patients and their practice?
This article explores essential SOAP note examples and best practices tailored for various medical fields. By offering insights that can transform the documentation process into a powerful ally in patient care, we aim to support you in overcoming these hurdles. Together, we can ensure that the focus remains on what truly matters: the well-being of our patients.
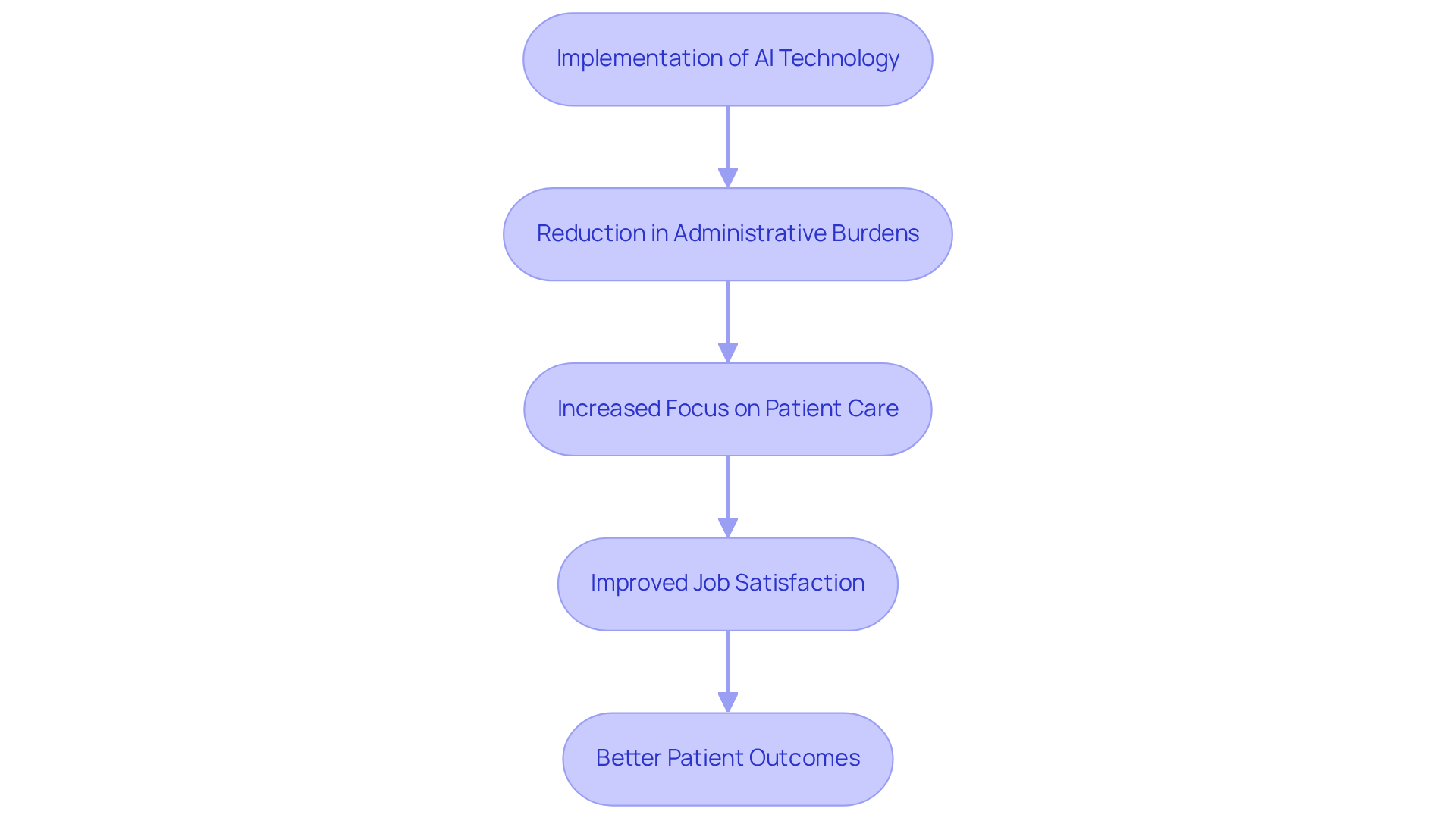
CosmaNeura: AI-Driven SOAP Note Management for Healthcare Providers
Healthcare providers often face overwhelming emotional challenges due to the administrative burdens that come with their roles. CosmaNeura recognizes this struggle and harnesses cutting-edge AI technology to automate the creation and management of a soap.note example. By seamlessly merging client intake, record-keeping, and billing processes, CosmaNeura significantly alleviates these burdens, allowing clinicians to devote more time to what truly matters: supporting their clients.
