Introduction
Mastering the art of SOAP doctor notes can feel overwhelming for many healthcare professionals. The emotional weight of effective documentation often adds to the already heavy administrative burdens they face. How can we transform this daunting task into a seamless practice that not only eases the workload but also enhances patient care?
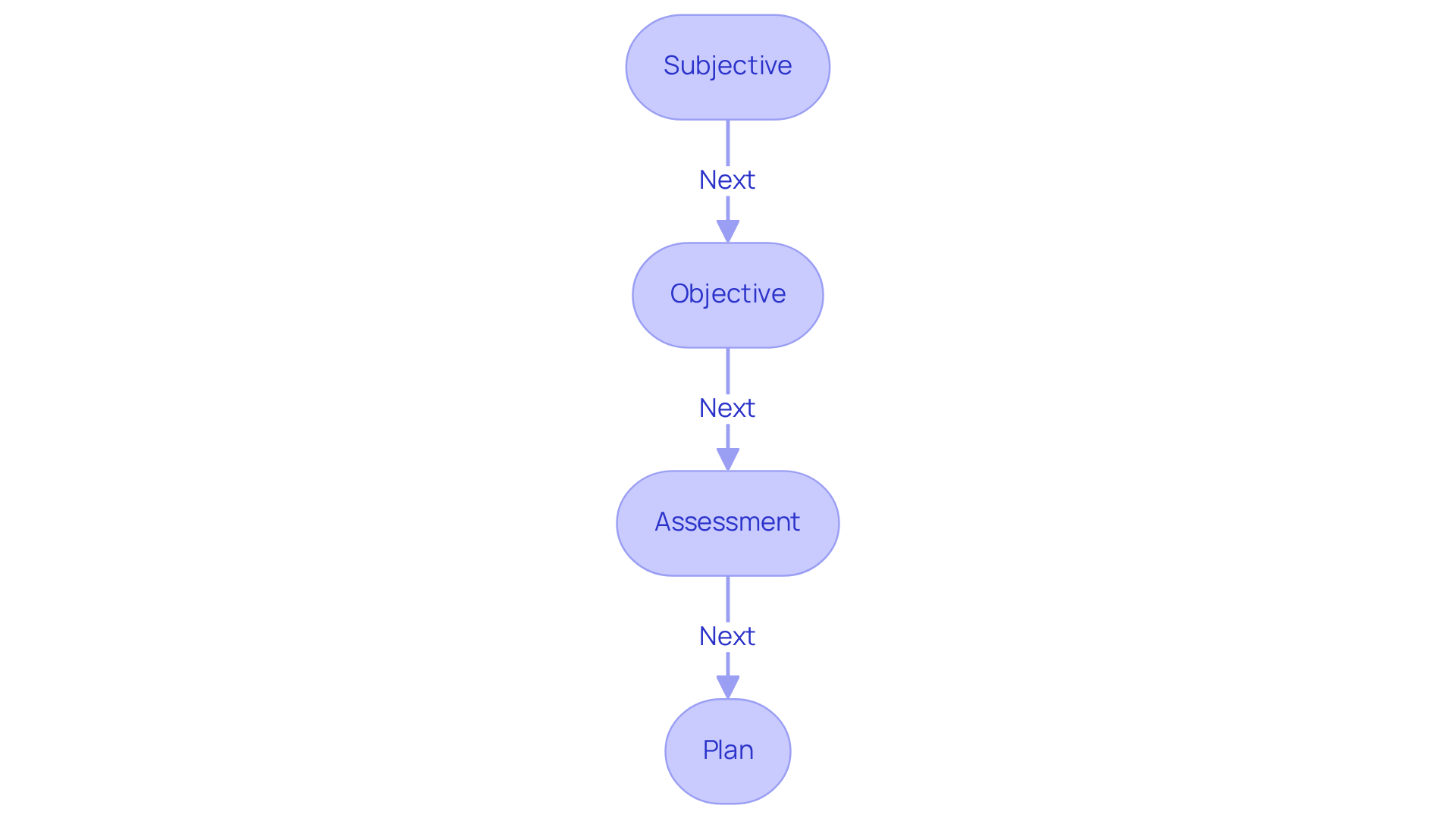
This structured approach - Subjective, Objective, Assessment, and Plan - streamlines the recording process, improves communication, and reduces the risk of errors in patient care. By embracing this framework, healthcare providers can alleviate some of their stress and focus more on what truly matters: their patients.
