Overview
This article addresses the emotional challenges faced by healthcare providers, particularly in the context of documentation and patient care. It provides essential examples of SF 600 SOAP notes, highlighting their significance in alleviating administrative burdens. By utilizing structured SOAP notes, especially the SF 600 format, healthcare professionals can enhance communication and streamline tasks, ultimately improving compliance with medical standards.
Imagine the relief of having a clear and effective documentation process. This not only eases the workload but also fosters better patient outcomes. The benefits of using SF 600 SOAP notes extend beyond mere compliance; they nurture a more compassionate approach to care, allowing providers to focus more on their patients.
As you reflect on your own experiences, consider how structured documentation can transform your practice. We encourage you to explore the SF 600 format further, as it may just be the solution you need to enhance both your efficiency and the quality of care you provide. Together, let’s strive for a healthcare environment where every note contributes to the well-being of our patients.
Introduction
In the fast-paced realm of healthcare, every moment truly counts. Yet, the burden of documentation can weigh heavily on providers, often pulling them away from their primary focus: patient care. This is where the SF 600 SOAP note example becomes essential. It streamlines the documentation process, ensuring compliance and enhancing communication among care teams.
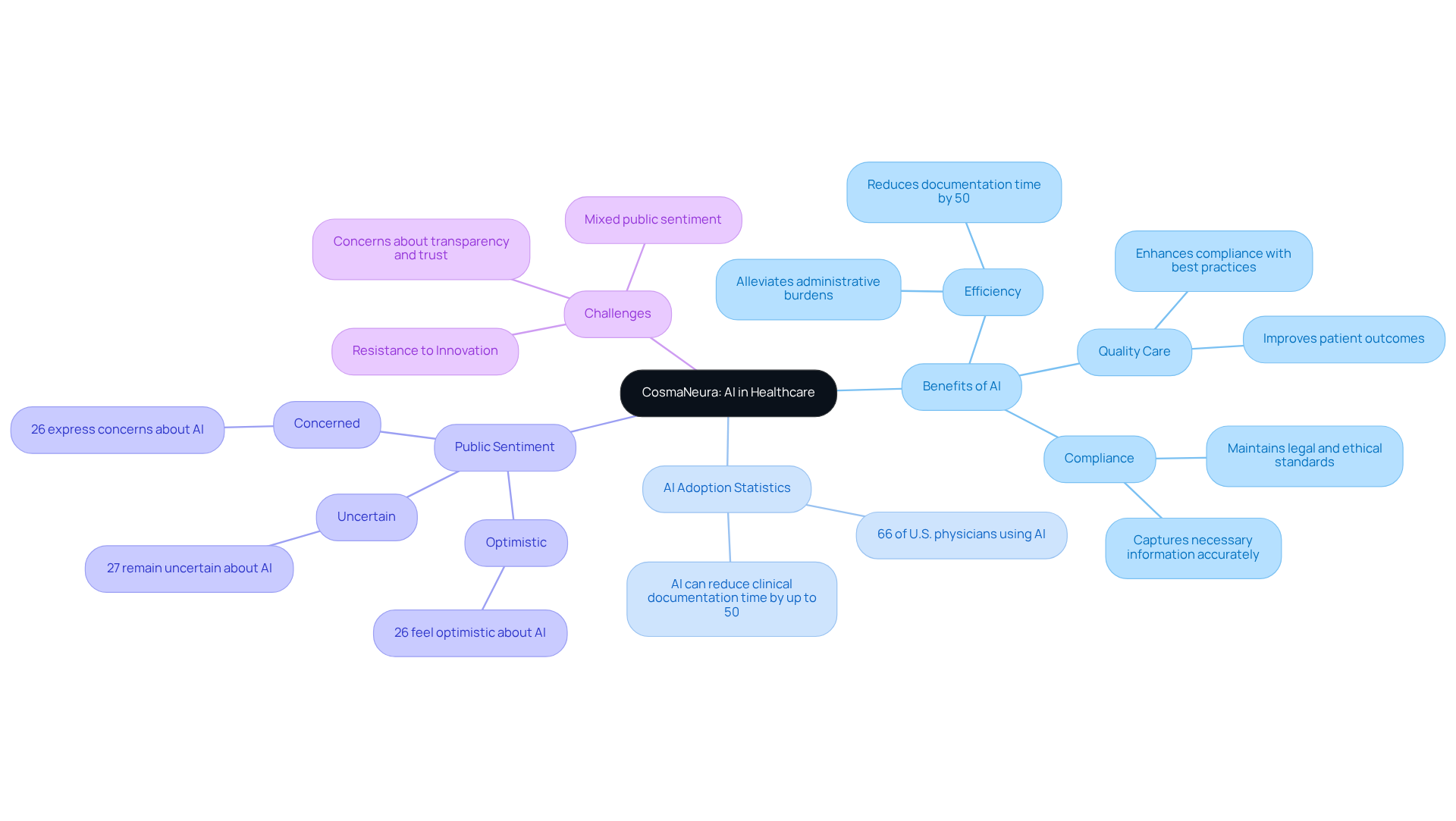
As we witness the growing integration of AI technologies like CosmaNeura, important questions arise:
- How can healthcare professionals navigate the complexities of adopting these innovations while still maintaining the quality of care?
- What strategies can help overcome resistance and ensure that both providers and patients benefit from this evolution in medical documentation?
Reflecting on these challenges is crucial. The emotional toll of administrative burdens can be overwhelming, impacting not just providers but also the patients who rely on their care. By addressing these concerns, we can pave the way for a more supportive and efficient healthcare environment. Together, let’s explore the solutions that can make a difference.
CosmaNeura: Streamline SOAP Note Documentation with AI
In the demanding world of healthcare, providers often face overwhelming administrative burdens that can detract from their primary mission: delivering quality patient care. CosmaNeura's AI platform is here to help. By automating SOAP note management, utilizing an sf 600 soap note example not only simplifies documentation but also addresses the resistance to innovation that is often encountered in medical settings. Traditional accelerators frequently fall short in supporting health startups, leaving providers feeling stuck.
Imagine a solution that allows you to focus on what truly matters—your patients. Utilizing advanced algorithms, CosmaNeura generates precise sf 600 soap note examples in real-time during client interactions. This alleviates concerns about maintaining quality care while integrating new technologies. With this innovation, healthcare professionals can prioritize client care over paperwork, significantly improving efficiency.
Studies show that AI can reduce clinical documentation time by up to 50%. This means reclaiming valuable hours each day, directly addressing the issue of physician burnout caused by overwhelming administrative tasks. The automation of SOAP notes, as demonstrated in the sf 600 soap note example, not only streamlines workflows but also ensures compliance with best practices, ultimately enhancing the quality of care provided to individuals.
