Overview
The article titled "10 SOAP Examples for Effective Healthcare Documentation" highlights the vital role of SOAP notes in healthcare documentation and their potential to significantly enhance patient care. Have you ever felt overwhelmed by the administrative burdens that can detract from your focus on patient well-being? Mastering the four components of SOAP notes—Subjective, Objective, Assessment, and Plan—can be a game changer. By integrating technology and training resources, you can improve communication and reduce these burdens, ultimately leading to better patient outcomes.
Understanding the emotional challenges you face is essential. The stress of documentation can weigh heavily on healthcare providers, impacting the quality of care delivered to patients. However, by embracing effective SOAP note practices, you can alleviate some of this pressure. Not only does this approach streamline your workflow, but it also fosters a stronger connection with your patients, allowing you to provide the compassionate care they deserve.
Imagine the difference it could make in your daily practice. Enhanced communication can lead to clearer insights into patient needs, while reduced administrative tasks free up precious time for you to engage with those you care for. Let’s take action together—explore these SOAP examples and consider how they might fit into your routine. Your commitment to mastering these techniques can transform the way you document and deliver care, ultimately benefiting both you and your patients.
Introduction
In the intricate landscape of healthcare, where every detail can profoundly impact patient outcomes, the significance of effective documentation is paramount. SOAP notes stand as a cornerstone for clinicians, offering a structured method to convey essential patient information and treatment plans. This article explores the transformative potential of SOAP documentation, highlighting how innovative tools like CosmaNeura's AI solutions can streamline processes, alleviate clinician burnout, and ultimately enhance patient care.
As the healthcare field continues to evolve, we must reflect: how can providers adapt their documentation practices to meet the increasing demands of technology while ensuring the highest standards of patient safety and communication?
CosmaNeura: Streamline SOAP Note Documentation with AI Efficiency
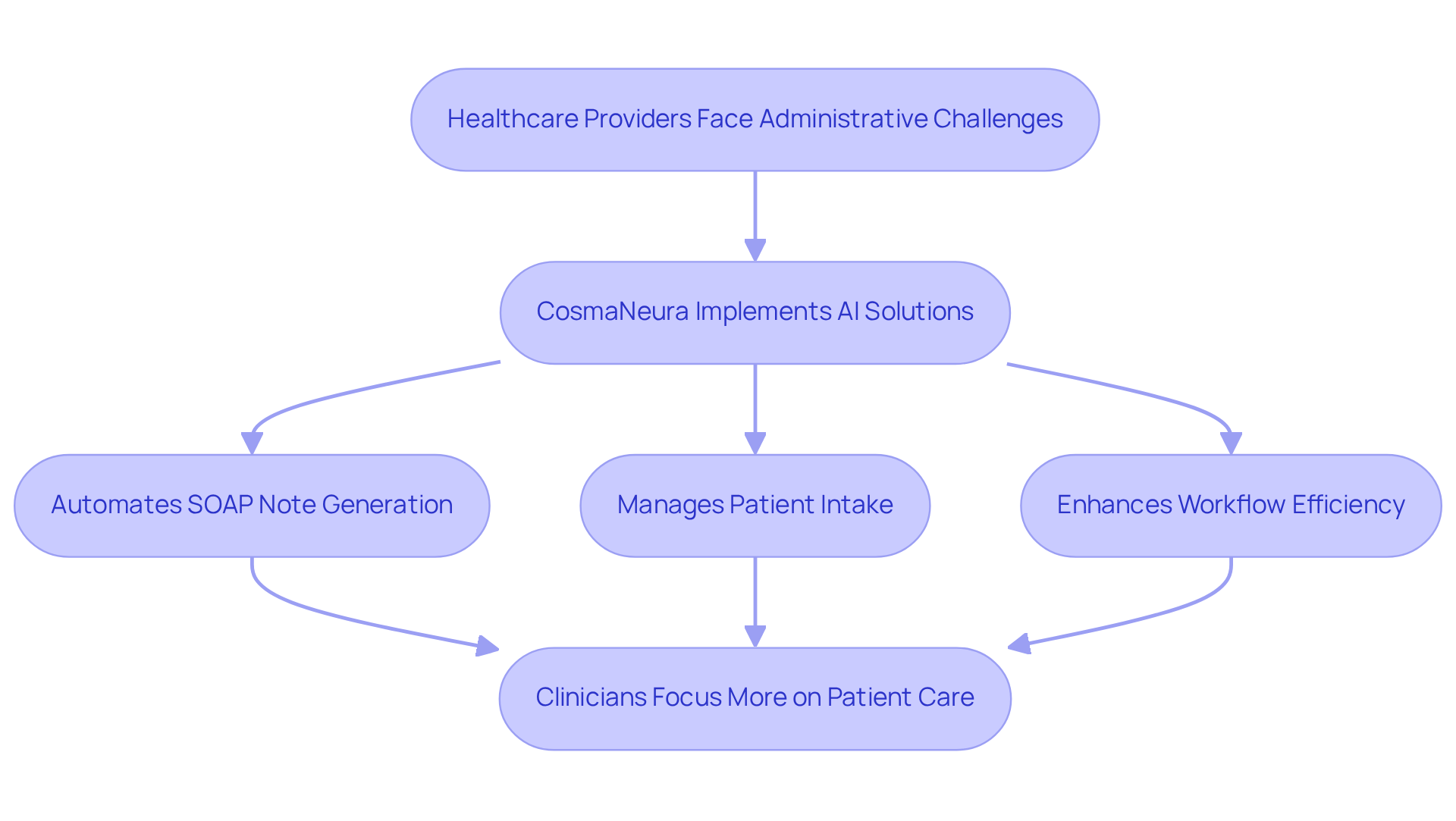
In the demanding world of healthcare, many providers face emotional challenges, often overwhelmed by the administrative tasks that consume their valuable time. CosmaNeura understands this struggle and utilizes advanced AI technology to automate the generation of SOAP examples, significantly reducing the time spent on record-keeping. By autonomously managing patient intake and triage, the platform empowers clinicians to prioritize what truly matters—their interactions with patients.
This streamlined approach not only enhances workflow efficiency but also ensures that records remain consistent and precise, aligning with the ethical standards of Catholic teachings. With studies indicating that 92% of clinicians attribute burnout to excessive administrative tasks, the integration of AI in documentation processes becomes crucial. It can enhance job satisfaction and improve overall care quality, allowing healthcare providers to focus on their patients rather than paperwork.
Imagine the relief of knowing that your note-taking is taken care of. AI-driven solutions have demonstrated the ability to accelerate clinical note-taking, with 78% of doctors reporting considerable time savings. This enables them to concentrate more on direct care, fostering a deeper connection with their patients. By automating SOAP examples, CosmaNeura not only alleviates the administrative burden but also strengthens the commitment to compassionate, ethically aligned medical care.