Imagine a world where healthcare providers can focus on patient care rather than paperwork. This AI-driven methodology not only boosts operational efficiency but also addresses the rising costs of healthcare. By streamlining operations and ensuring that documentation complies with ethical standards rooted in Catholic teachings, CosmaNeura helps create a more compassionate healthcare environment.
Moreover, it tackles the adverse feedback loops generated by the gap between direct compensation and insurance, which often leads to postponed care and increased financial pressure on individuals. As a result, healthcare providers can experience greater job satisfaction, ultimately leading to better outcomes for those receiving care.
Case studies reveal that hospitals utilizing AI solutions have noted a 50% decrease in clinical documentation time. This remarkable efficiency enables more concentrated interactions with individuals receiving care, fostering deeper connections. With the global AI healthcare market projected to reach $238.5 billion by 2032, the demand for such innovative solutions is growing rapidly.
In light of these developments, it’s essential for healthcare settings to adopt AI technologies. By doing so, we can alleviate physician burnout and enhance overall care quality. Are you ready to embrace the future of healthcare with compassion and efficiency?
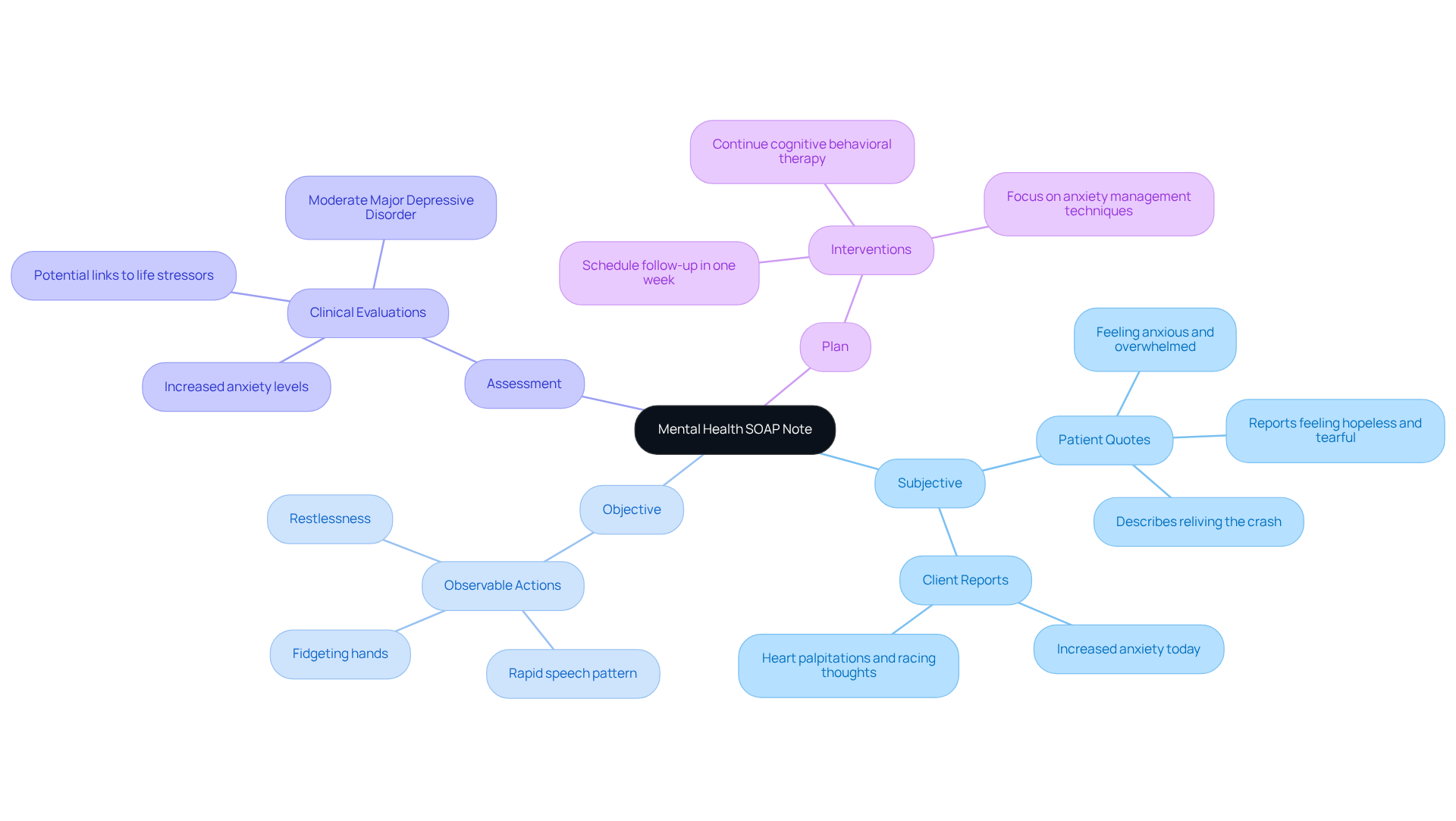
Mental Health SOAP Note Example: Best Practices for Documentation
In mental health environments, SOAP records serve as a vital tool for documenting a patient's personal experiences, observable actions, and clinical evaluations. Have you ever considered how these records can impact patient care? For instance, a well-structured mental health SOAP note might include:
- Subjective: "Patient reports feeling anxious and overwhelmed, stating, 'I can't seem to relax.'"
