Overview
The article titled "10 Full SOAP Note Examples for Effective Healthcare Documentation" addresses the emotional challenges faced by healthcare providers. It provides practical examples and insights into the structure and importance of SOAP notes in healthcare documentation. Have you ever felt overwhelmed by paperwork? These structured notes not only enhance clarity but also improve patient outcomes and reduce administrative burdens. This allows healthcare providers to focus more on what truly matters—patient care.
By implementing SOAP notes, you can alleviate some of the pressures that come with documentation. Imagine spending less time on paperwork and more time connecting with your patients. This shift not only benefits you but also enriches the care you provide.
In conclusion, consider exploring these examples to help streamline your documentation process. Embrace the opportunity to enhance your practice and improve patient interactions. Together, we can create a more compassionate healthcare environment.
Introduction
In the intricate realm of healthcare, where every moment is precious, the burden of detailed documentation can feel overwhelming for providers. This article explores the transformative potential of SOAP notes, presenting ten insightful examples that not only simplify record-keeping but also elevate patient care.
As the healthcare landscape continues to shift, how can professionals navigate the delicate balance between thorough documentation and meaningful patient interactions? This exploration offers practical strategies and innovative solutions designed to lighten administrative loads while nurturing deeper connections between providers and their patients.
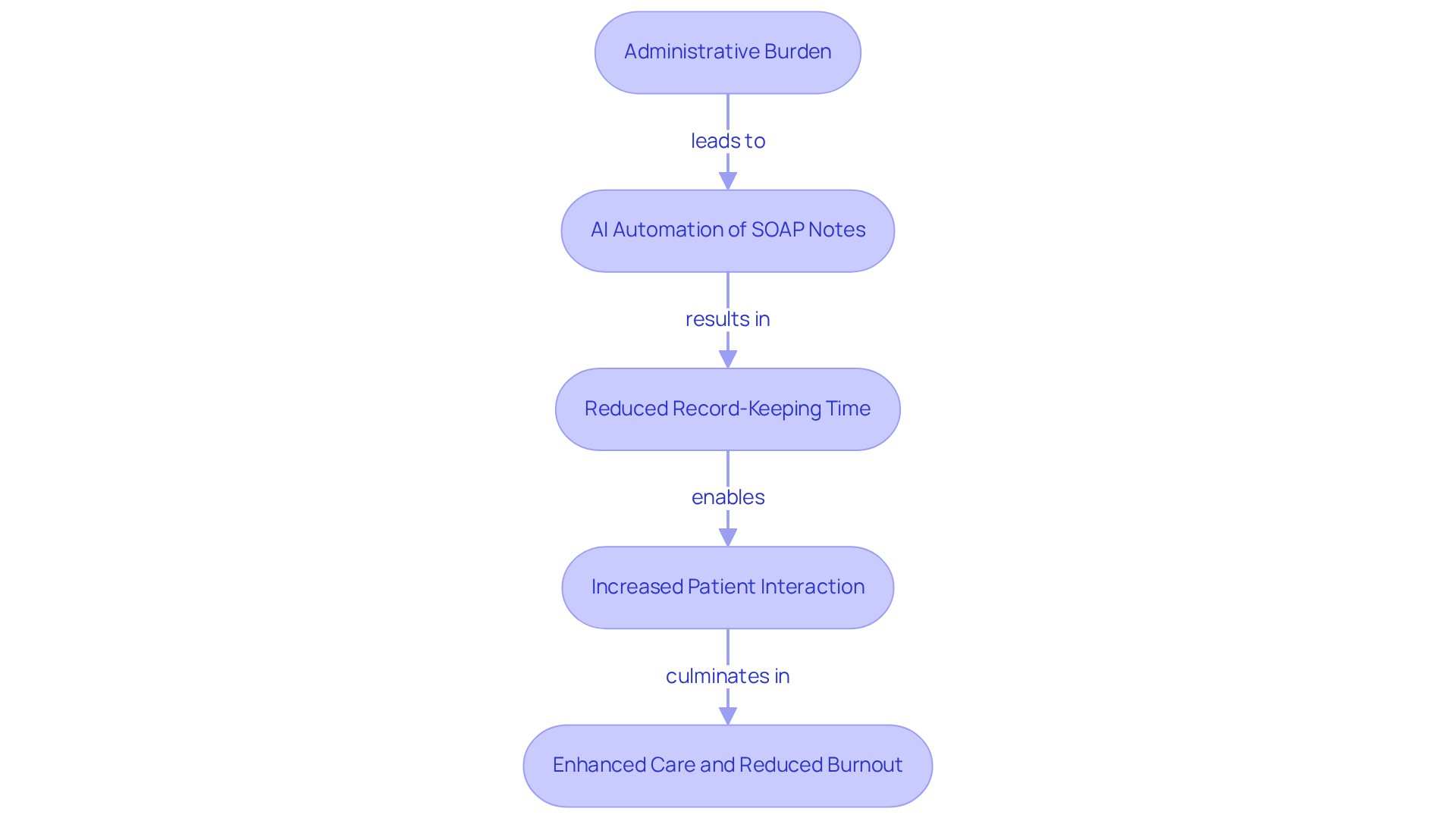
CosmaNeura: AI-Driven Administrative Efficiency for SOAP Notes
Healthcare providers often face overwhelming emotional challenges due to administrative burdens. How much time do you spend on record-keeping rather than connecting with your patients? CosmaNeura understands these struggles and utilizes advanced AI technology to automate the generation of a full soap note example, which significantly decreases record-keeping time.
By independently handling client intake and triage, CosmaNeura enables clinicians to focus on what truly matters: their interactions with individuals. This shift not only enhances productivity but also ensures that documentation is completed accurately and promptly. Imagine the relief of having more time to engage with your patients, fostering deeper connections and providing better care.
Furthermore, by alleviating the administrative load, CosmaNeura's solutions play a vital role in reducing physician burnout. This aligns with the ethical principles of Catholic teachings, promoting quality care while addressing financial pressures on both providers and clients. Together, we can create a healthier work environment that prioritizes compassionate care. If you're ready to explore how CosmaNeura can support you, let's take the next step together.