Moreover, the increasing expenses of medical services create adverse behavior feedback loops, where individuals postpone seeking care due to financial pressures. By enhancing financial efficiency through AI automation, CosmaNeura aids in alleviating these pressures, ultimately improving care in faith-focused healthcare environments.
Isn’t it time to embrace a solution that allows you to focus on what you love—caring for your patients? Let’s explore how CosmaNeura can transform your practice and enhance your ability to provide compassionate care.
Understanding SOAP Notes: Key Components Every Provider Must Know
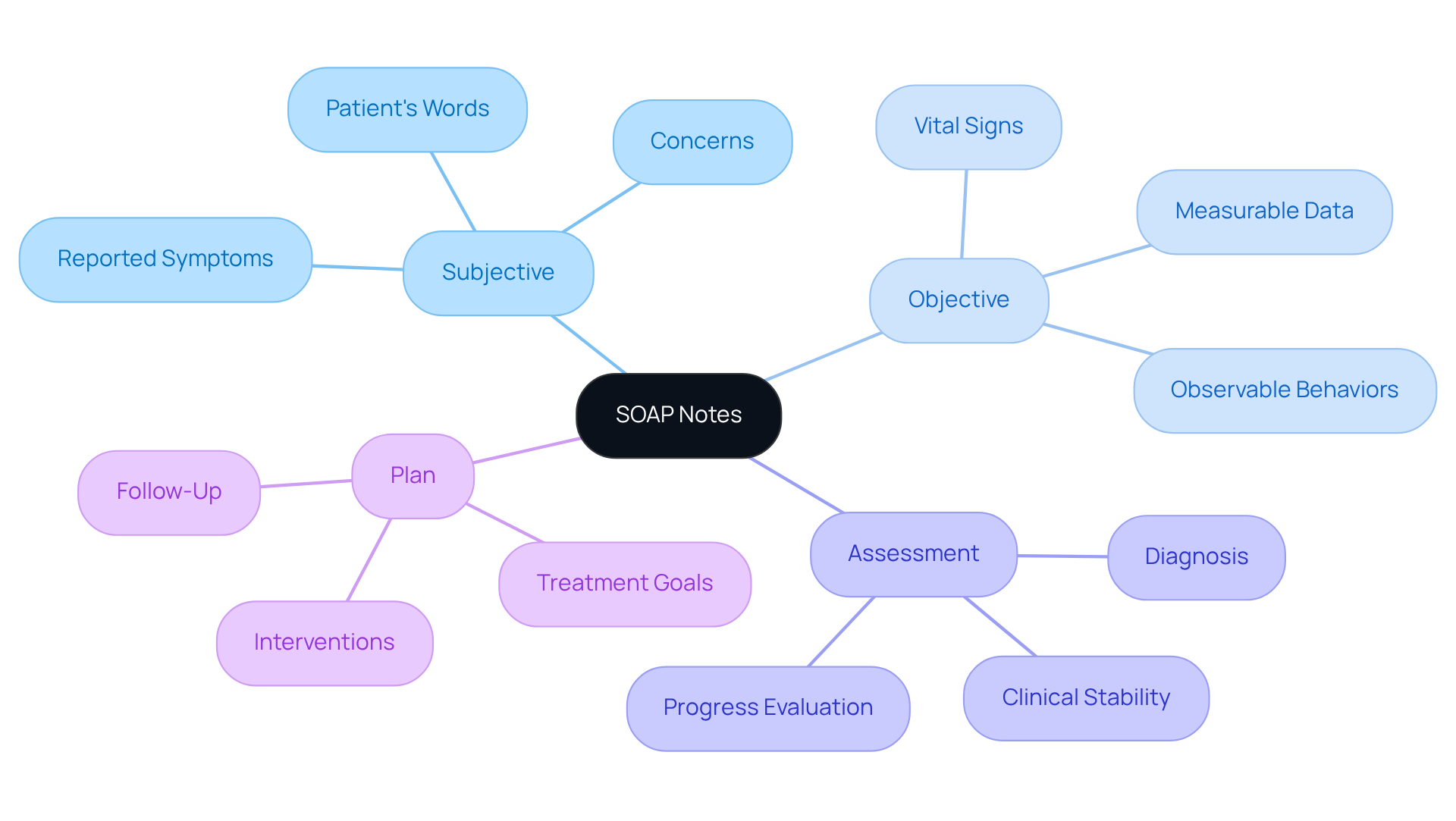
SOAP notes are more than just documentation; they are a vital tool in understanding and addressing the needs of patients. Comprising four key components—Subjective, Objective, Assessment, and Plan—each section plays a crucial role in fostering effective communication. The Subjective section captures the individual's reported symptoms and concerns, while the Objective section provides measurable data, such as vital signs. The Assessment offers the clinician's diagnosis, and the Plan outlines the proposed treatment. Mastery of these components is essential for creating thorough and precise patient records.
Have you ever considered how poor communication can impact patient safety? Statistics reveal that it is one of the most frequent contributing factors to sentinel events. This highlights the importance of clear recording methods like SOAP formats in minimizing risks. Dr. Salwa Zeineddine emphasizes that composing SOAP notes immediately after each session not only fosters consistency but also strengthens communication among medical professionals.
To enhance the clarity of the Subjective section, consider using the OPQRST acronym, which standardizes the reporting of symptoms. By incorporating these organized components, healthcare providers can ensure comprehensive records that ultimately improve treatment outcomes. Remember, clear communication is not just a professional obligation; it is a compassionate response to the challenges faced in healthcare. Let’s embrace these practices to enhance our connections with patients and each other.