Here are five key steps to mastering SOAP notes:
- Understand the framework: Familiarize yourself with each component to enhance clarity.
- Practice regularly: Consistent practice leads to confidence and efficiency.
- Seek feedback: Collaborate with colleagues to refine your approach.
- Utilize templates: Simplify the process with structured templates that guide your documentation.
- Reflect on outcomes: Regularly assess how improved documentation impacts patient care.
Exploring these steps reveals a pathway to clearer documentation and better healthcare delivery. By taking action today, you can improve not only your own practice but also the outcomes for your patients.
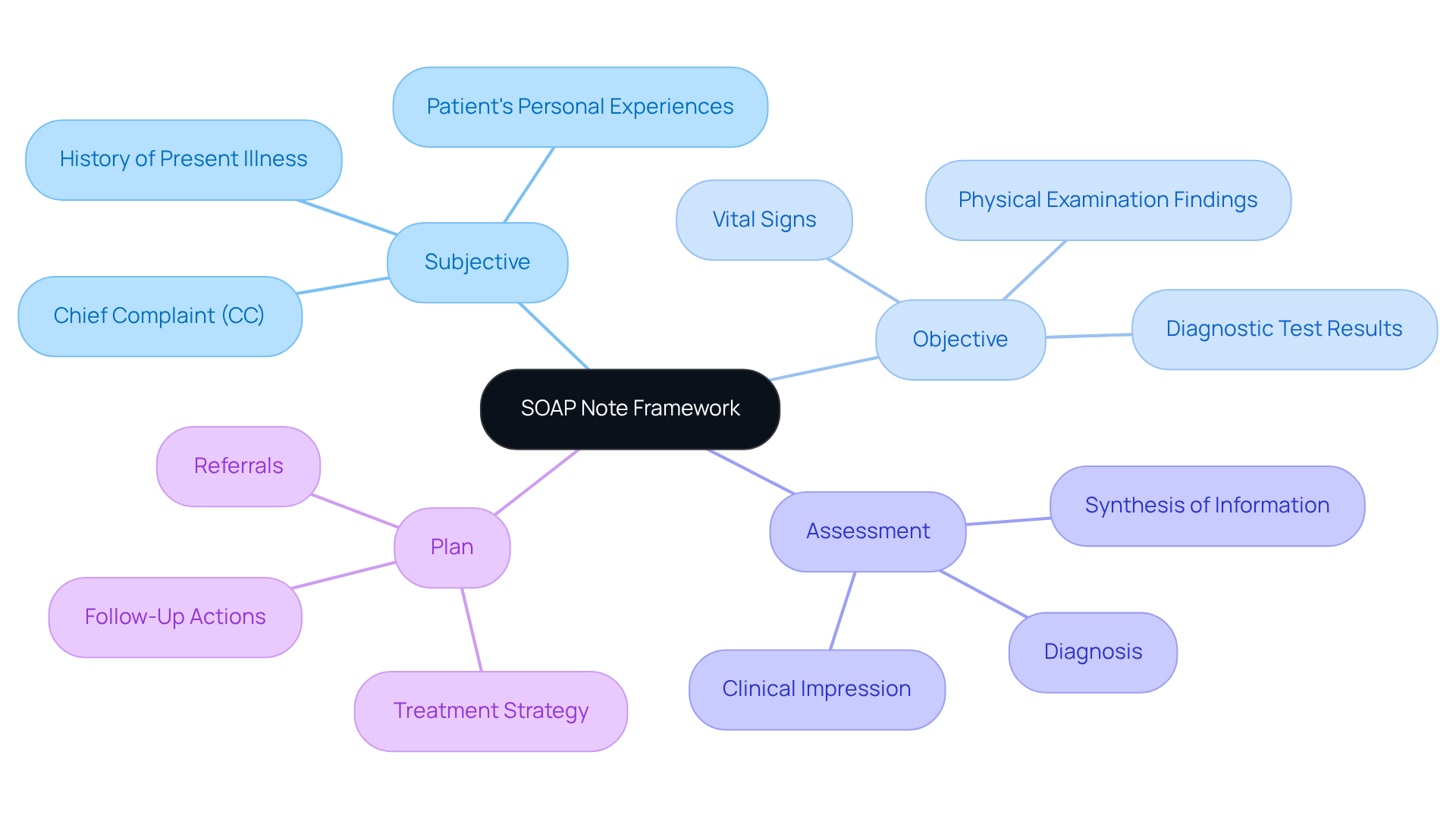
Understand the SOAP Note Framework
Structured notes represent a standardized approach to documentation that healthcare professionals rely on to effectively capture client interactions. Have you ever felt overwhelmed by the sheer volume of information to document? The SOAP acronym - Subjective, Objective, Assessment, and Plan - provides a clear framework that can ease this burden.