- Objective: "Patient appears restless, exhibiting a rapid speech pattern and fidgeting hands."
- Assessment: "Increased anxiety levels noted, potentially linked to recent life stressors."
- Plan: "Continue cognitive behavioral therapy sessions, focusing on anxiety management techniques. Schedule a follow-up in one week."
Following these best practices not only ensures thorough and compassionate records but also aligns with mental health reporting standards, which underline the importance of subjective information. Have you thought about how precise documentation can significantly influence treatment results? It enables clinicians to monitor symptom progression and adjust treatment plans effectively. Moreover, utilizing standardized soap.note example templates can enhance communication among healthcare professionals, ultimately leading to better care for individuals. Let's work together to ensure our documentation reflects the empathy and understanding our patients deserve.
Physical Therapy SOAP Note Example: Tailoring Documentation to Patient Needs
In physical therapy, it’s essential to recognize the unique emotional and physical challenges that each patient faces. Tailoring the SOAP note example records to reflect individual needs and progress not only addresses these concerns but also enhances the care provided. For example, consider how a well-structured SOAP note can make a difference:
- Subjective: "Patient reports pain in the right knee, rating it a 7 out of 10 during activity."
- Objective: "Range of motion in the right knee is limited to 90 degrees; swelling observed as noted in the soap.note example."
