Overview
In the demanding world of healthcare, writing effective nurse SOAP notes can often feel overwhelming. This article presents a structured approach that emphasizes the four essential components: Subjective, Objective, Assessment, and Plan. By understanding how each section contributes to comprehensive patient care, healthcare providers can alleviate some of the administrative burdens that impact their ability to connect with patients.
Imagine how much smoother communication among healthcare providers can be when each note is clear and concise. This framework not only enhances collaboration but also leads to better patient outcomes. By focusing on these key elements, nurses can improve their documentation practices, ultimately fostering a more nurturing environment for their patients.
The structured approach outlined here encourages you to reflect on your current practices. Are there moments when the complexity of documentation feels like a barrier to providing the compassionate care your patients deserve? Embracing this framework can empower you to navigate these challenges with greater ease.
By adopting this method, you can enhance your documentation skills while ensuring that your patients receive the attentive care they need. Let’s take this step together towards more efficient and effective patient care.
Introduction
In the realm of healthcare, effective documentation is not just a bureaucratic necessity; it is a cornerstone of quality patient care. This understanding can be overwhelming for many healthcare providers. The SOAP note framework—encompassing Subjective, Objective, Assessment, and Plan—serves as a vital tool for nurses, transforming the way patient interactions are recorded and understood. By mastering this structured approach, healthcare providers can enhance communication and improve patient outcomes.
Yet, the challenge remains: how can one ensure that each SOAP note is not only comprehensive but also reflective of the patient’s unique journey? Administrative burdens can often feel like an insurmountable barrier to providing the best care. It’s essential to recognize these challenges and seek solutions that allow for a more compassionate approach to documentation.
Imagine a world where each note not only captures clinical details but also tells the story of the patient’s journey. This is possible through effective use of the SOAP framework. By embracing this method, you can navigate the complexities of clinical documentation with confidence, ultimately fostering a deeper connection with your patients. Let’s explore how you can make your documentation not only effective but also meaningful.
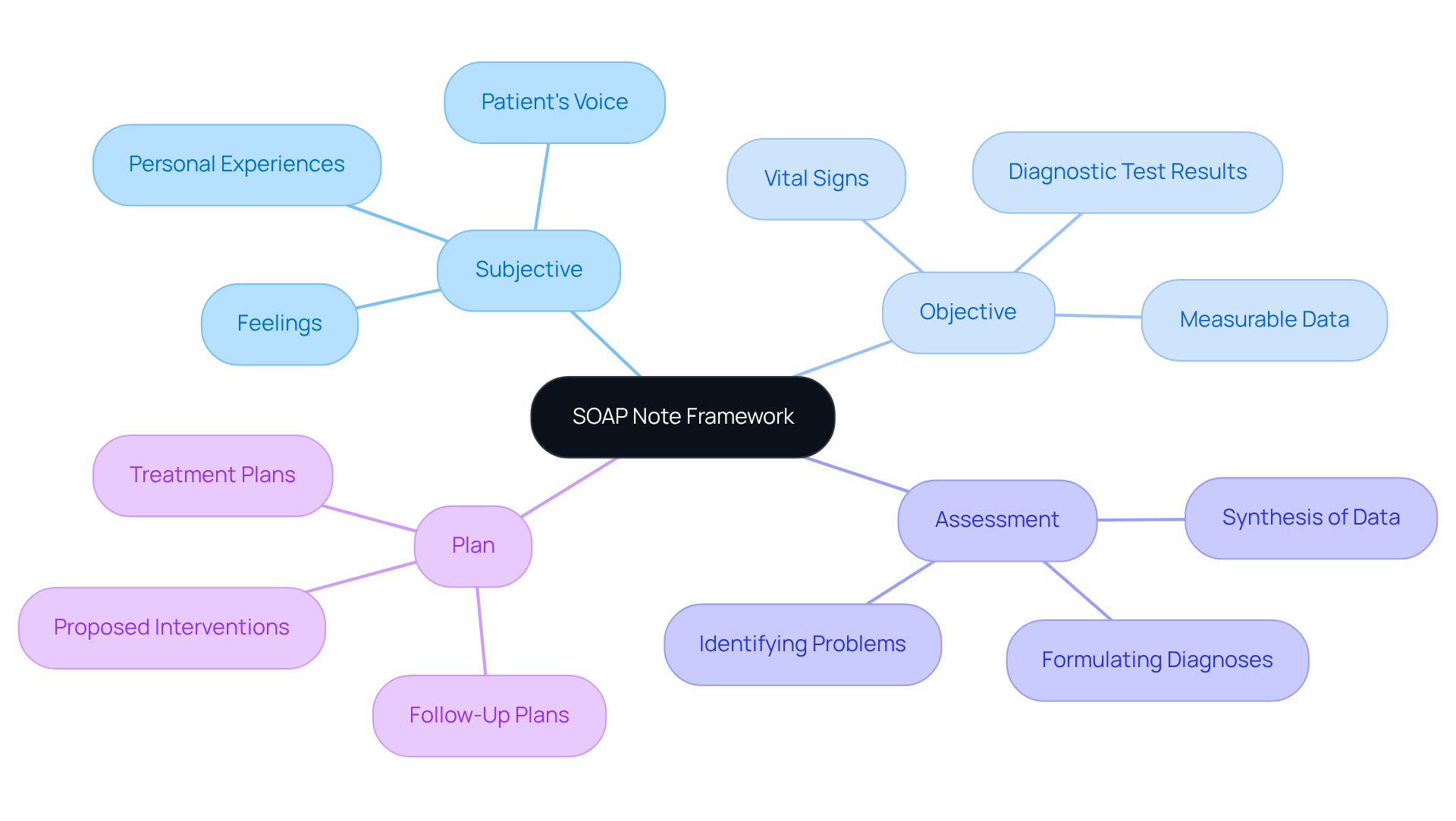
Understand the SOAP Note Framework