- Subjective: This section captures the patient's personal experiences and feelings about their condition, often in their own words. Identifying the Chief Complaint (CC) is crucial here, even if multiple complaints are reported.
- Objective: This part includes measurable data such as vital signs, physical examination findings, and diagnostic test results, providing a factual basis for clinical decisions.
- Assessment: Here, clinicians synthesize the subjective and objective information to formulate a diagnosis or clinical impression, guiding treatment effectively.
- Plan: The final section outlines the proposed treatment strategy, including follow-up actions and referrals, ensuring that all healthcare team members are aligned on the individual's management.
The importance of standardized record-keeping techniques like soap doctor notes cannot be overstated. They enhance communication among healthcare providers, reduce the risk of medical errors, and improve outcomes for individuals. Did you know that a significant percentage of healthcare providers utilize standardized record-keeping methods? This underscores their value in clinical practice. For instance, healthcare experts have noted that using soap doctor notes not only simplifies documentation but also fosters improved client involvement and satisfaction. As Dr. Shelagh Fraser shared, "In the past, I would dedicate 2-2.5 hours preparing records for a complete day of consulting individuals. Now with AI tools, I've got that down to around 40 minutes." This efficiency allows providers to focus more on care, ultimately enhancing the quality of healthcare delivery.
By embracing structured documentation like soap doctor notes, you can alleviate some of the administrative burdens that often weigh heavily on your practice. Imagine the difference it could make in your day-to-day interactions with patients. Let's continue to explore ways to improve our documentation processes together.
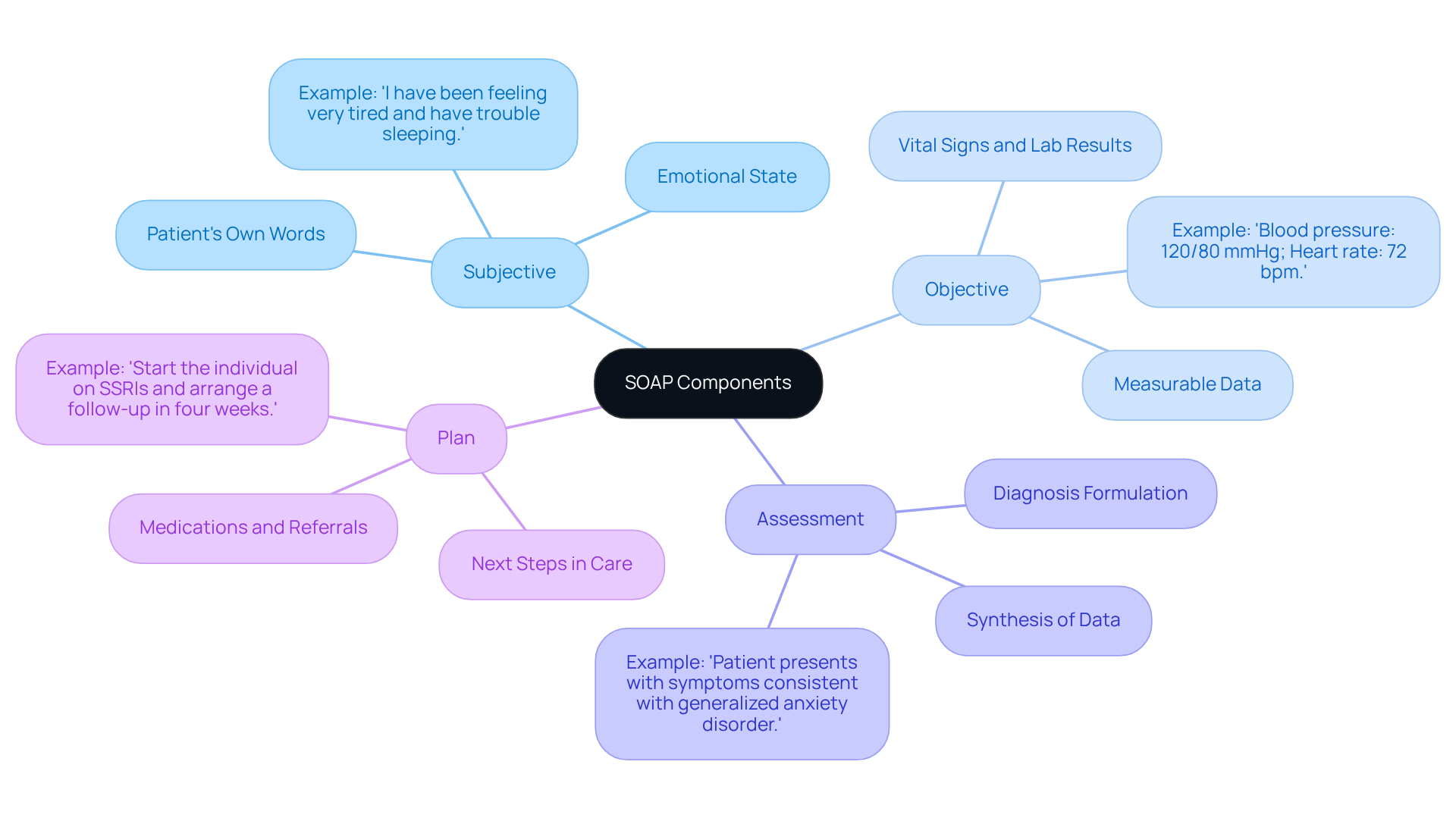
Identify the Components: Subjective, Objective, Assessment, and Plan
Each component of the soap doctor notes plays a vital role in patient care, and understanding them can truly make a difference.
-
Subjective: This section captures the patient's own words about their symptoms, history, and concerns. For instance, someone might say, "I have been feeling very tired and have trouble sleeping." This firsthand account is crucial; it reflects the individual's perspective and emotional state, which are essential for accurate assessment. Have you ever noticed how these personal insights can shape a clinician's understanding? AI algorithms can analyze this subjective data, identifying patterns in individual history and symptoms that enhance clinicians' comprehension of the individual's concerns.
