Overview
In the demanding world of healthcare, the emotional challenges faced by nurses and healthcare providers can be overwhelming. Effective documentation is not just a task; it is a vital part of patient care that often adds to their administrative burden. This is where nurse charting templates come into play.
Utilizing structured templates, such as SOAP and DAR notes, can significantly enhance efficiency. These tools not only streamline the documentation process but also improve the quality of care provided to patients. Imagine being able to focus more on supporting your patients rather than being bogged down by paperwork.
By alleviating the administrative load, healthcare professionals can devote more time to what truly matters: patient interaction and support. This shift not only benefits the providers but also enriches the patient experience, fostering a nurturing environment.
As you consider how to improve your documentation practices, think about the potential impact of integrating these templates into your workflow. Embracing structured documentation can lead to a more fulfilling and effective approach to patient care. Let’s take this step together towards a more compassionate healthcare experience.
Introduction
In the fast-paced realm of healthcare, where every second counts, the burden of meticulous documentation can weigh heavily on nursing professionals. This challenge can lead to feelings of overwhelm, impacting not only the efficiency of care but also the quality of patient interactions. With the rise of innovative tools like AI-powered nurse charting templates, there lies an opportunity to transform how nurses manage their record-keeping. These templates promise to streamline documentation, ultimately enhancing patient care.
Yet, amidst these advancements, a pressing question remains: how can these templates not only ease the administrative load but also ensure that the compassionate nature of patient interactions is preserved? This article delves into seven essential nurse charting templates that promise to revolutionize documentation practices while fostering a nurturing healthcare environment.
Consider how these templates can alleviate the stress of documentation, allowing nurses to focus more on what truly matters—their patients. By embracing these innovations, we can create a supportive atmosphere that prioritizes both efficiency and empathy in healthcare.
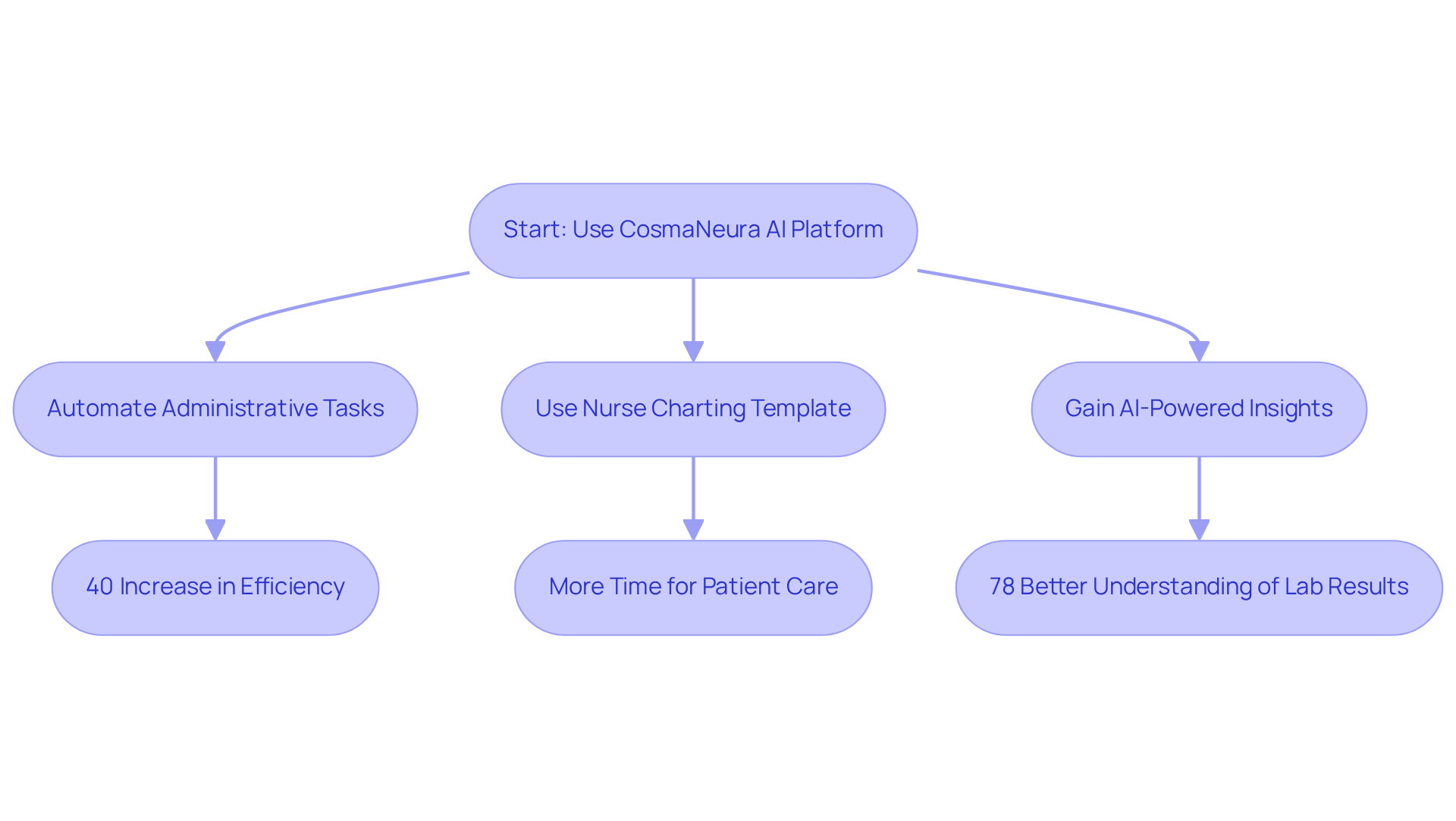
CosmaNeura: AI-Powered Nurse Charting and Documentation Solution
In the demanding world of primary healthcare, professionals often face overwhelming emotional challenges. Caregivers and healthcare providers are burdened with administrative duties that detract from their ability to focus on what truly matters: client support. CosmaNeura understands this struggle and offers an innovative AI-driven platform designed specifically for these dedicated individuals.
By automating administrative tasks, CosmaNeura empowers healthcare professionals to redirect their energy toward patient care. Imagine a scenario where nurses can utilize a nurse charting template to log interactions quickly and accurately, all while adhering to ethical principles grounded in Catholic teachings. This integration of technology not only streamlines workflow but also enhances the quality of patient support.