Specialty-Specific SOAP Note Examples: Tailoring Documentation to Patient Needs
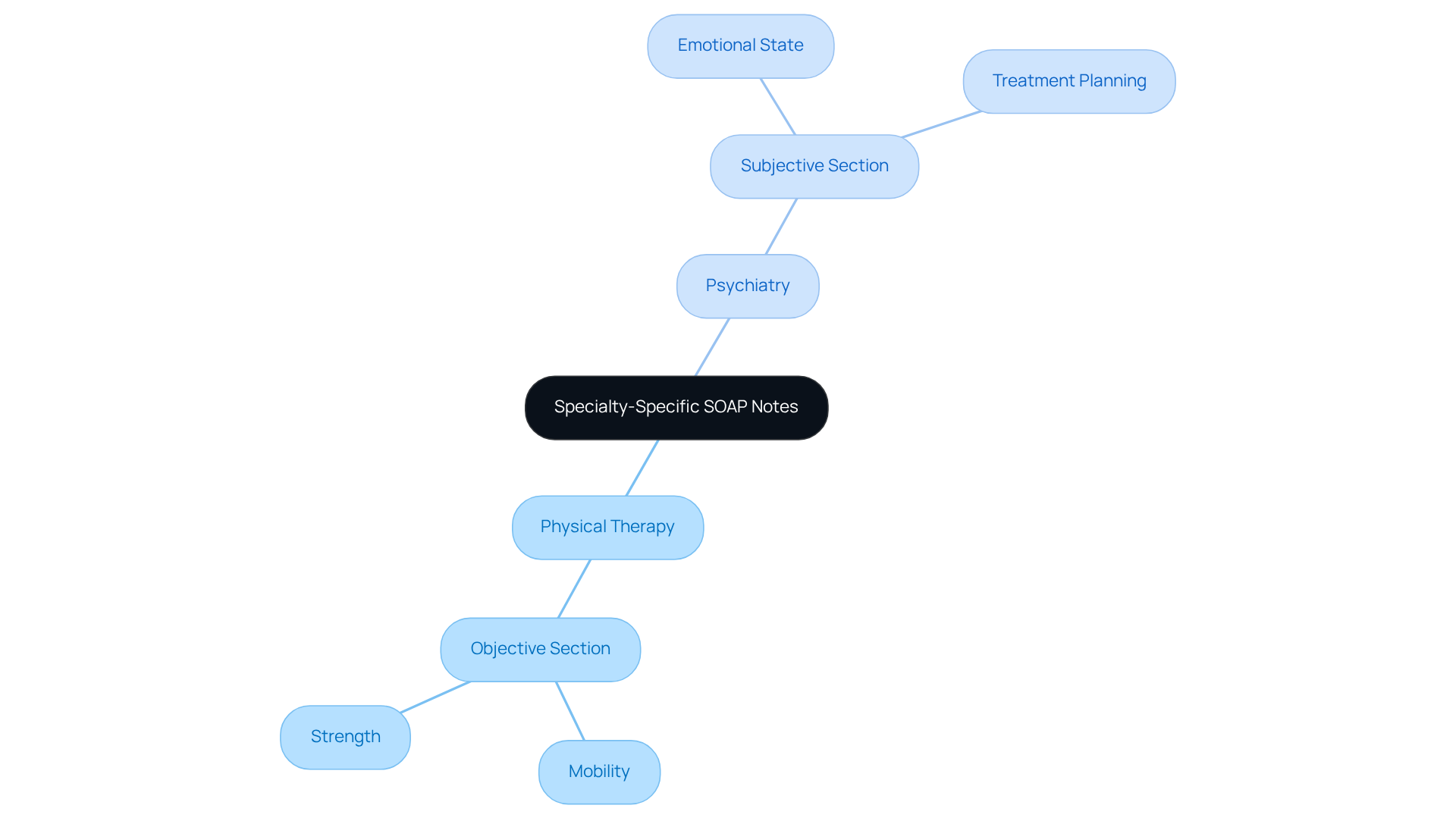
Different medical specialties encounter unique emotional challenges when dealing with SOAP examples in documentation. For instance, in physical therapy, the Objective section often highlights functional evaluations, detailing an individual's mobility and strength. On the other hand, psychiatrists may focus more on the individual's emotional state in the Subjective section, capturing the nuances of mental health that are essential for effective treatment planning. Customizing SOAP notes not only enhances clarity but also improves the quality of care, ensuring that records are relevant and tailored to each specialty's needs.
Have you ever considered how specialty-specific record-keeping practices can profoundly impact patient outcomes? Research indicates that when doctors adapt their record-keeping techniques, they often report increased satisfaction and effectiveness in their workflows. The median dedicated records percentage after implementation was 5.0%, showcasing the efficiency gains linked to customized records. Furthermore, physicians using leading EHR providers experienced higher rates of organized record-keeping compared to those relying on smaller suppliers. By providing SOAP examples tailored to various specialties, clinicians can better understand how to document interactions with individuals effectively, ultimately fostering improved communication and care coordination throughout the healthcare continuum.
Avoiding Common SOAP Note Mistakes: Enhancing Documentation Accuracy
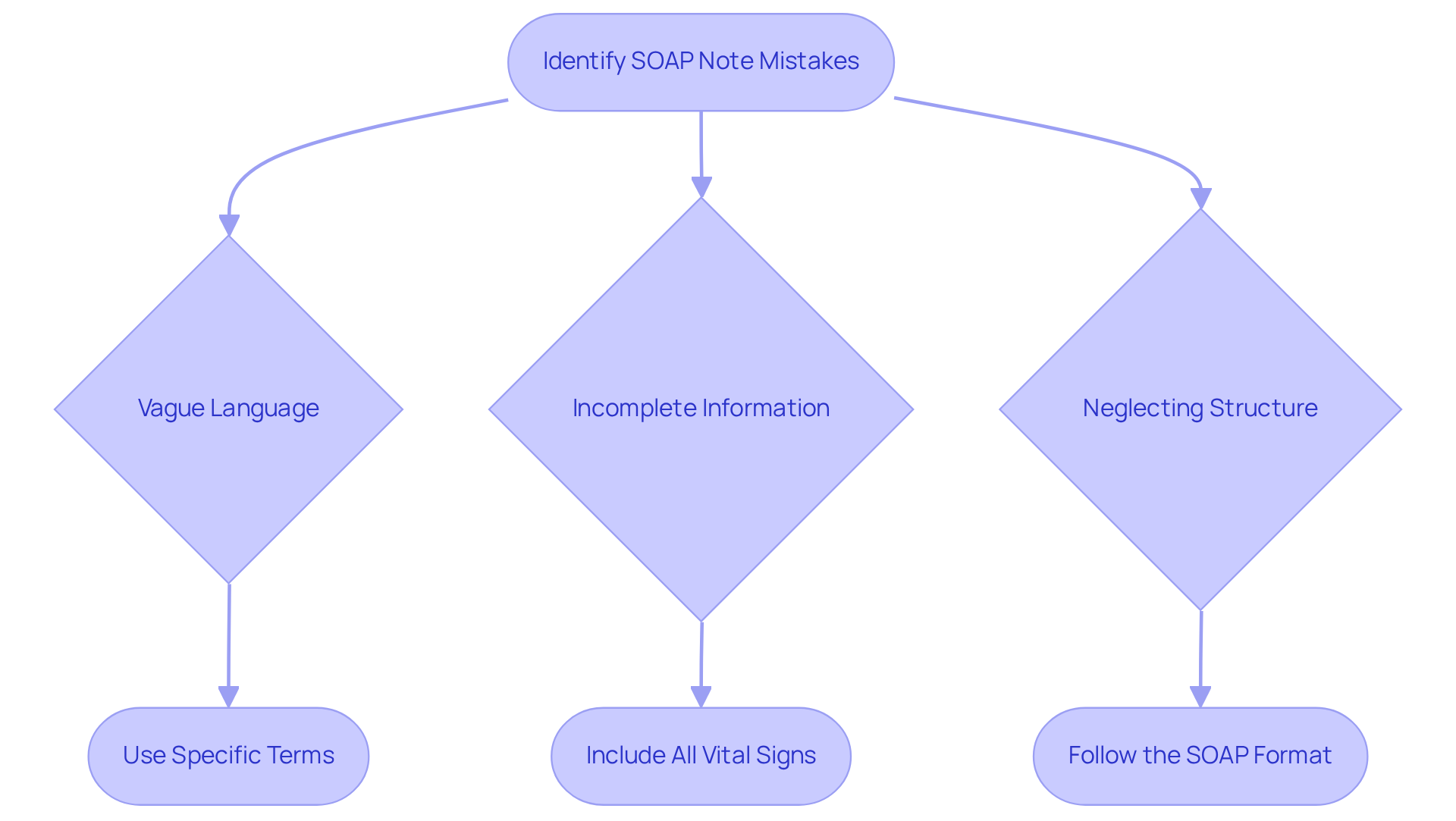
Frequent mistakes in SOAP records can significantly hinder the care provided to individuals. Have you ever considered how vague language, incomplete information, or neglecting the structured format might lead to misunderstandings? For instance, omitting vital signs or providing inadequate detail in the Assessment section can obscure an individual's true condition.