-
Objective: Here, measurable data is documented, including vital signs, lab results, and physical examination findings. For example, one might note, "Blood pressure: 120/80 mmHg; Heart rate: 72 bpm." This objective data provides a factual foundation for clinical decisions and helps monitor the individual's progress over time. Can you see how AI can assist in recognizing trends in this data, such as abnormal vital signs, leading to more precise and timely interventions?
-
Assessment: In this section, the clinician synthesizes the subjective and objective data to formulate a diagnosis. An example could be, "Patient presents with symptoms consistent with generalized anxiety disorder." This analysis is essential for guiding treatment choices and ensuring that care is tailored to the individual's needs. Imagine the support AI can provide by analyzing extensive medical data to assist in making accurate diagnoses, thereby enhancing the reliability of the assessment.
-
Plan: This outlines the next steps in care for individuals, including medications, referrals, and follow-up appointments. For example, one could say, "Start the individual on SSRIs and arrange a follow-up in four weeks." A well-defined plan is crucial for continuity of care and helps establish clear expectations for both the clinician and the individual receiving care. How beneficial would it be if AI could suggest personalized treatment plans based on the analysis of similar cases and outcomes, improving the overall effectiveness of the care plan?
Understanding these elements is essential for developing thorough and impactful soap doctor notes. It not only enhances communication among healthcare professionals but also ensures that care is well-recorded and legally defensible. By incorporating advanced algorithms into the documentation process, healthcare providers can significantly improve diagnostic accuracy and enhance overall outcomes for individuals. Let's embrace these tools to foster better care together.
Write Each Section: Step-by-Step Instructions
To effectively write each section of soap doctor notes, it’s important to approach it with care and understanding. Here’s how you can do it:
-
Subjective:
- Start by asking open-ended questions that invite the patient to share their story. Using their exact words can help you connect better.
- Example: "What brings you in today?"
-
Objective:
- Document measurable data from your examination and tests. Be specific and use standard medical terminology to ensure clarity.
- Example: "Temperature: 98.6°F; Respiratory rate: 16 breaths per minute."
-
Assessment:
- Analyze the subjective and objective data to arrive at a diagnosis. Keep your reasoning concise and clear, focusing on the patient’s needs.
