Overview
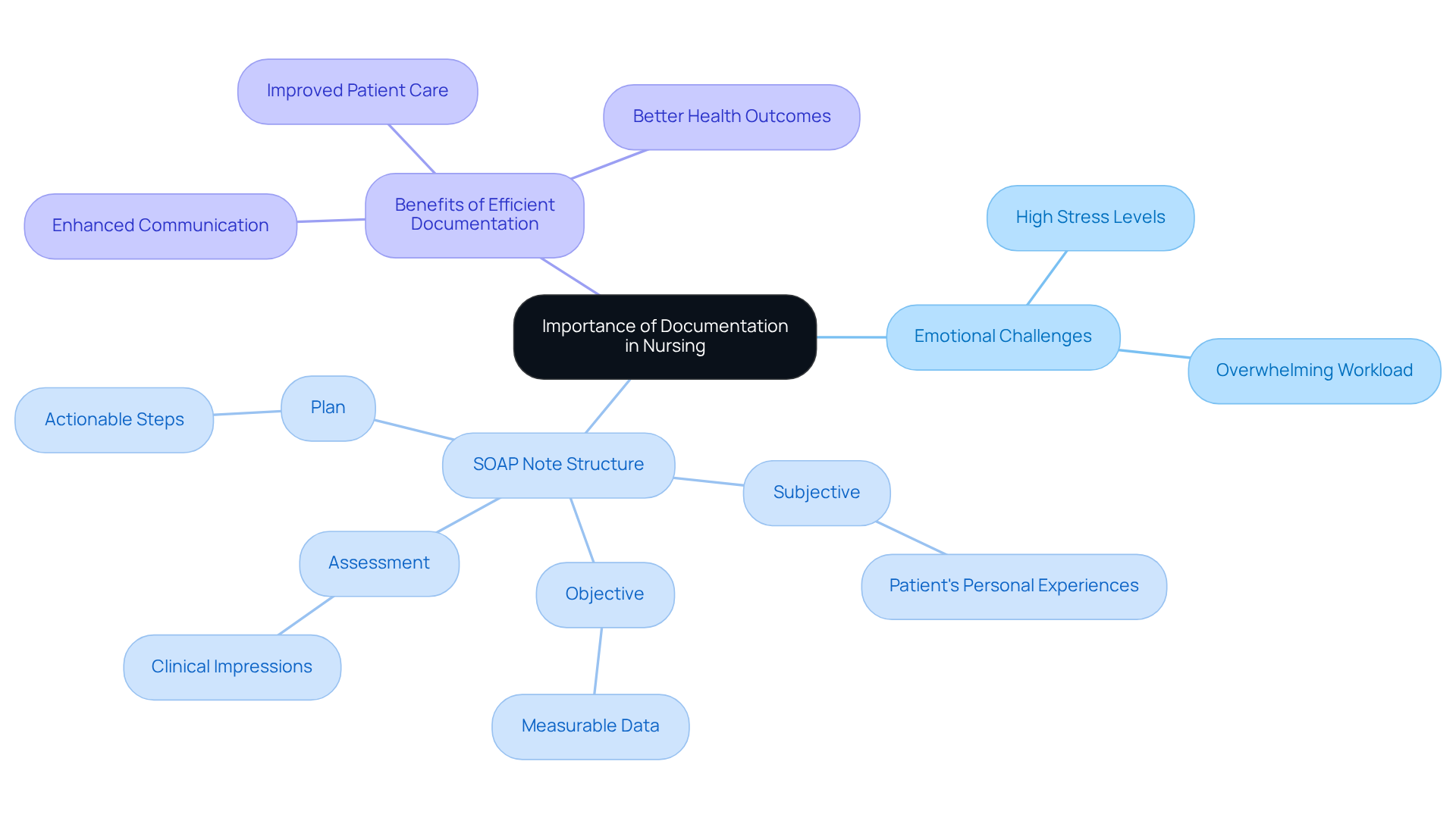
The article titled "7 Essential Nursing SOAP Note Templates for Effective Documentation" addresses the emotional challenges that healthcare providers often encounter in their daily practice. It recognizes the overwhelming administrative burdens that can detract from the quality of patient care. By providing essential templates for nursing SOAP notes, this article offers a solution that not only streamlines record-keeping but also fosters better communication among healthcare providers.
These templates are designed to enhance documentation practices, allowing nurses to efficiently capture and organize critical information during patient interactions. This improvement ultimately leads to better patient care outcomes, as it enables healthcare providers to focus more on their patients rather than on paperwork.
Consider how much easier your documentation process could be with these tools at your disposal. Imagine reducing the time spent on administrative tasks and instead dedicating that time to meaningful patient interactions. By adopting these templates, you can transform your documentation experience and improve the overall quality of care you provide.
In summary, utilizing these nursing SOAP note templates not only lightens the administrative load but also enhances the quality of care delivered to patients. Take a step towards more effective documentation today and discover the positive impact it can have on your practice and your patients.
Introduction
In the fast-paced world of healthcare, nursing professionals often face overwhelming documentation demands that can divert attention from the care they provide to patients. This article explores seven essential nursing SOAP note templates, designed to streamline documentation processes and enhance communication, ultimately leading to improved patient outcomes.
How can these structured templates not only alleviate administrative burdens but also empower nurses to offer more compassionate and effective care?
Dive in to discover the transformative potential of these tools in modern nursing practice. By addressing these emotional challenges, we can foster an environment where nurses feel supported and equipped to focus on what truly matters—their patients.
CosmaNeura: AI-Driven SOAP Note Automation for Healthcare Providers
Healthcare providers often face overwhelming documentation burdens that can detract from their ability to deliver compassionate care. CosmaNeura understands these emotional challenges and offers a solution through advanced AI technology that automates the generation of clinical records. By seamlessly incorporating client intake and clinical data, the platform generates precise and compliant nursing soap note templates. This allows providers to uphold high standards of care while significantly reducing administrative tasks.