Furthermore, the integration of AI helps maintain compliance with legal and ethical standards, capturing all necessary information accurately and promptly. As the medical field continues to embrace AI technologies, the impact on practitioner efficiency is notable. In fact, 66% of U.S. physicians reported using AI tools in 2024, indicating a growing trend towards improved operational effectiveness in clinical environments.
However, it's essential to acknowledge that public sentiment towards AI is mixed. Approximately 26% of individuals feel optimistic about AI, while 27% remain uncertain and another 26% express concerns. This highlights the importance of ongoing conversations about AI's role in medical services, ensuring that both providers and patients can navigate this transformative landscape together. How can we foster a supportive dialogue that addresses these concerns and builds trust in AI solutions?
SF 600 Form: Key Example for Military Healthcare Documentation
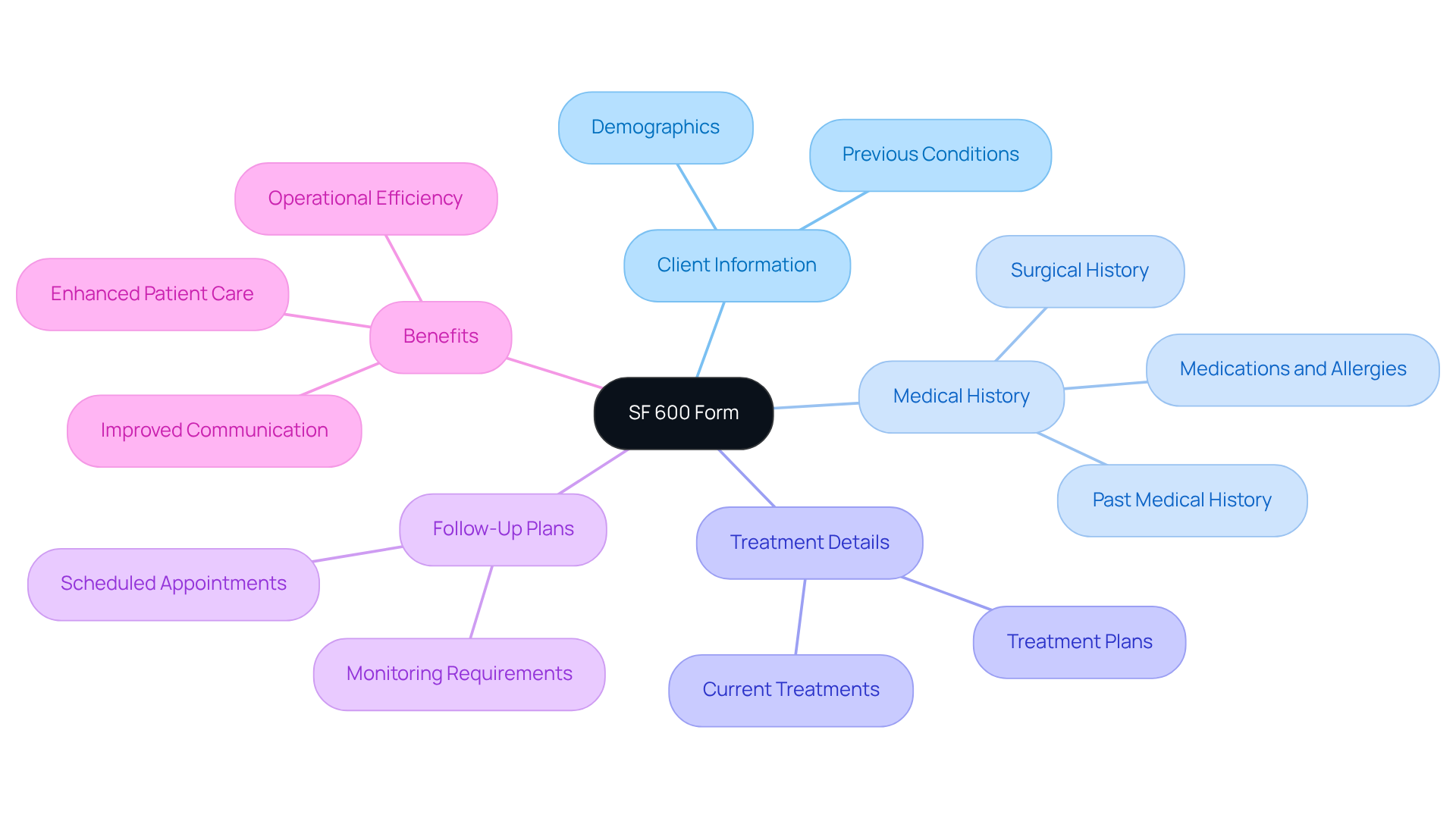
The SF 600 soap note example serves as a crucial tool in military medical environments, aiding in the creation of a chronological record of medical care. Have you ever considered how this form captures essential client information, such as medical history, treatment details, and follow-up plans? Understanding how to effectively utilize the SF 600 soap note example is crucial for medical providers operating in military contexts. It not only ensures adherence to military regulations but also fosters seamless communication among care teams.
Adequate records on the SF 600 soap note example can significantly impact health outcomes by providing a clear and comprehensive medical history. This clarity can alleviate some of the administrative burdens that healthcare providers face, allowing them to focus more on patient care. Recent statistics highlight the widespread use of the SF 600 in military healthcare settings, underscoring its role in maintaining high standards of care and operational efficiency.
As we navigate the complexities of healthcare, let’s remember the importance of effective documentation. By embracing the SF 600, we can enhance our ability to provide compassionate care. Together, we can ensure that our patients receive the attention and support they deserve.