To enhance the precision of your records, it's essential to adopt a proactive approach. Regularly reviewing your writings for clarity and thoroughness not only aligns with documentation standards but also nurtures better communication among medical teams. This practice can ultimately lead to improved outcomes for those you care for.
By taking these steps, you are not just adhering to best practices; you are actively contributing to a supportive environment that prioritizes patient well-being. Together, let's strive for excellence in documentation and patient care.
Collaborative Care and SOAP Notes: Ensuring Comprehensive Patient Management
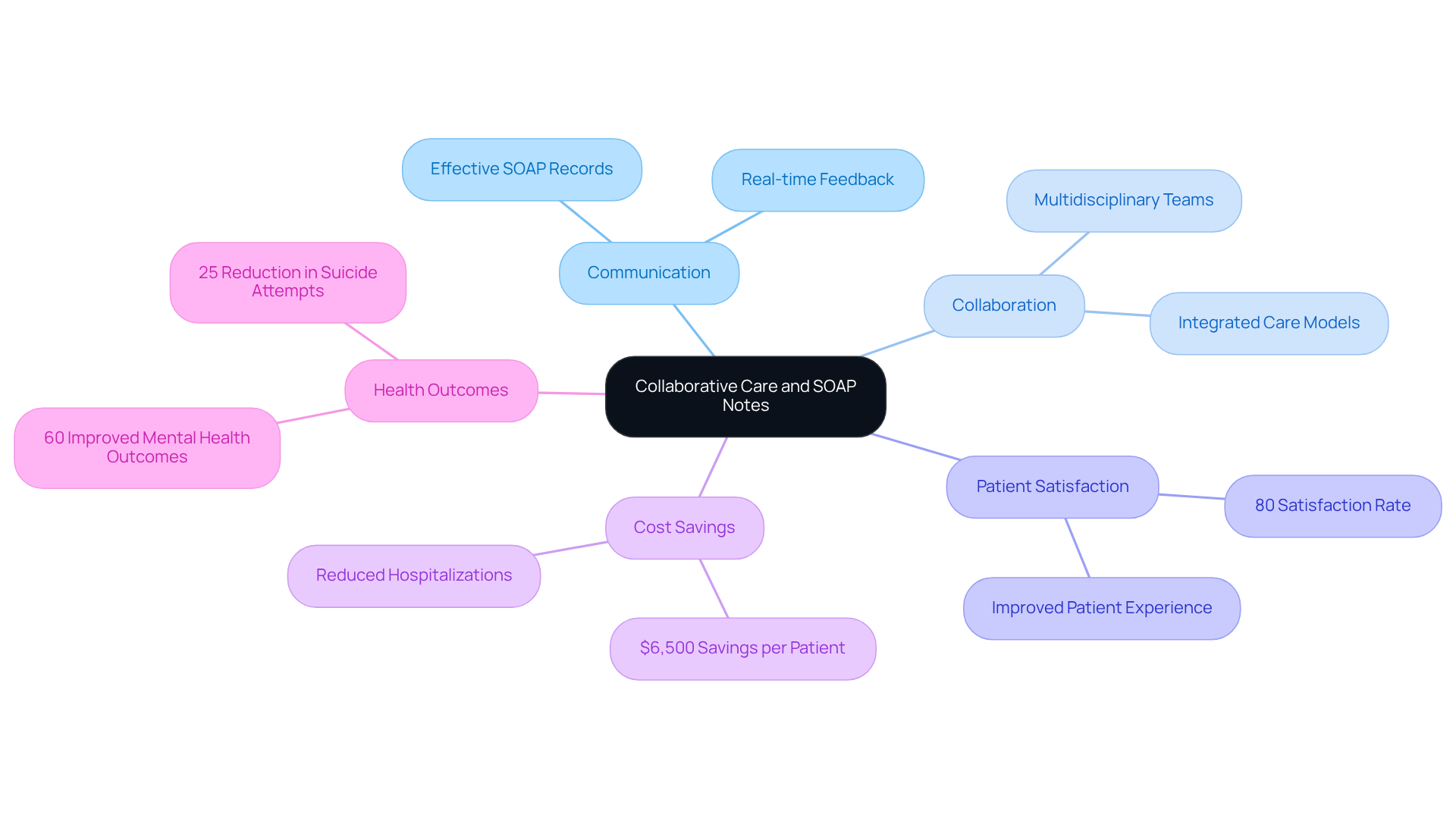
SOAP records serve as a vital communication tool among healthcare professionals, ensuring that every team member is informed about a person's condition and treatment strategy. Have you ever considered how sharing SOAP notes fosters collaboration? This collaboration leads to comprehensive management for individuals receiving care, which is especially important in multidisciplinary teams where various specialists contribute to an individual's well-being.
Research indicates that effective communication in medical settings can significantly enhance outcomes for individuals. For instance, 80% of individuals receiving care through Collaborative Care Models (CoCM) reported greater satisfaction compared to traditional care. Furthermore, incorporating mental wellness services into primary care through models like CoCM can substantially reduce medical expenses, saving an average of $6,500 for each individual over four years. This approach also improves mental health results, with individuals being 60% more likely to see progress.
As healthcare expert Don Berwick emphasizes, "Genuinely hearing from individuals and integrating their feedback is essential to improving the experience for those receiving care." Effective SOAP examples not only facilitate the exchange of information but also enhance the overall quality of care. They provide a structured format for documenting interactions and treatment plans.