Consider the impact: case studies reveal that healthcare providers utilizing AI solutions have experienced a remarkable 40% increase in efficiency. This significant improvement means less time spent on record-keeping and more time dedicated to compassionate care. Furthermore, 78% of users have reported a deeper understanding of lab results through AI-powered explanations, showcasing a positive influence on clinical decision-making.
As healthcare leaders increasingly recognize the importance of automation in addressing staffing challenges, CosmaNeura stands at the forefront, enabling caregivers to provide the compassionate support their clients deserve. Together, let’s embrace these advancements and foster a healthcare environment where professionals can thrive by using a nurse charting template to maintain high standards of record-keeping. How can you take the next step towards enhancing your practice with CosmaNeura?
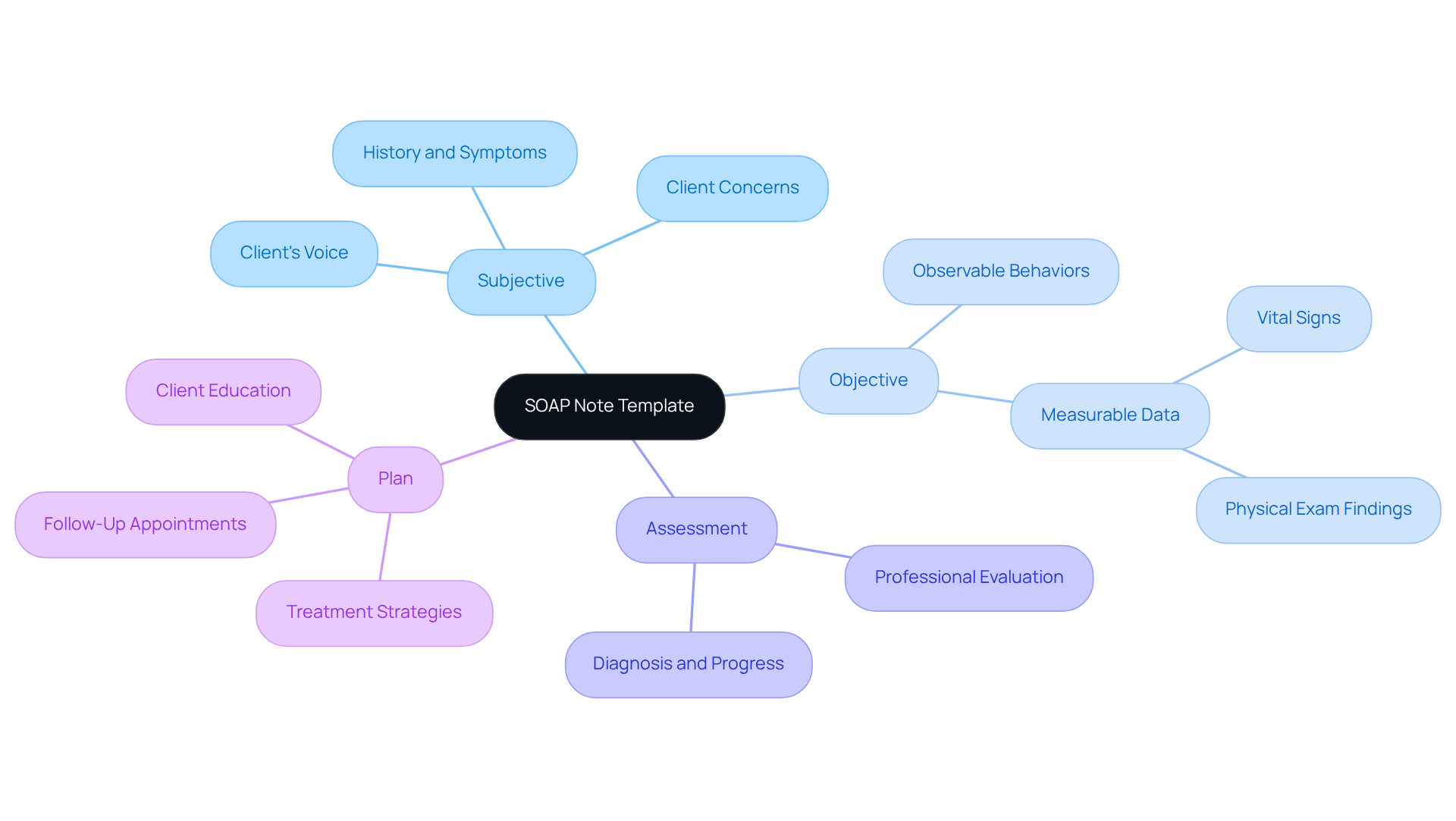
SOAP Note Template: Structured Patient Documentation for Nurses
Healthcare providers often face emotional challenges due to the overwhelming demands of record-keeping. The SOAP (Subjective, Objective, Assessment, Plan) note template serves as a vital structure, helping to organize individual information in a way that eases this burden. By clearly outlining subjective reports, objective findings, assessments, and planned interventions, SOAP notes enhance communication among healthcare teams. How much easier would your day be if you had a comprehensive overview of patient care at your fingertips?
Utilizing SOAP notes not only supports clinical decision-making but also fosters continuity of care. Research indicates that organized records can reduce record-keeping time by up to 42%, while simultaneously improving note quality by 36.6%. These efficiencies are crucial, especially considering that over 78% of healthcare providers spend more than 10 hours each week on documentation. Imagine what you could accomplish with that time back!
The integration of generative AI further optimizes the record-keeping process, enabling automated data entry and enhancing accuracy. Case studies reveal that hospitals implementing SOAP notes have seen significant improvements in both satisfaction and quality of service. This highlights the importance of adopting this documentation approach in nursing practice.
By embracing AI and structured documentation, healthcare providers can alleviate administrative workloads, allowing for more meaningful interactions with clients. This shift not only improves service delivery but also nurtures the compassionate care that every patient deserves. Let’s take steps together towards a more efficient and supportive healthcare environment.