In the fast-paced world of healthcare, the nurse soap note framework serves as a beacon of clarity and support in documentation. Comprising four essential components—Subjective, Objective, Assessment, and Plan—this structure is not just a guideline but a lifeline for effective patient care.
- Subjective (S): Here, we listen to the patient’s voice, capturing their personal experiences, feelings, and concerns in their own words. This section is vital, offering crucial context that helps healthcare providers understand the individual’s unique perspective, fostering a compassionate approach to care.
- Objective (O): This segment provides measurable and observable data—think vital signs and diagnostic test results. It lays down the factual foundation that supports clinical decision-making, ensuring that assessments are rooted in objective evidence, which is essential for building trust and confidence in care.
- Assessment (A): Within this section, healthcare providers synthesize the subjective and objective data to formulate diagnoses or identify problems. This process showcases the clinician's reasoning and judgment, key elements in managing individual care effectively and compassionately.
- Plan (P): The final piece outlines proposed interventions, treatments, and follow-up plans derived from the assessment. It serves as a roadmap for future care, ensuring continuity and coherence in managing individuals’ health journeys.
Understanding this structure is crucial for crafting , enhancing care, and promoting effective communication among healthcare providers. Research shows that organized records can improve the quality of electronic health entries significantly—by 12.8 points—underscoring their importance in clinical practice. Moreover, healthcare professionals who consistently use structured formats report better patient outcomes and greater satisfaction with their documentation practices.
Notably, 75% of mentors require students to write clinical summaries during Advanced Pharmacy Practice Experiences (APPEs), highlighting the prevalence and importance of this format in healthcare education. While clinical documentation is widely practiced, it’s essential to acknowledge its limitations, such as the challenge of capturing changes over time. In specific clinical situations, alternative formats like DAP and BIRP records may also be beneficial.
By embracing the nurse soap note framework, we can reduce some of the administrative burdens that heavily impact healthcare providers, ultimately enhancing the quality of care we provide to our patients. Let’s continue to support one another in this journey, ensuring that our documentation practices reflect the compassion and dedication we strive to provide in every patient interaction.