SOAP Note Structure: Essential Framework for Patient Records
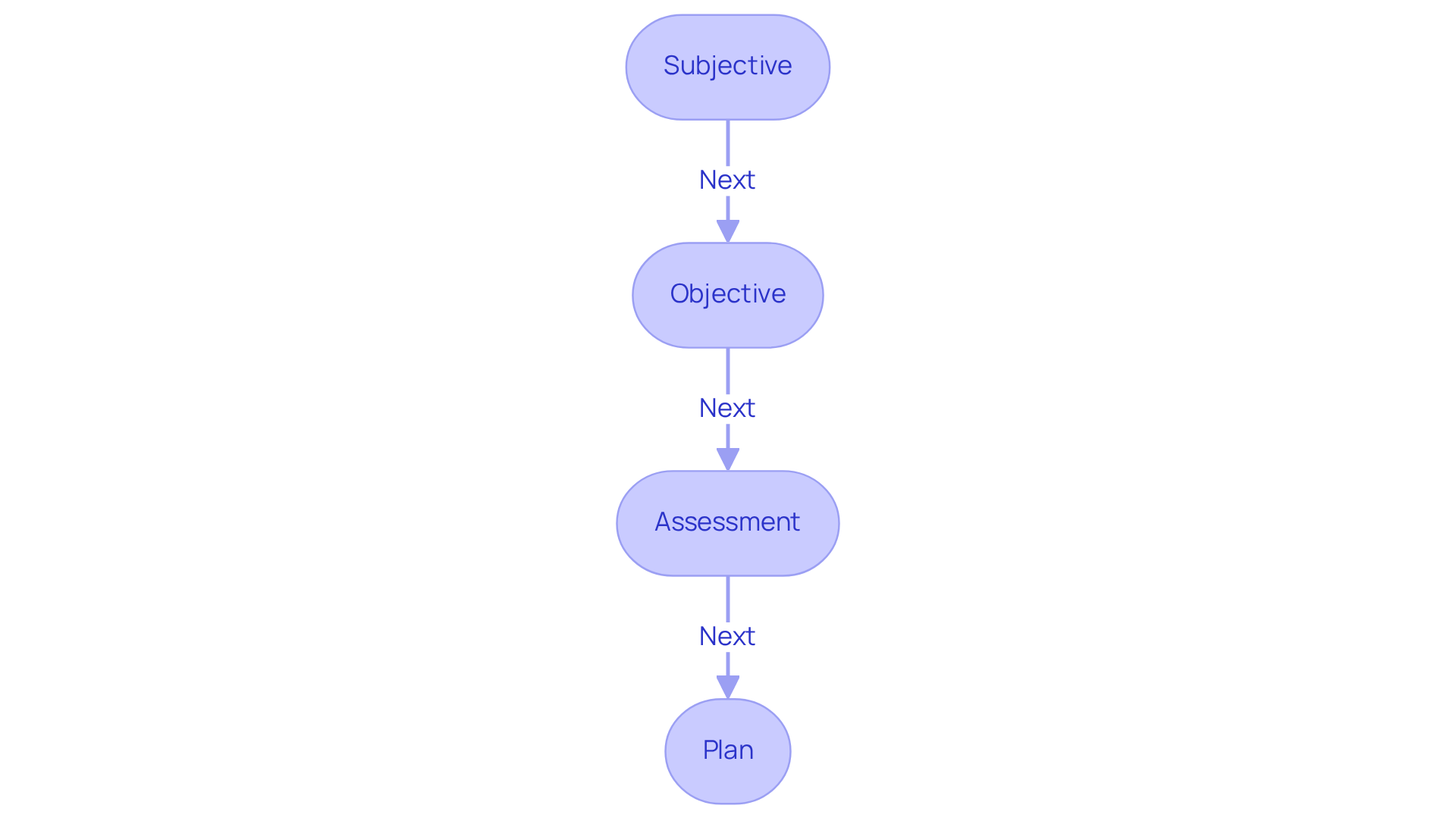
The sf 600 soap note example includes four essential components: Subjective, Objective, Assessment, and Plan. Each serves a unique purpose in patient documentation, such as the sf 600 soap note example, aiming to enhance the overall care experience.
-
Subjective (S): This section captures the patient's perspective, detailing their symptoms, concerns, and medical history as reported by them, as illustrated in the sf 600 soap note example. Understanding the individual's experience is crucial for guiding clinical assessment. Have you considered how generative AI can enhance this section? By utilizing AI-powered tools that analyze patient-reported data, healthcare providers can gain a more comprehensive understanding of patients' needs.
-
Objective (O): In the sf 600 soap note example, observable and measurable data are recorded by medical professionals, including vital signs, physical examination findings, and laboratory results. This objective information is vital for supporting clinical assessments and treatment decisions. Imagine the relief when AI assists in automating the collection and analysis of this data, streamlining documentation and reducing the administrative burden on healthcare providers.
-
Assessment (A): This section involves the clinician's analysis of the individual's condition, synthesizing subjective and objective data as demonstrated in an sf 600 soap note example to arrive at a diagnosis or problem list. AI algorithms can help recognize patterns and trends in health data, enhancing the accuracy of evaluations and guiding treatment plans. How might this technology improve your practice?
-
Plan (P): The sf 600 soap note example includes outlined proposed treatment strategies, follow-up appointments, and necessary referrals. This segment is essential for directing future treatment and ensuring that all medical professionals involved are coordinated in managing the individual. Generative AI can enhance communication among practitioners, ensuring that the plan is effectively shared and comprehended across the care team.
Using the sf 600 soap note example as an organized method not only improves clarity and consistency in records but also promotes effective communication among healthcare professionals, ultimately enhancing care outcomes. As specialists highlight, precise records serve as a safeguard that protects both healthcare providers and patients, ensuring that all pertinent information is readily available for clinical decision-making. Additionally, a study discovered that 80% of clinicians were content or highly content with the APSO format, emphasizing the efficiency of structured records. This historical context, presented by Dr. Larry Weed in the 1960s, underscores the enduring significance of this recording method.
In embracing these strategies, we can alleviate some of the emotional challenges faced in healthcare, fostering a more compassionate and effective environment for both providers and patients.

