Overview
The article titled "10 SOAP Method Medical Examples to Enhance Your Documentation" addresses the emotional challenges healthcare providers face in their daily practices. Are you feeling overwhelmed by the administrative burdens that can detract from patient care? You’re not alone. Many healthcare professionals struggle with documentation that feels tedious and time-consuming, impacting their ability to focus on what truly matters—providing excellent patient care.
Utilizing structured SOAP notes can be a game-changer. By adopting this method, you can enhance communication among healthcare providers, ensuring that everyone is on the same page. Imagine the clarity in care plans and the improved coordination among specialists. This structured approach not only streamlines documentation but also fosters a collaborative environment that benefits both providers and patients.
Here are some key benefits of using the SOAP method:
- Improved clarity in care plans, making it easier for all team members to understand patient needs.
- Enhanced communication among specialists, leading to better coordinated care.
- Increased efficiency in documentation, allowing you to spend more time with your patients.
As you consider implementing the SOAP method, think about how it can alleviate some of the pressures you face. Wouldn’t it be wonderful to have a system that supports your efforts and enhances patient care? By embracing this structured approach, you can transform your documentation practices and ultimately improve the quality of care you provide.
Take the first step towards better documentation today. Explore the SOAP method and see how it can make a difference in your practice. Your patients deserve the best, and so do you.
Introduction
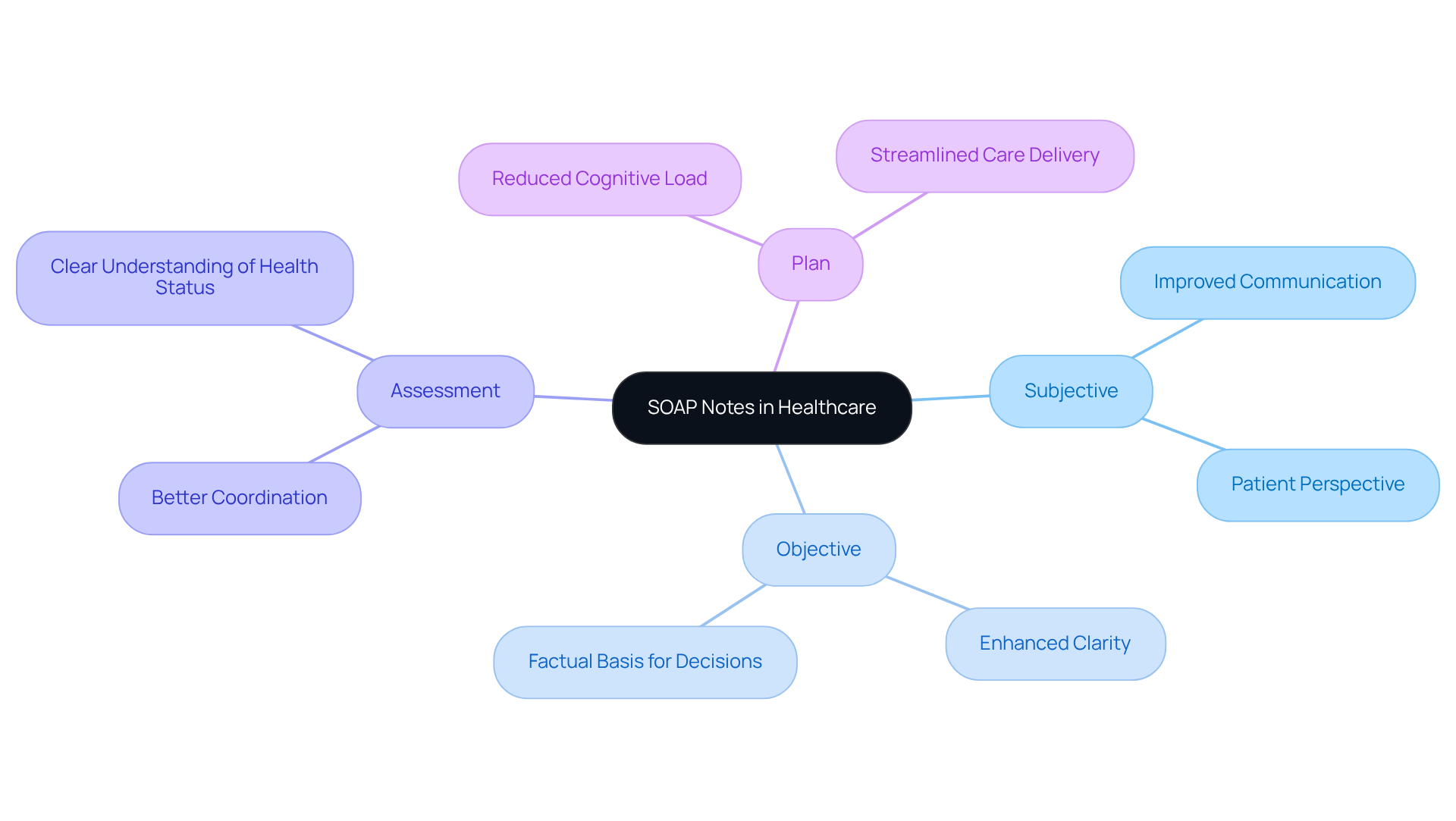
Healthcare professionals often face the emotional strain of balancing quality patient care with the demands of extensive documentation. It’s a tough situation, isn’t it? The SOAP method—Subjective, Objective, Assessment, and Plan—offers a structured way to ease this burden. But how can providers truly implement it to enhance their practice and alleviate some of that stress?
This article explores ten compelling examples of SOAP notes that not only illustrate best practices but also showcase the potential of innovative tools and templates. By diving into these examples, healthcare providers can uncover strategies to improve their documentation efficiency. Imagine the relief of spending less time on paperwork and more time with patients, ultimately leading to better outcomes.
Here are some key benefits of utilizing the SOAP method effectively:
- Streamlined documentation processes
- Enhanced clarity in patient assessments
- Improved communication among healthcare teams
By embracing these strategies, you can transform your practice. Let’s take a closer look at how these examples can inspire you to elevate your documentation and, in turn, your patient care.
CosmaNeura: Streamline SOAP Note Documentation with AI-Powered Efficiency
Healthcare providers often face overwhelming administrative burdens that can detract from their ability to deliver quality care. Have you ever felt that the time spent on record-keeping takes away from meaningful interactions with your patients?
CosmaNeura understands these challenges and offers a solution. By utilizing advanced AI technology, it automates the generation of SOAP method medical example notes, significantly reducing the time you spend on documentation. This innovation allows you to focus on what truly matters—providing compassionate care to individuals in need.
With CosmaNeura, you can expect:
- Faster note creation that adheres to best practices in clinical records.
- Improved accuracy and compliance, ensuring that your documentation meets necessary standards, is illustrated by a soap method medical example.