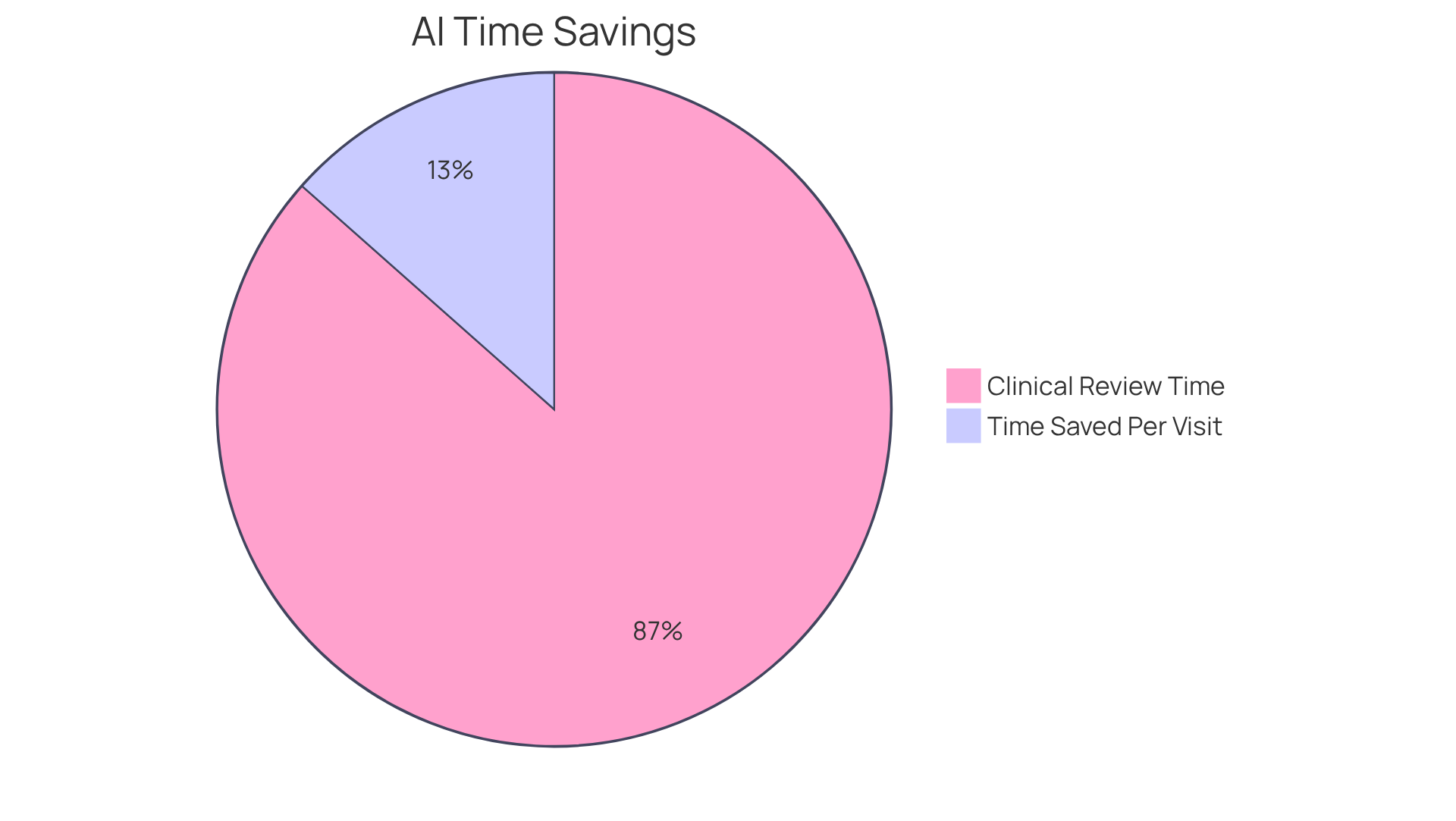
Imagine being able to concentrate more on your interactions with patients rather than getting lost in paperwork. Recent advancements in AI show that practices employing such technology can achieve a remarkable 45% decrease in clinical review time. This means clinicians can spend more quality time with individuals, fostering stronger relationships and better outcomes.
Moreover, healthcare professionals have reported notable enhancements in job satisfaction. Many have observed that AI-driven record-keeping tools have positively altered their workflow. In fact, a study indicated that AI-supported record-keeping can save clinicians an average of 7 minutes per patient visit, translating into more time dedicated to patient care.
This innovative approach not only improves the quality of records but also aligns with ethical care principles, reinforcing our dedication to compassion in healthcare. Are you ready to explore how CosmaNeura can transform your practice and support your commitment to high-quality patient care? Let’s take this journey together.