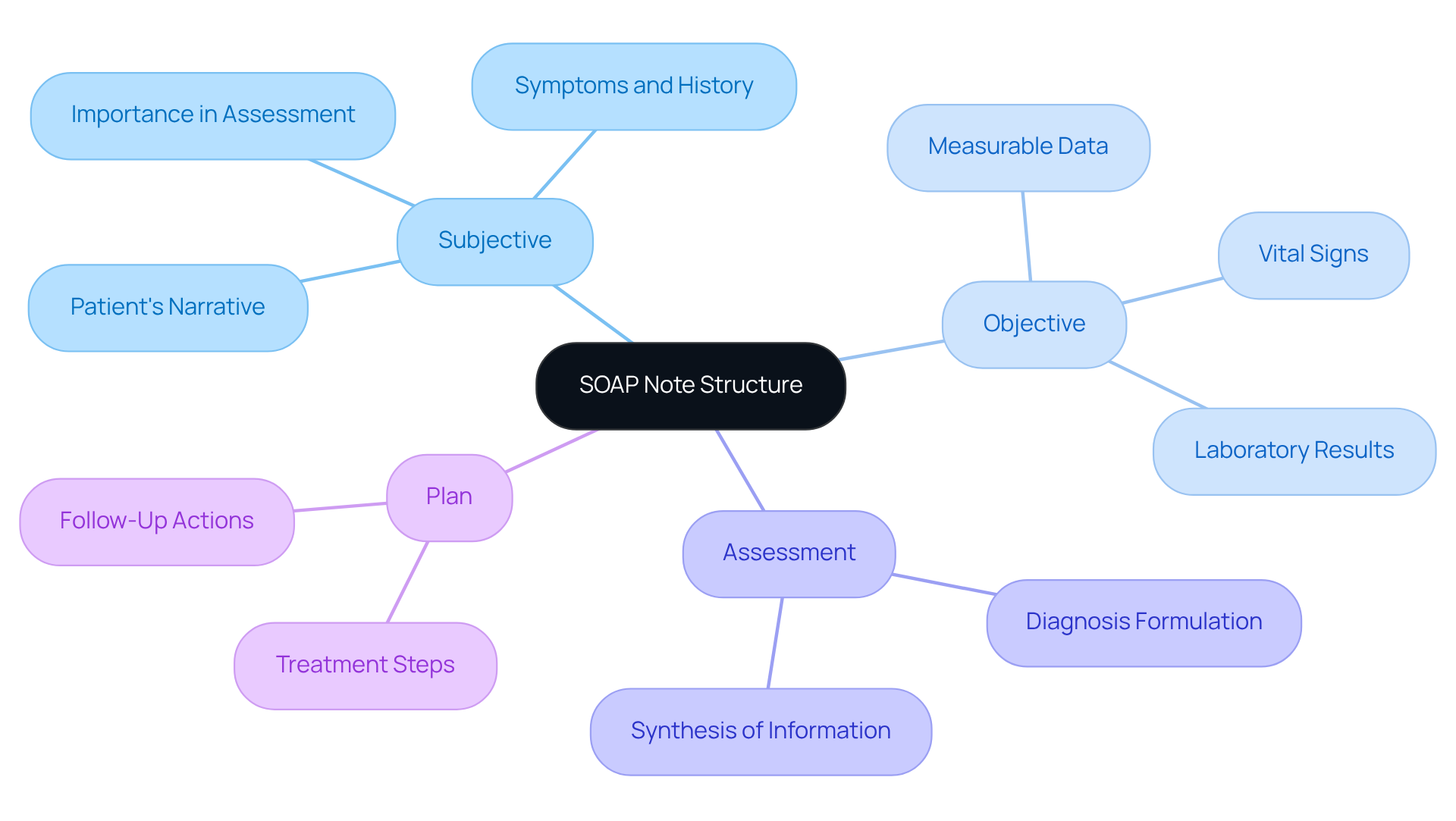
SOAP Note Structure: Understanding Subjective, Objective, Assessment, and Plan
An example of a full soap note is organized into four essential components: Subjective, Objective, Assessment, and Plan. These elements are not just procedural; they are vital tools that can ease the emotional burdens healthcare providers face daily. The Subjective section captures the individual's narrative, including their symptoms and personal history, which is crucial for understanding their condition. In contrast, the Objective section presents measurable data, such as vital signs and laboratory results, providing a factual basis for clinical assessments.
The Assessment synthesizes this information to formulate a diagnosis, while the Plan outlines the subsequent steps in treatment, ensuring a clear path forward for patient care. Mastering this structure is essential for healthcare providers, as it enhances clarity, facilitates effective communication, and supports continuity of care, which can be illustrated by a full soap note example. As Dr. David Schillinger highlights, "Ninety-five percent of guaranteeing suitable reimbursement is simply effective record-keeping practices that most of our clinicians are aware of." This statement underscores the significance of organized records in improving the quality of observations and adherence to healthcare standards.
When these elements are properly employed, they not only enhance patient outcomes but also simplify administrative tasks, ultimately benefiting both healthcare providers and patients. Consider how effective documentation can alleviate some of the stress you may experience in your practice. By embracing these structured practices, you can foster a more supportive environment for your patients and yourself.