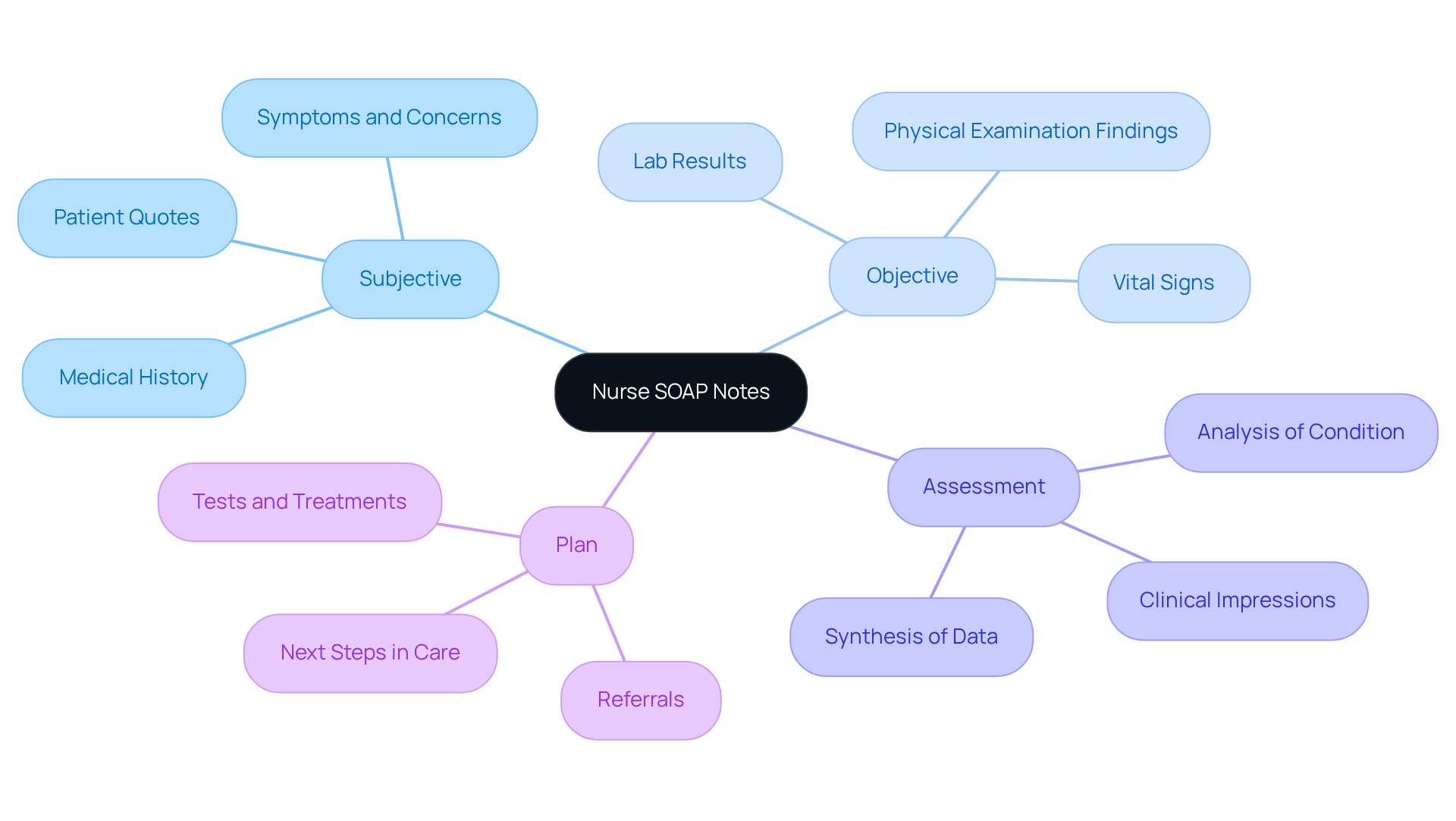
Identify the Key Components: Subjective, Objective, Assessment, and Plan
Writing effective is not just a task; it’s a vital part of providing compassionate care. Understanding the specific elements that make up each component is essential for healthcare providers who strive to support their patients fully.
- Subjective: This section captures the patient’s direct quotes regarding their symptoms, concerns, and medical history. For instance, when a patient says, "I have been feeling dizzy for the past three days," it offers valuable insight into their experience, guiding further assessment and understanding.
- Objective: Documenting measurable data in this section is crucial. This includes vital signs, lab results, and physical examination findings. For example, writing down "Blood pressure: 120/80 mmHg; Heart rate: 72 bpm" provides solid evidence of the individual’s current health, assisting in informed clinical decision-making.
- Assessment: Here, a clear and concise analysis of the individual’s condition is provided based on the subjective and objective data. An example could be, "Patient presents with symptoms consistent with dehydration," which synthesizes the gathered information and informs the next steps in care.