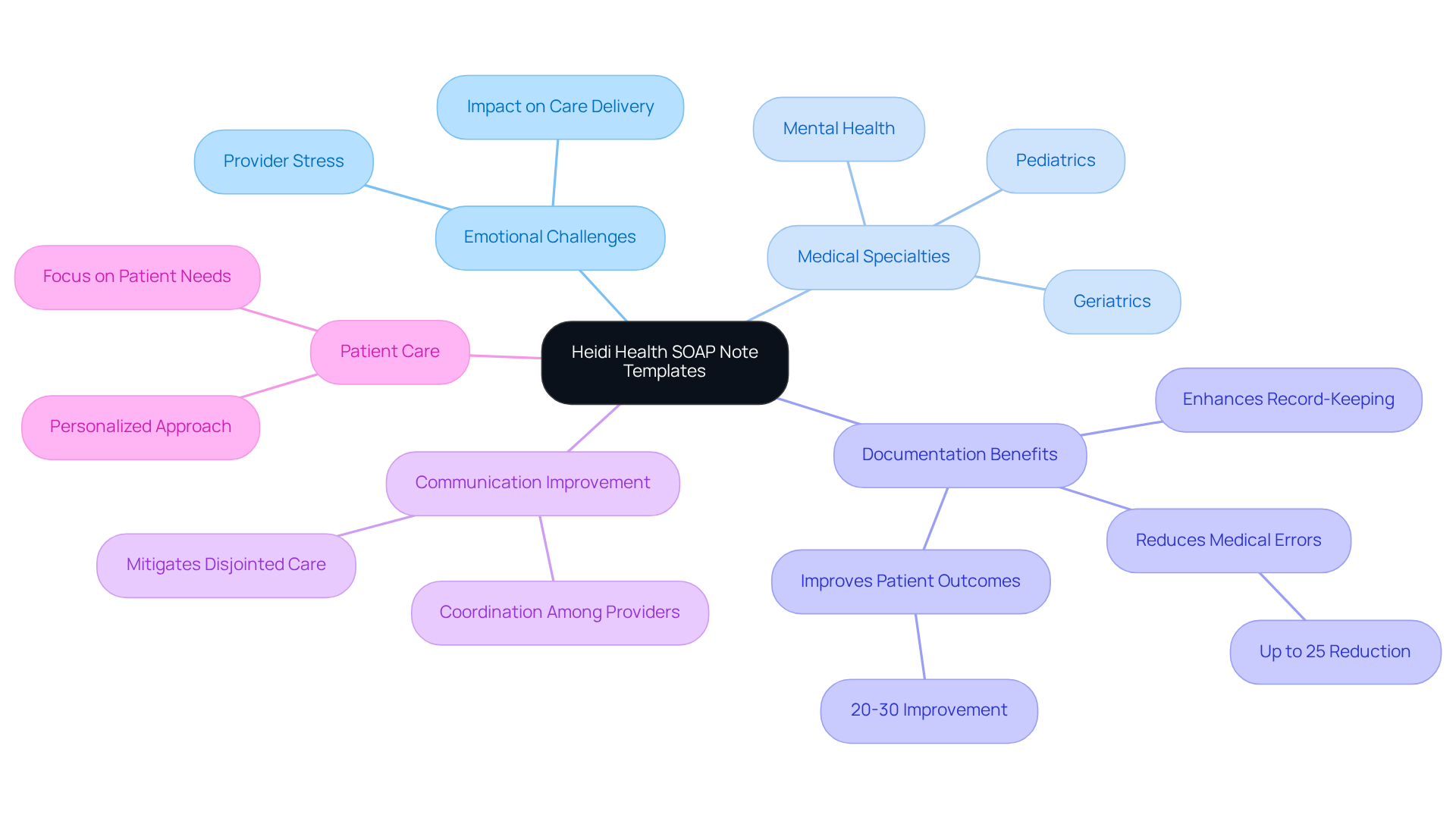
Heidi Health: Comprehensive SOAP Note Templates for Diverse Medical Specialties
In the demanding world of healthcare, providers often face emotional challenges that can impact their ability to deliver the best care. Heidi Health understands these struggles and offers a versatile array of customizable nursing soap note templates designed for various medical specialties, including pediatrics, geriatrics, and mental health. These templates empower healthcare professionals to tailor their documentation to meet specific needs, ensuring a thorough recording of vital individual information.
By utilizing these organized templates, healthcare specialists can significantly enhance their record-keeping methods. This improvement not only promotes better outcomes for individuals but also streamlines workflow effectiveness. Imagine a system where your documentation reflects the unique needs of each patient, allowing for a more personalized approach to care. In fragmented healthcare systems, this level of customization is essential.