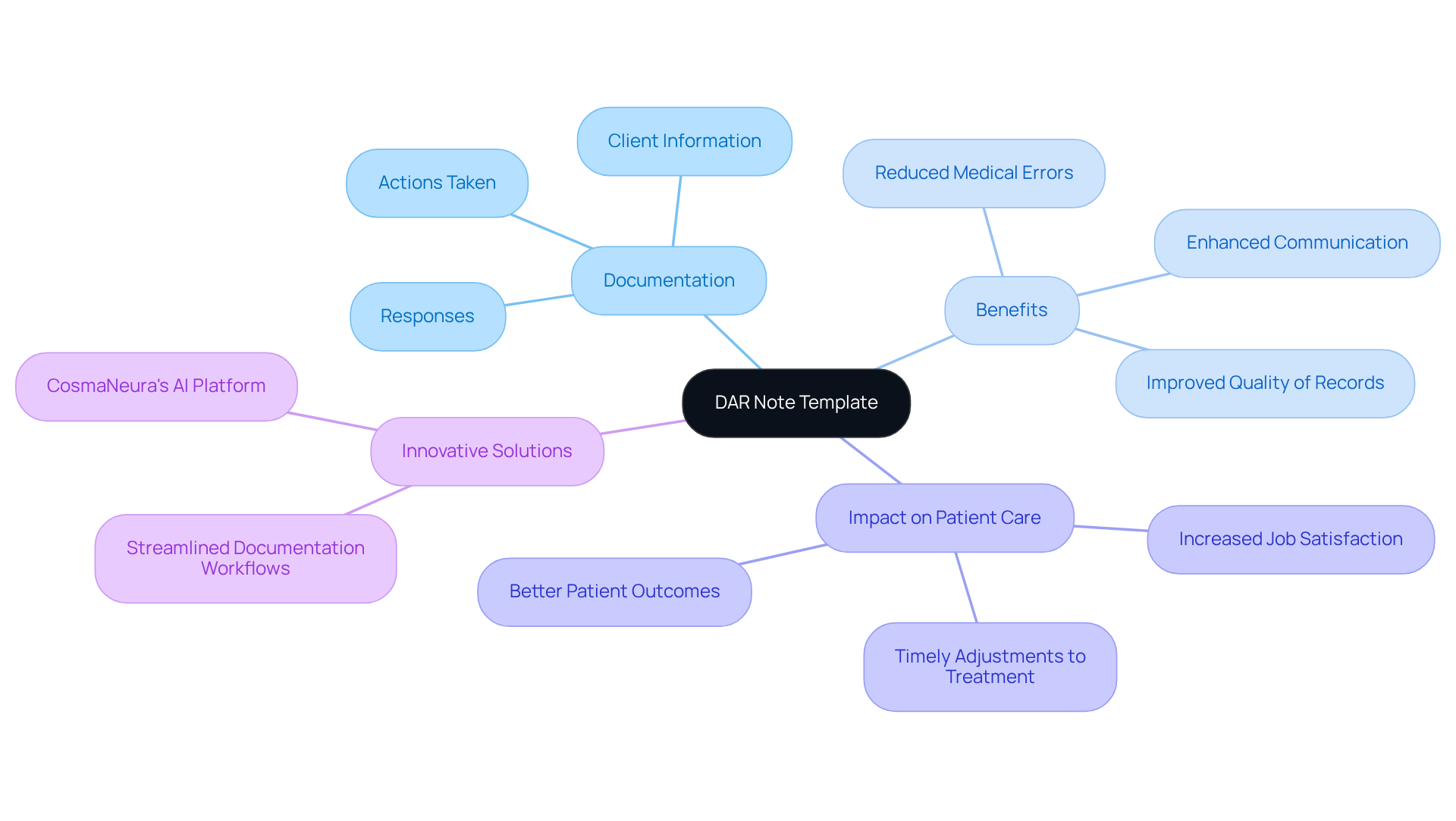
DAR Note Template: Effective Documentation of Patient Interventions
The DAR note template serves as a vital resource for healthcare professionals, enabling them to systematically record client information, the actions taken, and the individual's responses. This organized approach not only facilitates efficient monitoring of interventions and outcomes but also ensures that support is tailored to meet each person's unique needs. By adopting the DAR format, healthcare providers can create a coherent account of care that supports ongoing evaluation and timely adjustments to treatment strategies.
In the face of healthcare challenges, such as physician burnout and resistance to innovation, the importance of the DAR note template becomes even more pronounced. Have you ever felt overwhelmed by administrative tasks? Studies reveal that organized records, like DAR notes, significantly improve the quality of nursing entries, ultimately leading to enhanced patient outcomes. For instance, one study found that employing the DAR model improved critical thinking organization among healthcare professionals, fostering greater job satisfaction.
Moreover, accurate record-keeping methods, including DAR notes, have been shown to reduce medical errors and enhance communication within healthcare teams. By utilizing the nurse charting template, you can streamline your documentation workflows, ensuring that essential individual information is recorded with precision and remains easily accessible. This not only improves the overall tracking of treatment but also contributes to better care for your patients.
The incorporation of CosmaNeura's innovative Agentic Platform further enhances this process by leveraging AI solutions to simplify administrative burdens. This allows healthcare providers to focus more on what truly matters: the well-being of their clients. Together, we can create a more compassionate healthcare environment where every detail counts.