- Enhanced efficiency in your workflow, leading to more meaningful interactions with your patients.
Imagine the difference it could make in your daily routine. With AI-driven solutions, you can reclaim precious time, allowing you to nurture your relationships with patients and improve overall care outcomes.
Take the first step towards a more efficient and compassionate approach to healthcare. Explore how CosmaNeura can support you in prioritizing quality care over administrative tasks.
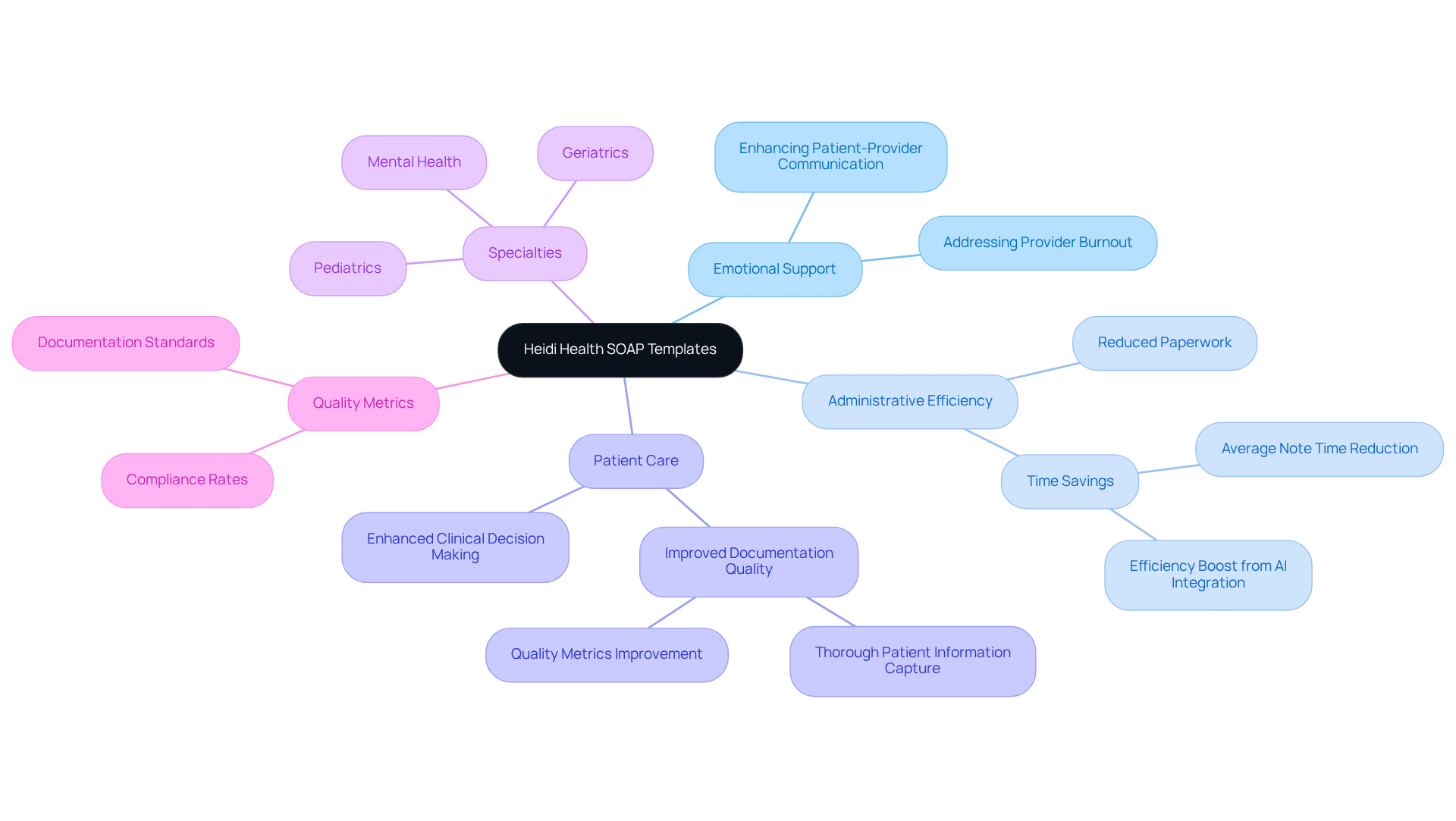
Heidi Health: Access Specialized SOAP Note Templates for Diverse Medical Fields
Heidi Health understands the emotional challenges healthcare providers face daily. The administrative burdens can often feel overwhelming, impacting the quality of patient care. That’s why we offer a range of templates as SOAP method medical examples tailored for various medical specialties, including pediatrics, geriatrics, and mental health.
These templates come equipped with prompts that guide clinicians in capturing essential patient information. This ensures that no critical details are overlooked, allowing you to focus more on what truly matters—your patients. By utilizing these tailored templates, you can improve the standard of your records while saving valuable time.
Imagine enhancing communication and coordination among medical providers, tackling the challenges of fragmented medical systems. By simplifying paperwork procedures, these templates also reduce administrative pressures, enabling you to concentrate more on individual care and enhancing overall service delivery.
Research shows that the SOAP method medical example, which includes structured templates, can significantly enhance adherence to record-keeping standards. Some reports indicate quality metrics rising from 38.2% to 87.2% after template implementation. Furthermore, incorporating generative AI into these processes can boost administrative efficiency by automating routine tasks, allowing you to dedicate more time to direct patient care.
Are you ready to transform your practice? Explore how these solutions can alleviate your administrative burdens and improve patient outcomes. Together, we can create a more compassionate healthcare environment.