Moreover, these templates foster enhanced communication and coordination among providers, which can mitigate the risks associated with disjointed care. By addressing administrative burdens, we can collectively focus on what truly matters—our patients. Are you ready to take a step towards improving your documentation and patient care? Explore how these customizable nursing soap note templates can transform your practice and enhance your commitment to compassionate healthcare.
Nurse.org: Step-by-Step SOAP Note Writing Guide with Practical Examples
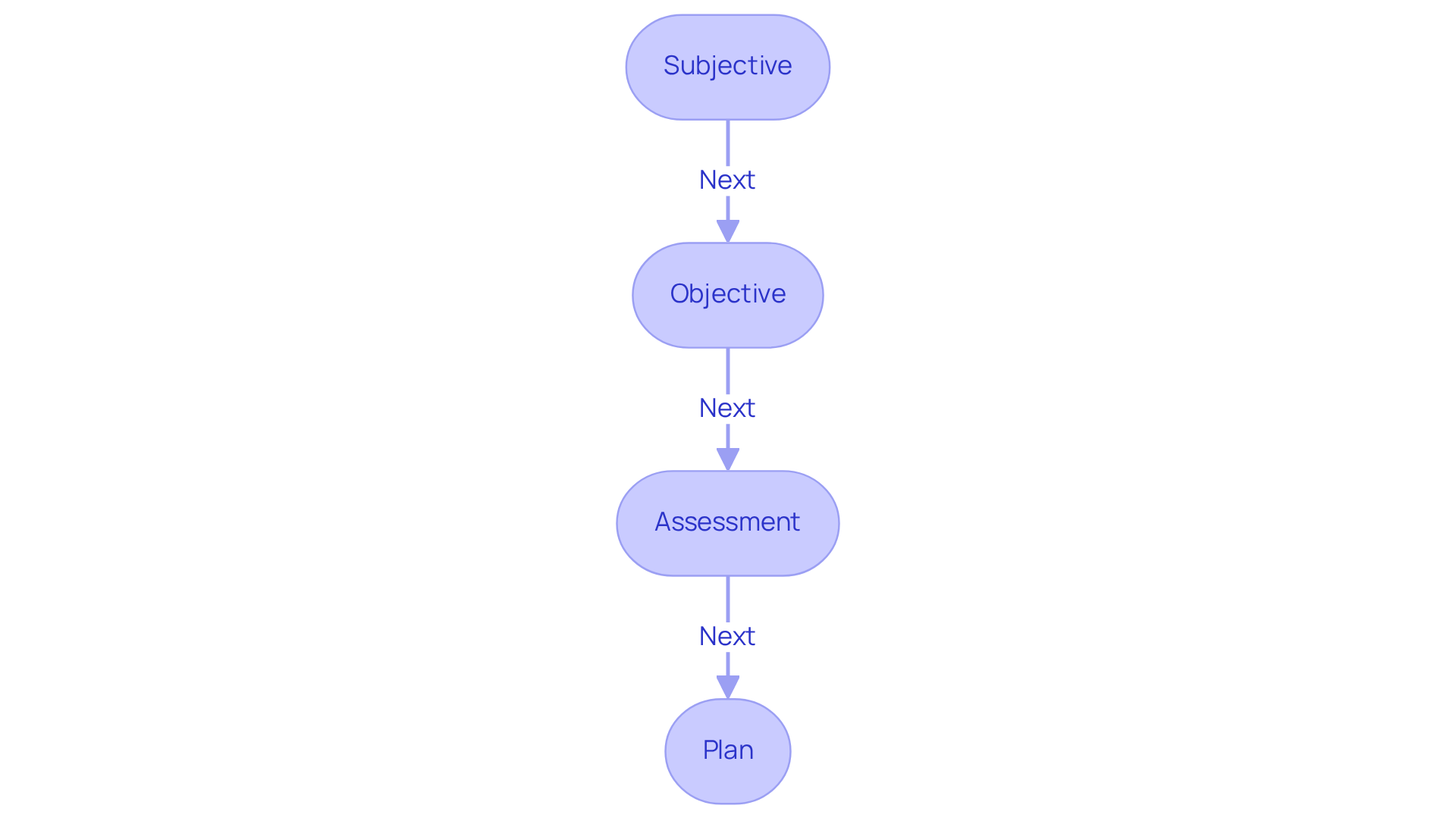
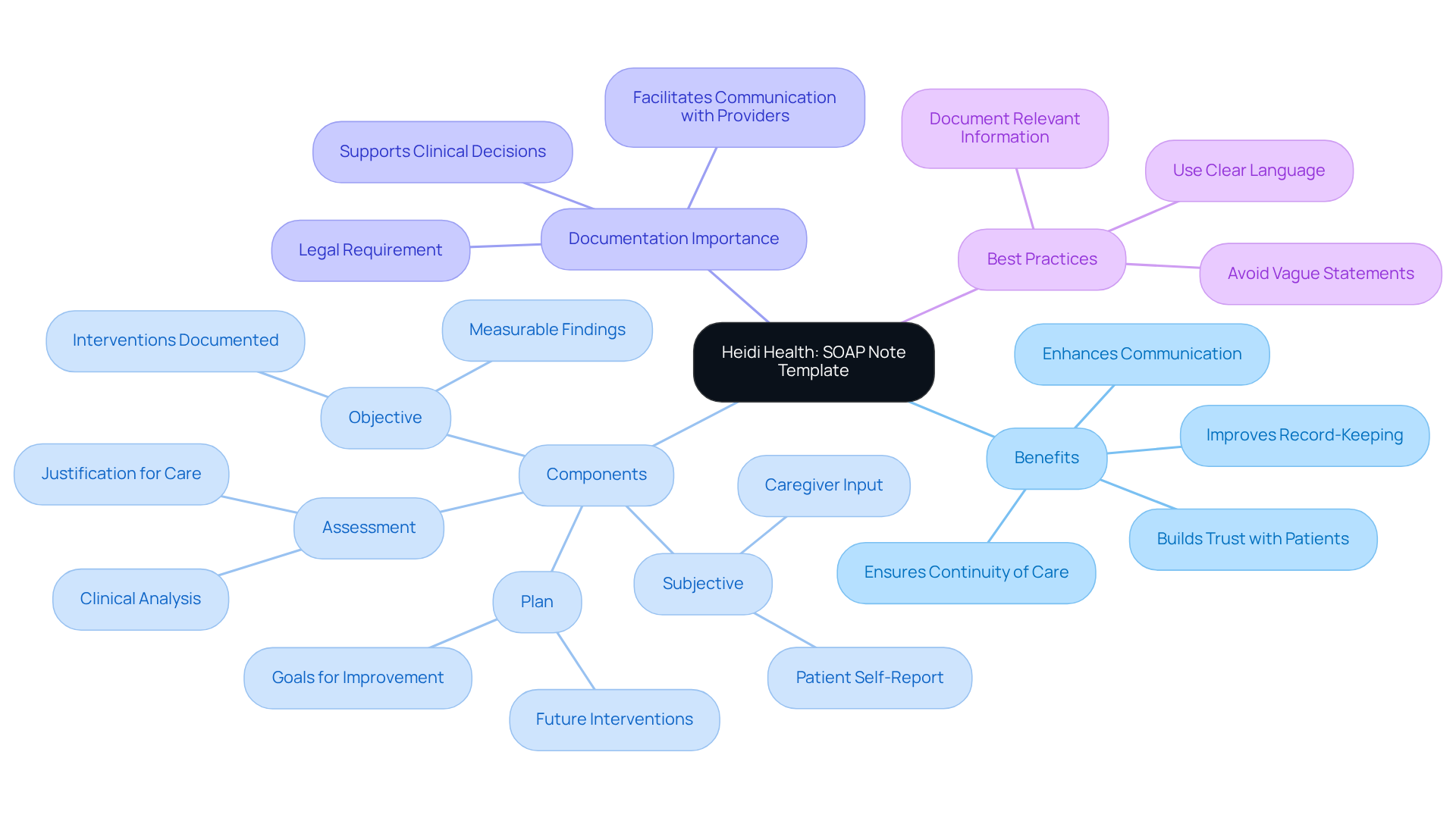
At Nurse.org, we understand the emotional challenges faced by healthcare providers when it comes to documentation. That’s why we provide a nursing soap note template as an extensive, sequential guide for composing clinical documentation, complete with practical examples. This guide thoughtfully analyzes each element of the Subjective, Objective, Assessment, and Plan format, providing nurturing advice on how to collect and record pertinent information efficiently. By utilizing a nursing soap note template, nurses can follow an organized method to ensure their documentation is thorough, ultimately promoting improved communication with other healthcare professionals.