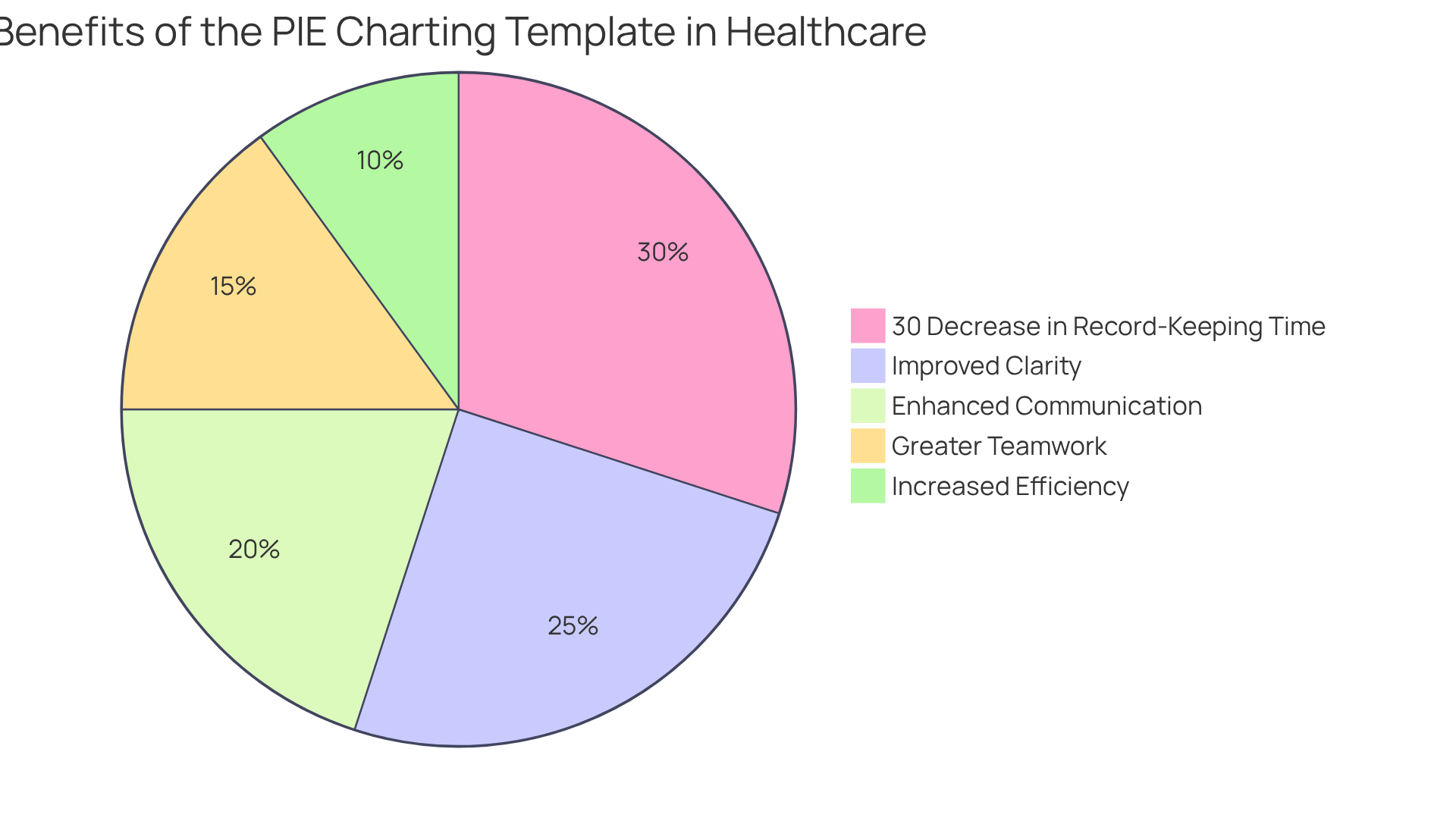
PIE Charting Template: Concise Documentation of Patient Care
The PIE charting template serves as an invaluable resource for healthcare professionals, enabling them to record client issues, actions, and assessments with clarity and precision. Have you ever felt overwhelmed by administrative tasks? This organized method not only improves clarity and efficiency but also allows nurses to swiftly assess the effectiveness of the services they provide. By centering on essential elements of individual support, the PIE template fosters enhanced communication and teamwork among healthcare professionals.
Consider the impact of case studies conducted across various healthcare settings. These studies have shown that utilizing the PIE system simplifies record-keeping and enhances continuity of support, ensuring that all team members remain informed and aligned in their approach. For instance, a case study at a prominent medical facility revealed a remarkable 30% decrease in record-keeping time, allowing caregivers to focus more on meaningful interactions with those receiving care.
As nursing leaders emphasize, clear record-keeping techniques like PIE are crucial for maintaining high standards of client support while alleviating the administrative burden on healthcare providers. Furthermore, the integration of generative AI solutions can significantly enhance the efficiency and accessibility of the PIE system by automating routine tasks. This innovation enables nurses to dedicate more time to the individual needs of their clients.
However, it's essential to acknowledge that the PIE system may inadvertently lead to the neglect of long-term objectives due to the absence of distinct treatment plans. This challenge can complicate the thorough management of individuals. Ultimately, the nurse charting template stands as a valuable tool, promoting better outcomes for individuals through effective record-keeping methods and creative strategies for treatment. How might this tool transform your approach to patient care?
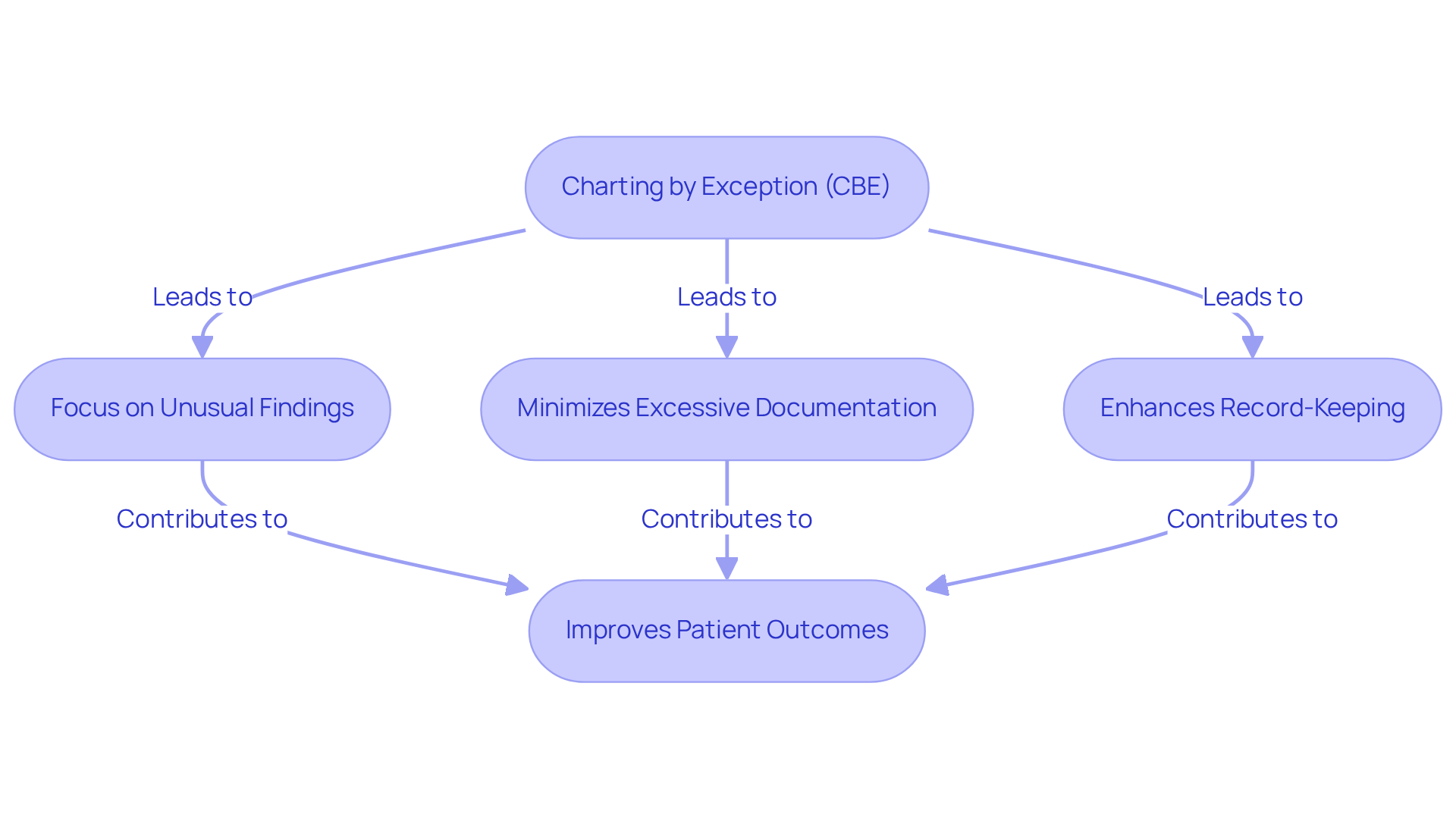
Charting by Exception (CBE) Template: Efficient Documentation for Nurses
Charting by Exception (CBE) is an efficient record-keeping approach that allows caregivers to focus primarily on unusual findings or significant changes in an individual's condition. This focused strategy minimizes excessive documentation, enabling nurses to dedicate more time to direct patient care. By concentrating on exceptions, CBE not only enhances the record-keeping process but also ensures that essential client information is accurately noted.