- Assessment: "Knee pain likely due to post-surgical recovery; further evaluation needed to adjust the soap.note example therapy plan."
- Plan: "Increase therapy frequency to twice a week, focusing on strengthening exercises and range of motion activities. Reassess in two weeks."
This thoughtful approach ensures that records remain relevant and actionable. It aligns with best practices that highlight the importance of objective data in monitoring outcomes for individuals. Have you considered how efficient record-keeping can positively impact patient management and service quality? Research indicates that such practices can significantly boost recovery rates and enhance patient satisfaction.
By incorporating specific, measurable observations, healthcare providers can foster better communication among team members and ensure continuity of care. This not only supports patients in their recovery journey but also alleviates some of the administrative burdens that can weigh heavily on providers. Together, let’s strive for a system that prioritizes compassionate care and effective communication.
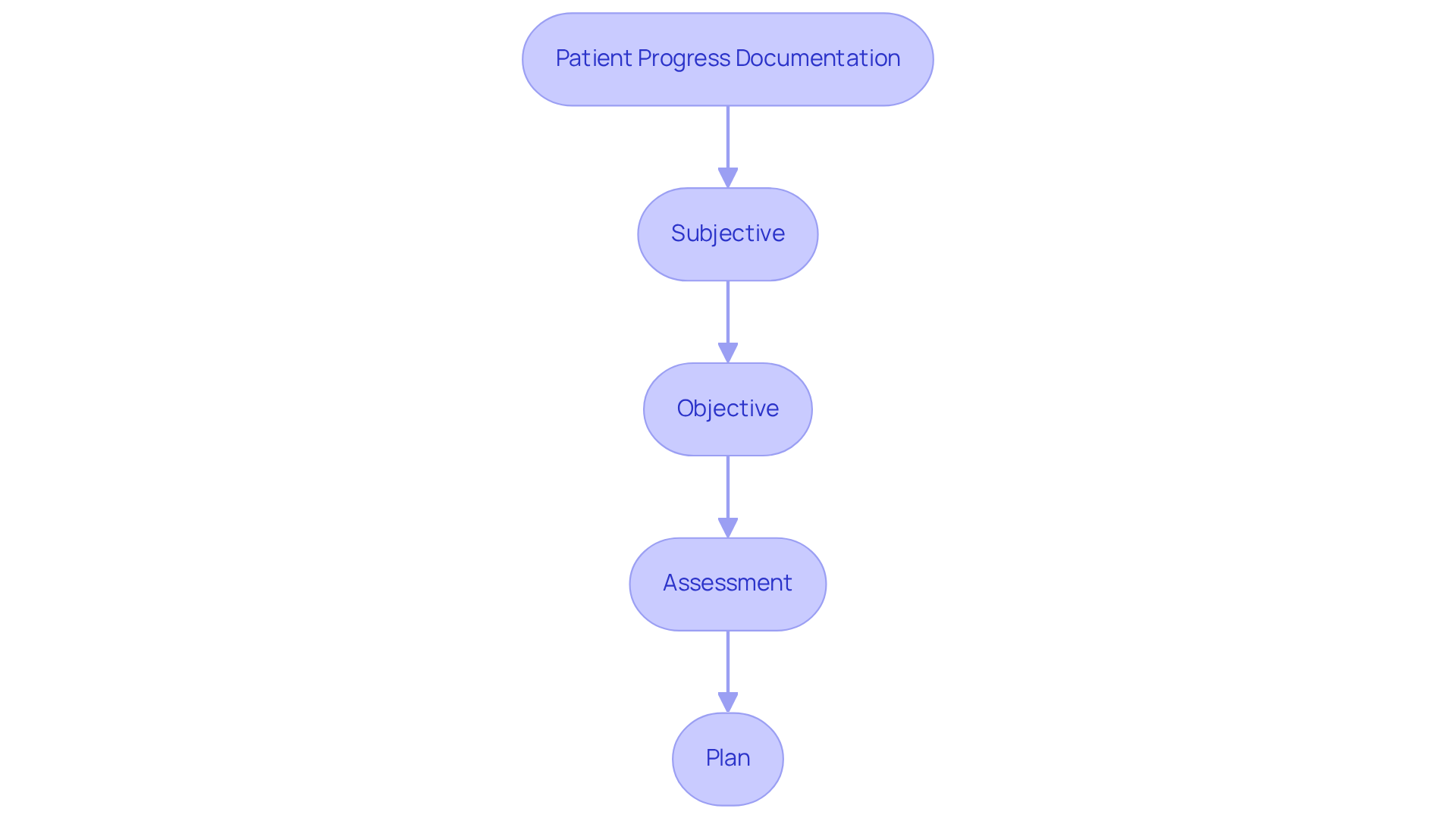
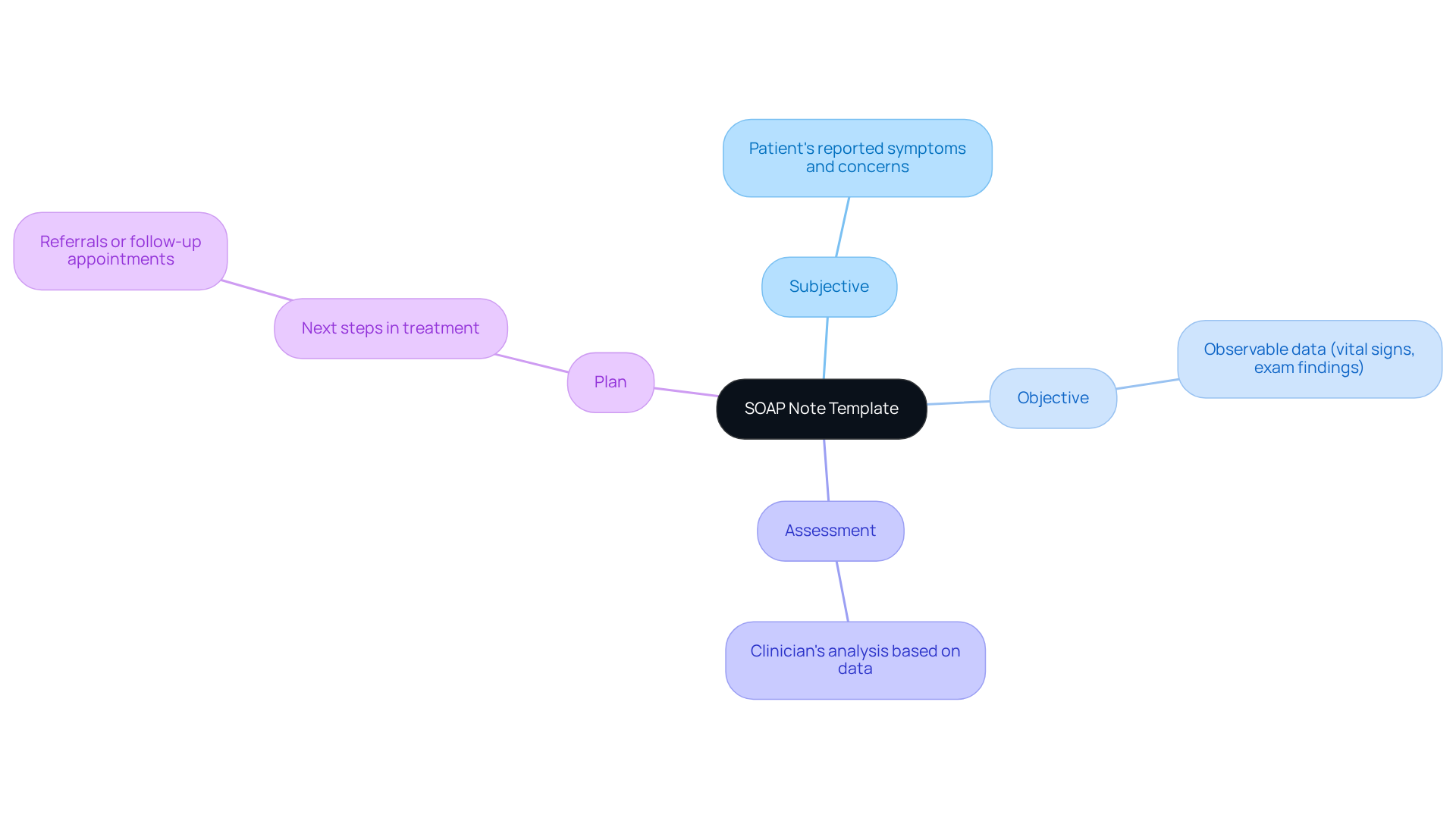
SOAP Note Template: Streamlining Documentation for Efficiency
In the demanding world of healthcare, providers often face emotional challenges that can weigh heavily on their ability to deliver quality care. A standardized soap.note example template can significantly alleviate some of these burdens, enhancing record-keeping efficiency. Here’s a simple template to consider:
- Subjective: Patient's reported symptoms and concerns.