MedWriter.ai: Master SOAP Notes with Expert Guides and Best Practices
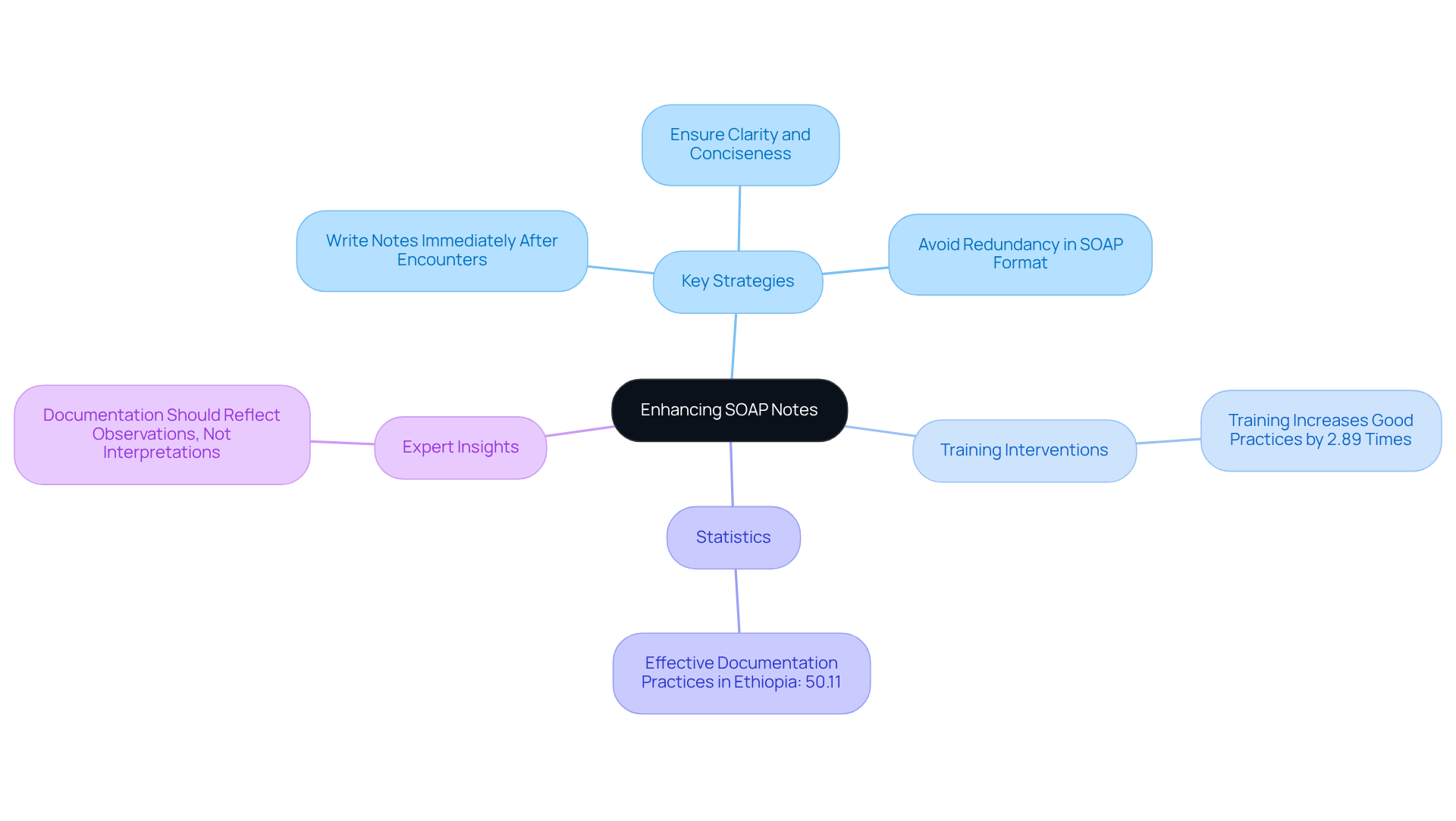
Efficient clinical note recording is crucial for enhancing care and communication among medical teams. Have you ever felt overwhelmed by the administrative tasks that take time away from patient care? By following professional guidelines, medical providers can significantly improve their record-keeping abilities, alleviating some of that burden.
Key strategies include:
- Writing notes immediately after patient encounters to capture fresh information.
- Ensuring clarity and conciseness in each section.
- Avoiding redundancy in the soap method medical example format.
Training interventions have shown to enhance record-keeping practices. In fact, medical professionals who underwent training on clinical records are 2.89 times more likely to exhibit good record-keeping habits. This is a powerful reminder of how support and education can lead to better outcomes.
Furthermore, the aggregated level of effective documentation practices among medical professionals in Ethiopia was reported at 50.11%. This statistic highlights the ongoing need for improvement in this area. An organized method not only aids in better clinical decision-making but also fosters a culture of accountability and precision in health records.
As one medical expert wisely noted, "Your documentation should represent what you see and what the individual reports—not your interpretations or assumptions." By adopting these best practices, you can elevate the standard of care offered to individuals and enhance overall health outcomes. Let's work together to make a difference in our documentation practices and, ultimately, in the lives of our patients.
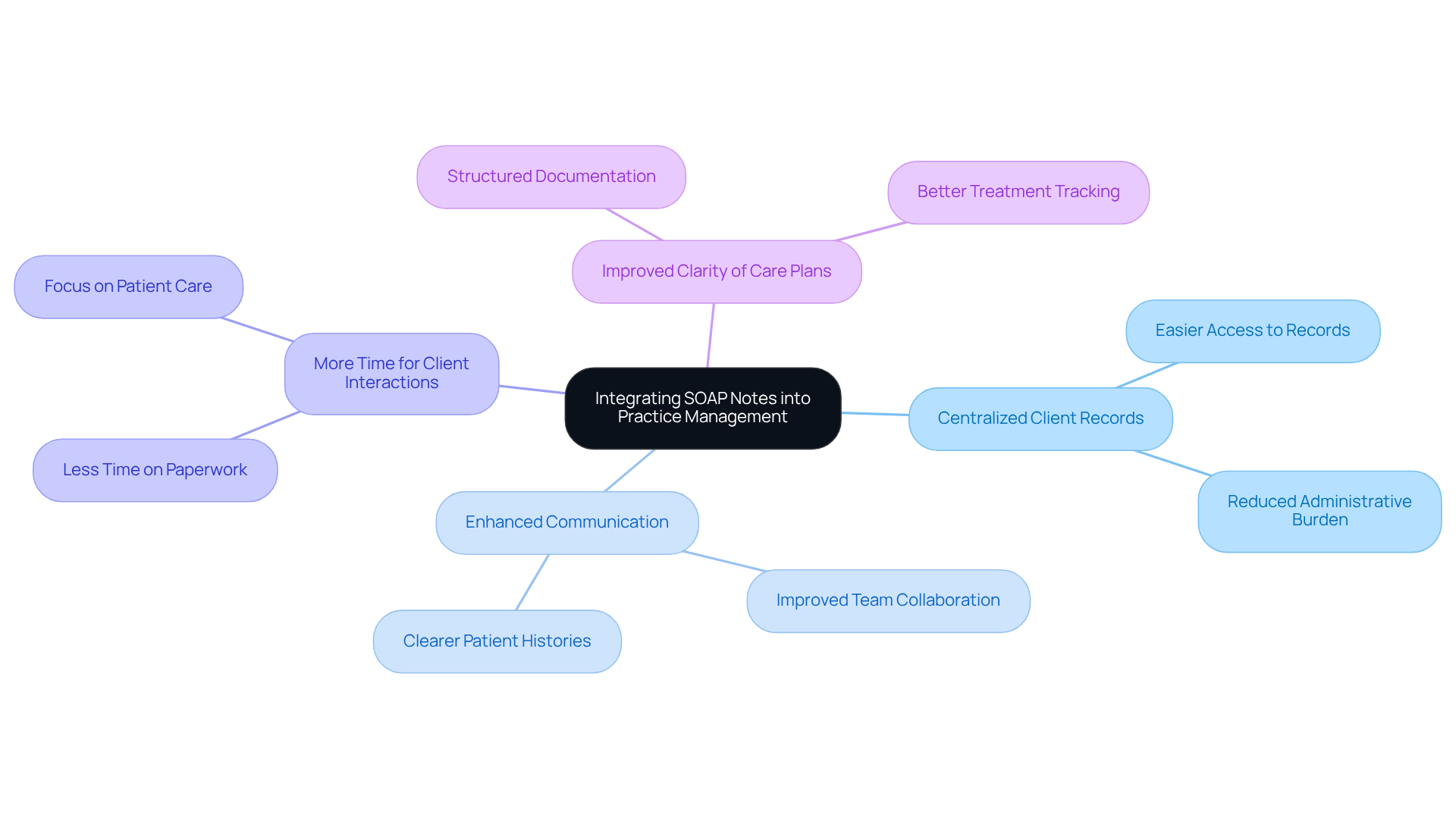
SimplePractice: Integrate SOAP Notes into Your Practice Management System
Healthcare providers often face overwhelming administrative burdens that can detract from their primary focus: patient care. Have you ever felt that your time with clients is cut short by paperwork? It’s a common struggle, and it can lead to frustration and burnout.