- Plan: This outlines the subsequent steps in the individual's care, including tests, treatments, or referrals. For instance, stating, "Administer IV fluids and re-evaluate in 2 hours" ensures a clear direction for ongoing management, fostering a sense of security for both the provider and the patient.
The structured format, created by Dr. Lawrence Weed in the 1960s, has been widely embraced in healthcare for its organized approach to record-keeping, fostering clear communication among providers. By carefully identifying and recording these components, healthcare providers can create thorough and effective nurse soap notes that significantly enhance patient care and support clinical reasoning. However, it is important to be mindful of common errors such as vague assessments or irrelevant information, which can undermine the effectiveness of documentation. Remember, the objective information gathered serves a crucial function in clinical decision-making, emphasizing its significance in this format.
Reflecting on these practices can enhance the quality of care provided, ensuring that every patient feels heard and valued.
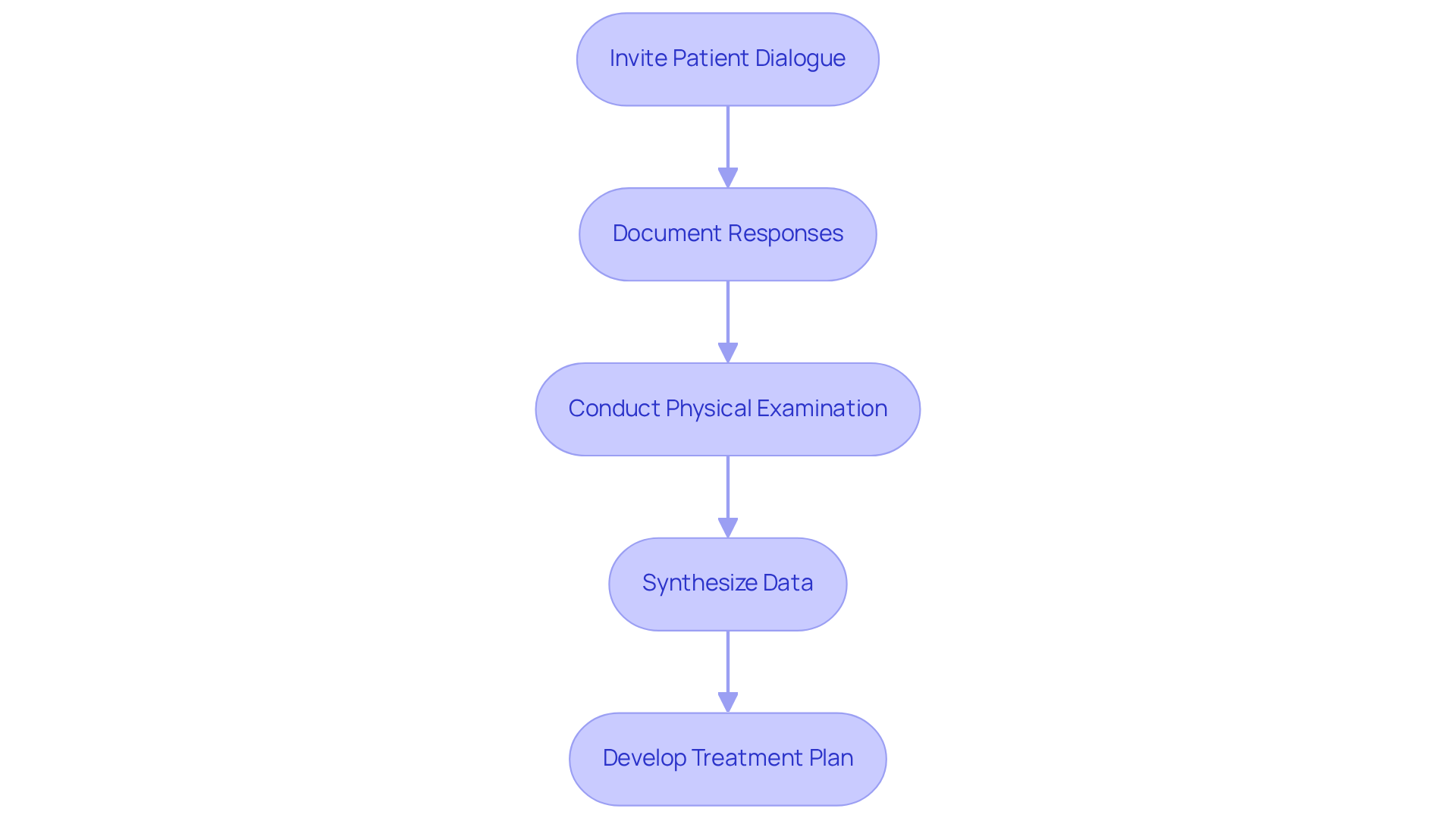
Follow a Step-by-Step Process to Write Each Section
To effectively write each section of a nurse soap note, it is important to approach the task with care and compassion. Begin by inviting your patients to share their feelings and experiences through open-ended questions. For example, you might ask, "Can you describe how you've been feeling lately?" This not only encourages dialogue but also helps you capture their words verbatim, ensuring their voices are accurately reflected.