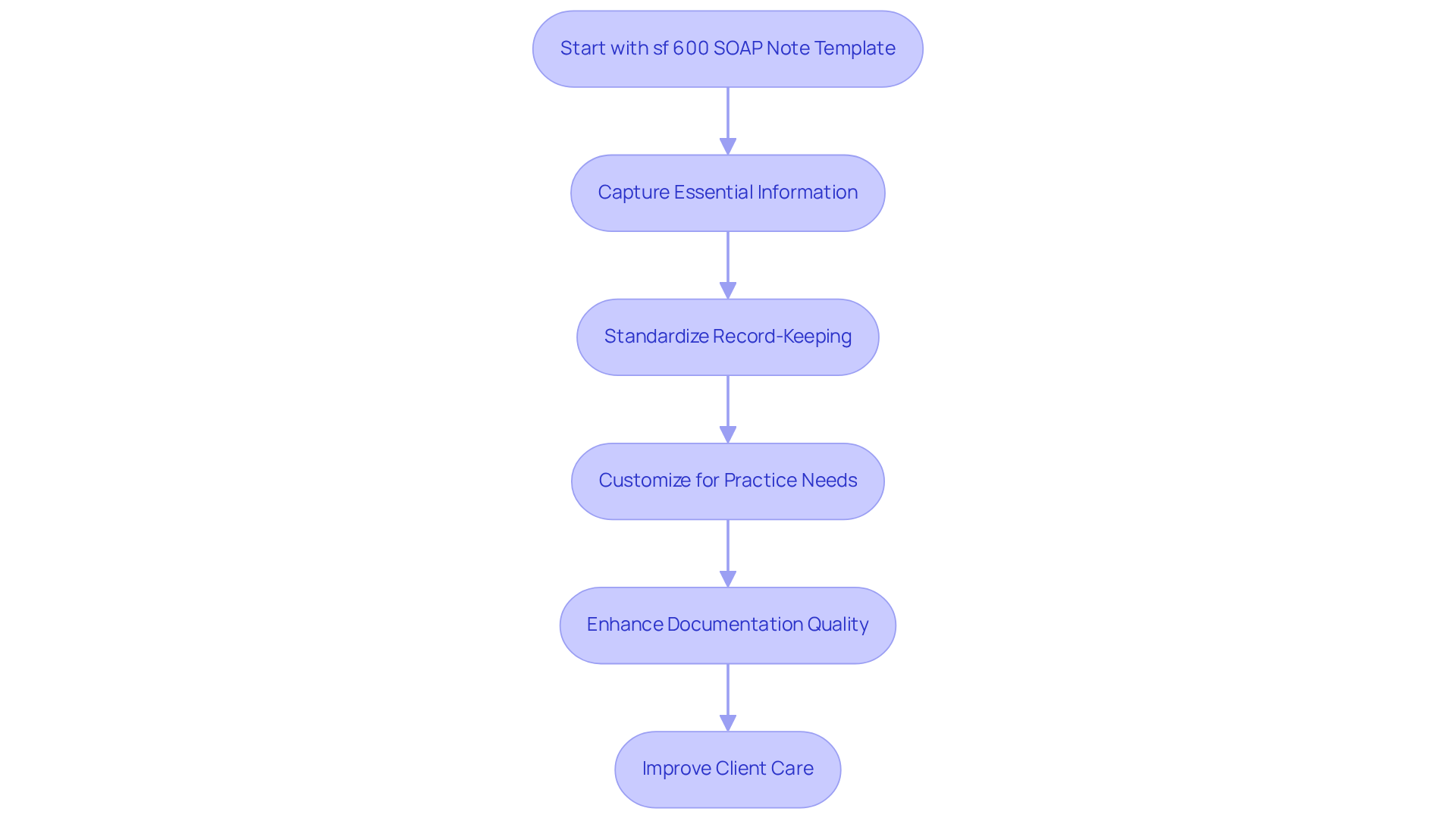
SOAP Note Templates: Enhance Efficiency in Documentation
The use of an sf 600 soap note example can significantly alleviate the stress of record-keeping for healthcare providers. The sf 600 soap note example provides a structured format that helps clinicians capture essential information, reducing the risk of overlooking critical details. By standardizing the record-keeping process, as illustrated in the sf 600 soap note example, they minimize variability and ensure that all relevant data is consistently noted.
Digital platforms, such as CosmaNeura, offer customizable templates like the sf 600 soap note example, tailored to specific practice needs, further streamlining the record-keeping process. This customization allows providers to focus more on client care rather than administrative tasks. Have you ever felt overwhelmed by paperwork? Recent studies show that the sf 600 soap note example, when using structured templates, can lead to remarkable improvements in documentation quality, with compliance rates soaring from 38.2% to 87.2% after adopting standardized practices.
Moreover, the integration of digital tools enhances the efficiency of note-taking, enabling immediate capture and organization of information. Insights from over 40 customer interviews conducted by CosmaNeura between August 2023 and October 2023 have confirmed these challenges in medical administration, highlighting the urgent need for innovative AI solutions to address obstacles in medical delivery. As the healthcare landscape continues to evolve, utilizing an sf 600 soap note example as a customizable template is becoming increasingly vital for improving clinical documentation and enhancing overall client care. Let's explore how these tools can transform your practice and support your dedication to patient well-being.
Real-World SOAP Note Examples: Practical Insights for Providers
Real-world examples, such as the sf 600 soap note example, offer invaluable insights for healthcare providers, especially in moments of stress and uncertainty. Consider a patient presenting with chest pain:
- Subjective: The patient reports a sharp pain in the chest that began two hours ago, accompanied by shortness of breath.
- Objective: Vital signs indicate elevated blood pressure at 150/90 mmHg and a heart rate of 110 bpm. The physical examination reveals mild respiratory distress.
- Assessment: The clinician evaluates the individual as potentially experiencing angina, warranting further evaluation.
- Plan: The plan includes ordering an ECG, administering nitroglycerin, and closely monitoring the individual.
Such examples highlight the necessity of effectively documenting healthcare encounters, which can be illustrated by an sf 600 soap note example. This ensures that all relevant information is captured for ongoing care, which can feel overwhelming at times. Did you know that structured documentation, like SOAP notes, can significantly reduce charting time—up to 70% in some cases? This is evidenced by Priority Physicians' experience with the Heidi platform. By streamlining these processes, providers can focus more on what truly matters: client care.
The SOAP note format, utilized since the 1970s, demonstrates reliability and effectiveness in clinical practice. By embracing these structured formats, medical professionals can enhance communication and continuity of care. This ultimately leads to improved client outcomes, fostering a nurturing environment where patients feel understood and cared for.