A systematic approach to composing nursing notes using a nursing soap note template is essential for effective documentation. The nursing soap note template, based on the SOAP format—Subjective, Objective, Assessment, and Plan—offers a clear framework that enhances communication among healthcare providers. Each component serves a vital purpose:
- Subjective: This section captures the patient's feelings, concerns, and symptoms, often gathered through direct dialogue. For instance, a nurse might record an individual's report of chest pain, detailing its onset and severity.
- Objective: Here, nurses document observable data, such as vital signs and physical examination findings. Accurate documentation in this section is crucial; studies reveal that 96.6% of vital sign sheets were completed and documented well, underscoring the importance of thoroughness.
- Assessment: This part integrates information from the subjective and objective sections, allowing nurses to interpret the individual's condition. For example, a nurse might assess that a patient with chest pain is experiencing anxiety, which could influence their overall health.
- Plan: The plan outlines the treatment strategy, including short- and long-term goals. It should specify what will be addressed in the next session and expectations for treatment duration.
Effective record-keeping practices, such as utilizing a nursing soap note template, are not just a legal requirement; they are essential for continuity of care. Research shows that health professionals' routine practice records were found to be 51.1%, emphasizing the necessity for enhancement in this area. Moreover, a strong understanding of routine practice records enhances the chances of accurate recording by 1.4 times. Utilizing electronic systems for record-keeping improves efficiency, making health professionals 2.2 times more likely to report their practices accurately.
Nursing instructors emphasize the importance of organized records. One educator noted, "Documentation is the primary clinical information source to fulfill legal and professional standards," highlighting its critical role in ensuring quality care for individuals. By following this structured format, nurses can enhance their documentation quality, ultimately resulting in improved outcomes for individuals and better care coordination. We encourage you to engage with this guide, as it’s designed not only to support your documentation needs but also to foster a compassionate approach to patient care.
Physio-pedia: Historical Context and Benefits of SOAP Notes in Nursing
The historical evolution of SOAP records began in the 1960s when Dr. Lawrence Weed introduced them as a standardized approach for documenting client interactions. This organized method significantly enhances communication among healthcare providers, facilitating clearer exchanges of essential information regarding individuals' health. By structuring clinical data into four unique elements—Subjective, Objective, Assessment, and Plan—using a nursing soap note template enhances the precision and efficiency of records, which is vital in today’s fast-paced healthcare setting.
But have you ever considered the emotional challenges faced by healthcare providers? The advantages of employing a nursing soap note template extend beyond mere documentation; it is crucial for improving care for individuals. By offering a reliable structure, documentation allows healthcare professionals to monitor client progress efficiently and maintain continuity of care. This standardization reduces the likelihood of errors and omissions, especially in interdisciplinary contexts where multiple providers are involved.
Furthermore, the use of a nursing soap note template in structured documentation fosters enhanced communication between providers, which is essential for coordinated care. A well-organized medical document not only assists healthcare professionals in clinical decision-making but also empowers individuals by clearly detailing their health condition and treatment strategies. As healthcare progresses, the concepts of structured documentation remain essential for promoting effective communication and ensuring high-quality care for individuals. Let’s embrace these practices together to foster a supportive environment for both providers and patients.

SoapNoteAI: Tailored SOAP Note Templates for Registered Nurses
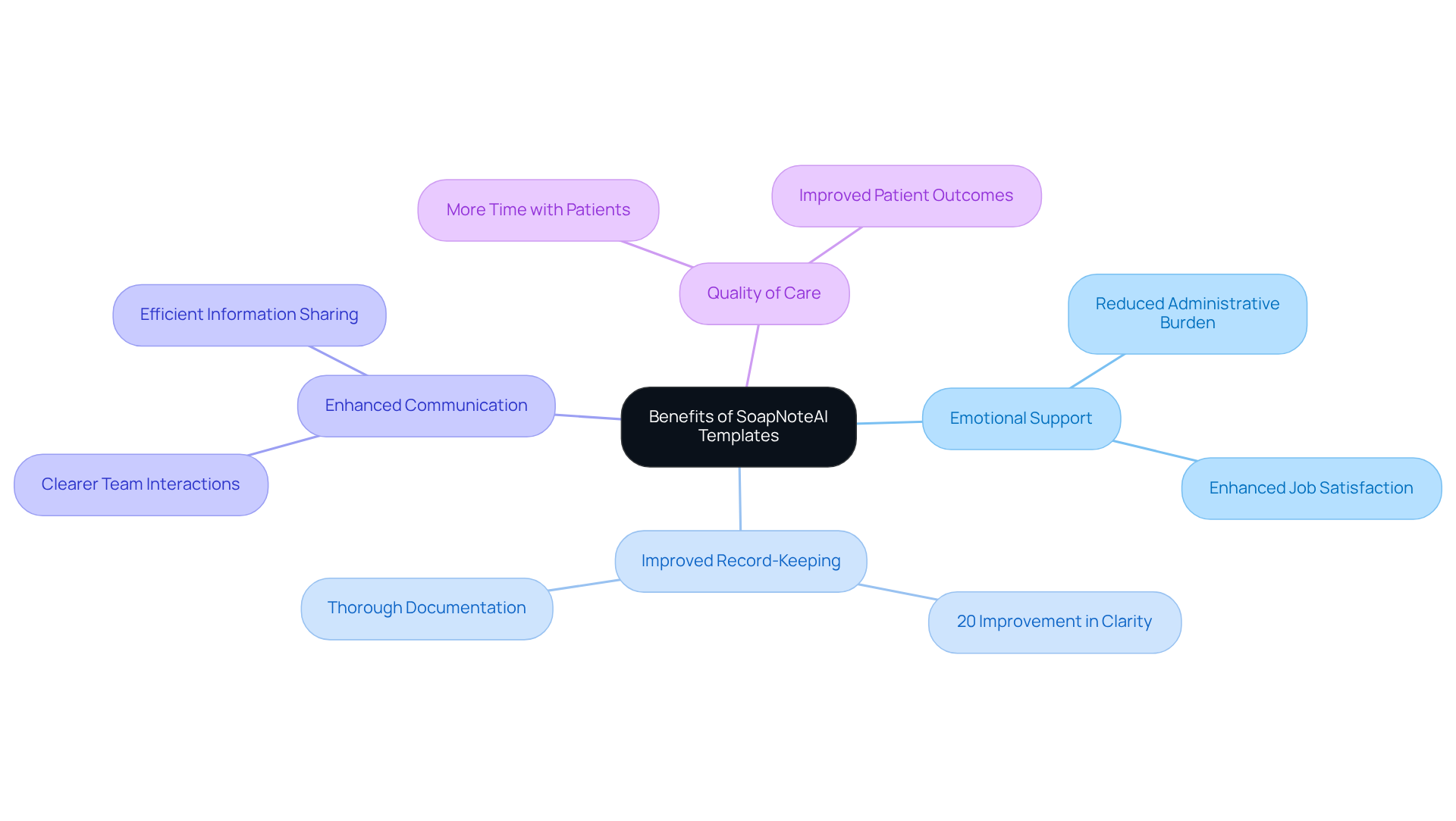
At SoapNoteAI, we understand the emotional challenges that registered nurses face in their daily practice. The administrative burdens can often feel overwhelming, impacting the quality of care provided to patients. Our collection of specialized nursing soap note templates is specifically designed to meet the unique recording needs of nursing practice, ensuring that all relevant client information is captured thoroughly.