Consider how SOAP examples can clarify an individual's progress and inform necessary adjustments to their care plan. This ultimately leads to improved health outcomes. By embracing the power of SOAP records, you can contribute to a more compassionate and effective healthcare experience for everyone involved.
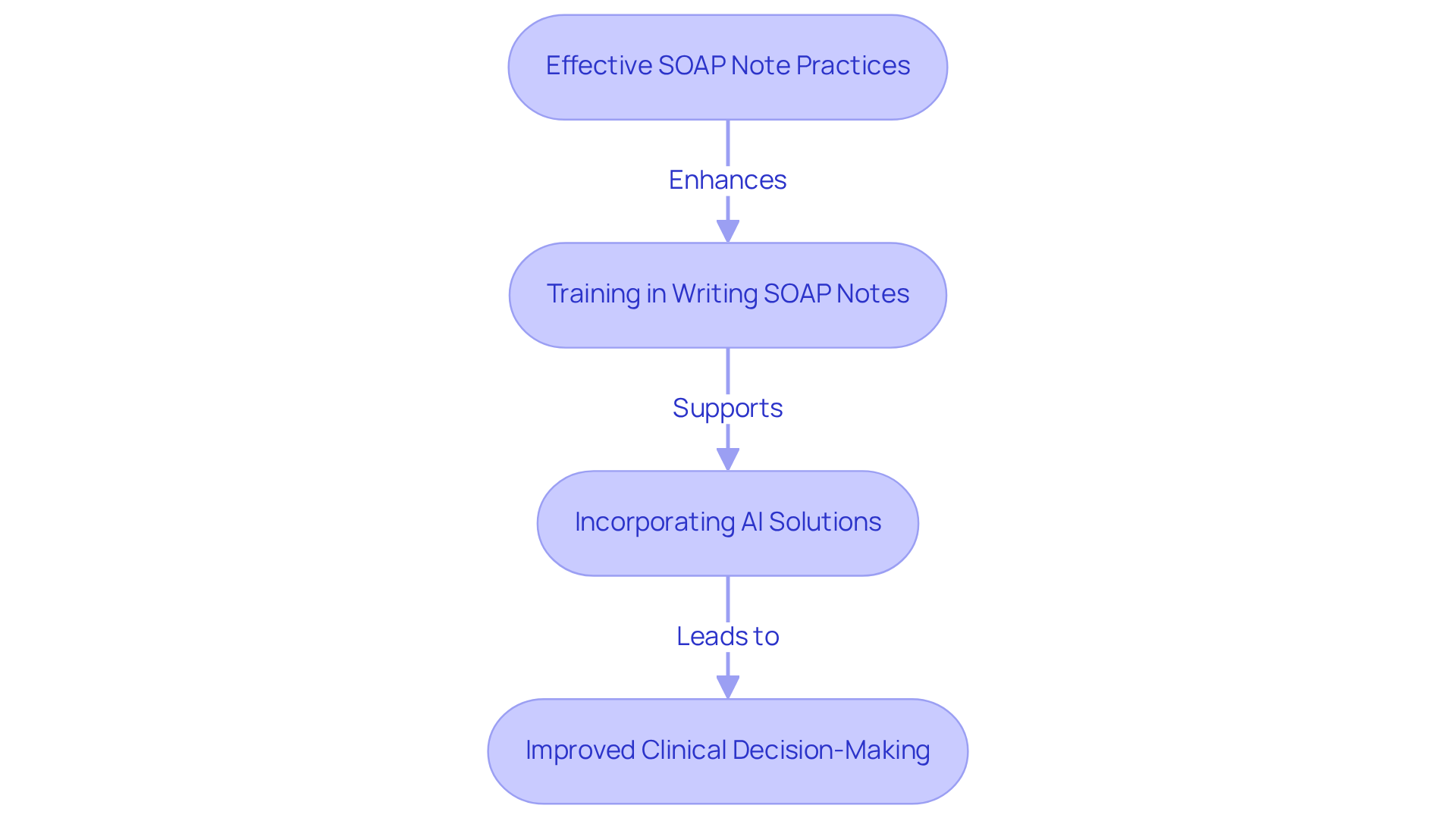
Improving Patient Outcomes Through Effective SOAP Note Practices
Effective practices using SOAP examples are vital in improving outcomes for individuals, especially when supported by innovative AI solutions like CosmaNeura's Agentic Platform. Have you ever considered how precise records can empower healthcare professionals to make informed clinical decisions? By recognizing patterns in an individual's condition, timely interventions can be made. Research shows that clinical decision support systems (CDSS) enhance record quality, leading to improved clinical decision-making and safety for individuals. For example, Mount Sinai’s predictive analytics CDS reduced avoidable adverse drug events (ADEs) by 40% among high-risk individuals, highlighting the significant impact of efficient documentation practices.
Incorporating generative AI can alleviate administrative burdens, allowing healthcare providers to focus more on caring for individuals. Regular training in writing SOAP notes and adherence to best practices are essential for maximizing the benefits of SOAP examples. Detailed records not only support clinical reasoning but also serve as legal protection for providers, ensuring that all interactions with clients are thoroughly documented. As Dr. Lawrence Weed emphasized, the need for uniform records is crucial for enhancing the quality of care for individuals.
By fostering a culture of thorough record-keeping, healthcare organizations can greatly improve the quality of care provided to patients, ultimately enhancing efficiency and accessibility in healthcare delivery. Let’s work together to embrace these practices and create a more compassionate healthcare environment.