The effectiveness of CBE is underscored by its ability to alleviate record-keeping burdens. For example, a case study revealed that a patient post-neurosurgery was found in a vegetative state due to a missed brain bleed, linked to inconsistent use of CBE. This highlights the risks associated with inadequate record-keeping practices. When implemented correctly, CBE can lead to improved outcomes for individuals by ensuring that critical deviations from normal findings are promptly addressed.
Healthcare professionals have observed that CBE can promote a more efficient workflow. As one specialist noted, "CBE was created to lessen paperwork, freeing up nurses for more urgent tasks or enabling them to engage more with patients." This sentiment reflects a shared understanding that efficient documentation strategies are vital for enhancing the quality of care. However, it is crucial to recognize that CBE requires well-defined guidelines and standards of practice to be effective.
Moreover, CBE's structured approach enhances communication among healthcare teams. By providing clear instructions on what constitutes normal findings, nurses can quickly identify and report deviations, ensuring that all relevant information is accessible at the patient's bedside. This not only improves continuity of care but also highlights the importance of collaboration in nursing. Each facility has its own standards for defining what is 'normal' for an individual, which is essential for the effective application of CBE.
In conclusion, the CBE method is recognized as a valuable resource for nurses, improving efficiency in record-keeping while prioritizing client well-being. Its implementation can lead to significant enhancements in both job satisfaction and client outcomes, making it an essential strategy in modern nursing practice. Furthermore, the importance of backup records cannot be overlooked, as they provide critical context and evidence in healthcare.
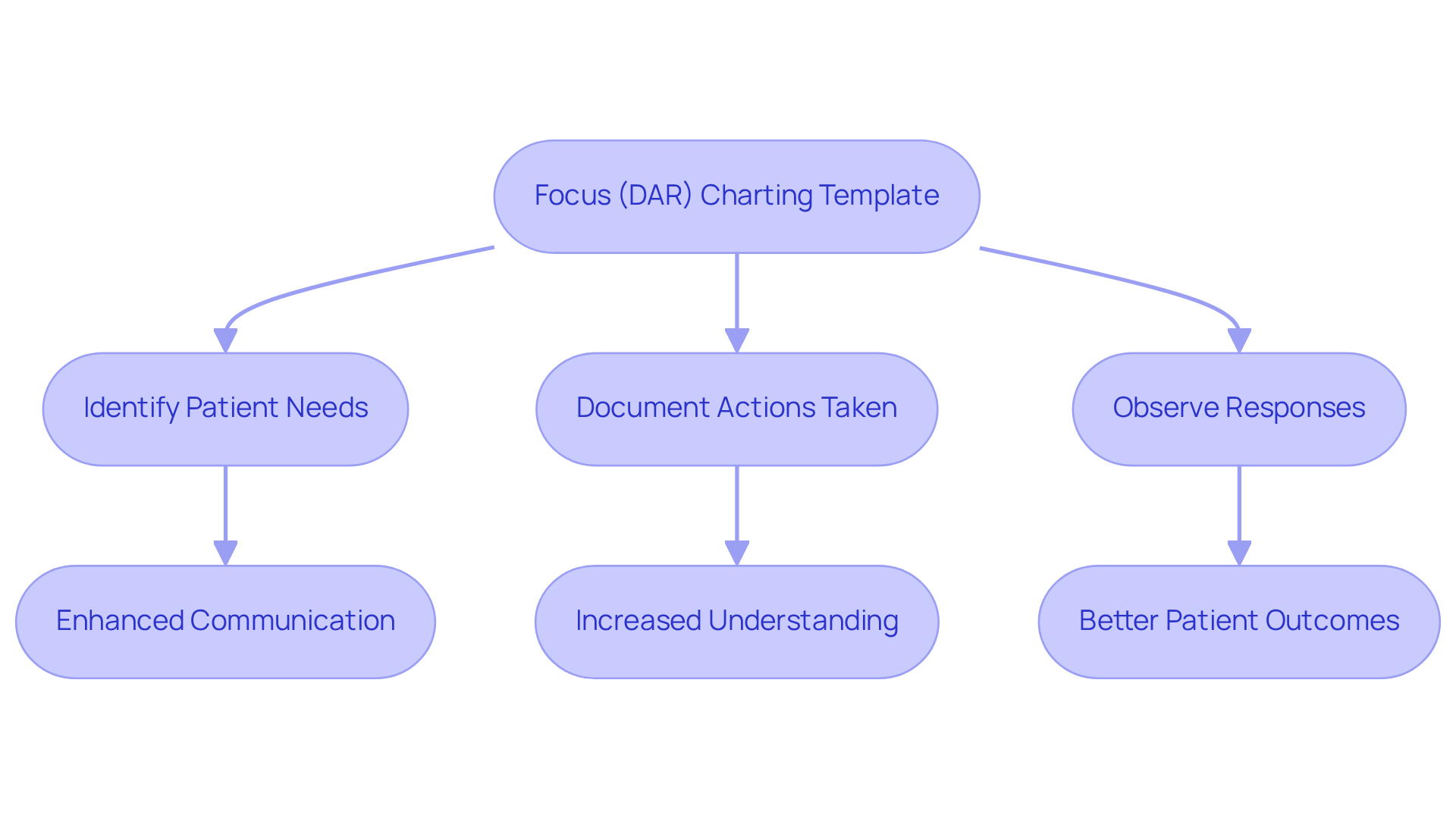
Focus (DAR) Charting Template: Prioritizing Patient Care Documentation
The Focus (DAR) nurse charting template serves as a vital tool for nurses, allowing them to record client support by prioritizing the unique needs and concerns of each individual. This structured approach not only highlights specific issues faced by patients but also details the actions taken by healthcare professionals and the responses observed. Such thorough documentation ensures that records remain relevant and meaningful.