By utilizing these tailored tools, registered nurses can significantly enhance their record-keeping processes. This improvement not only elevates the quality of care but also fosters clearer communication within the healthcare team. Imagine being able to spend more time with your patients, knowing that your documentation is organized and efficient.
The implementation of these organized records has shown to lead to a remarkable 20% improvement in clarity and organization. This efficiency allows you to focus on what truly matters—your interactions with individuals, ultimately enriching the overall quality of care you provide. We invite you to explore how the nursing soap note template can assist you in your vital role, making a meaningful difference in your practice and the lives of those you care for.
NurseTogether: Importance of Documentation and SOAP Note Examples
NurseTogether recognizes the emotional challenges faced by nurses, particularly the burden of record-keeping. Precise and prompt clinical summaries are essential for efficient patient care, yet current statistics reveal that nurses spend an average of 8.0 hours per week on clinical documentation. This workload can feel overwhelming, with 52.4% of community nurses reporting high levels of stress due to documentation demands. How can we alleviate this burden?
Organized formats, such as the nursing soap note template, which includes Subjective, Objective, Assessment, and Plan, play a crucial role in managing this workload effectively. Each element contributes to a comprehensive understanding of a patient's condition. For instance, the Subjective section captures personal experiences and symptoms, while the Objective section records measurable data like vital signs and lab results. This structured approach not only enhances communication among healthcare teams but also ensures continuity of care.
Studies show that efficient documentation can lead to better health outcomes. Healthcare experts emphasize that well-prepared records enhance prompt decision-making and reduce the likelihood of errors, ultimately promoting improved care coordination. As Rajeev Rajagopal wisely notes, 'improving medical records with this structure supports continuity of care, efficient communication, and improved health results.'
By prioritizing comprehensive documentation and utilizing a nursing soap note template while regularly reviewing their records, nurses can significantly enhance the quality of care they provide. This ensures that vital information is not only accessible but also actionable. Together, let’s embrace these practices to support our commitment to patient care and well-being.
StatPearls: Clinical Significance and Best Practices for SOAP Notes
In healthcare, a nursing soap note template is essential for creating structured records, serving as a systematic way to document individual interactions and promote effective communication among providers. It's important to approach clinical documentation with clarity, brevity, and precision, which can be effectively achieved by using a nursing soap note template to capture the nuances of healthcare. For instance, well-documented subjective sections help clinicians understand the individual's perspective, while objective sections provide factual observations that support clinical evaluations.
Have you considered how well-crafted nursing soap note templates can significantly enhance patient outcomes? By following best practices and utilizing a nursing soap note template, healthcare providers can elevate the quality of their documentation, leading to more efficient care delivery. A study revealed that accurate personal observations allow healthcare teams to tailor interventions, ultimately enhancing health outcomes for patients.
Healthcare practitioners recognize the critical role of documentation in their practice. As one physician expressed, "Documenting routine practice is significant for better diagnosis, treatment, continuity of care, and medicolegal issues." This insight underscores the necessity of maintaining high standards in clinical record-keeping by utilizing a nursing soap note template, as it not only supports clinical reasoning but also fosters trust in the healthcare system.
Integrating these optimal methods into daily record-keeping can lead to improved care and satisfaction for individuals. This highlights the essential role of structured communication in the healthcare field. Together, let's embrace these practices to enhance our collective efforts in providing compassionate care.