Common SOAP Note Mistakes: Avoiding Pitfalls in Documentation
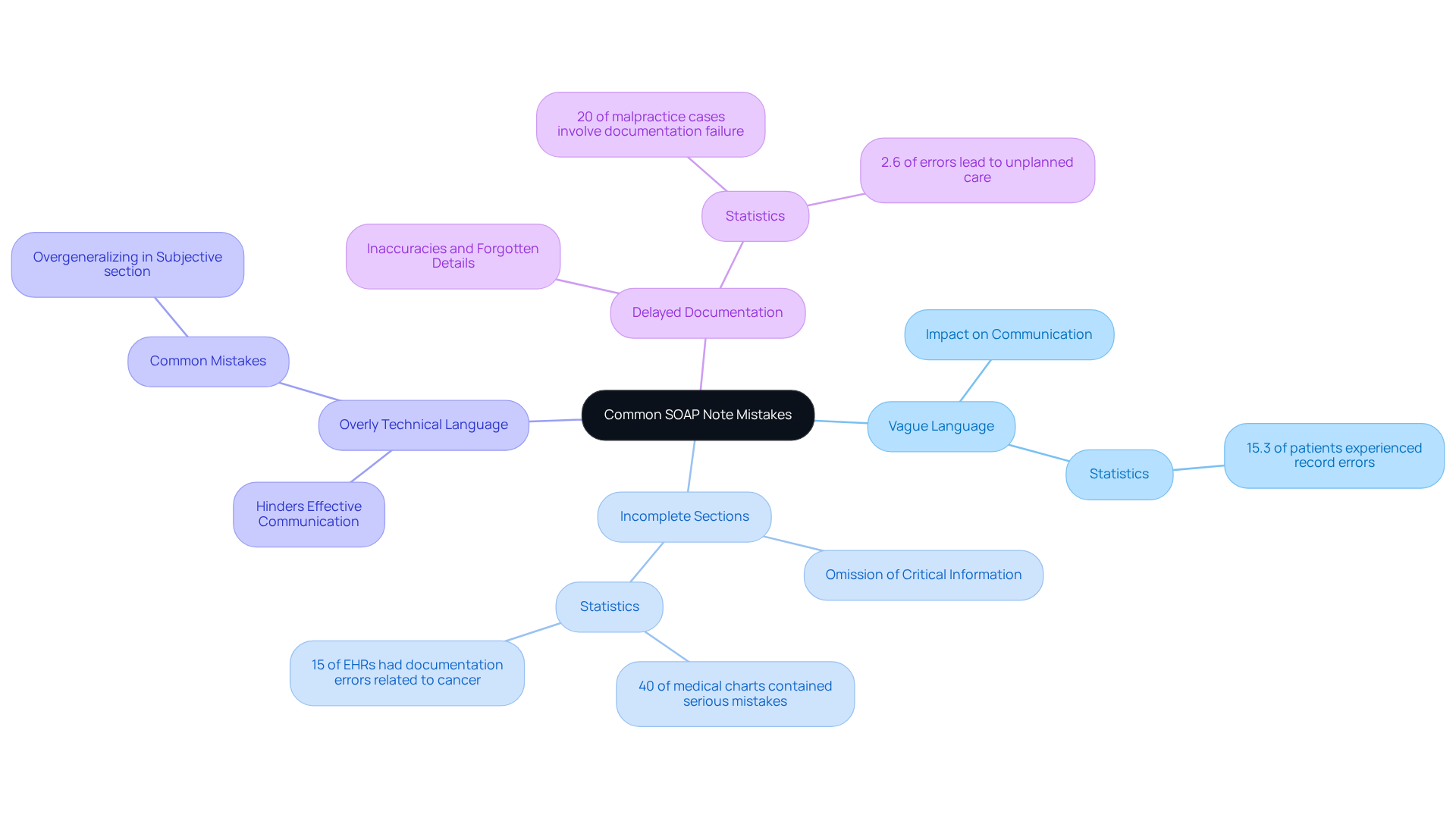
Frequent errors in SOAP note entries can deeply affect the integrity of medical records, posing challenges for healthcare providers. Have you ever felt overwhelmed by the administrative burdens that can distract from patient care? Recognizing these common pitfalls is the first step toward improvement.
- Vague Language: The use of ambiguous terms can lead to misunderstandings and misinterpretations. Specificity is essential; clear descriptions improve communication among healthcare providers and ensure that individual conditions are accurately conveyed. It's concerning to note that 15.3% of individuals experienced at least one record error or inconsistency in their electronic medical files, underscoring the impact of vague language on patient care.
- Incomplete Sections: Omitting critical information from any SOAP component can obscure the individual's condition and treatment plan. For instance, 40% of medical charts contained serious mistakes, while 15% of reviewed electronic health records (EHRs) had documentation errors related to cancer diagnosis and treatments. This highlights the pressing need for comprehensive data collection to support effective patient management.
- Overly Technical Language: Using jargon that may not be universally understood can hinder effective communication within the healthcare team. Standardizing language helps maintain clarity and accessibility, ensuring all team members are aligned. As noted by HealthOrbit AI, "One of the most common mistakes is overgeneralising in the Subjective section, using vague phrases instead of specific patient-reported symptoms or direct quotes."
- Delayed Documentation: Writing notes long after the patient encounter can lead to inaccuracies and forgotten details. Research suggests that record-keeping errors can cause significant medical issues, with 2.6% of these mistakes resulting in unplanned care. Alarmingly, 20% of medical malpractice cases include at least one record-keeping failure. This emphasizes the crucial importance of timely documentation to safeguard both patient outcomes and legal standing. Therefore, documenting as soon as possible after the visit is vital for maintaining accuracy.
By recognizing and addressing these frequent errors, healthcare professionals can significantly enhance the quality of their documentation. This not only leads to better outcomes for individuals but also fosters a sense of professional satisfaction and connection. Together, let’s strive for clearer, more accurate medical records that truly reflect the care we provide.
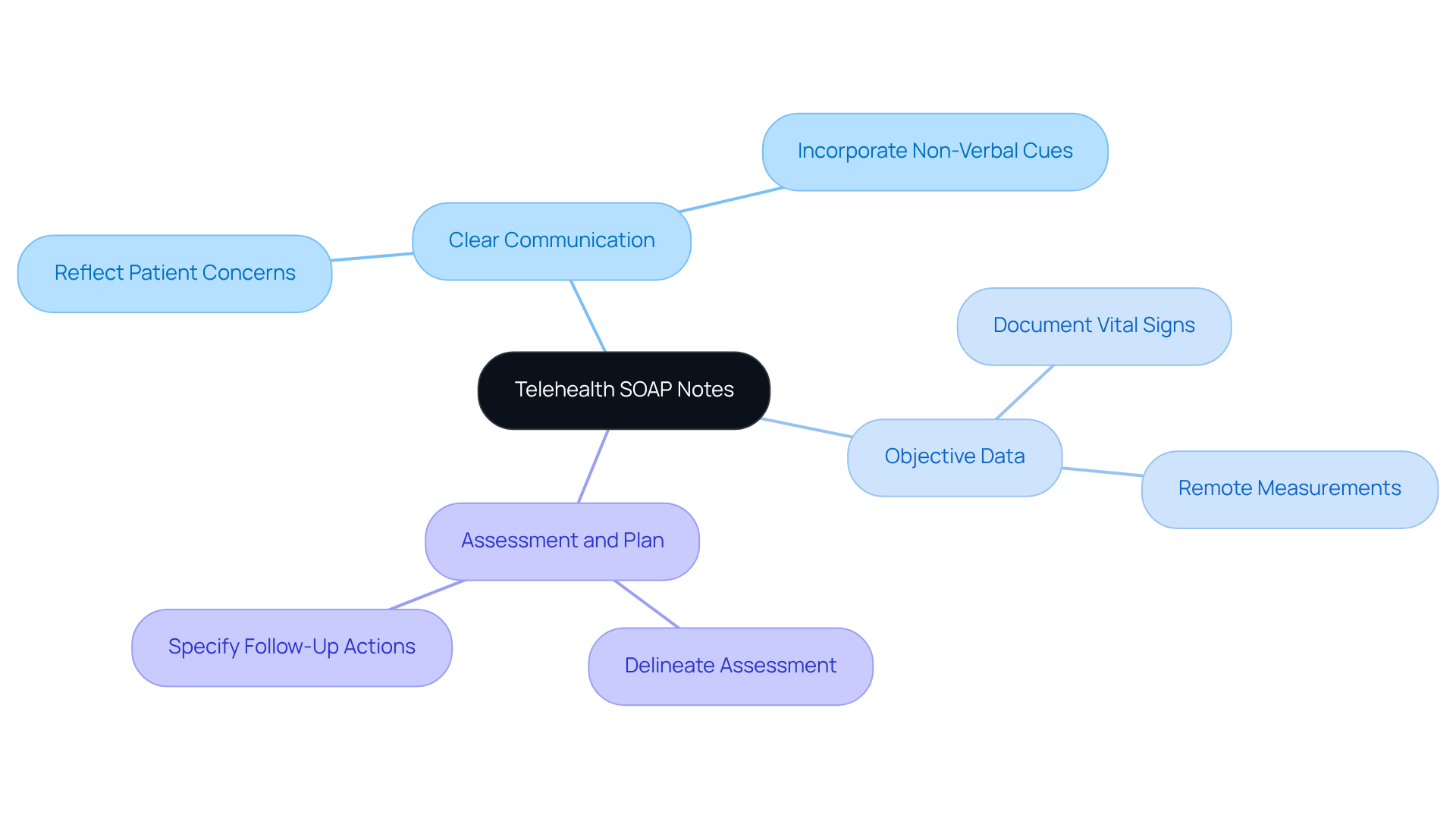
Telehealth SOAP Notes: Adapting Documentation for Remote Care
Telehealth SOAP notes require specific modifications to effectively address the unique dynamics of remote client interactions. It's important to recognize the emotional challenges healthcare providers face in this setting. Key considerations include:
- Clear Communication: The subjective section should accurately reflect the patient's concerns as articulated during the virtual visit. This includes any non-verbal cues that may be discerned through video, allowing for a deeper understanding of their needs.