SimplePractice offers a solution by seamlessly integrating the soap method medical example into practice management systems. This centralization means that all client records are easily accessible and updatable, allowing you to spend more time interacting with your clients rather than getting lost in administrative tasks. Imagine the relief of having organized clinical notes that enhance communication among your medical team and keep clear records of complaints and treatment strategies.
In high-volume environments, where every moment counts, precise and efficient record-keeping is essential for effective care. By optimizing the record-keeping process, you can focus on what truly matters—your clients. Structured notes not only clarify care plans but also foster collaboration among care teams, ultimately promoting a more individual-focused medical environment.
However, navigating regulatory challenges like HIPAA can complicate the integration of these systems. Dr. Lawrence Weed’s creation of structured notes is a soap method medical example that has paved the way for a uniform recording approach, enhancing communication and improving care for individuals. This innovation addresses the pressing need for change in medical services, despite the resistance that often accompanies it.
Key Benefits of Using SimplePractice:
- Centralized client records for easy access
- Enhanced communication among medical teams
- More time for client interactions
- Improved clarity of care plans
Let’s embrace these solutions together. By prioritizing efficient record-keeping, we can create a nurturing environment that truly supports our clients' needs.
Upheal.io: Explore Practical SOAP Note Examples for Improved Documentation
Efficient documentation techniques utilizing structured notes are essential for enhancing care quality and meeting legal and insurance standards. By organizing clinical notes effectively, healthcare professionals can create clear, actionable records that foster better communication among team members and support improved clinical decision-making.
Have you ever felt overwhelmed by the demands of documentation? It’s a common challenge in healthcare. Practical illustrations of the soap method medical example can demonstrate how to record various client encounters, such as medication management or therapy sessions. For instance, a clinical note for a client dealing with anxiety might include subjective accounts of symptoms, objective observations from the clinician, a thorough evaluation, and a clear follow-up care plan.
To structure SOAP notes effectively, clinicians should follow this established format:
- Subjective: Capture the patient's perspective, including their chief complaint and relevant history. For example, an individual might say, "I feel anxious about work, but my mood has improved since starting medication."
- Objective: Document measurable data, such as vital signs and physical exam findings. This section should include observations that support the assessment.