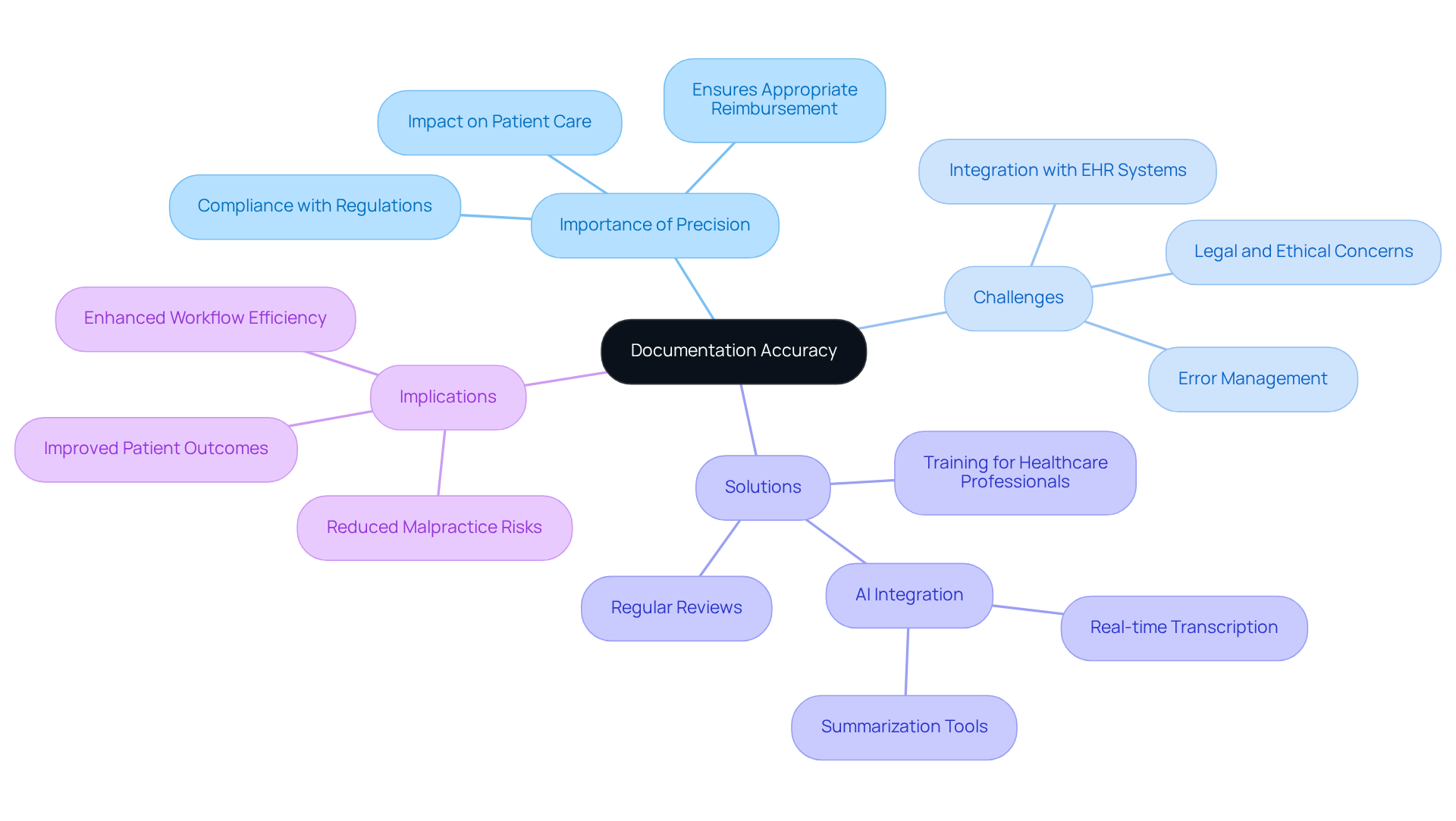
Documentation Accuracy: Ensuring Compliance and Quality in SOAP Notes
Ensuring precision in SOAP documentation is essential for healthcare providers, as it directly impacts their ability to adhere to regulations and standards. Have you ever felt overwhelmed by the administrative burdens that come with documentation? Regular reviews of notes can help confirm completeness and clarity, ensuring that all pertinent information is captured. Integrating AI tools, like CosmaNeura, can significantly ease this process. With real-time transcription and summarization capabilities, these tools not only reduce the risk of mistakes and oversights but also simplify record-keeping. This allows healthcare professionals to focus more on what truly matters—patient care.
Consider this: effective documentation practices can account for up to 95% of ensuring appropriate reimbursement. This statistic underscores the critical nature of maintaining high standards in clinical documentation. By prioritizing accuracy and clarity, we can support one another in overcoming the challenges of documentation. Let’s embrace these innovative solutions together, enhancing our ability to provide compassionate care while ensuring that our administrative tasks are manageable.
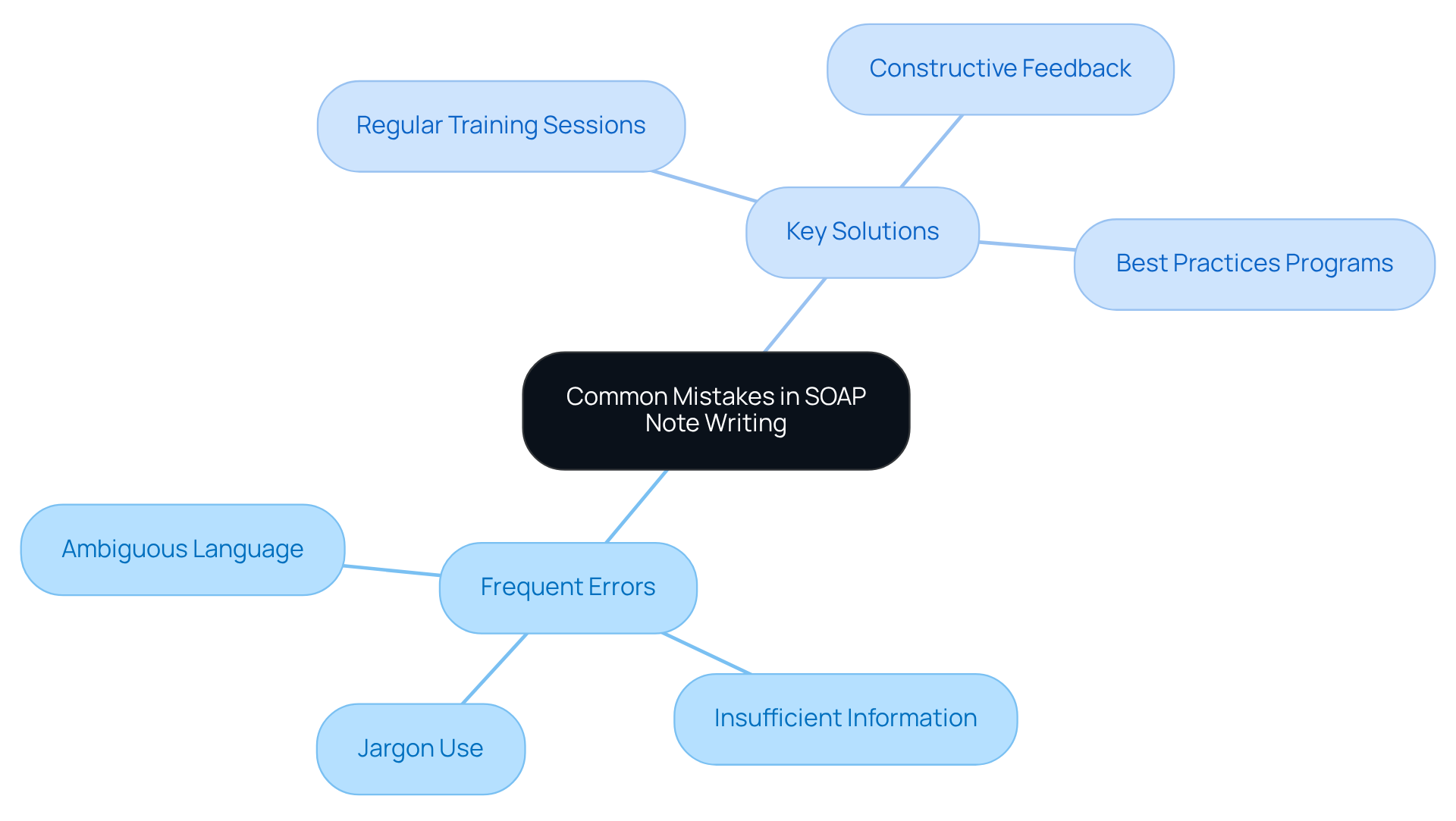
Common Mistakes: Avoiding Pitfalls in SOAP Note Writing
Frequent errors in documentation writing can be frustrating for healthcare providers, often stemming from ambiguous language and insufficient information. It's important to recognize how these challenges can impact patient care. Providers should avoid jargon that may confuse other professionals, ensuring that each section of the full soap note example is well-developed. For instance, unclear terms in the Subjective section can hinder effective communication about a patient's condition.