- Objective: Observable data, such as vital signs and physical exam findings.
- Assessment: Clinician's analysis based on subjective and objective data.
- Plan: Next steps in treatment, including referrals or follow-up appointments.
Using this soap.note example enables healthcare providers to swiftly and precisely record client interactions, ensuring that all essential information is captured. Have you ever felt overwhelmed by the volume of paperwork? Research shows that organized records can lead to a remarkable 70% decrease in charting time, as seen in practices that have embraced such templates. Moreover, uniform records enhance clarity and brevity, ultimately improving the quality of care for individuals.
By simplifying the documentation process, providers can focus more on meaningful client interactions rather than administrative tasks. This shift not only fosters a more efficient healthcare environment but also nurtures the compassionate care that patients deserve. Embracing these tools can help you reclaim valuable time and enhance your connection with those you serve.
Subjective Component in SOAP Notes: Capturing Patient Voices
The subjective component of SOAP notes is vital for capturing the individual's perspective, offering a deeper understanding of their experiences and emotions. This section should include direct quotes from individuals, reflecting their feelings about their conditions. For instance, when someone expresses, 'I feel like my anxiety is getting worse, and I can't sleep at night,' it not only illuminates their experience but also empowers clinicians to tailor their evaluations and treatment strategies more effectively.
Recent research highlights that including individual perspectives in healthcare records can significantly enhance engagement. A study analyzing electronic health records found that quoted text is more prevalent among inpatients and individuals from diverse ethnic backgrounds. This underscores the necessity for clinicians to focus on capturing these voices. Additionally, healthcare professionals have noted that recording personal experiences fosters a more empathetic approach to support, as it promotes a deeper understanding of the individual's journey.
Statistics reveal that when healthcare providers actively involve individuals in their documentation, it leads to improved outcomes and satisfaction. By emphasizing the personal experiences of individuals in SOAP note examples, providers can ensure that care is not only clinically sound but also compassionate and aligned with the individuals' needs.
Incorporating these elements into practice can transform patient care:
- Enhance patient engagement
- Foster empathetic support
- Improve overall satisfaction
By prioritizing the voices of individuals, we can create a healthcare environment that truly understands and addresses their needs.

Objective Data in SOAP Notes: Importance of Accurate Clinical Information
In the world of healthcare, we understand the emotional challenges you face while striving to provide the best care for your clients. The objective section of the soap.note example records plays a crucial role in this journey. It should encompass quantifiable and visible information gathered during your interactions with clients. This includes vital signs, physical examination findings, and results from diagnostic tests.
Consider this:
- Blood pressure at 120/80 mmHg
- A heart rate of 72 bpm
- Physical exam findings that reveal tenderness in the lower back
These details are not just numbers; they are essential pieces of the puzzle that help evaluate an individual's condition and guide treatment choices. By focusing on accurate objective data, you can utilize a soap.note example to empower yourself to make informed decisions that truly benefit your clients.
Let’s reflect on how this data can alleviate some of the administrative burdens you encounter. When you have clear, objective information at your fingertips, it can enhance your confidence in the care you provide. We encourage you to prioritize gathering this data, as it not only supports your clinical decisions but also fosters a deeper connection with your clients, ensuring they feel understood and cared for.

Assessment in SOAP Notes: Analyzing Patient Information for Better Outcomes
The assessment segment of a soap.note example plays a vital role in weaving together information from both subjective and objective elements, allowing for a comprehensive evaluation of an individual's condition. Have you ever considered how much clarity a well-structured assessment can bring? For instance, an effective evaluation in the soap.note example could state:
"Assessment indicates that the individual is experiencing acute lower back pain likely due to muscle strain, with no signs of neurological deficits."