- Assessment: Synthesize information from the subjective and objective sections to provide a professional evaluation of the individual's condition. This could involve noting any changes in symptoms or responses to treatment.
- Plan: Outline the next steps for patient care, including referrals, additional testing, or modifications to the treatment plan.
Utilizing the soap method medical example can significantly enhance clinicians' record-keeping skills. By examining well-organized SOAP method medical examples, healthcare professionals can focus on relevant details and avoid unnecessary information, ultimately enhancing the quality of their records. Did you know that incomplete records accounted for 32.52% of inadequate routine practice records among health professionals? This statistic underscores the importance of thoroughness in documentation.
Experts stress the value of concise and accurate note-taking. As Tague noted, "Learning how to write concise but accurate notes is such an important skill, just for your own self-care as a provider." This highlights the dual benefit of efficient record-keeping: it not only aids in patient care but also supports clinician well-being.
By incorporating these practices into their routine, healthcare providers can enhance their record-keeping abilities, leading to better outcomes for individuals and more efficient healthcare delivery. Are you ready to take the next step in improving your documentation skills?
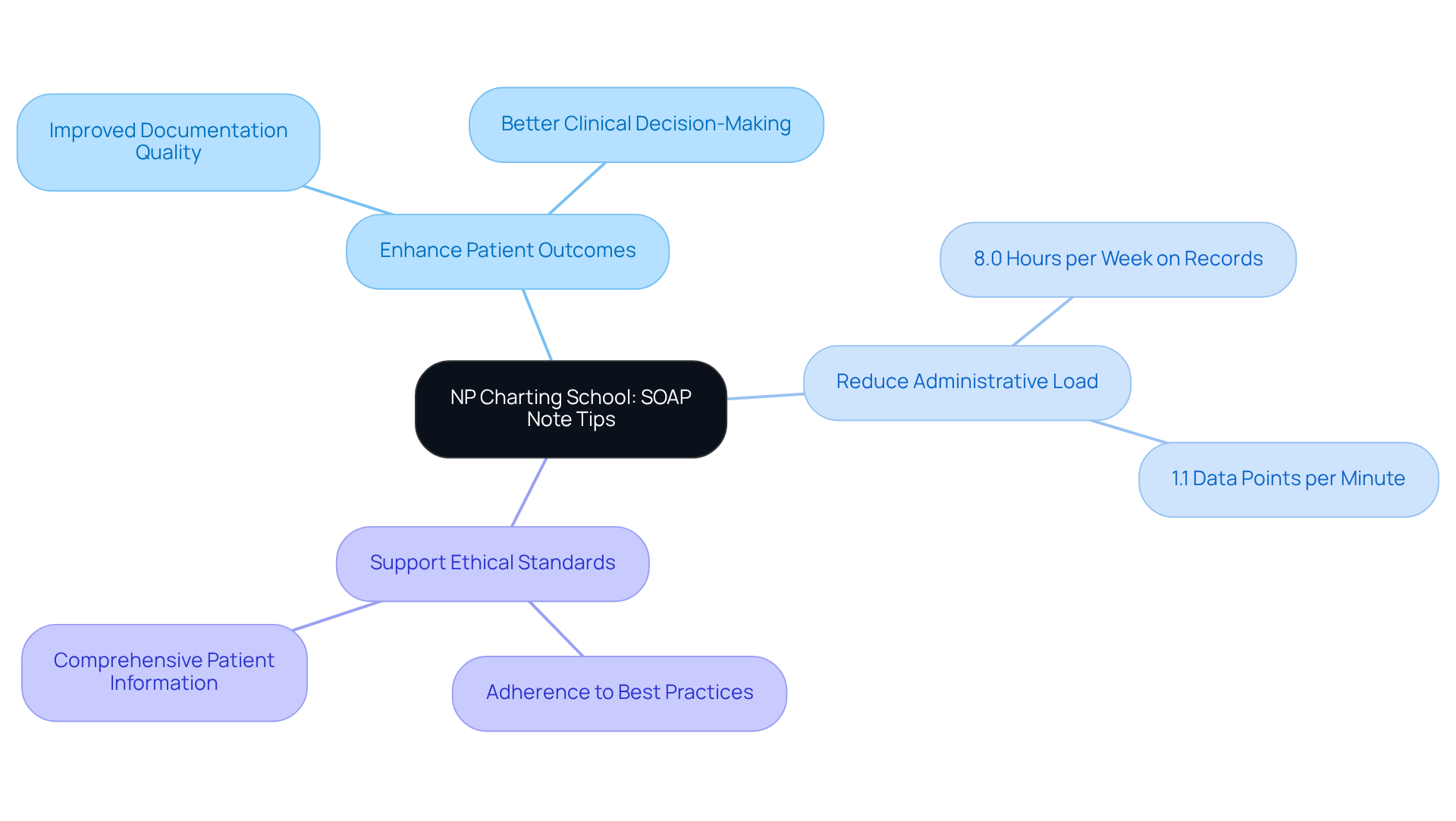
NP Charting School: Tailored SOAP Note Tips and Examples for Nurse Practitioners
At NP Charting School, we understand the unique challenges that nurse practitioners face, especially when it comes to record-keeping. It can often feel overwhelming, can't it? The demands of clinical documentation can weigh heavily on your shoulders, impacting not just your workload but also the quality of care you provide to your patients.
That’s why we offer tailored resources designed specifically to meet your recording needs. Our customized advice and illustrations help you gather comprehensive patient information while adhering to best practices in clinical record-keeping. Imagine being able to streamline your documentation process, allowing you to focus more on what truly matters—your patients.
Consider this: studies show that community nurses spend an average of 8.0 hours each week on clinical records. During a 12-hour shift, they can only record about 1.1 data points per minute. This highlights the pressing need for efficient record-keeping strategies. By implementing our customized note techniques, you can enhance the quality of your records, ultimately improving client outcomes and reducing the administrative burden that often leads to burnout.
This approach not only supports better clinical decision-making but also aligns with the ethical standards of care. It ensures that your documentation practices meet the comprehensive needs of your patients.