As you document their responses, remember to summarize any pertinent medical history or previous treatments that may influence the current visit. This context is vital for your assessment, and distinguishing between symptoms and signs can significantly impact your overall evaluation.
Next, conduct a thorough physical examination and organize your findings clearly. Including vital signs and relevant laboratory or imaging results will provide a comprehensive view of the individual's condition. Use precise and straightforward language to describe observable data, steering clear of ambiguity.
In the assessment phase, take the time to synthesize the subjective and objective data. Formulating a diagnosis or identifying significant issues requires clear articulation of your clinical reasoning and any differential diagnoses considered. This transparency fosters trust and understanding.
Finally, develop a detailed treatment plan that encompasses medications, referrals, and follow-up appointments. Ensure that your plan is specific, actionable, and tailored to the unique needs of each individual, facilitating effective care.
By following these steps, you can create thorough and effective nurse soap notes that enhance patient care and communication among healthcare teams. The structure developed in the 1950s by Lawrence Weed is an essential resource for healthcare professionals. Additionally, the APSO sequence (Assessment, Plan, Subjective, Objective) has shown improvements in efficiency and practicality in record-keeping. Remember, timely documentation is crucial for maintaining accuracy and continuity of care.
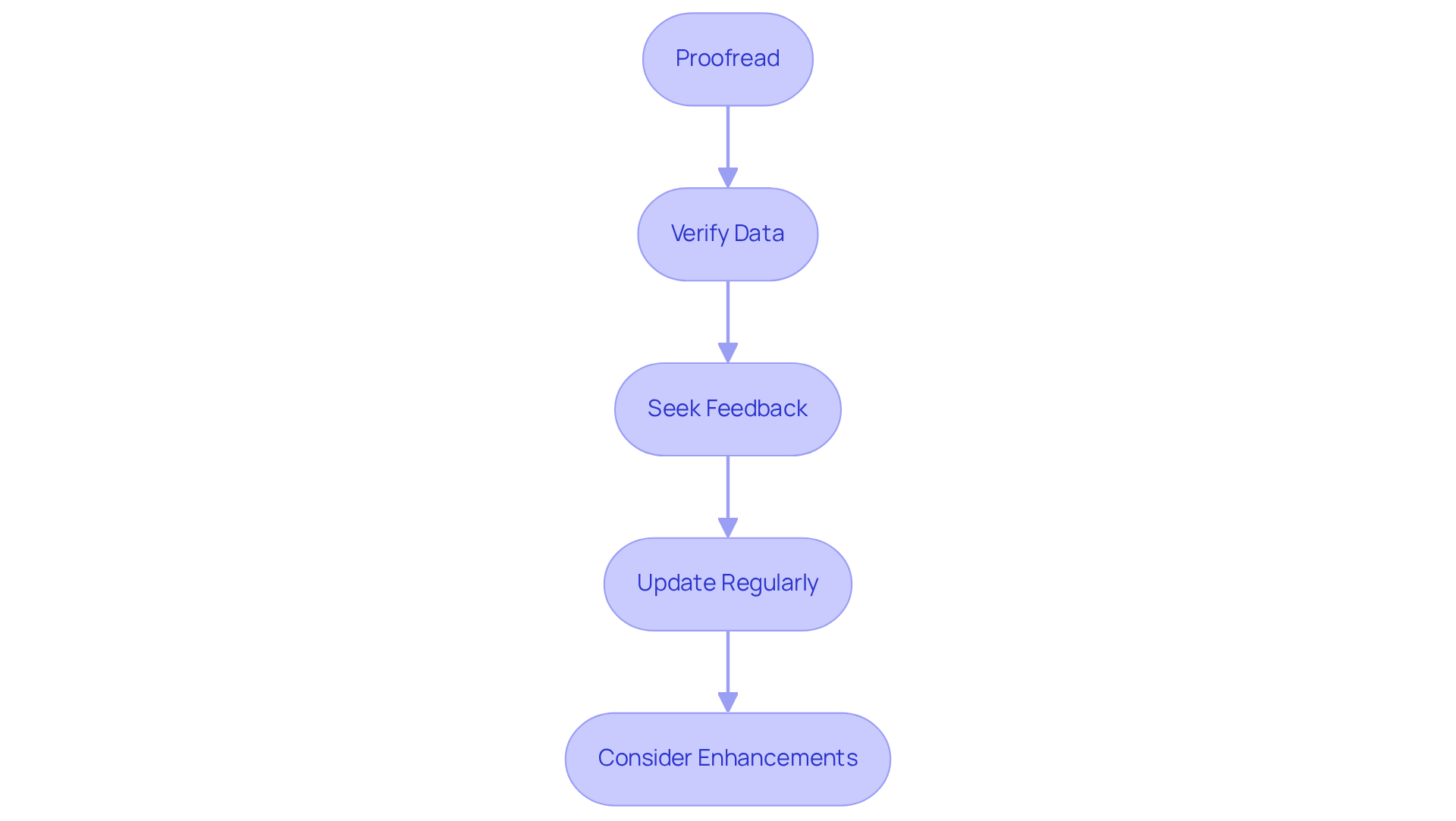
Review and Refine Your SOAP Notes for Accuracy
To ensure the accuracy and effectiveness of your SOAP notes, it's important to follow these essential review and refinement steps:
- Proofread: Take a moment to carefully read through your SOAP notes for any spelling and grammatical errors. Clear and professional documentation is not just a formality; it reflects the quality of care you provide, which is vital in healthcare.
- Verify Data: Cross-check the subjective and objective information against the individual's records. This step is crucial to , as discrepancies can lead to misunderstandings in patient care, which we all want to avoid.
- Seek Feedback: If possible, consider having a coworker examine your records for clarity and completeness. A fresh perspective can catch errors you might have overlooked, significantly enhancing the overall quality of your documentation. In fact, a survey revealed that 62% of ambulatory care preceptors stress the importance of precise documentation, highlighting the value of peer evaluation.