What if there were ways to improve this situation? Consistent training sessions and constructive critiques are essential in addressing these issues. They can significantly enhance the quality of records, leading to better patient outcomes. Programs that incorporate a full soap note example in their focus on best practices in documentation writing have shown that clarity and adherence can improve dramatically.
By fostering a culture of ongoing improvement in record-keeping methods, healthcare providers can prevent common mistakes. This not only ensures that documentation serves as a reliable resource for patient care but also supports the emotional well-being of both providers and patients. Let's embrace these strategies together for a more effective and compassionate healthcare environment.
Key Solutions:
- Regular training sessions
- Constructive feedback mechanisms
- Programs on best documentation practices
By implementing these practices, we can create a supportive atmosphere that enhances the quality of care we provide.
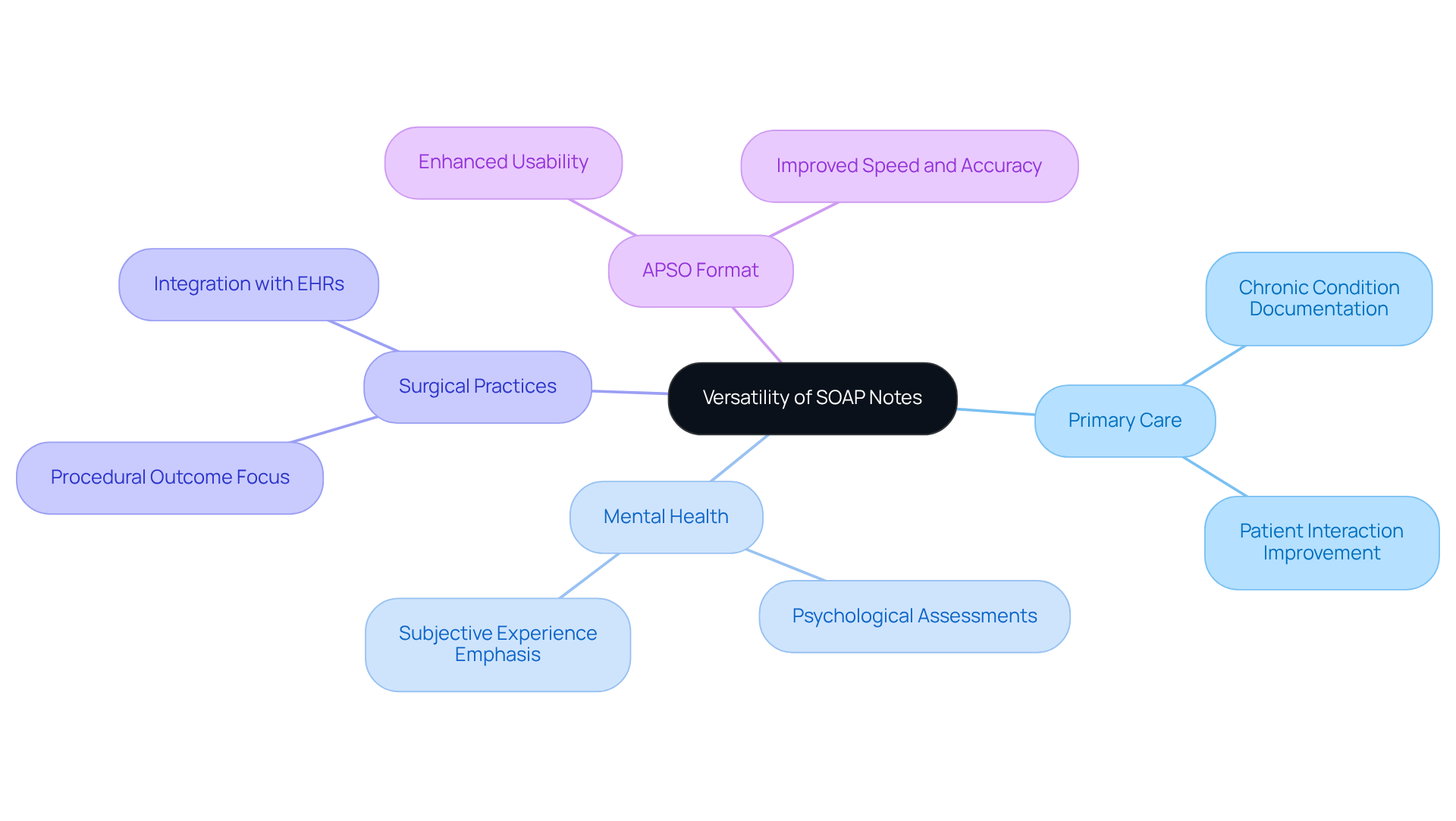
Versatility of SOAP Notes: Applications Across Healthcare Disciplines
In the ever-evolving landscape of healthcare, adaptability is crucial. Healthcare providers, whether in primary care, mental health, or specialized practices, often face emotional challenges that can impact patient care. These observations serve as a full soap note example of the structured documentation format introduced by Dr. Larry Weed in the 1960s, which has evolved to meet the unique needs of each discipline. For example, mental health practitioners might integrate psychological assessments, while surgical teams concentrate on procedural outcomes.