Key Benefits of Our Resources:
- Elevate record quality to enhance patient outcomes.
- Reduce administrative load to prevent burnout.
- Support ethical standards in documentation.
We invite you to explore how our resources can make a difference in your practice. Together, we can create a more efficient and compassionate healthcare environment.
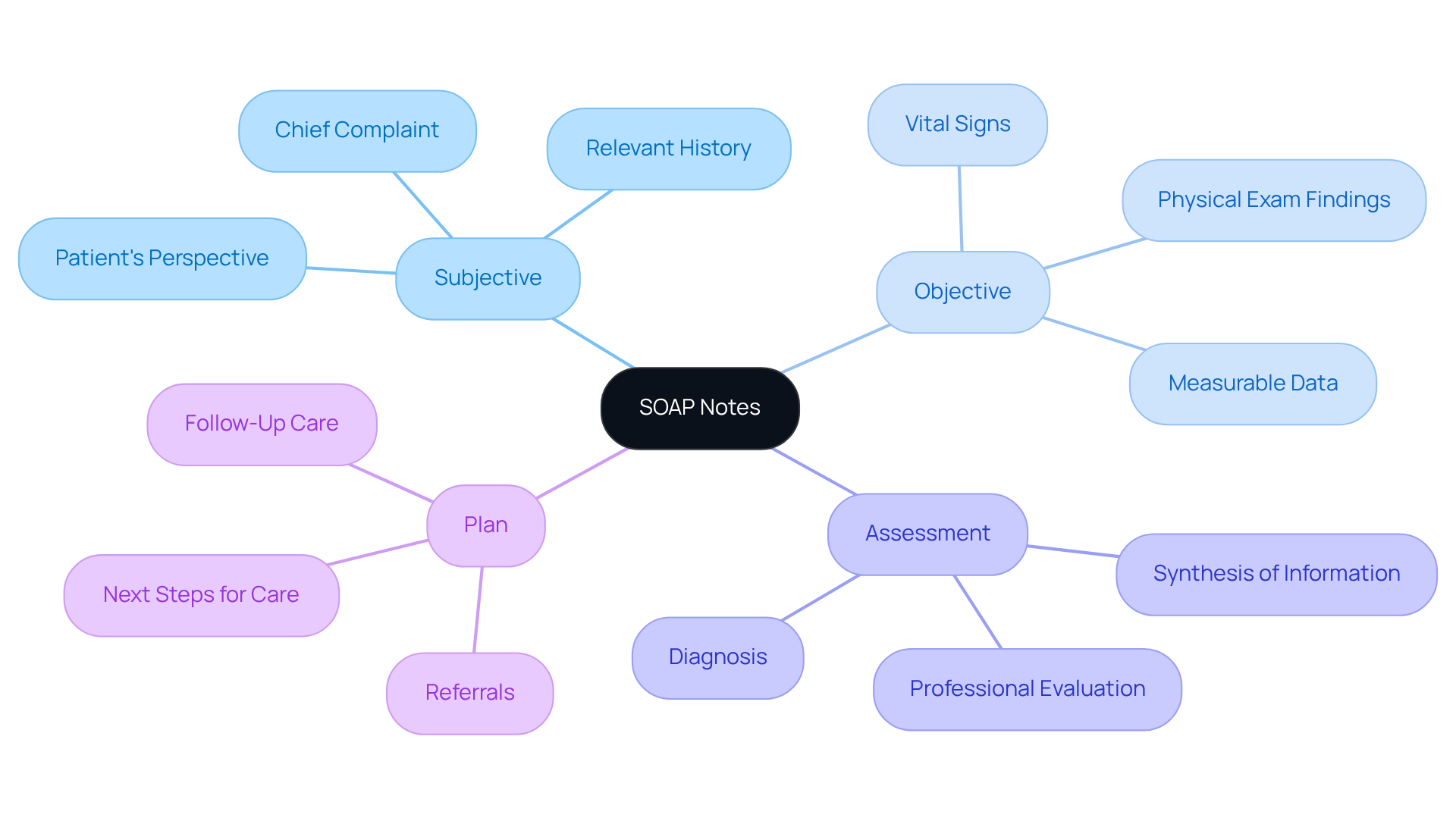
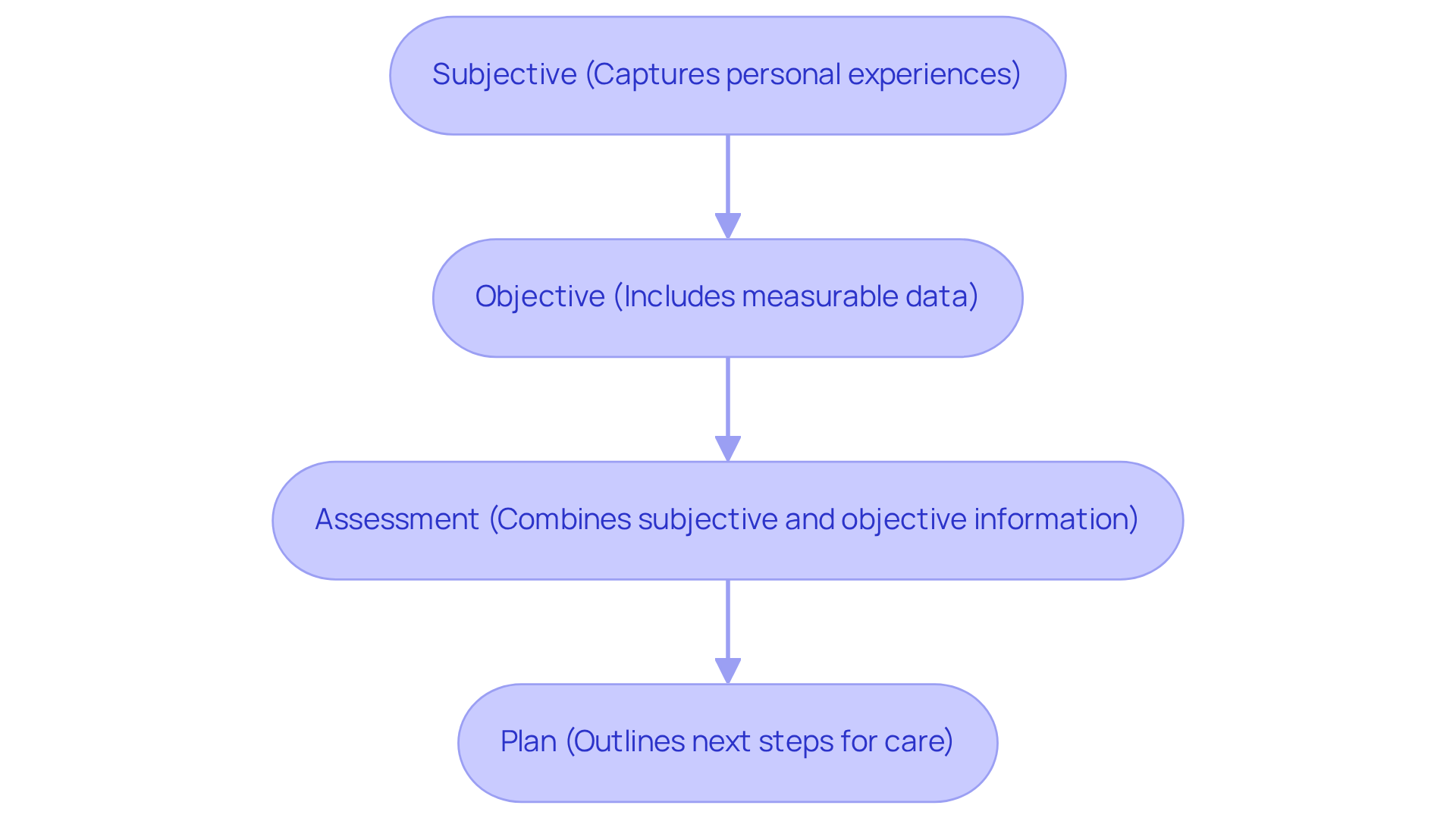
EssayPro: Understand the Structure of SOAP Notes for Effective Documentation
Understanding the framework of the SOAP method medical example—Subjective, Objective, Assessment, and Plan—is crucial for healthcare professionals who want to document client interactions effectively. Each part plays a significant role in making sure that notes are comprehensive and support ongoing care.
Have you ever felt overwhelmed by the sheer volume of documentation? The Subjective section captures personal experiences and chief complaints, giving context for the clinician's evaluation. Meanwhile, the Objective section includes measurable data, like vital signs and physical exam findings, which are essential for supporting clinical assessments.
The Assessment combines both subjective and objective information to reach a diagnosis, while the Plan serves as a soap method medical example by outlining the next steps for care, including further testing and referrals. Research shows that standardized medical notes significantly reduce the risk of miscommunication among specialists, enhancing collaboration and improving client outcomes. In fact, healthcare professionals who adhere to note guidelines often find their record-keeping efficiency improves, alleviating administrative pressures.
Imagine being able to focus more on patient care rather than deciphering unclear notes. By utilizing generative AI tools, such as automated systems for creating clinical notes like those offered by CosmaNeura, healthcare providers can significantly cut down on time spent on record-keeping and reduce the likelihood of errors. This technology not only enhances the accuracy of records but also allows for quicker retrieval than traditional paper notes, ultimately improving the quality of care.
By embracing this approach and integrating AI solutions, clinicians can refine their record-keeping practices and contribute to better outcomes for their patients. Additionally, rearranging the order to APSO (Assessment, Plan, Subjective, Objective) can further streamline access to relevant patient information, prioritizing the most critical components for immediate clinical decision-making.
Key Solutions:
- Implement standardized note-taking practices.
- Utilize AI tools for efficient documentation.
- Rearrange note order to enhance accessibility.
By taking these steps, you can transform your documentation process, allowing you to devote more time to what truly matters—your patients.