- Update Regularly: As new information arises or the individual's condition changes, make it a practice to update your SOAP notes accordingly. This ensures your records reflect the most current data, which is crucial for maintaining precise and pertinent client records, in line with ethical standards in record-keeping.
- Consider Enhancements: After each client interaction, take a moment to reflect on your recording process. Think about what worked well and what might be enhanced for future documentation. Ongoing improvement in record-keeping methods is essential for providing efficient care to individuals.
By implementing these review and refinement practices, you can significantly enhance the quality of your nurse SOAP notes. Additionally, leveraging AI tools, such as those offered by CosmaNeura, can help streamline the documentation process, ensuring adherence to ethical standards while improving patient outcomes and satisfaction.
Conclusion
Embracing the nurse SOAP note framework is essential for enhancing patient care and ensuring effective communication within healthcare teams. This structured approach—comprising Subjective, Objective, Assessment, and Plan—not only streamlines documentation but also fosters a compassionate understanding of each patient's unique experience. By integrating these elements, healthcare providers can create thorough records that support clinical reasoning and promote better patient outcomes.
Throughout the article, we discussed key insights that emphasize the importance of each SOAP note component. The Subjective section captures the patient's voice, while the Objective segment provides measurable data that grounds clinical assessments. The Assessment synthesizes this information, and the Plan outlines actionable steps for future care. These components work together to facilitate clear communication and effective decision-making, ultimately enhancing the quality of care delivered.
In conclusion, the significance of meticulous documentation cannot be overstated. By following best practices in crafting and reviewing SOAP notes, healthcare professionals can ensure accuracy and clarity in their records. This commitment to excellence not only benefits individual patient interactions but also strengthens the overall healthcare system. Embracing the SOAP note framework is a call to action for all healthcare providers to reflect on their documentation practices, continuously improve, and prioritize the compassionate care that every patient deserves.