This thorough examination is essential for crafting an effective treatment strategy that truly meets the individual's specific needs.
By integrating insights from the individual's reported experiences alongside observable clinical data, healthcare providers can significantly enhance the accuracy of their evaluations. This ultimately leads to improved treatment effectiveness and outcomes, fostering a better experience for both the patient and the provider. It’s important to recognize that the quality of soap.note example may vary among providers, highlighting the need for uniform recording practices.
Using the patient's own words in the subjective section can offer a more authentic representation of their experiences. Furthermore, the soap.note example fulfills critical legal and insurance requirements, making comprehensive evaluations even more essential. Writing SOAP records immediately after a session helps capture pertinent information while it is still fresh, ensuring precision and thoroughness.
Research indicates that organized documentation not only improves the quality of records but also reduces the time spent on documentation. By prioritizing clarity and consistency in your SOAP notes, you can alleviate some of the administrative burdens that often distract from patient care, allowing you to focus on what truly matters—your patients.

Plan in SOAP Notes: Developing Effective Patient Care Strategies
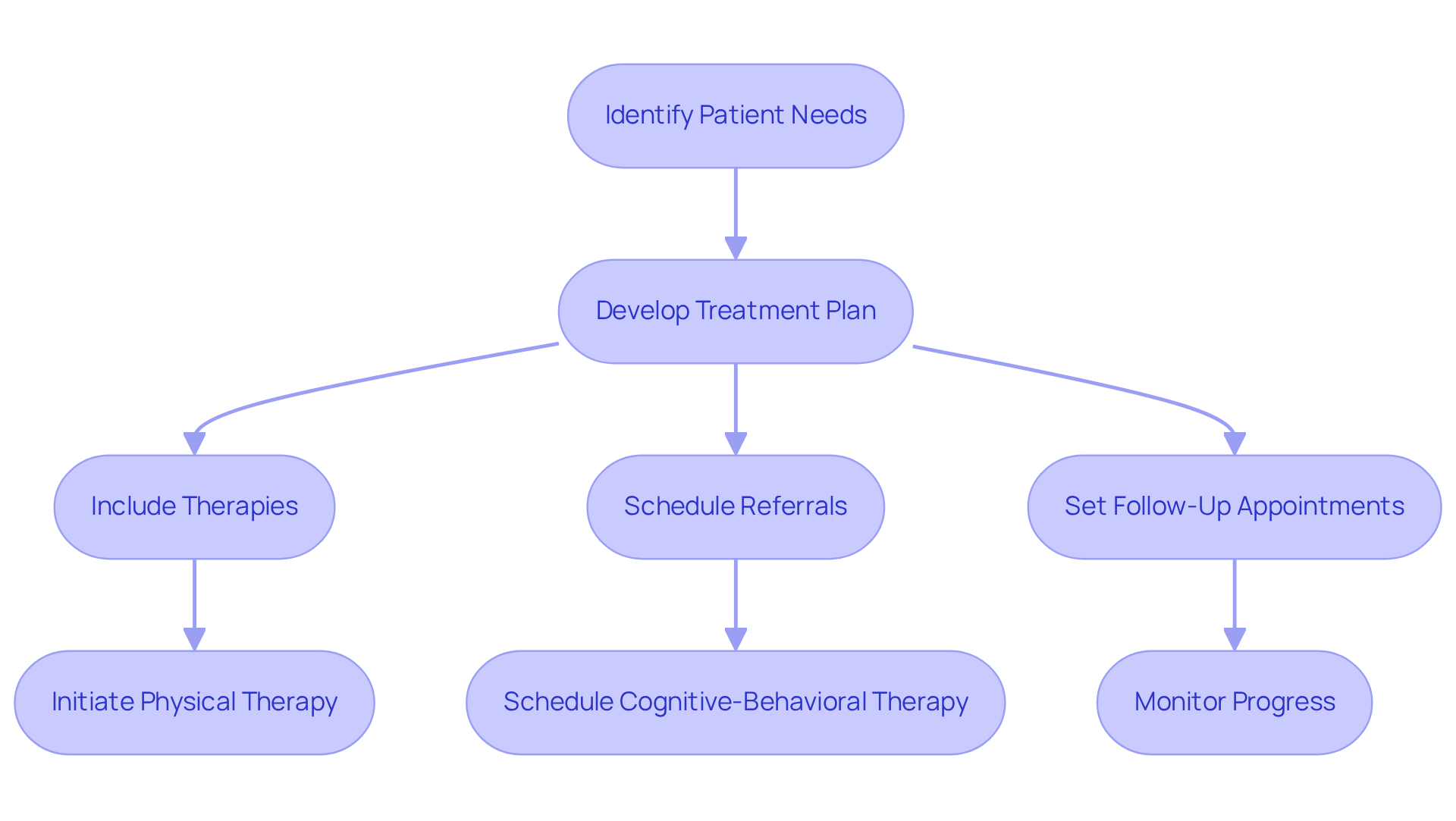
The plan segment of a soap.note example is vital for outlining the next steps in an individual's treatment, encompassing therapies, referrals, and follow-up appointments. For example, a clear plan may specify: "Initiate physical therapy twice a week for the next month, with a follow-up appointment scheduled in four weeks to reassess progress." This clarity in planning is essential, as it ensures individuals receive the support they need for their recovery.