- Example: "The individual’s symptoms and examination findings suggest a diagnosis of acute bronchitis."
-
Plan:
- Outline a thoughtful treatment plan that includes medications, lifestyle changes, and follow-up appointments. Be clear about the next steps to take.
- Example: "Prescribe albuterol inhaler and schedule a follow-up in two weeks to reassess symptoms."
By following these steps, you can create clear and effective documentation, including soap doctor notes, that not only improves patient care but also fosters a supportive environment for healing.
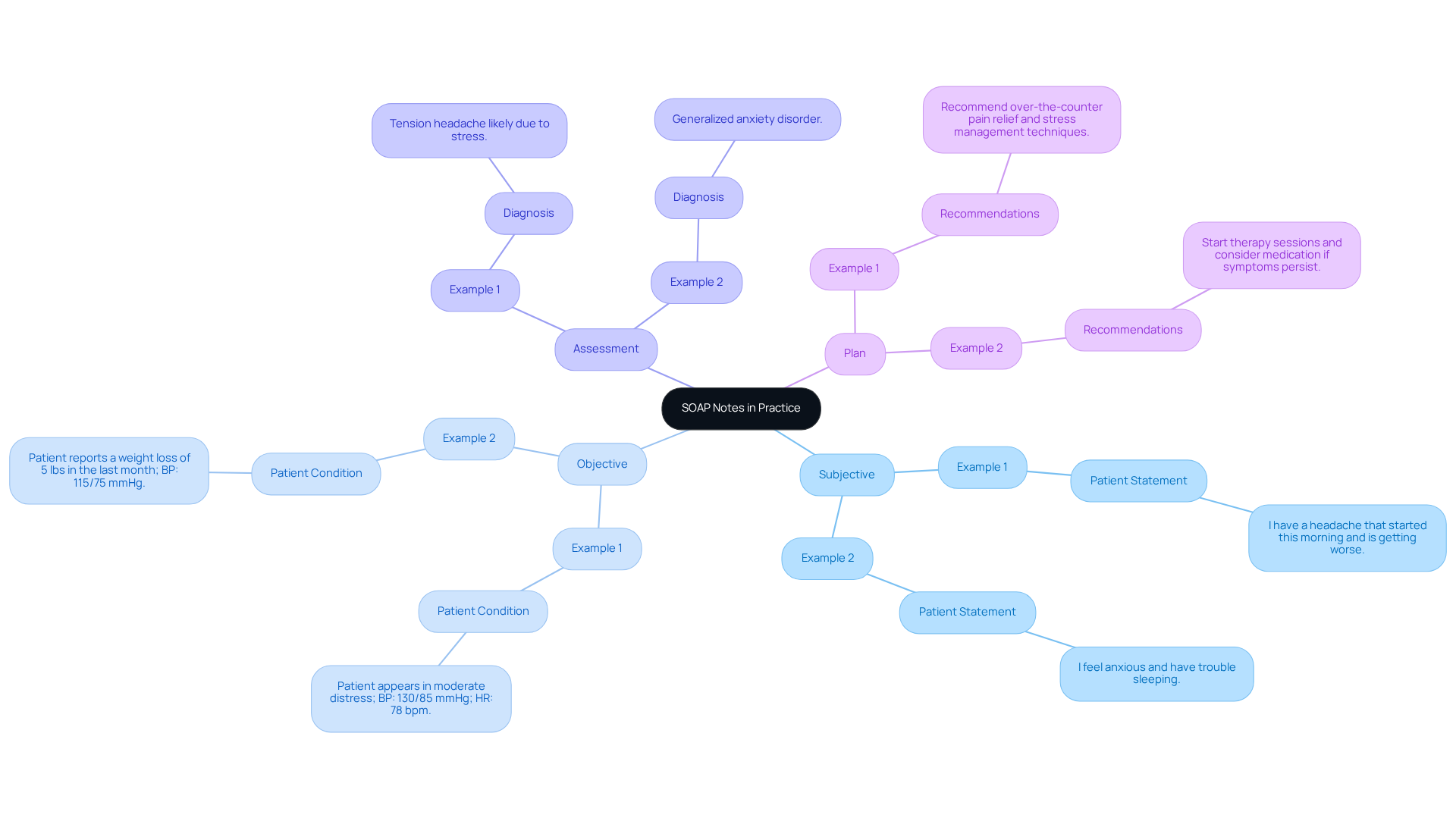
Review Examples of SOAP Notes in Practice
Here are a few examples of SOAP notes that demonstrate effective documentation:
-
Example 1:
- Subjective: "I have a headache that started this morning and is getting worse."