This adaptability not only enhances the documentation process but also nurtures a patient-centric approach, ultimately leading to improved healthcare outcomes. Have you ever felt overwhelmed by the cognitive demands of documentation? Data suggests that structured documentation can alleviate this burden, fostering better communication among healthcare providers. In multidisciplinary teams, a well-organized format ensures that everyone is aligned in their understanding of a patient's condition and treatment strategy.
Consider how a primary care physician records a chronic condition using a full soap note example, while a mental health expert emphasizes the individual’s subjective experiences. This collaborative approach ensures that all aspects of care are acknowledged and addressed. Additionally, the APSO format, which modifies the traditional order of documentation, has been shown to enhance the speed and accuracy of gathering relevant information during client visits.
This thorough method underscores the significance of documentation in delivering cohesive and efficient care. Let's embrace these structured approaches to not only ease our administrative burdens but also enhance the quality of care we provide to our patients. Together, we can foster a more supportive and effective healthcare environment.
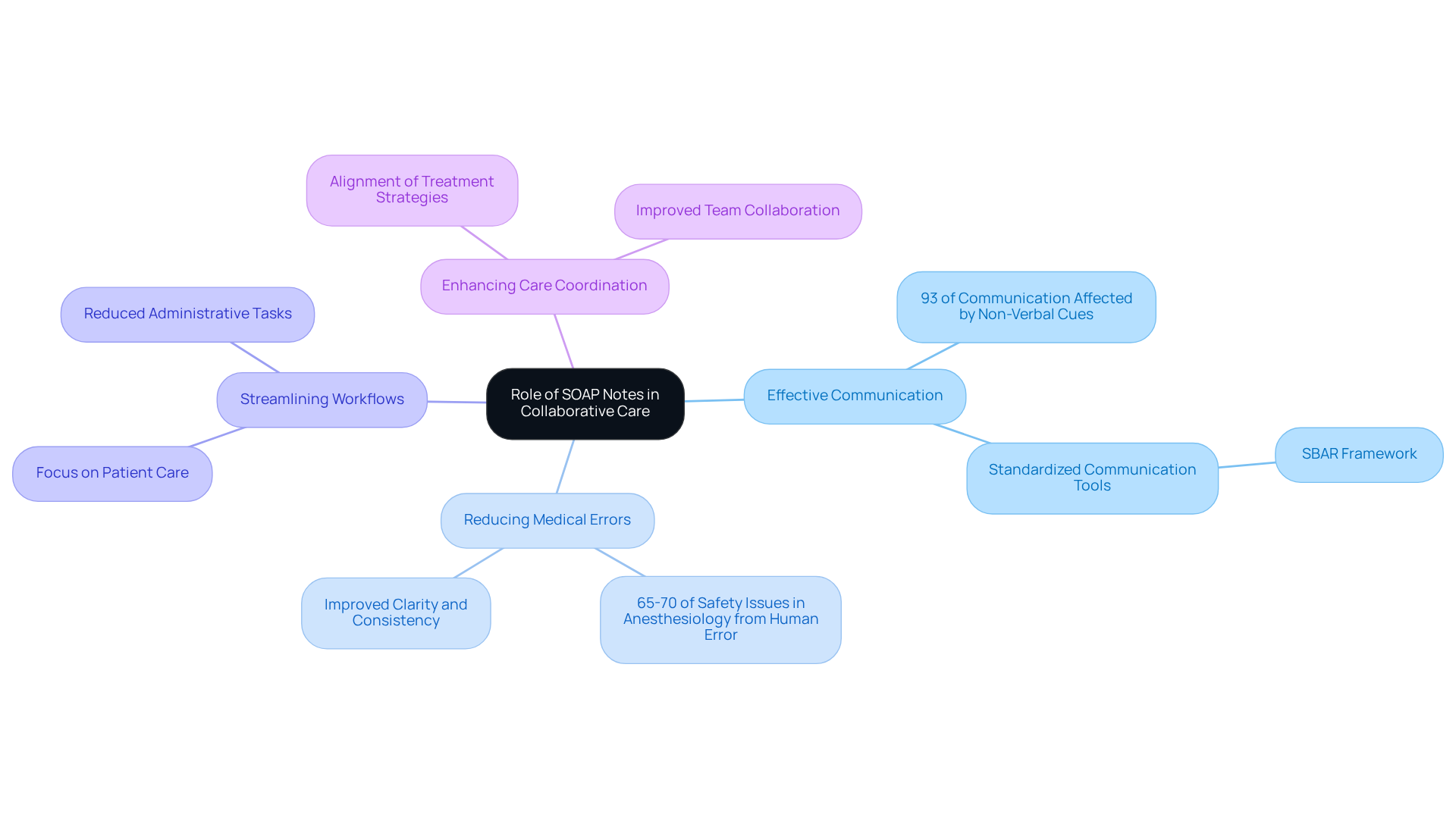
Collaborative Care: The Role of SOAP Notes in Multidisciplinary Teams
In multidisciplinary groups, documentation plays a vital role in fostering effective communication, ensuring that every team member is aware of an individual's status and treatment plan. Have you ever considered how crucial it is for everyone involved to be on the same page? By providing a clear and concise overview of client interactions, documentation nurtures teamwork among providers from various specialties, ultimately enhancing the quality of care we deliver.
Refreshing documentation regularly during team gatherings can significantly boost collaboration and health outcomes. For instance, organized documentation has been shown to reduce medical errors—one of the leading causes of harm to individuals—by improving clarity and consistency in clinical communication. Did you know that studies indicate 65-70 percent of safety issues in anesthesiology stem from human mistakes? This underscores the importance of structured documentation in preventing such errors.