Efficient treatment planning is supported by data showing that organized record-keeping significantly enhances individual outcomes. Research reveals that clear planning in healthcare documentation improves communication among providers, ensuring continuity of service and reducing the risk of errors. Additionally, incorporating SMART goals—Specific, Measurable, Achievable, Relevant, and Time-bound—into the plan can further enhance treatment objectives, allowing for better tracking of individual progress. For instance, a SMART goal might aim to reduce panic attacks from 4 per week to 1 per week within 3 months.
Effective care strategies, as highlighted in a soap.note example, often underscore the importance of careful planning. An individual with anxiety, for instance, might have a plan that includes cognitive-behavioral therapy sessions, medication evaluation, and lifestyle modifications, all tailored to their unique needs. This structured approach not only facilitates effective treatment but also nurtures a collaborative environment between healthcare providers and patients.
Recent discussions in healthcare highlight the need for clear planning in documentation. As medical records evolve into electronic formats, it becomes increasingly crucial to present clinically relevant data in an organized manner, with the soap.note example serving as a valuable tool for achieving this goal. By leveraging innovative AI solutions, such as those offered by CosmaNeura's Agentic Platform, healthcare providers can streamline administrative tasks and enhance the clarity of their planning processes. Dr. Salwa Zeineddine emphasizes that effective planning significantly impacts individuals' lives, underscoring the importance of clarity and structure in the plan section. By prioritizing these elements, healthcare providers can enhance the quality of service provided to those they assist.
Common SOAP Note Mistakes: Avoiding Pitfalls in Documentation
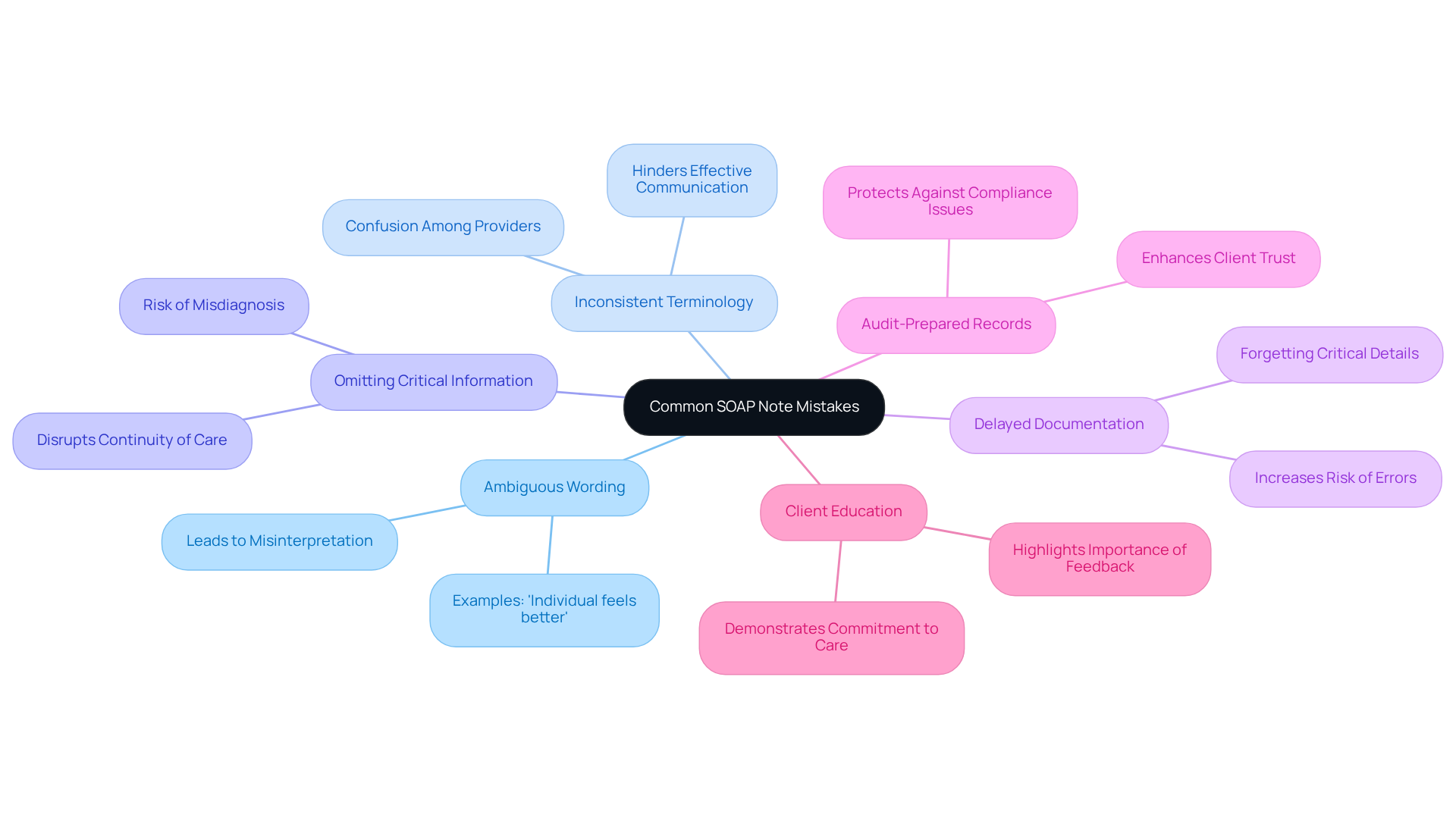
Frequent errors in the soap.note example records can deeply impact client treatment outcomes, leaving healthcare providers feeling overwhelmed. Have you ever experienced the frustration of ambiguous wording? General statements like 'individual feels better' can lead to misinterpretation of a client's condition. Instead, using direct quotes and detailed descriptions can significantly enhance clarity.
Inconsistent terminology is another common pitfall. Without standardized terms, confusion can arise among healthcare providers, hindering effective communication. By using consistent terminology throughout records, we can ensure that all members of the patient support team are aligned, fostering a collaborative environment.
Omitting critical information is a serious concern. Leaving out essential details—such as vital signs or patient-reported symptoms—can disrupt continuity of care, potentially leading to misdiagnosis or inappropriate treatment. Thorough records are vital for informed decision-making, ensuring that every aspect of patient care is addressed.
Have you ever found yourself composing notes long after the encounter? Postponed records increase the risk of errors and overlooked specifics. Prompt updates are crucial for preserving the integrity of medical records, ensuring that every detail is captured accurately.