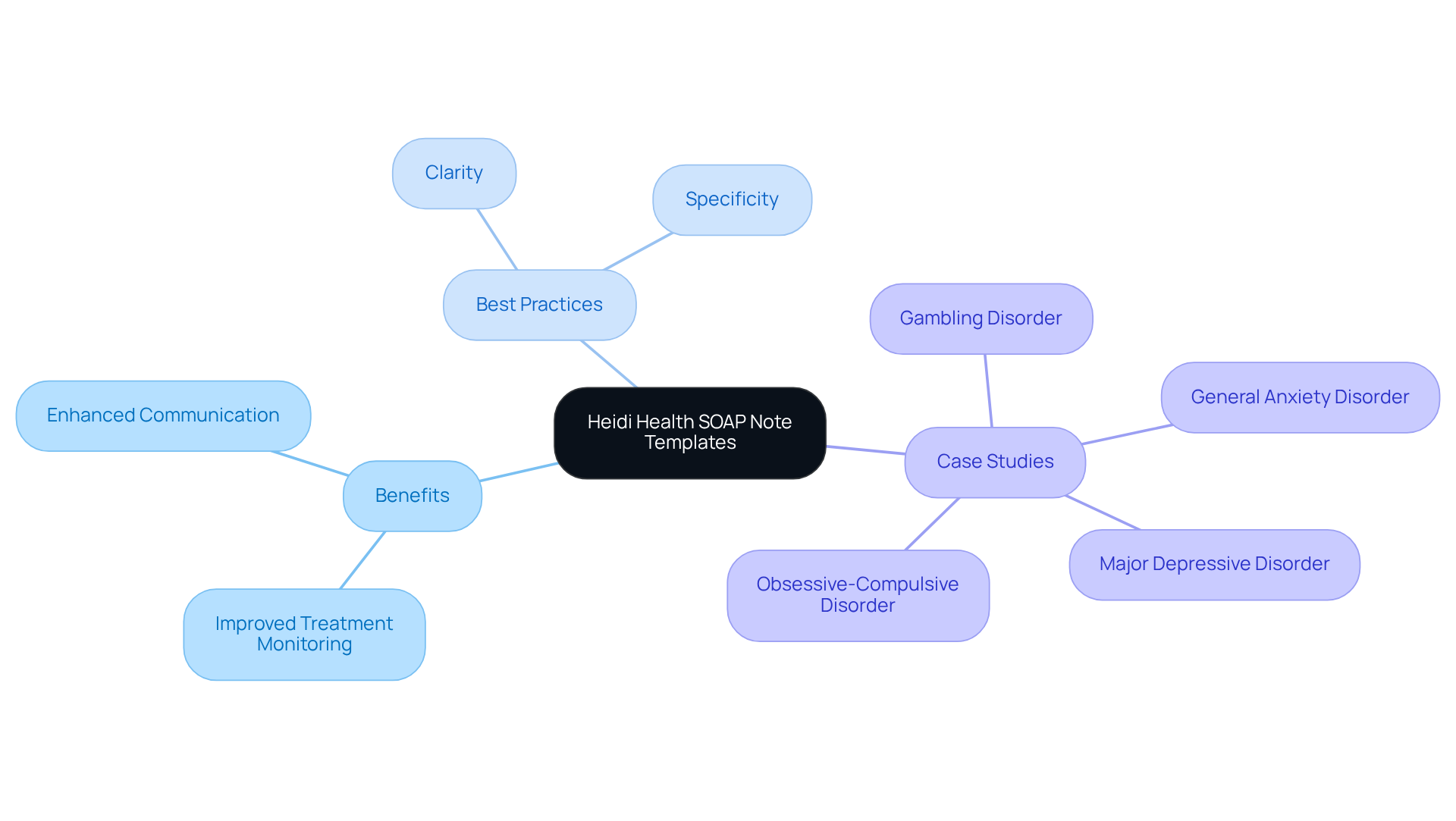
Heidi Health: Specialized SOAP Note Template for Mental Health Professionals
Heidi Health understands the emotional challenges that mental health practitioners face. The administrative burdens of record-keeping can be overwhelming, often detracting from the time spent with patients. That’s why we offer tailored nursing soap note templates specifically designed to meet your needs. These customized nursing soap note templates ensure that your records reflect the unique intricacies of mental health evaluations and treatment strategies.
Imagine how organized records can assist in monitoring progress and treatment effectiveness. For instance, a case study on Major Depressive Disorder illustrates how thorough documentation can lead to enhanced outcomes for individuals. Mental health experts emphasize that precise and thorough records are vital for monitoring progress and guiding treatment choices.
Best practices in mental health record-keeping advocate for clarity and specificity. Each patient's unique experiences and challenges deserve to be thoroughly documented. This organized method not only aids in clinical decision-making but also fosters improved communication among healthcare professionals. Careful record-keeping is essential in mental health care, as insufficient records can lead to misunderstandings and impede efficient care.
By employing customized medical summaries, you can ensure that you are addressing the specific needs of those you serve effectively. Let’s work together to enhance your practice and improve the lives of your patients.