Moreover, effectively utilizing documentation can streamline workflows, allowing healthcare practitioners to focus more on patient care rather than administrative tasks. As Vivian Chung Easton insightfully notes, the clarity and structure of clinical records enhance consistency in medical reporting, which in turn improves care coordination for individuals. This collaborative approach not only strengthens communication but also ensures that all team members are aligned in their treatment strategies, thereby enhancing overall care coordination.
Let’s continue to support one another in overcoming these challenges, ensuring we provide the best possible care for our patients.
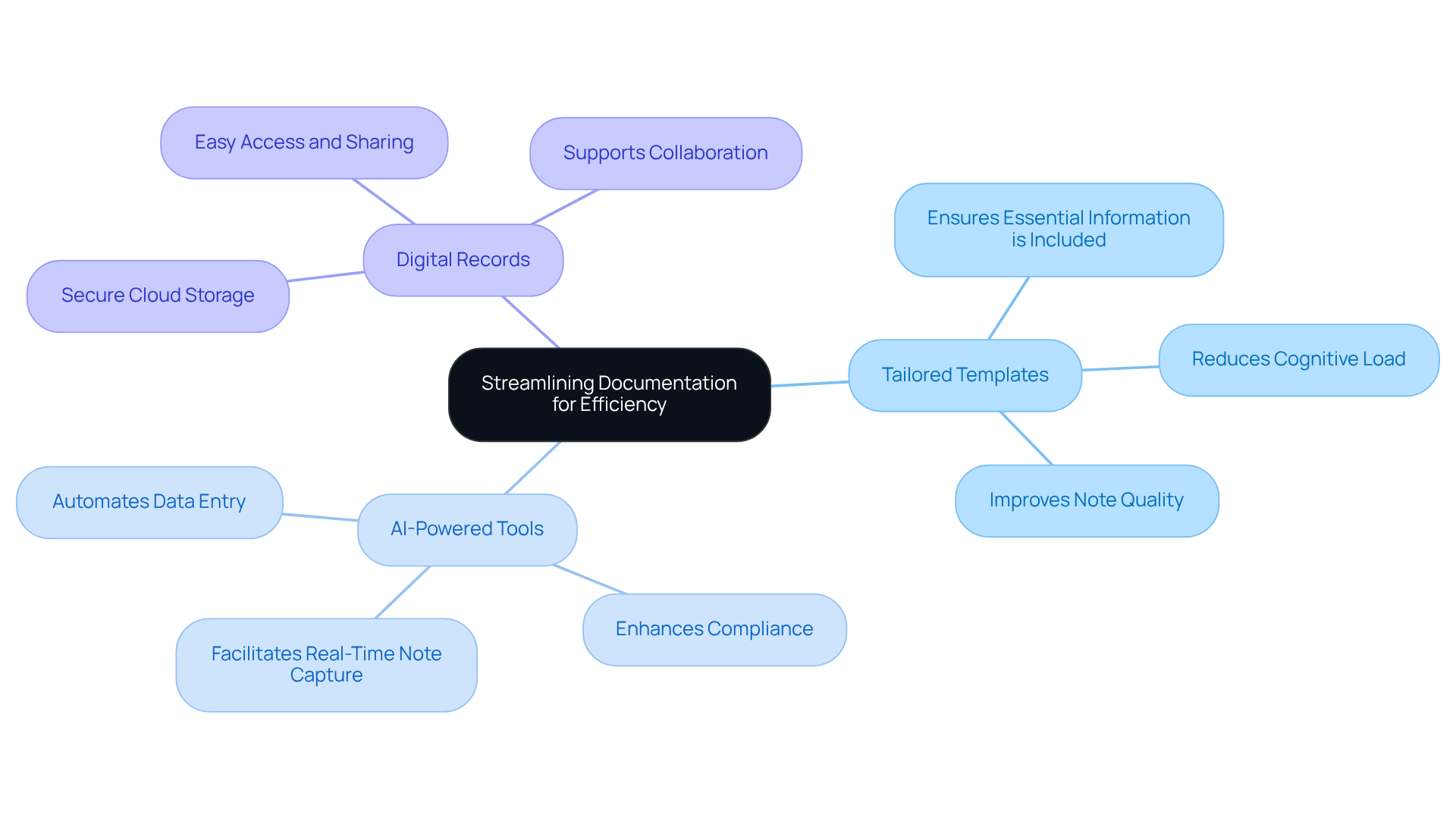
SOAP Note Templates: Streamlining Documentation for Efficiency
Healthcare professionals often face emotional challenges due to the burdens of record-keeping. Templates, such as a full soap note example, can significantly alleviate these pressures by allowing providers to enter essential information without starting from scratch. Have you ever felt overwhelmed by the demands of documentation? Tailored templates ensure that vital components are always included, allowing you to focus more on the care you provide.
By streamlining record-keeping, you can dedicate more time to patient care, which not only enhances your job satisfaction but also leads to better outcomes for your patients. Research indicates that organized documentation—like that provided by structured formats—improves clarity and brevity, fostering better decision-making and coordination within care teams. For instance, a study revealed that implementing structured templates led to a remarkable improvement in observation quality, with clarity and conciseness metrics showing significant gains.
Moreover, utilizing digital records allows for secure, cloud-based storage, enabling swift access and sharing of information among healthcare professionals. This enhances communication and teamwork, creating a more supportive environment for both staff and patients. To further ease your administrative burdens, consider integrating AI-powered tools that automate data entry and retrieval.
Overall, the incorporation of tailored templates, enhanced by generative AI, is a vital step toward creating a full soap note example and improving record efficiency in healthcare settings. Embrace these solutions to lighten your load and enhance the care you provide.
Key Solutions:
- Tailored templates for essential information.
- AI-powered tools for automated data entry.
- Digital records for secure, easy access.
These improvements not only make your work easier but also enrich the patient experience, paving the way for a more compassionate healthcare system.
Training Resources: Enhancing SOAP Note Writing Skills for Providers
Ongoing training is vital for healthcare providers who strive to enhance their SOAP note writing skills. Have you ever felt overwhelmed by the demands of documentation? Engaging in workshops, online courses, and peer review sessions offers not only valuable feedback but also fosters a nurturing environment for continuous improvement in writing practices. For instance, customized workshops have shown significant improvements in staff understanding of electronic health record (EHR) systems, leading to better accuracy and safety for patients.