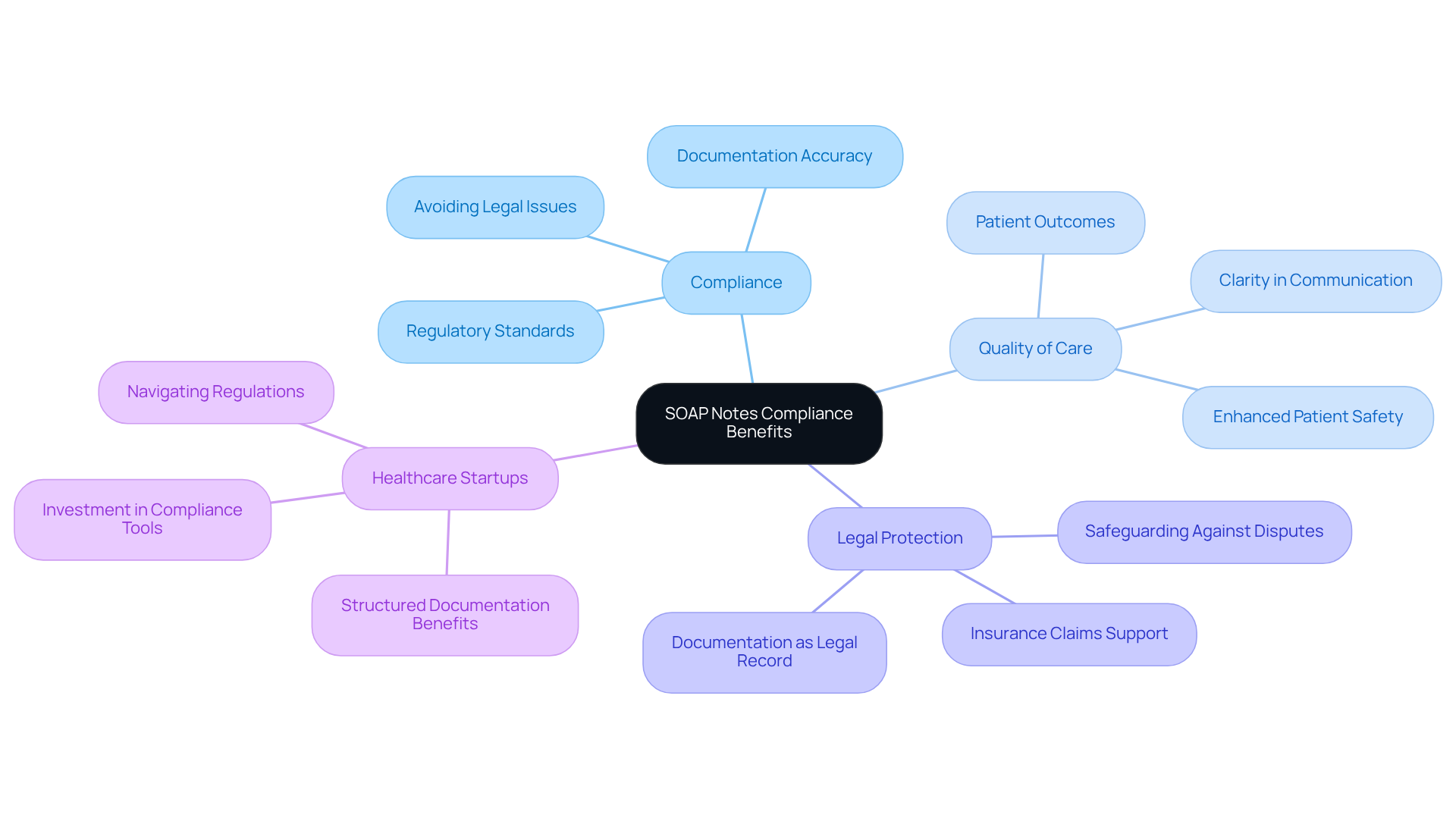
Headway.co: Discover Compliance Benefits of Using SOAP Notes
Navigating the complexities of healthcare can be overwhelming for providers. The administrative burdens often distract from what truly matters—patient care. This is where structured notes in clinical records come into play, offering significant compliance benefits that can ease some of that burden.
By employing the soap method medical example—Subjective, Objective, Assessment, and Plan—clinicians can create records that not only meet legal and regulatory standards but also enhance the quality of care they provide. Imagine the peace of mind that comes from knowing your documentation protects you against potential legal disputes while simultaneously improving patient outcomes.
In a world where healthcare startups face strict regulations, organized records become essential. Research indicates that structured notes lead to clearer and more concise documentation, with record quality scores jumping from 64.35 for unstructured notes to 77.2 for organized notes after implementation. This improvement is not just a statistic; it represents a tangible benefit for both clinicians and patients.
Precise records serve as a legal account of diagnoses and treatments, safeguarding everyone involved in case of disputes or insurance claims. Non-compliance with the soap method medical example notes can lead to serious legal and financial repercussions, highlighting the need for rigorous documentation practices.
To effectively navigate these challenges, medical startups need specialized support that understands the unique regulatory landscape. As Austin Chia wisely points out, 'The soap method medical example illustrates that SOAP notes don’t just assist medical professionals—they benefit individuals, too.' This dual benefit underscores the importance of adopting structured documentation.
So, how can you enhance your utilization of structured notes? By embracing these practices, you not only meet evolving regulatory requirements but also contribute to a more compassionate healthcare environment. Let's work together to ensure that your documentation supports both your practice and your patients.
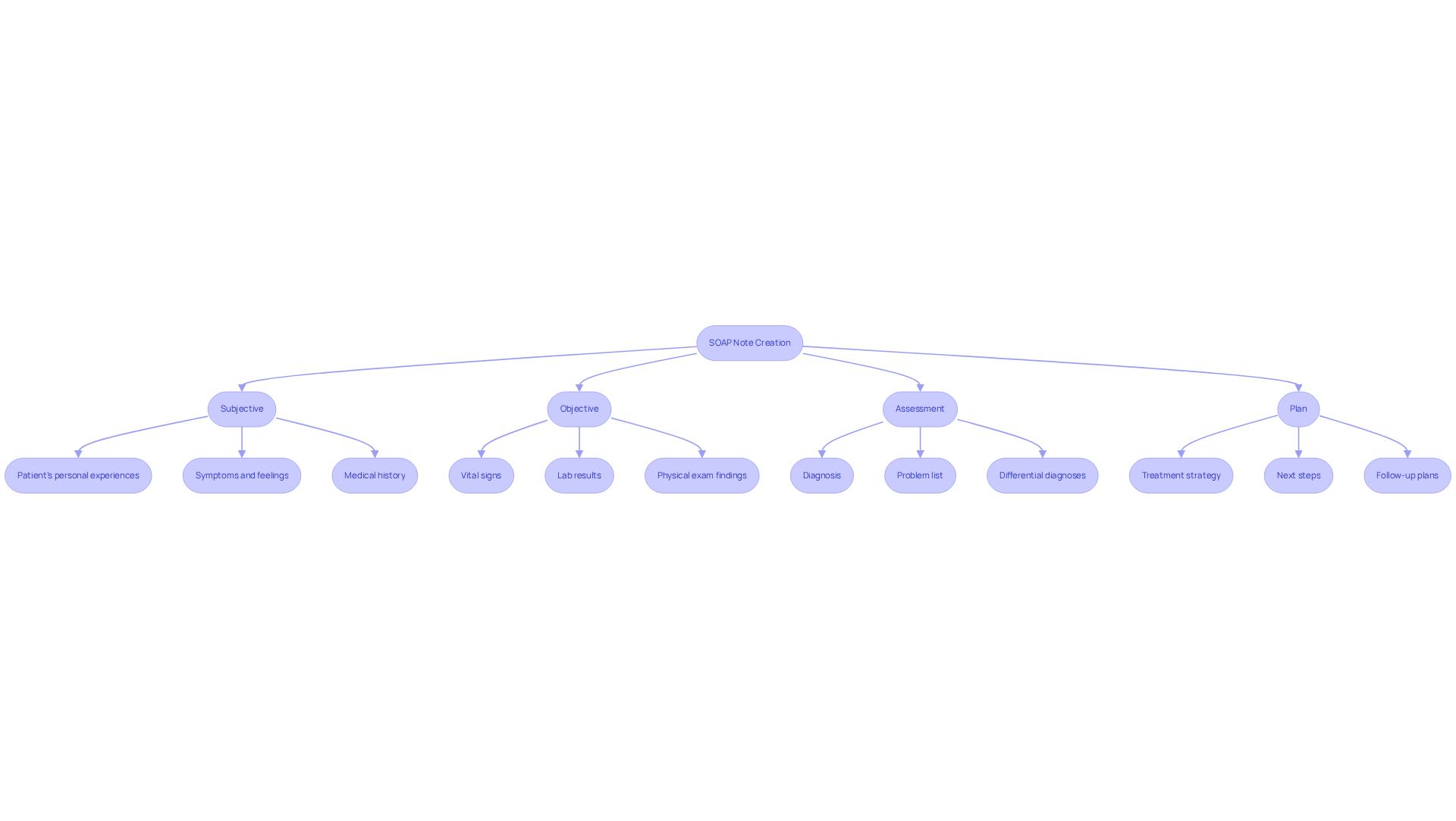
SoapNoteAI: Step-by-Step Guide to Writing Effective SOAP Notes
Creating effective notes is essential for precise client records, and SoapNoteAI provides a comprehensive, sequential guide that serves as a soap method medical example to help healthcare providers navigate this process. Each element of the SOAP method medical example—Subjective, Objective, Assessment, and Plan—is clearly defined, providing practical guidance for documenting encounters. By following the soap method medical example, you can significantly enhance the quality of your records, leading to better care outcomes and addressing the challenges posed by disjointed healthcare systems.
Have you ever felt overwhelmed by the administrative burdens that can impact patient care? Organized record-keeping practices can truly make a difference. They enhance adherence and transparency in medical files, especially in fragmented systems where communication barriers, like those posed by HIPAA, can hinder efficient care. For example, a study at Hasahesa Hospital showed that implementing standardized templates improved documentation compliance from 38.2% to 87.2%. This structured approach not only aids in systematically assessing individual information but also fosters better interaction among healthcare professionals.
By adhering to organized documentation protocols, you can expect to see tangible benefits in your practice. The APSO order (Assessment, Plan, Subjective, Objective) has been found to enhance speed and usability during client visits, allowing you to access critical information more efficiently. Imagine how much smoother your interactions could be with a clear structure in place.
Moreover, precise documentation is vital for ensuring safety and quality of care, as exemplified by the SOAP method medical example. The Subjective section captures your patients' personal experiences and symptoms, while the Objective section includes measurable data, such as vital signs and lab results. This comprehensive approach guarantees that all relevant information is documented, facilitating better clinical decision-making and ultimately leading to improved patient outcomes.