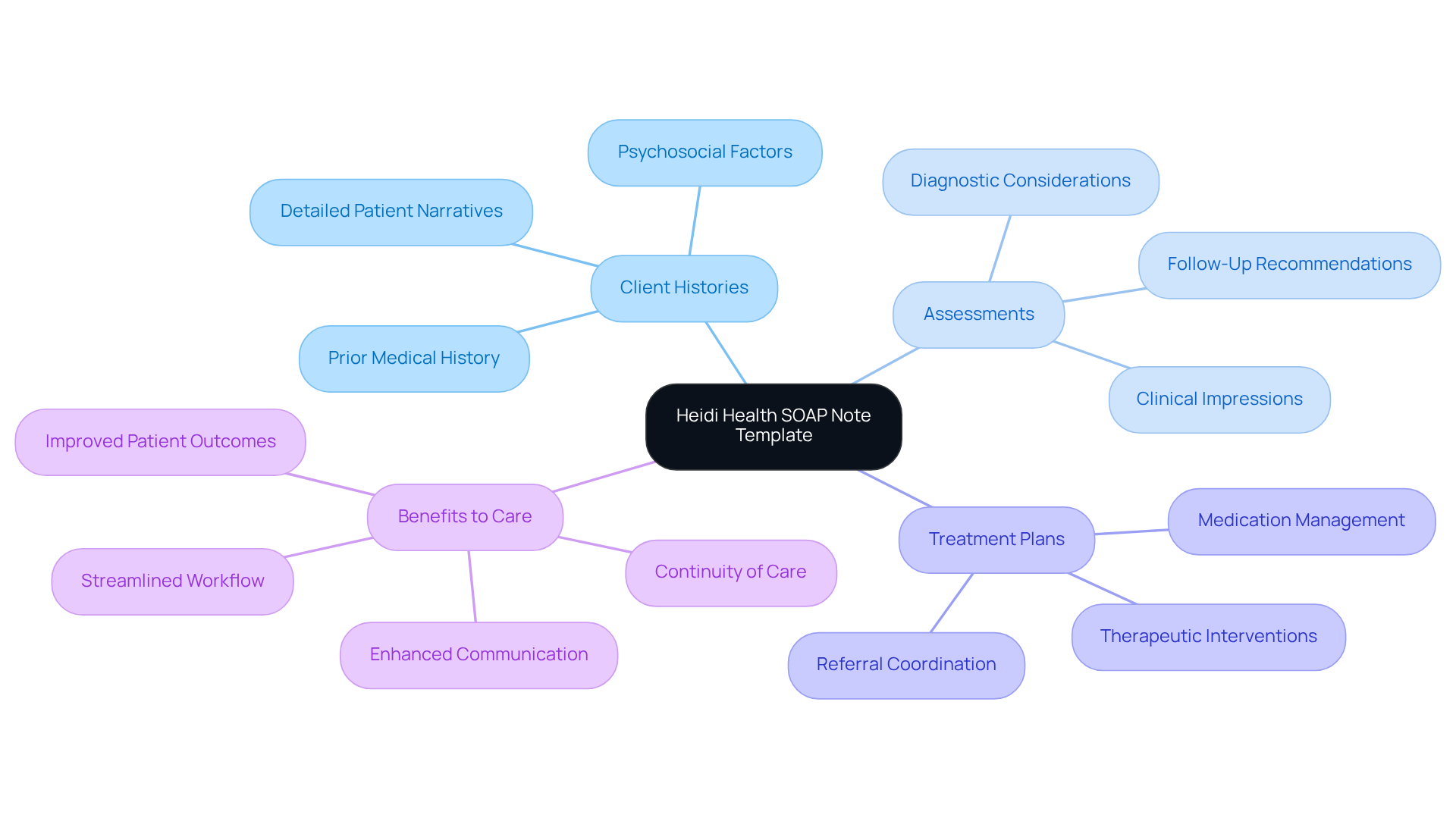
Heidi Health: SOAP Note Template Tailored for Physical Therapy
Heidi Health understands the emotional challenges faced by physical therapy professionals. The administrative burdens can often feel overwhelming, impacting the quality of patient care. That’s why we provide customized nursing soap note templates that are designed to simplify the recording process. These templates enable the precise collection of essential information regarding evaluations, treatment plans, and progress notes.
By utilizing the nursing soap note template, physical therapists can significantly improve their record-keeping practices. This ensures that documentation reflects individual progress and treatment outcomes comprehensively. The importance of meticulous documentation in physical therapy cannot be overstated; it serves not only as a legal requirement but also as a means to demonstrate medical necessity and communicate effectively with other healthcare providers.
Well-organized documentation enhances the clarity of client interactions. It allows therapists to monitor progress and justify treatment choices. As Dr. Sean Ormond wisely states, "Effective documentation assists in capturing the intricacies of pain management, enabling you to record an individual’s experience in a manner that facilitates identifying patterns, monitoring changes, and communicating with other providers."
Precise records promote confidence with clients and guarantee continuity of care, especially when numerous providers are engaged. To avoid common pitfalls, therapists should focus on using clear and simple language, avoiding vague statements, and ensuring that all relevant information is documented.
By utilizing customized treatment records, physical therapists can improve their documentation efficiency. Ultimately, this leads to enhanced care and better treatment results. Let’s embrace this opportunity to simplify your documentation process and focus more on what truly matters—your patients.
Heidi Health: Family Medicine SOAP Note Template for Comprehensive Patient Care
Heidi Health understands the emotional challenges faced by family medicine providers. Our specialized nursing soap note template is designed to alleviate administrative burdens, thereby promoting comprehensive care for individuals. This template is thoughtfully crafted with sections that capture detailed client histories, assessments, and treatment plans, ensuring that all relevant information is thoroughly recorded.
By adopting this structured approach, family medicine providers can significantly enhance their record-keeping practices. This improvement leads to better patient care outcomes and fosters stronger communication within the healthcare team. Imagine how much smoother your workflow could be with standardized fields for primary complaints and treatment plans, directly addressing the challenges posed by fragmented healthcare systems.
Using our nursing soap note template, you can enhance coordination and continuity of care. This cohesive and effective care delivery model not only improves documentation but also helps overcome the obstacles often encountered in healthcare settings. We invite you to explore how this tool can make a positive difference in your practice and contribute to a more nurturing healthcare environment.
Conclusion
The significance of utilizing nursing SOAP note templates is profound in the quest for effective healthcare documentation. These templates are essential tools that streamline the documentation process, allowing healthcare professionals to devote more attention to patient care rather than administrative tasks. By integrating structured approaches to note-taking, providers can enhance communication, ensure continuity of care, and ultimately improve patient outcomes.
Have you ever felt overwhelmed by administrative duties? Throughout this article, we explored various solutions, such as CosmaNeura's AI-driven automation, which significantly reduces clinical review time, and Heidi Health's customizable templates tailored for diverse medical specialties. The benefits of these tools extend beyond mere efficiency; they cultivate improved job satisfaction among healthcare providers and encourage a more compassionate approach to patient interactions.
Moreover, the historical context of SOAP notes highlights their evolution and importance in modern clinical practice, underscoring the necessity for structured documentation to ensure high-quality care. Embracing the use of nursing SOAP note templates is vital for healthcare professionals seeking to enhance their documentation practices and the quality of patient care.
As the healthcare landscape continues to evolve, integrating these best practices will not only alleviate the burdens of paperwork but also empower providers to deliver compassionate and efficient care. The call to action is clear: prioritize effective documentation strategies today to foster a healthier tomorrow for both providers and patients alike.