By investing in such training, providers can ensure their documentation meets the highest standards of precision and clarity. This commitment ultimately enhances patient care outcomes, which is what we all strive for. As healthcare professionals often emphasize, effective training is not merely an option; it is a necessity for maintaining excellence in clinical records. Let’s embrace this opportunity for growth together.

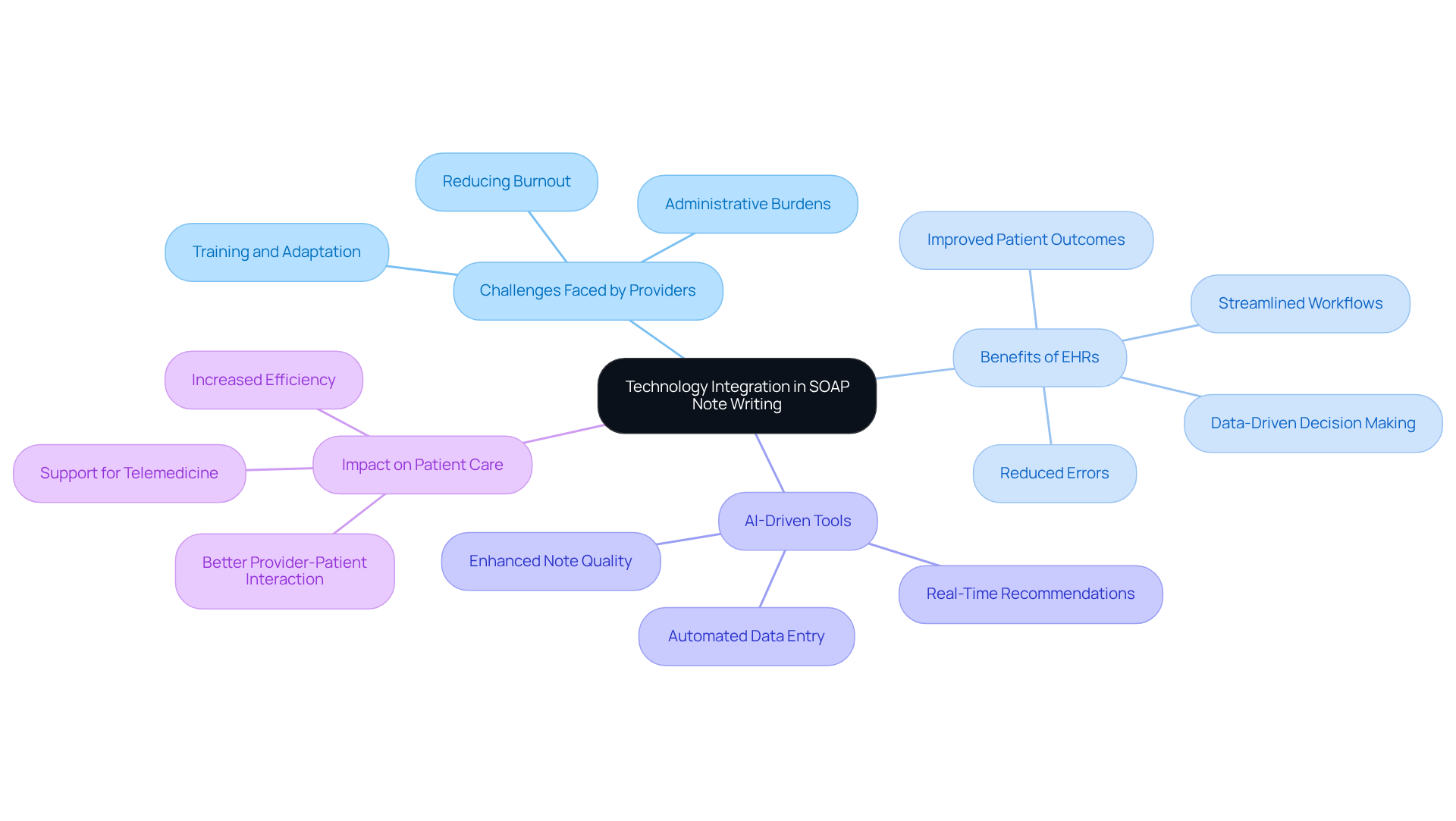
Technology Integration: Enhancing SOAP Note Writing with Digital Tools
Integrating digital tools into the SOAP note writing process can profoundly alleviate the emotional challenges faced by healthcare providers, significantly enhancing both efficiency and accuracy. Many providers experience administrative burdens that contribute to burnout, impacting their ability to deliver quality patient care. Electronic health records (EHR) systems and AI-driven record-keeping software automate data entry, allowing healthcare professionals to focus more on their patients rather than administrative tasks.
EHRs optimize workflows by incorporating clinical guidelines and decision-support tools directly into the recording process. This not only reduces the time spent on note-taking but also minimizes errors, fostering a more supportive environment for both providers and patients. Research indicates that methods utilizing EHRs save thousands of clinician hours each year, underscoring how these systems can positively influence record-keeping efficiency and the overall well-being of healthcare professionals.
Moreover, AI-driven tools provide real-time recommendations for enhancing note quality, ensuring that records are thorough and compliant with regulatory standards. Platforms like Twofold and Noterro offer organized outputs tailored for specific clinical settings, improving record accuracy while streamlining the process for providers. By embracing these technologies, healthcare professionals can significantly reduce their administrative load, leading to better outcomes for their patients and a more efficient workflow.
Have you considered how adopting these digital solutions could transform your daily practice? By taking this step, you not only lighten your workload but also enhance the care you provide. Together, let’s explore how these innovations can support you in your vital role.