- Objective Data: Document vital signs or measurements that patients can provide remotely, such as home blood pressure readings or glucose levels. Ensuring accuracy in the clinical record is vital for maintaining trust and continuity of care.
- Assessment and Plan: Clearly delineate the assessment derived from the virtual interaction and specify follow-up actions. This might include referrals for in-person visits when necessary, reinforcing the commitment to comprehensive care.
By customizing SOAP notes for telehealth, providers can maintain strict record-keeping standards while ensuring continuity of care, even in a remote context. This adaptation is crucial, especially as telehealth visits have surged. With a reported 89% increase in telehealth utilization from 2019 to 2020, the need for effective documentation practices in this evolving landscape cannot be overstated. Let’s embrace these changes together, ensuring that we continue to provide compassionate care to our patients, no matter the distance.
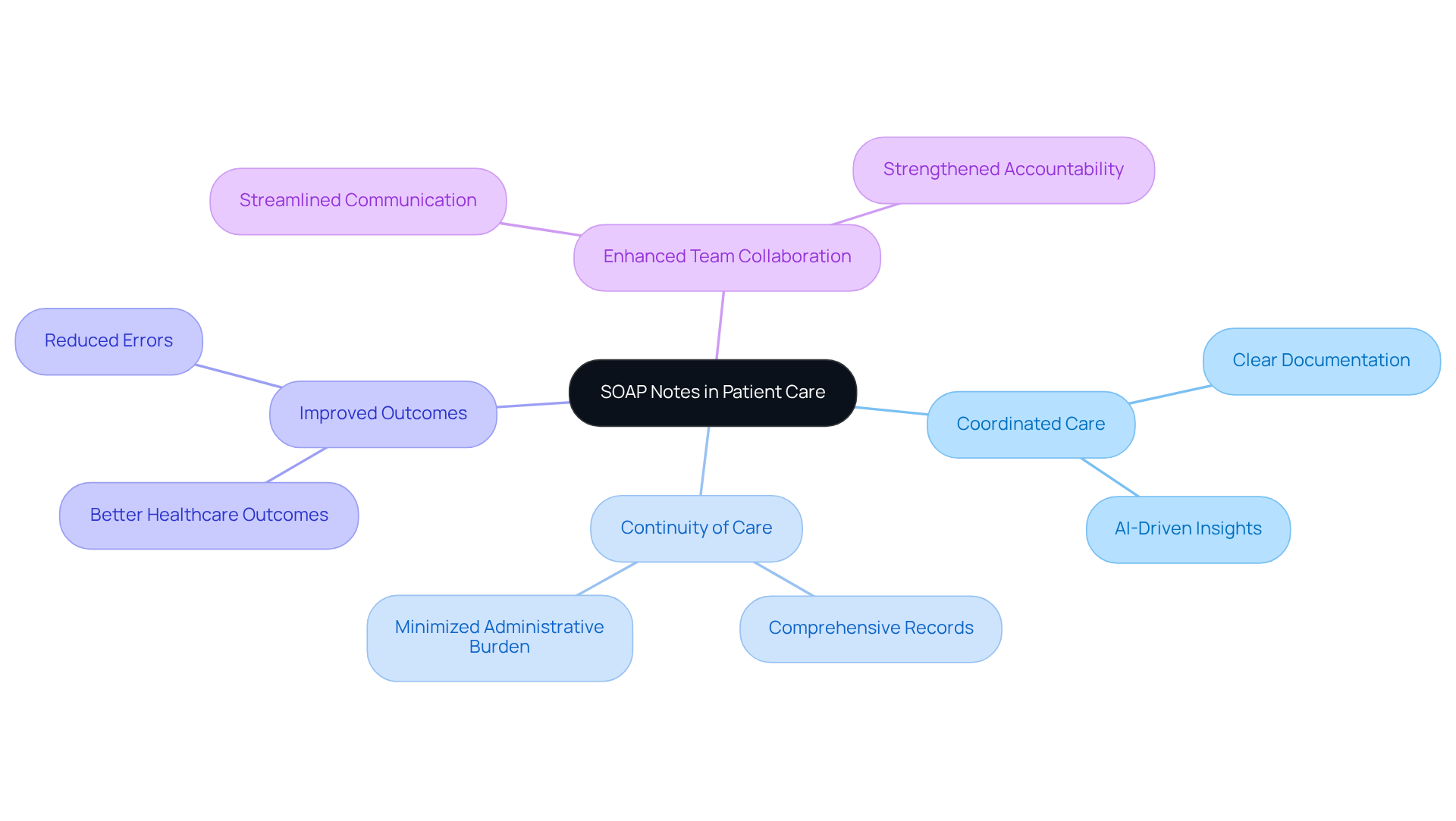
Interdisciplinary Communication: The Role of SOAP Notes in Patient Care
SOAP notes are not just a tool; they are a vital communication lifeline among interdisciplinary healthcare teams, especially when enhanced by innovative AI solutions like CosmaNeura's Agentic Platform. By providing a standardized format for recording client interactions, SOAP notes ensure that all team members have access to the same crucial information. This leads to several key benefits:
- Coordinated Care: Clear documentation, supported by AI-driven insights, allows different providers to grasp the patient's history, current status, and treatment plan, fostering seamless collaboration.