By embracing this patient-centered methodology, we enhance the quality of care provided, fostering improved communication among healthcare providers. Have you ever considered how streamlined documentation can lead to better patient outcomes? Case studies reveal that utilizing the nurse charting template simplifies record-keeping and encourages a deeper understanding of patient conditions, ultimately leading to enhanced clinical results.
The emphasis on patient-oriented documentation is essential, as it aligns with our shared goal of delivering compassionate and effective healthcare. Let us continue to support one another in this journey, ensuring that every patient's voice is heard and valued.
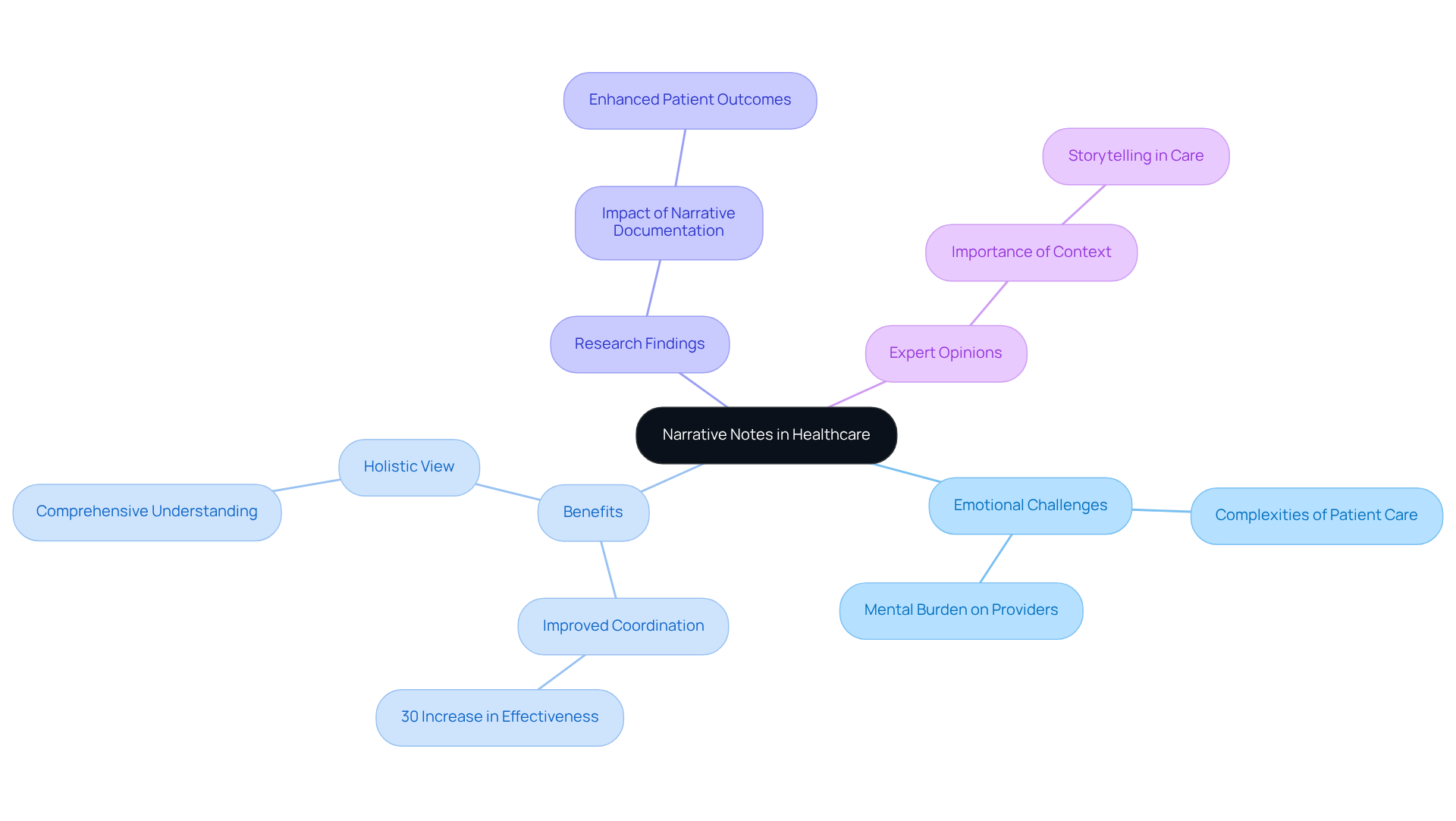
Narrative Notes Template: Detailed Patient Interaction Documentation
Healthcare professionals often face emotional challenges as they navigate the complexities of patient care. The narrative notes template offers a compassionate solution, enabling them to create a comprehensive record of interactions that captures the nuances of support often overlooked by structured templates. This approach is particularly beneficial for documenting intricate cases or significant experiences of individuals.
By providing a thorough account, nurses enhance understanding among the support team, ensuring continuity of assistance. Imagine the difference it could make when everyone involved has a clear picture of the individual's journey. Research shows that comprehensive narrative documentation can lead to improved outcomes, allowing for a more holistic view of each person's experience.
For instance, a study on narrative notes in complex cases revealed that healthcare providers who utilized detailed accounts reported a remarkable 30% increase in coordination effectiveness. This is not just a statistic; it reflects the real impact of storytelling on patient care. Experts in the field emphasize the importance of these detailed individual accounts for informed decision-making. One healthcare professional stated, 'Narrative notes are essential; they provide context that numbers alone cannot convey.' This underscores how vital storytelling records are in enhancing the quality of healthcare.