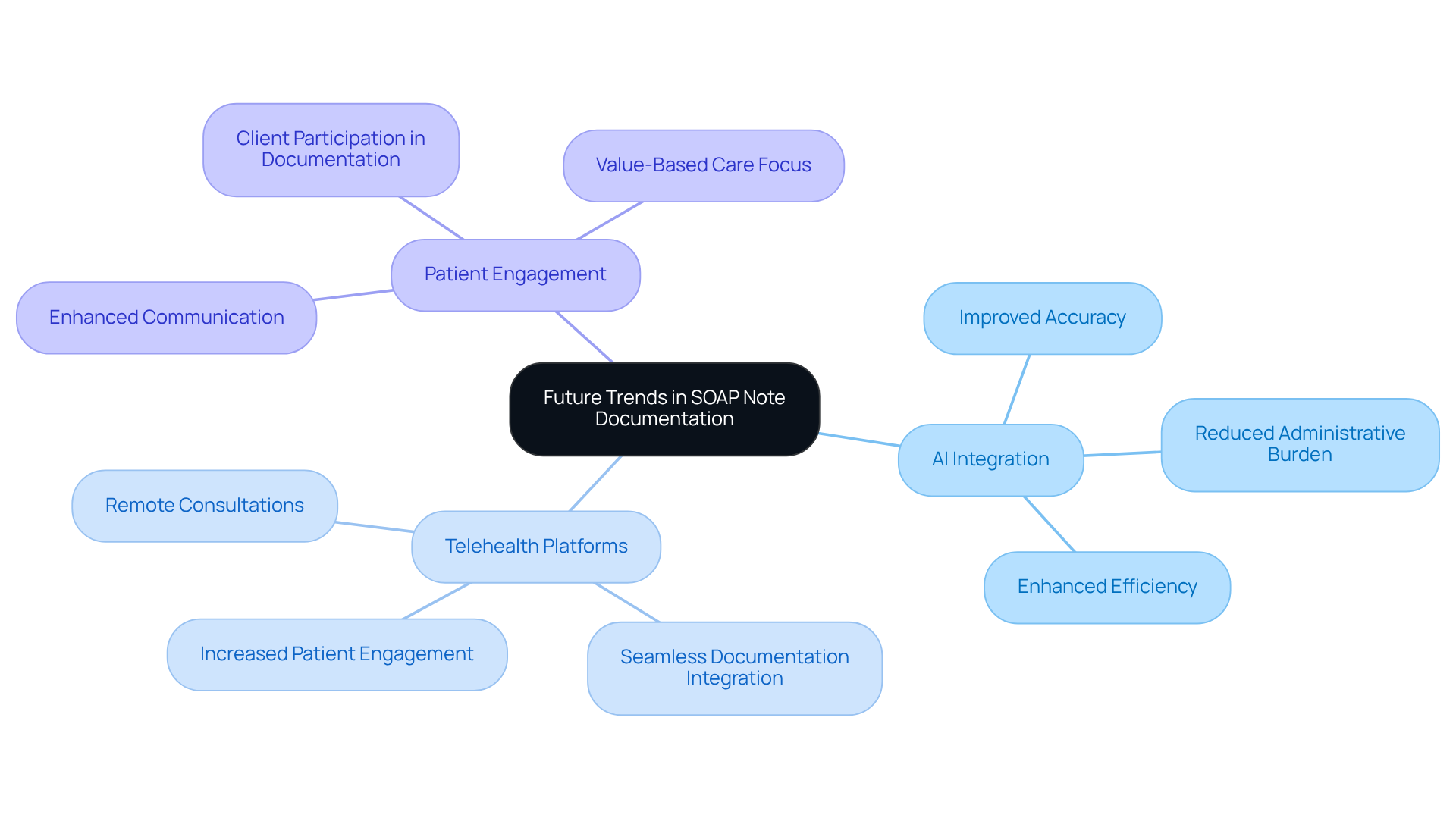
Future Trends: Evolving Practices in SOAP Note Documentation
As the healthcare landscape evolves, the practices surrounding the recording of a full soap note example must also adapt. The integration of AI is set to revolutionize record-keeping, allowing providers to focus more on what truly matters—patient care. Imagine AI-driven tools that streamline documentation, enhancing both accuracy and efficiency. In fact, 83% of doctors believe that AI can significantly reduce administrative burdens, ultimately improving healthcare delivery and transforming how clinical documentation is created.
Telehealth platforms are becoming increasingly vital in shaping the future of SOAP notes. With the surge in remote consultations, it's essential that documentation practices evolve to seamlessly integrate with telehealth systems. This transition not only boosts the efficiency of note-taking but also fosters greater engagement among individuals, as over 75% feel that digital tools enhance their healthcare experience. This vital connection between telehealth and individual engagement is crucial for elevating the quality of SOAP notes.
Moreover, the emphasis on client participation in documentation is gaining importance. As healthcare transitions to value-based care, understanding individual perceptions and experiences is essential. Open dialogue between providers and individuals can enrich documentation quality, making it more reflective of their unique needs and outcomes. Dr. Glen Stream highlights that consumer health technologies can strengthen the patient-physician connection, which is increasingly important in this changing landscape.
In summary, a full soap note example will illustrate that the future of SOAP note documentation will be marked by increased automation through AI, better integration with telehealth, and a heightened focus on patient engagement. It’s crucial for providers to remain informed about these trends, adapting their practices to ensure compliance with regulatory standards while delivering compassionate, high-quality care.
Conclusion
In summary, effective SOAP note documentation is a cornerstone of high-quality healthcare delivery. Have you ever felt overwhelmed by the administrative burdens that can detract from patient care? By mastering the structure of Subjective, Objective, Assessment, and Plan, healthcare providers can significantly enhance their documentation practices. This leads not only to improved patient outcomes but also to a reduction in those burdens that can weigh heavily on your daily responsibilities.
The integration of AI technology, as demonstrated by CosmaNeura, exemplifies how automation can streamline record-keeping. Imagine being able to focus more on what truly matters—your patients—rather than getting lost in paperwork. Key insights from the article highlight the importance of:
- Accuracy in documentation
- Necessity of avoiding common pitfalls
- Versatility of SOAP notes across various healthcare disciplines
Furthermore, the adoption of tailored templates and ongoing training resources can empower you to refine your writing skills. This ultimately fosters a culture of continuous improvement in your practice. As the healthcare landscape continues to evolve, embracing these innovations and best practices is crucial. By prioritizing effective documentation and leveraging technology, you can alleviate administrative burdens while enhancing the quality of care delivered to your patients.
The journey toward improved healthcare documentation is a shared responsibility. Let’s take proactive steps together to create a more efficient, compassionate, and patient-centered healthcare environment. Your commitment to these practices not only benefits you but also profoundly impacts the lives of those you care for.