Leveraging Technology for Enhanced SOAP Note Documentation
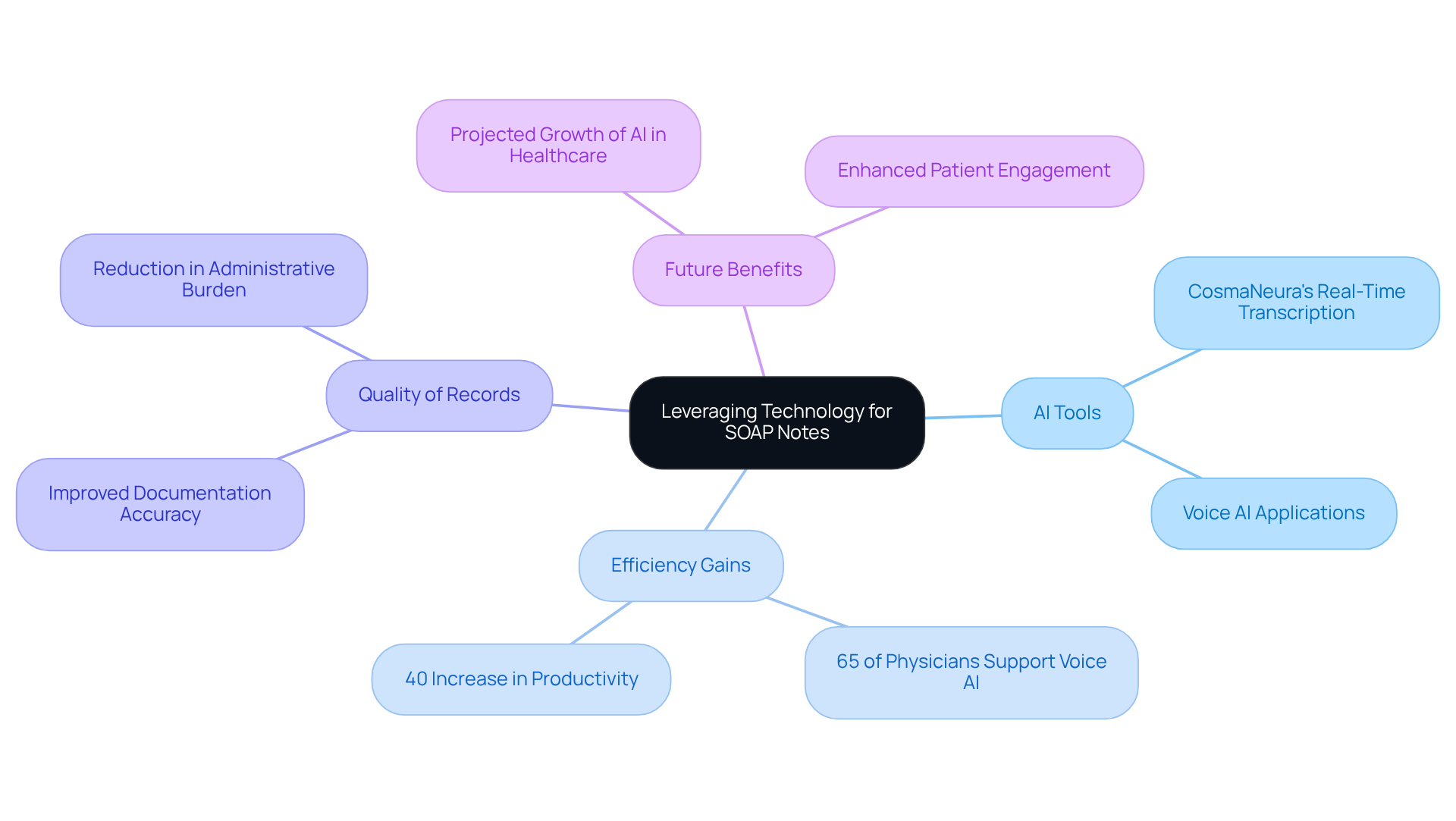
In today's fast-paced healthcare environment, many providers face the emotional challenge of overwhelming administrative tasks that detract from patient care. Technology is stepping in to help, transforming the management of SOAP examples and record keeping through AI-driven tools that automate data entry. These tools ensure that notes are generated quickly and accurately, significantly improving the record-keeping process.
For instance, CosmaNeura's platform offers real-time transcription of interactions, allowing providers to focus more on delivering care rather than getting bogged down by paperwork. This shift not only simplifies workflows but also enhances the quality of records, as shown by various SOAP examples. As a result, medical professionals can maintain high standards of care while alleviating the burden of administrative duties.
As AI continues to evolve, its integration into healthcare record-keeping processes promises even greater efficiency and precision, ultimately benefiting both providers and patients alike. It's encouraging to note that 65% of physicians believe that voice AI can enhance their workflow efficiency. This reinforces the positive impact these technologies can have on the healthcare landscape.
Imagine a future where you can spend more time with your patients and less time managing paperwork. Embracing these innovations can lead to a more fulfilling practice, where the focus remains on care and compassion. Let's explore how we can support each other in navigating these changes together.
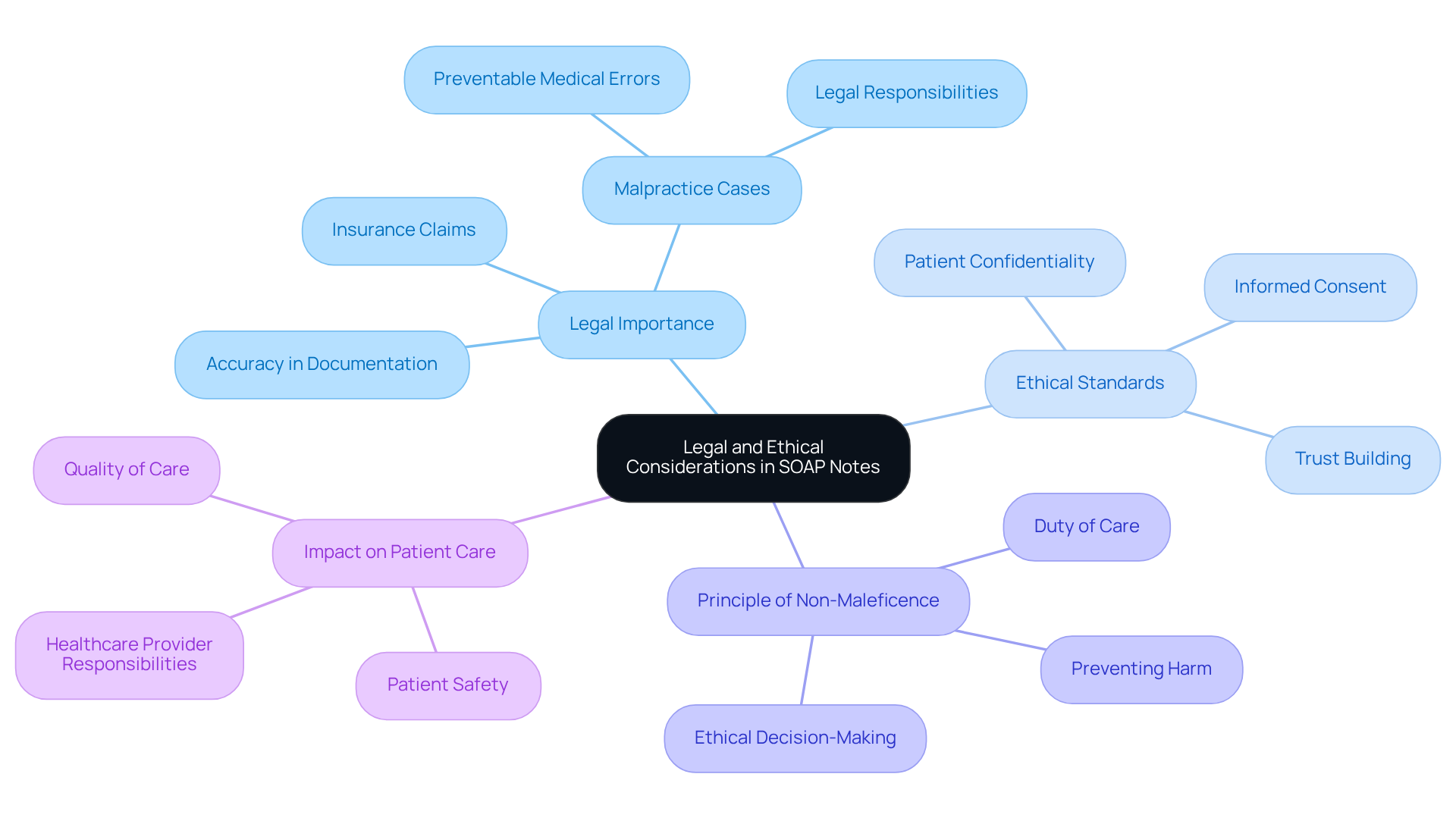
Legal and Ethical Considerations in SOAP Note Documentation
SOAP notes are not just clinical documents; they are legal records that hold immense importance for healthcare providers. The accuracy and completeness of these notes are vital, especially in malpractice cases and insurance claims. Have you ever considered how these records impact your practice? It's crucial to follow ethical standards, ensuring that patient confidentiality is respected and informed consent is secured.