As we move forward, consider how adopting narrative documentation can transform your practice. It’s not just about the records; it’s about the connections we make and the care we provide. Let’s embrace this compassionate approach together, ensuring every individual’s story is heard and valued.
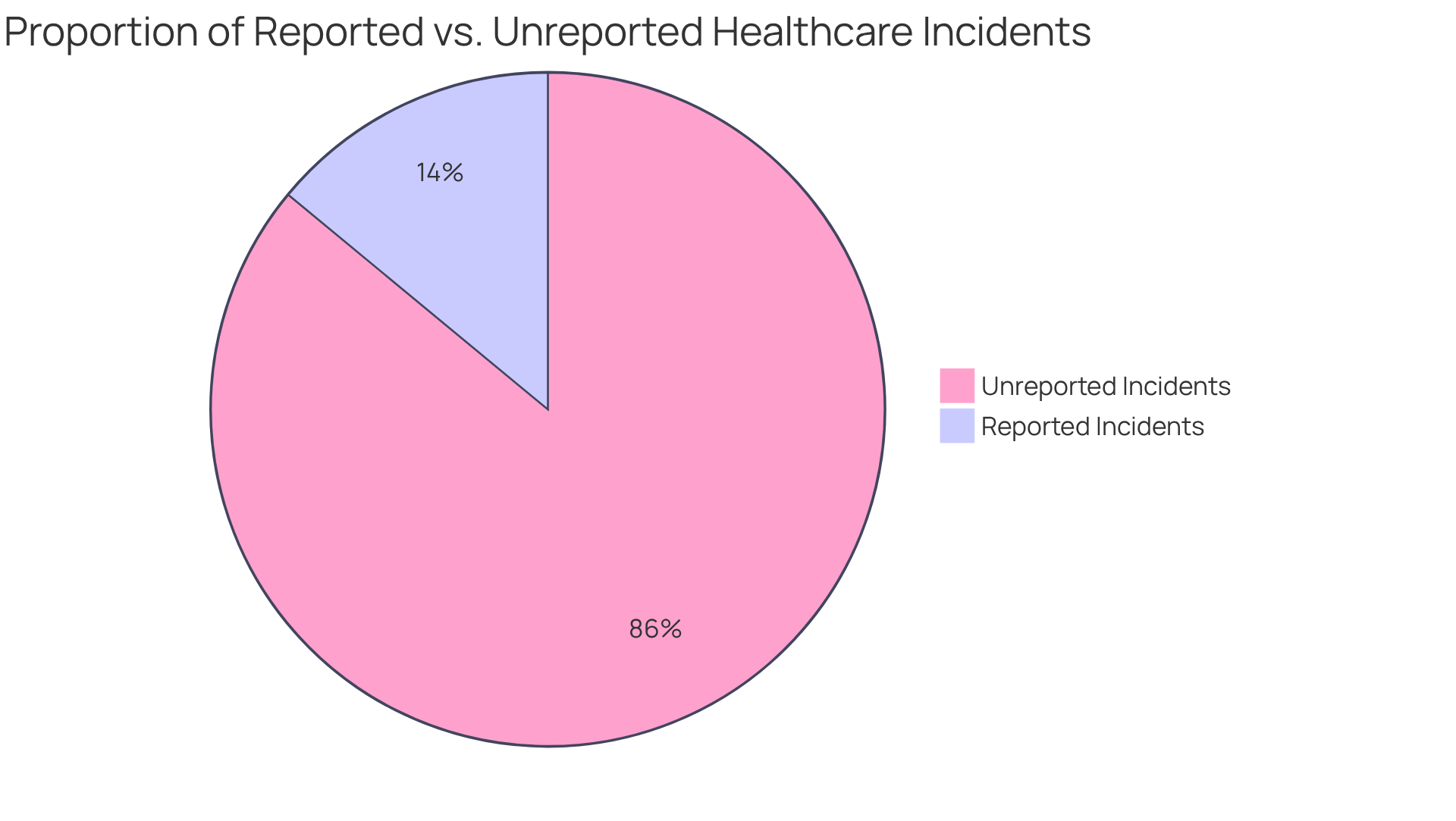
Incident Report Template: Documenting Patient Care Events
The incident report template serves as a vital resource for documenting unforeseen events or negative situations in healthcare. Accurate records are crucial for recognizing trends, implementing corrective actions, and ultimately enhancing patient safety. By carefully capturing incident details, nurses contribute significantly to quality improvement initiatives, ensuring that lessons learned are effectively integrated into future care practices.
Have you ever considered the emotional weight of unreported incidents? Studies reveal that 86% of hospital incidents go unreported, often due to unclear reporting requirements. This underscores the urgent need for comprehensive documentation. In fact, 62% of incidents were deemed non-reportable by staff because of these ambiguous guidelines, highlighting the necessity for improved reporting practices.
Incident reports not only facilitate immediate responses but also play a pivotal role in long-term safety improvements. They inform training sessions and policy updates, fostering a culture of safety. As healthcare leaders emphasize, "Accurate and timely incident reporting is essential for ensuring safety and promoting transparency within healthcare operations."
To effectively document incidents, healthcare providers should follow the 5 W's—Who, What, Where, When, and Why. This approach ensures that all crucial details are covered, ultimately contributing to a safer environment for both patients and providers. Together, we can make a difference in how we approach incident reporting, enhancing the quality of care we provide.