- Continuity of Care: When multiple providers are involved in an individual's care, SOAP notes help maintain a comprehensive record that can be easily shared and referenced. This minimizes the administrative burdens that often hinder effective communication.
- Improved Outcomes: Effective communication through SOAP notes, bolstered by generative AI, can result in better healthcare outcomes. When all team members are informed and aligned in their approach, the potential for success increases. Research shows that organized documentation significantly improves communication clarity, reducing mistakes and enhancing safety during care transitions.
- Enhanced Team Collaboration: By adopting SOAP notes, medical teams can streamline their communication processes, leading to more efficient decision-making and a cohesive approach to care. This organized method reduces misunderstandings and strengthens accountability among team members, ultimately enhancing health and satisfaction. Furthermore, by addressing physician burnout and resistance to innovation, the incorporation of CosmaNeura's solutions paves the way for progress in medical delivery, tackling the challenges practitioners face today.
In a world where healthcare providers are often overwhelmed, embracing these tools can make a significant difference. How might your team benefit from improved communication and collaboration? Let’s explore these solutions together for a brighter, more effective healthcare experience.
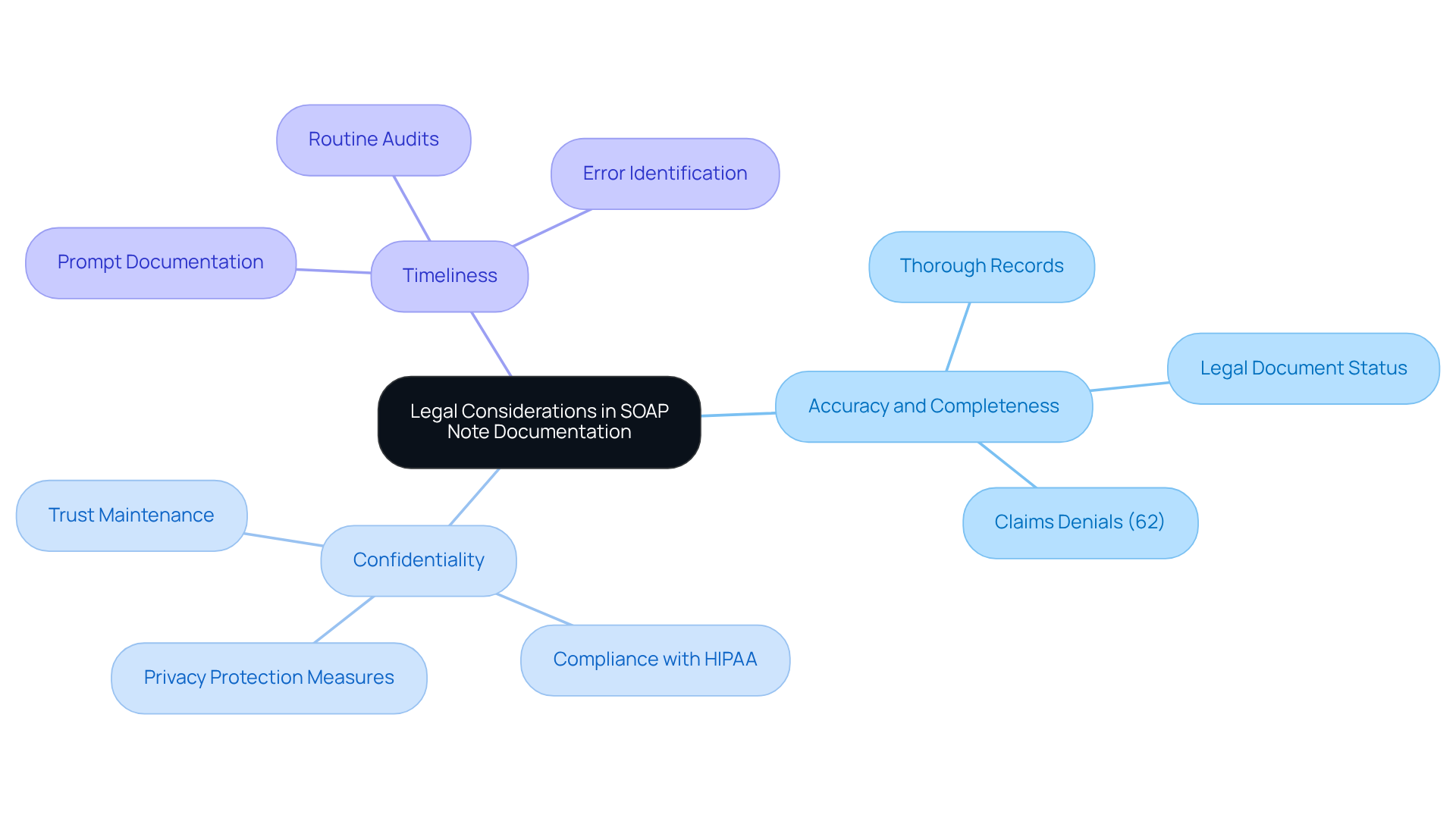
Legal Considerations: Ensuring Compliance in SOAP Note Documentation
SOAP notes are essential not just for compliance, but for the peace of mind they bring to healthcare providers and patients alike. Understanding the emotional challenges that come with legal and regulatory standards is crucial. Key legal considerations include:
- Accuracy and Completeness: It’s vital that SOAP notes are thorough and precise. These records may serve as legal documents in disputes or audits. Insufficient records can lead to claims rejections, with research indicating that 62% of these arise from inadequate data analytics. This highlights the importance of maintaining precise records, such as those in the sf 600 soap note example, to avoid potential financial consequences.
- Confidentiality: Protecting individual privacy is paramount. Providers must ensure that SOAP notes are securely stored and shared only with authorized personnel. This not only safeguards privacy but also helps maintain trust and compliance with regulations like HIPAA.
- Timeliness: Recording patient encounters promptly is essential. Delays can lead to inaccuracies and potential legal ramifications. Routine audits can help identify errors before they escalate, ensuring that records remain precise and compliant, as illustrated in the sf 600 soap note example.
As Mohd Aihatram Khan wisely noted, 'High-quality records enhance organized, uniform, and efficient communication among medical practitioners.' By recognizing and adhering to these legal factors, healthcare professionals can protect their practice and ensure ethical care for individuals. The significance of high-quality records cannot be overstated; they not only support regulatory compliance but also enhance patient outcomes and foster trust between caregivers and patients. Moreover, case studies like the 'Impact of Claims Denials' illustrate the real-world consequences of inadequate record-keeping practices, underscoring the need for diligence in this area.
Let’s embrace the journey towards better documentation together. By committing to these practices, we can alleviate administrative burdens and focus more on what truly matters—providing compassionate care for our patients.