- Objective: "Patient appears in moderate distress; BP: 130/85 mmHg; HR: 78 bpm."
- Assessment: "Tension headache likely due to stress."
- Plan: "Recommend over-the-counter pain relief and stress management techniques."
-
Example 2:
- Subjective: "I feel anxious and have trouble sleeping."
- Objective: "Patient reports a weight loss of 5 lbs in the last month; BP: 115/75 mmHg."
- Assessment: "Generalized anxiety disorder."
- Plan: "Start therapy sessions and consider medication if symptoms persist."
These examples illustrate the organized method of soap doctor notes, which not only improves clarity but also ensures continuity of care.
Why is this important? Efficient record-keeping is essential. Research shows that record errors can lead to serious safety concerns for individuals, with an estimated 1.3 million injuries each year in the USA stemming from such mistakes.
Moreover, involving individuals in examining their records has been shown to enhance accuracy and promote a collaborative approach to care. For instance, individuals who review their records are more likely to identify significant errors, highlighting the necessity of comprehensive documentation.
By adhering to the guidelines in the soap doctor notes, healthcare professionals can greatly enhance the quality of care and reduce the likelihood of mistakes.
What can you do? Consider reviewing your documentation practices today. Together, we can foster a safer and more effective healthcare environment.
Troubleshoot Common Issues in SOAP Note Writing
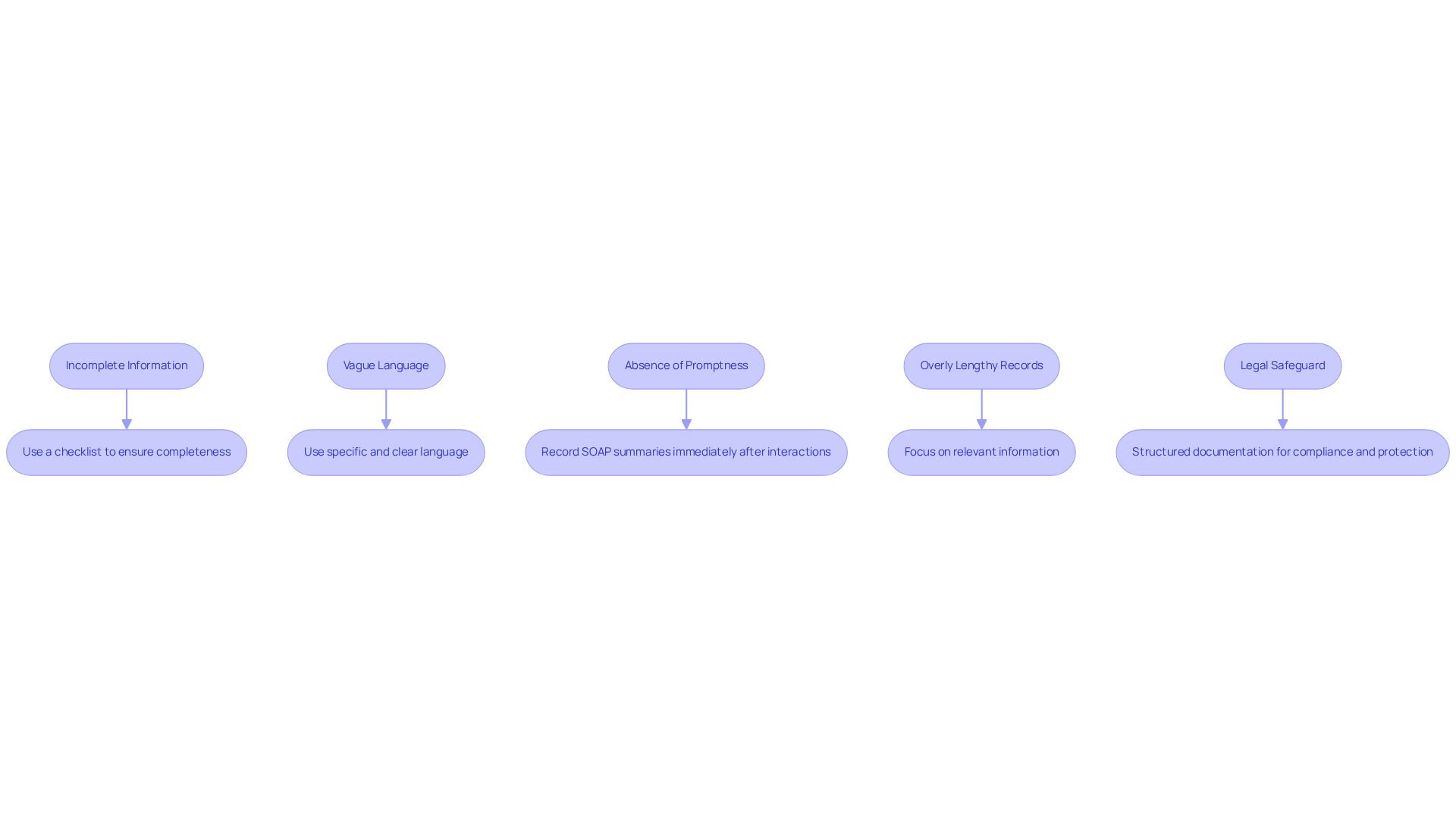
Common issues in SOAP doctor notes writing can be quite challenging for healthcare providers.