As specialists emphasize, "structured documentation can enhance provider efficiency and reduce documentation time." This highlights the importance of implementing these practices in clinical environments to improve service delivery.
Key Solutions:
- Utilize the SOAP format for comprehensive documentation.
- Implement standardized templates to enhance compliance.
- Adopt the APSO order for improved efficiency during visits.
By embracing these strategies, you can not only alleviate some of the burdens you face but also enhance the care you provide to your patients. Let's work together to create a more efficient and compassionate healthcare environment.
NCBI: Explore the Clinical Significance of SOAP Notes in Healthcare
SOAP notes play a crucial role in the medical field, serving as essential tools that enhance communication among providers and ensure continuity of care. Have you ever felt overwhelmed by the sheer volume of information to convey during patient encounters? By documenting client interactions in a structured format—Subjective, Objective, Assessment, and Plan—clinicians can share vital information clearly and efficiently. This organized approach not only aids in identifying problems but also fosters teamwork among medical groups, ultimately leading to better outcomes for patients.
Consider this: healthcare providers who utilize structured documentation often report improved clarity in care plans. This clarity facilitates better coordination among specialists, ensuring that every aspect of a patient's health is addressed. The use of these documentation notes offers a comprehensive view of an individual's health condition, empowering providers to make informed decisions based on accurate and organized information.
Moreover, structured documentation has been shown to reduce the cognitive load on healthcare providers. This allows them to focus more on delivering care rather than getting bogged down by administrative tasks. Such a shift not only enhances job satisfaction among medical professionals but also elevates the quality of service provided to patients. As experts point out, effective documentation acts as a legal safeguard for both practitioners and clients, ensuring compliance and minimizing liability risks during evaluations and insurance claims.
In summary, the structured format of the SOAP method medical example notes is vital for improving communication, enhancing patient outcomes, and streamlining service delivery. By mastering the SOAP method medical example, clinicians can significantly elevate their practice and contribute to a more efficient healthcare system. So, why not take the next step? Embrace the power of SOAP notes and witness the positive impact on your practice and your patients.
Conclusion
Mastering the SOAP method is crucial for healthcare professionals who want to improve their documentation practices and enhance patient care. This structured approach—Subjective, Objective, Assessment, and Plan—streamlines the recording process and fosters better communication among providers. It ensures that vital patient information is conveyed clearly and effectively.
Have you ever felt overwhelmed by administrative tasks? You're not alone. Many healthcare providers face significant challenges due to these burdens, which can detract from the quality of patient care. Solutions like AI-powered tools such as CosmaNeura automate documentation, easing these pressures. Specialized templates from Heidi Health cater to various medical fields, while best practices from MedWriter.ai and NP Charting School stress the importance of immediate note-taking and tailored resources. By integrating these strategies, you can elevate the standard of care provided to patients while reducing the stress associated with documentation.
Embracing the SOAP method and its associated practices is vital for creating a more efficient and compassionate healthcare environment. By prioritizing effective documentation, you not only safeguard against legal and compliance issues but also enhance the quality of care delivered to patients.
Key Solutions to Consider:
- AI-powered tools like CosmaNeura for automated documentation.
- Specialized templates from Heidi Health for diverse medical fields.
- Best practices from MedWriter.ai and NP Charting School for immediate note-taking.
The call to action is clear: invest in structured documentation practices today. Transform your approach to patient care and ensure a brighter future for both providers and patients alike.