The principle of non-maleficence, which emphasizes preventing harm, plays a significant role in healthcare ethics and directly influences record-keeping practices. Insufficient records can lead to legal responsibilities, as courts often evaluate whether providers have upheld their duty of care based on the files submitted. In fact, approximately 400,000 hospitalized individuals experience preventable harm each year due to medical mistakes, with over 200,000 fatalities attributed to avoidable medical errors. This statistic is alarming and serves as a reminder of our responsibilities.
Moreover, ethical considerations in SOAP note records highlight the necessity of clear, concise, and truthful entries. These not only fulfill legal obligations but also foster trust between providers and patients. By prioritizing these ethical standards, you can mitigate risks and enhance the quality of care you provide. The unique nature of the physician-patient relationship underscores the ethical responsibilities you hold in your record-keeping practices.
By embracing these principles, healthcare providers can ensure that their record-keeping aligns with both legal requirements and ethical standards. Let’s work together to create a healthcare environment that prioritizes safety and trust.
Training Resources for Mastering SOAP Note Writing
Healthcare providers often face emotional challenges as they navigate the complexities of documentation. The administrative burdens can feel overwhelming, impacting not only their workflow but also the quality of patient care they strive to provide. How can we alleviate this stress?
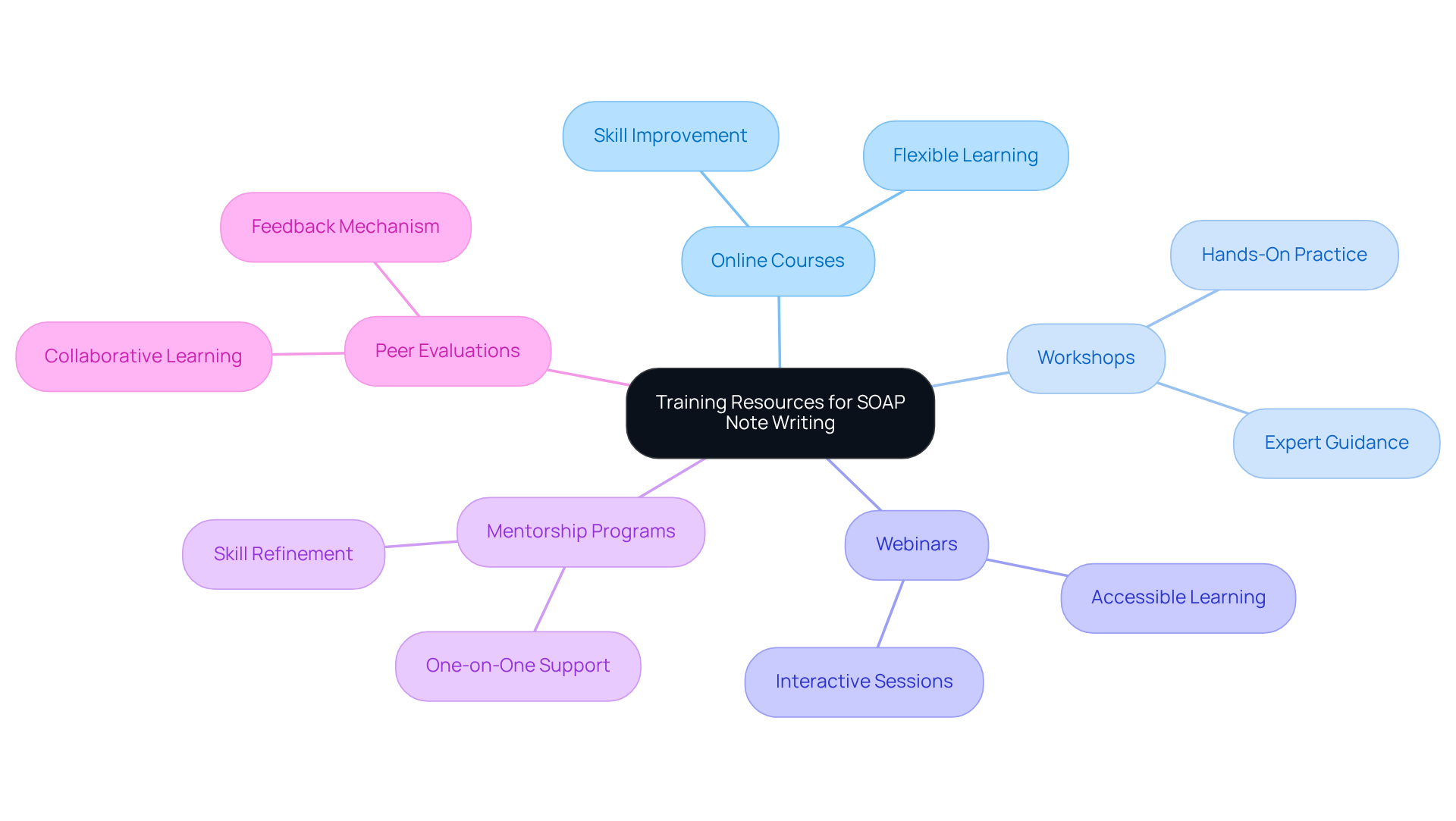
Fortunately, there are various training resources available to help improve skills in creating SOAP examples. Online courses, workshops, and webinars focused on best practices can offer valuable insights that resonate with your experiences. Additionally, mentorship programs and peer evaluations serve as supportive avenues for clinicians to refine their skills, ensuring that their SOAP examples fulfill the necessary criteria for quality and compliance.
By engaging with these resources, you can enhance your documentation practices while reducing the emotional toll of administrative tasks. Imagine the confidence you'll gain in your documentation abilities, leading to a more fulfilling patient care experience. We encourage you to explore these opportunities and take the next step towards improving your skills in a nurturing and supportive environment.