Nursing Progress Notes Template: Tracking Patient Care Over Time
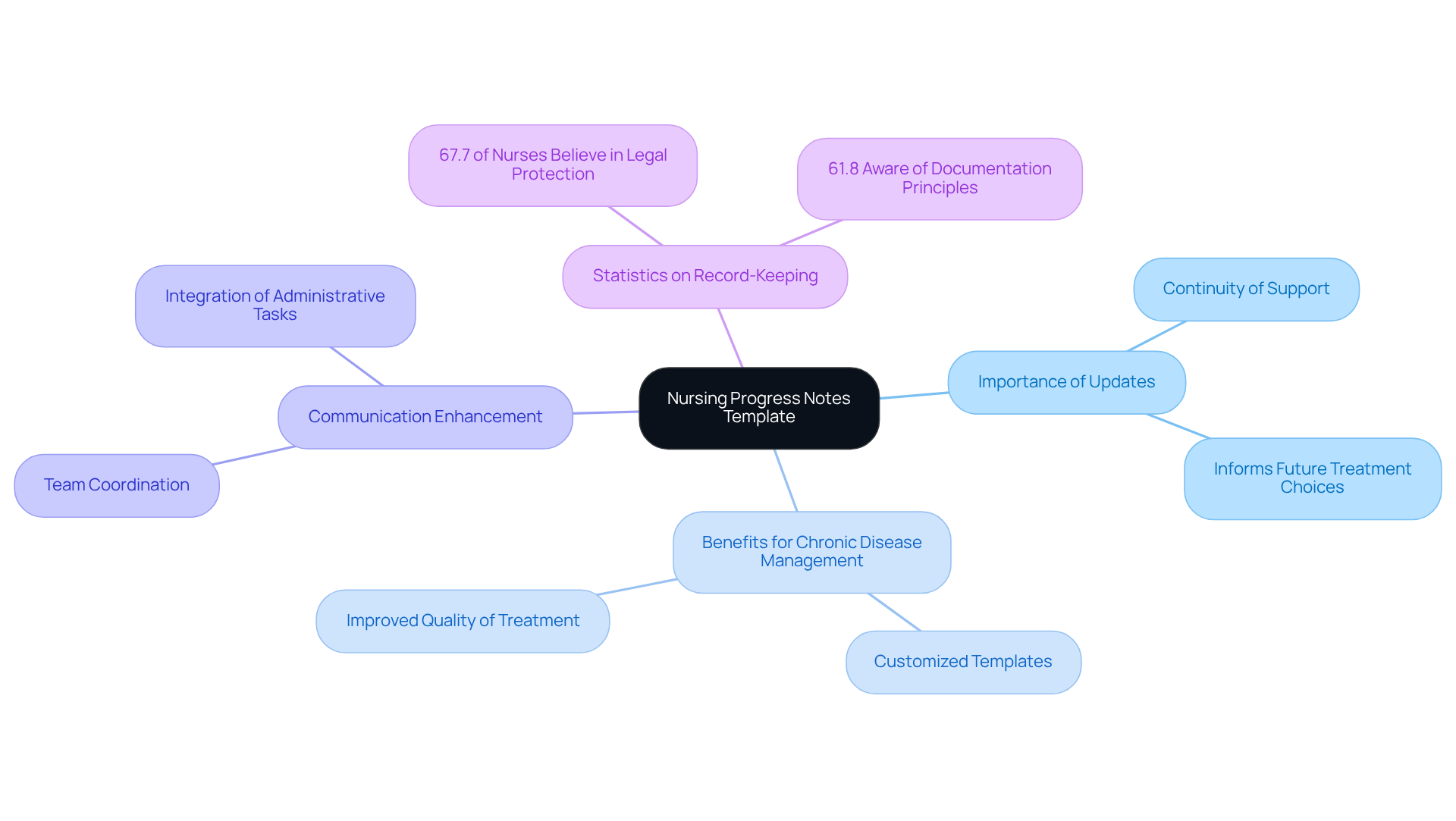
The nursing progress notes template plays a vital role in capturing the ongoing status of patient treatment, providing a holistic view of the patient's journey over time. Have you ever considered how frequent updates to these notes can be essential for ensuring continuity of support? They not only inform future treatment choices but also enhance communication among the healthcare team. Statistics reveal that 67.7% of nurses believe that consistent record-keeping can protect them from legal actions, highlighting the importance of meticulous record maintenance.
Clinicians managing chronic diseases particularly benefit from customized progress note templates. These tailored tools significantly improve the quality of treatment by addressing all relevant aspects of an individual's condition. As Dr. Lisa Gibson wisely notes, effective documentation allows for the seamless integration of administrative tasks into patient interactions, ultimately elevating the quality of service provided. By prioritizing accurate and timely progress notes, healthcare professionals can ensure that individual support remains coordinated and responsive to evolving needs.
Let’s reflect on how we can enhance our documentation practices together. By embracing these strategies, we can foster a more nurturing environment for both patients and providers, ensuring that every individual receives the care they deserve.
Handoff Report Template: Ensuring Effective Communication in Patient Care
Effective communication during transitions of assistance is crucial for healthcare providers. The handoff report template plays a vital role in this process, ensuring that essential client information is communicated clearly to the next caregiver. This organized documentation not only fosters continuity of care but also significantly improves safety. Have you ever considered how miscommunication can impact patient outcomes? Studies reveal that nearly 80% of significant medical mistakes stem from such misunderstandings during transfers.
By utilizing a structured handoff report, nurses can effectively convey essential details—like:
- Illness severity
- Summaries of individuals
- Action lists
- Situational awareness
- Contingency plans
This clarity reduces the risk of errors and enhances overall patient outcomes. For example, implementing the I-PASS handoff program resulted in a remarkable 23% reduction in medical errors and a 30% decrease in preventable adverse events among resident physicians. Isn't it comforting to know that such structured approaches can lead to safer patient care?
As healthcare leaders emphasize, "Excellent verbal communication is key. Aim to always speak with clarity, accuracy, and honesty." This statement underscores the critical role of structured handoff reports in facilitating effective communication. By prioritizing these practices, we can ensure safe, high-quality patient care. Let's work together to enhance our communication strategies and support one another in this vital aspect of healthcare.

Conclusion
In the realm of healthcare, effective documentation is not just important; it is essential for ensuring high-quality patient care. Have you ever felt overwhelmed by the administrative burdens that come with your role? The significance of utilizing nurse charting templates, such as SOAP, DAR, PIE, and others, becomes clear as they streamline the documentation process. By embracing these structured approaches, nurses can enhance communication, improve clinical decision-making, and ultimately devote more time to patient interactions.
These templates promote organization and clarity, significantly reducing record-keeping time. Imagine integrating AI-powered solutions like CosmaNeura to further optimize these processes. This integration allows for more efficient workflows and a better understanding of patient conditions. As healthcare providers increasingly recognize the value of structured documentation, it is evident that these tools are essential for fostering a compassionate and effective healthcare environment.
The journey towards improved documentation practices is a collective effort that can lead to enhanced patient outcomes and greater job satisfaction among healthcare professionals. By adopting these templates and leveraging technology, nurses can transform their approach to patient care, ensuring that every individual's story is heard and valued. Embracing these advancements is not just a step forward; it is a commitment to excellence in healthcare. Let us take this journey together, for the benefit of both patients and providers alike.