-
Incomplete Information: When sections are left unfilled, it can create gaps that negatively impact the care provided to individuals.
- Solution: Consider using a checklist to ensure every component is addressed before finalizing the note. This simple step can enhance thoroughness and compliance, making a significant difference in patient care.
-
Vague Language: Ambiguous terms can lead to misinterpretation and confusion, which no one wants in a healthcare setting.
- Solution: Aim for specific and clear language. For instance, instead of saying 'the individual is feeling bad,' specify 'the individual reports a pain level of 7 out of 10.' This provides measurable data that can guide treatment decisions.
-
Absence of Promptness: Delaying records increases the risk of overlooking important details or confusing individuals, which can jeopardize precision.
- Solution: Try to record SOAP summaries right after client interactions. This practice captures precise information and minimizes mistakes, ultimately enhancing the quality of care.
-
Overly Lengthy Records: Including too much information can clutter the record and obscure key details.
- Solution: Focus on relevant information that directly influences care and treatment decisions. This ensures clarity and keeps the attention on what truly matters.
-
Legal Safeguard: Structured documentation not only supports compliance but also offers legal protection for healthcare professionals, ensuring that accurate records are maintained for reimbursement objectives.
By recognizing these common challenges and implementing the suggested solutions, healthcare providers can significantly improve the quality and effectiveness of their SOAP doctor notes. This, in turn, enhances patient outcomes and supports regulatory compliance. Additionally, utilizing tools like HealthOrbit AI's smart templates and compliance checks can streamline the documentation process, ensuring that notes are both accurate and well-structured.
How can you start making these changes today?
Conclusion
Mastering the SOAP note framework is essential for healthcare professionals who want to improve their documentation practices. Have you ever felt overwhelmed by the administrative burdens that can distract from patient care? By understanding and implementing the structured approach of Subjective, Objective, Assessment, and Plan, providers can streamline their record-keeping, ultimately enhancing communication and patient care. This methodology not only simplifies the documentation process but also fosters a more collaborative environment between healthcare teams and patients.
Each component of the SOAP note plays a vital role. Subjective insights, objective data, thorough assessments, and clear plans all contribute to effective treatment strategies. Here are some practical steps to consider for writing each section:
- Subjective: Gather patient insights and concerns.
- Objective: Document measurable data and observations.
- Assessment: Analyze the information to form a diagnosis.
- Plan: Outline the next steps for treatment.
Avoiding common pitfalls ensures that healthcare professionals can create comprehensive and legally defensible records. The integration of technology, such as AI tools, further enhances the ability to make accurate diagnoses and develop personalized treatment plans, showcasing the evolving landscape of healthcare documentation.
In summary, adopting the SOAP note framework is not just about improving documentation; it’s about elevating the quality of care provided to individuals. By embracing these practices and continuously refining documentation skills, healthcare professionals can significantly reduce errors, enhance patient safety, and ultimately contribute to better health outcomes.
So, what’s next? It’s time to take action. Review your current documentation practices, implement the strategies discussed, and commit to mastering SOAP notes for a more effective healthcare delivery system. Together, we can make a difference in the lives of our patients.