Continuous Improvement: Evolving SOAP Note Practices for Better Care
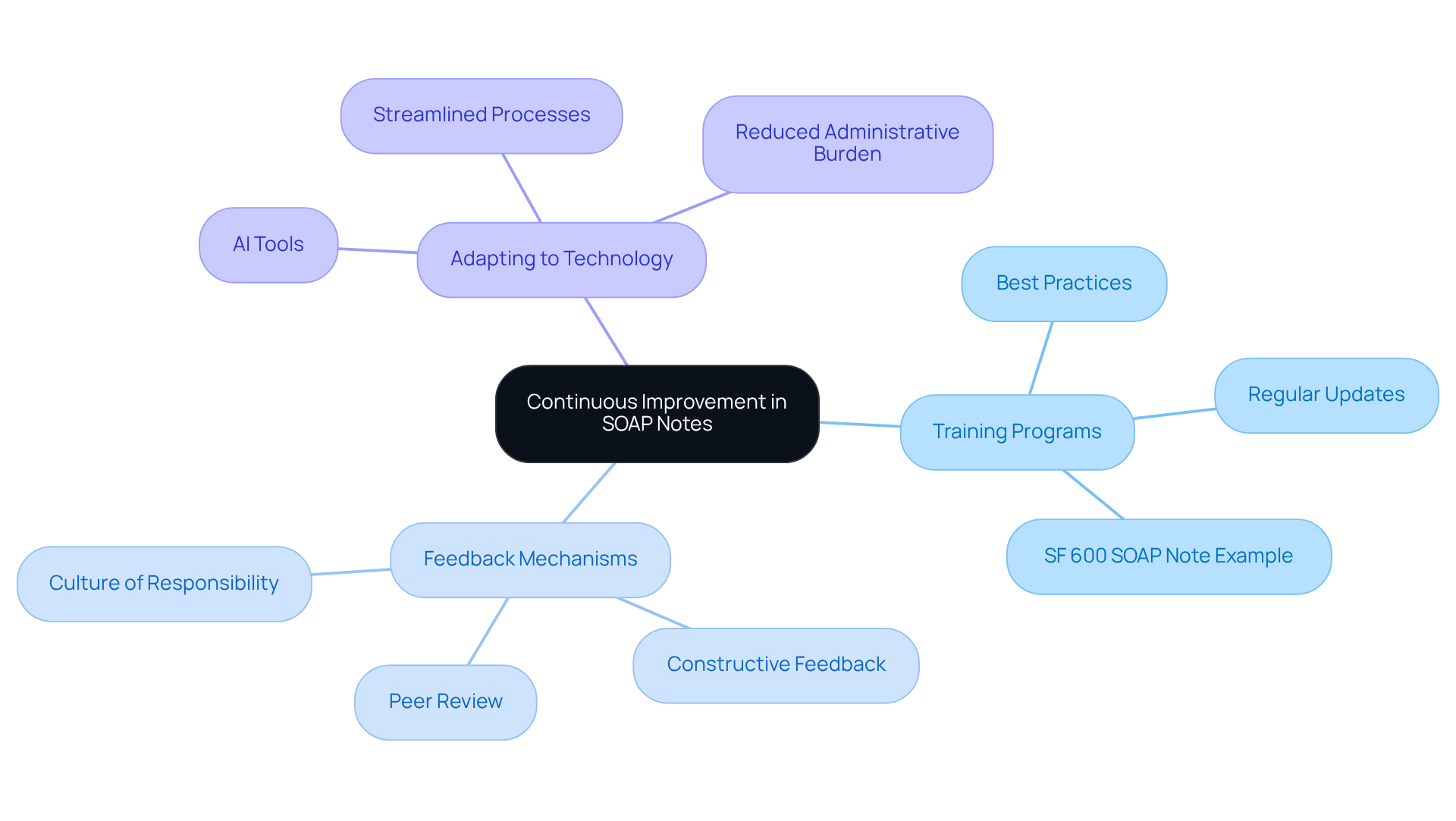
To ensure the ongoing effectiveness and relevance of SOAP note practices, it is essential for healthcare professionals to embrace continuous improvement initiatives. This commitment not only enhances documentation but also uplifts patient care.
Regular training programs that focus on best practices for SOAP note documentation, including the sf 600 soap note example, are vital. They significantly enhance both accuracy and efficiency, ensuring that providers are well-versed in the latest record-keeping standards and techniques. How can we ensure our skills are always sharp?
- Feedback Mechanisms: Establishing systems for peer review and constructive feedback is crucial. These mechanisms help identify specific areas for enhancement in record-keeping practices, fostering a culture of responsibility and growth. Engaging and empowering individuals involved in the work is essential for tackling complex healthcare challenges. What feedback can we seek to improve our practices?
- Adapting to Technology: Embracing innovative technologies, such as AI-driven recording tools, streamlines the SOAP note process. These tools not only reduce administrative burdens but also enhance the overall quality of records. How can technology support us in our daily tasks?
Statistics reveal that between 44,000 and 98,000 individuals lose their lives annually due to avoidable medical mistakes in the United States. This stark reality underscores the critical need for precise record-keeping and ongoing enhancement in medical practices. By committing to these continuous improvement strategies, healthcare providers can significantly elevate the quality of their documentation, such as the sf 600 soap note example, ultimately leading to improved patient care and outcomes.
As Benjamin Franklin wisely noted, 'Without continual growth and progress, such words as improvement, achievement, and success have no meaning.' Additionally, as George Bernard Shaw stated, 'Progress is impossible without change, and those who cannot change their minds cannot change anything.' Let us embrace these insights and commit to nurturing our practices for the benefit of our patients.
Conclusion
In the realm of healthcare, effective documentation is crucial for delivering quality patient care. The SF 600 SOAP note serves as an essential tool in achieving this goal. By integrating advanced technologies like CosmaNeura's AI platform, healthcare providers can streamline the documentation process. This allows them to focus more on their patients rather than administrative tasks. Have you considered how much time could be saved by adopting structured formats like the SF 600 SOAP note? This approach enhances communication, improves compliance, and ultimately elevates patient outcomes.
Throughout the discussion, key insights highlight the benefits of using the SF 600 SOAP note. Its role in military healthcare documentation, the structured components of SOAP notes, and the importance of avoiding common pitfalls that can compromise record integrity are all vital. The integration of AI tools further enhances the efficiency of note-taking. Continuous improvement initiatives encourage healthcare professionals to adapt and refine their documentation practices. How might embracing these tools transform your daily workflow?
As the healthcare landscape evolves, embracing innovative documentation strategies is vital for fostering a compassionate and effective environment for both providers and patients. By committing to high-quality record-keeping and leveraging available technologies, healthcare professionals can significantly improve their practices. This ensures that they provide the best possible care to their patients. The journey towards better documentation is ongoing, ultimately leading to enhanced patient trust and satisfaction. Let us reinforce the importance of diligent and thoughtful care in every interaction.