The Future of SOAP Notes: Trends and Innovations in Healthcare Documentation
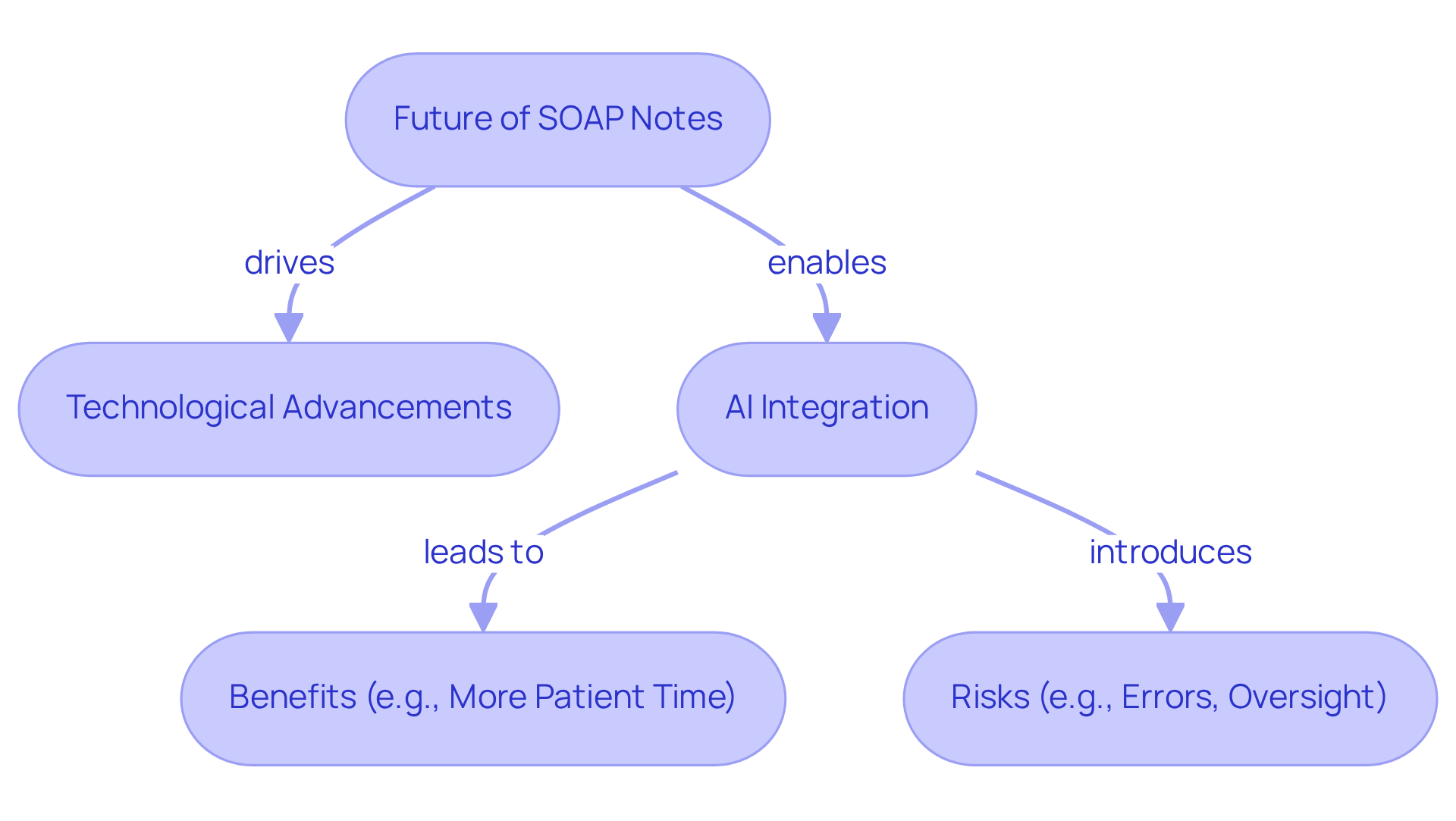
The future of SOAP documentation is on the brink of significant transformation, driven by technological advancements, particularly in AI and machine learning. These innovations, including voice recognition and automated record-keeping tools, are set to alleviate the administrative burdens that often weigh down healthcare providers. Imagine a world where clinicians can focus more on their interactions with patients rather than getting lost in documentation.
For instance, Athelas Scribe achieves an impressive 99.4% transcription precision, allowing healthcare professionals to dedicate their attention to what truly matters—their patients. Furthermore, the integration of electronic health records (EHRs) with AI capabilities will not only simplify record-keeping but also enhance the accuracy and accessibility of SOAP examples. This means less time spent on paperwork and more time for meaningful patient engagement.
However, it’s essential to recognize that ongoing technical improvements are necessary for effective integration, as highlighted in recent studies. This collaboration is expected to lead to better care and outcomes, enabling clinicians to access pertinent information swiftly and ensure comprehensive records. As healthcare professionals gradually embrace these technologies, we can envision a future where clinical workflows are enhanced, and patient engagement is prioritized.
Despite these promising advancements, we must remain vigilant about the potential risks associated with AI-generated materials, such as errors and the need for clinician oversight. Upholding the highest standards of patient care is paramount. As Khaled Diwan wisely noted, establishing clear guidelines regarding AI usage in clinical documentation is crucial for successful implementation. Let us move forward together, ensuring that these tools serve to uplift our healthcare practices and enhance the care we provide.
Conclusion
In the realm of healthcare, effective documentation through SOAP notes transcends mere task completion; it stands as a crucial element of patient care. How often do we find ourselves overwhelmed by administrative duties, diverting our focus from what truly matters—our patients? By leveraging advanced AI tools like CosmaNeura, healthcare providers can streamline their documentation processes, allowing for a renewed focus on patient interactions. The integration of technology in SOAP note practices not only enhances efficiency but also promotes clarity and precision, ensuring that patient records are comprehensive and actionable.
Throughout this article, we have shared key insights regarding the importance of mastering the components of SOAP notes, customizing them for various specialties, and avoiding common pitfalls that can compromise patient care. Have you considered how collaborative care models benefit from well-structured SOAP records? Such records ultimately lead to improved health outcomes. Furthermore, the legal and ethical implications of accurate documentation reinforce the necessity of maintaining high standards in record-keeping.
As the healthcare landscape continues to evolve with technological advancements, embracing these innovations will be vital for enhancing patient care and provider satisfaction. By prioritizing effective SOAP note practices, healthcare professionals can foster a more compassionate and efficient environment. Imagine the positive impact on health outcomes for individuals when we remain proactive in adopting training resources and staying informed about emerging trends. Let’s commit to ensuring that our documentation practices keep pace with the demands of modern healthcare.