Furthermore, audit-prepared records are essential. Ensuring that records are thorough and compliant protects against potential audit issues, safeguarding both practice revenue and client coverage. This diligence not only benefits the practice but also enhances client trust.
Lastly, consider the importance of client education. Recording client feedback or inquiries demonstrates a commitment to knowledgeable client support, highlighting the significance of thorough record-keeping practices. By recognizing and addressing these pitfalls, healthcare providers can significantly enhance the quality of their documentation, as illustrated by a soap.note example, ultimately leading to better patient care.
Allocating specific time after consultations to gather new insights can further enhance the completeness and practicality of records. Together, let’s strive for excellence in our documentation practices, ensuring that every client receives the compassionate care they deserve.
SOAP Note Variations: Adapting Documentation for Different Therapy Types
SOAP records can vary significantly depending on the type of therapy being offered, reflecting the unique emotional and practical needs of each context. Consider the following:
- Mental Health: Here, the focus is on emotional and psychological aspects, with detailed subjective reports that truly capture the patient's experience.
- Physical Therapy: This area emphasizes functional progress and measurable outcomes, showcasing the tangible improvements in a patient's abilities.
- Occupational Therapy: In this context, daily living skills and patient engagement in activities are highlighted, supporting a holistic approach to care.
By adapting the soap.note example format to fit the specific context of therapy, providers can not only ensure that documentation is relevant but also enhance its effectiveness, ultimately fostering a deeper connection with patients and improving their care experience.

Conclusion
Healthcare documentation plays a vital role in patient care, profoundly influencing the quality of service delivered. How often do we consider the emotional toll that documentation can take on healthcare providers? By utilizing effective SOAP note examples, providers can streamline their documentation processes, ensuring that patient interactions are recorded with accuracy and compassion. This approach not only alleviates administrative burdens but also enhances the experience for both providers and patients.
The article highlights several key points:
- The importance of AI-driven solutions like CosmaNeura in managing SOAP notes
- The necessity of capturing both subjective and objective data
- The value of tailored documentation for various therapeutic contexts
Each section emphasizes best practices that can lead to improved patient outcomes, greater provider satisfaction, and a more compassionate healthcare environment. By adopting standardized templates and avoiding common pitfalls in documentation, healthcare professionals can foster better communication and continuity of care.
Ultimately, embracing efficient documentation practices is not merely about reducing paperwork; it is about prioritizing patient care and enhancing the therapeutic relationship. As the healthcare landscape evolves, integrating innovative solutions will be essential in addressing the challenges providers face. By committing to high-quality documentation, healthcare professionals can ensure that their patients receive the compassionate and effective care they truly deserve.




