Introduction
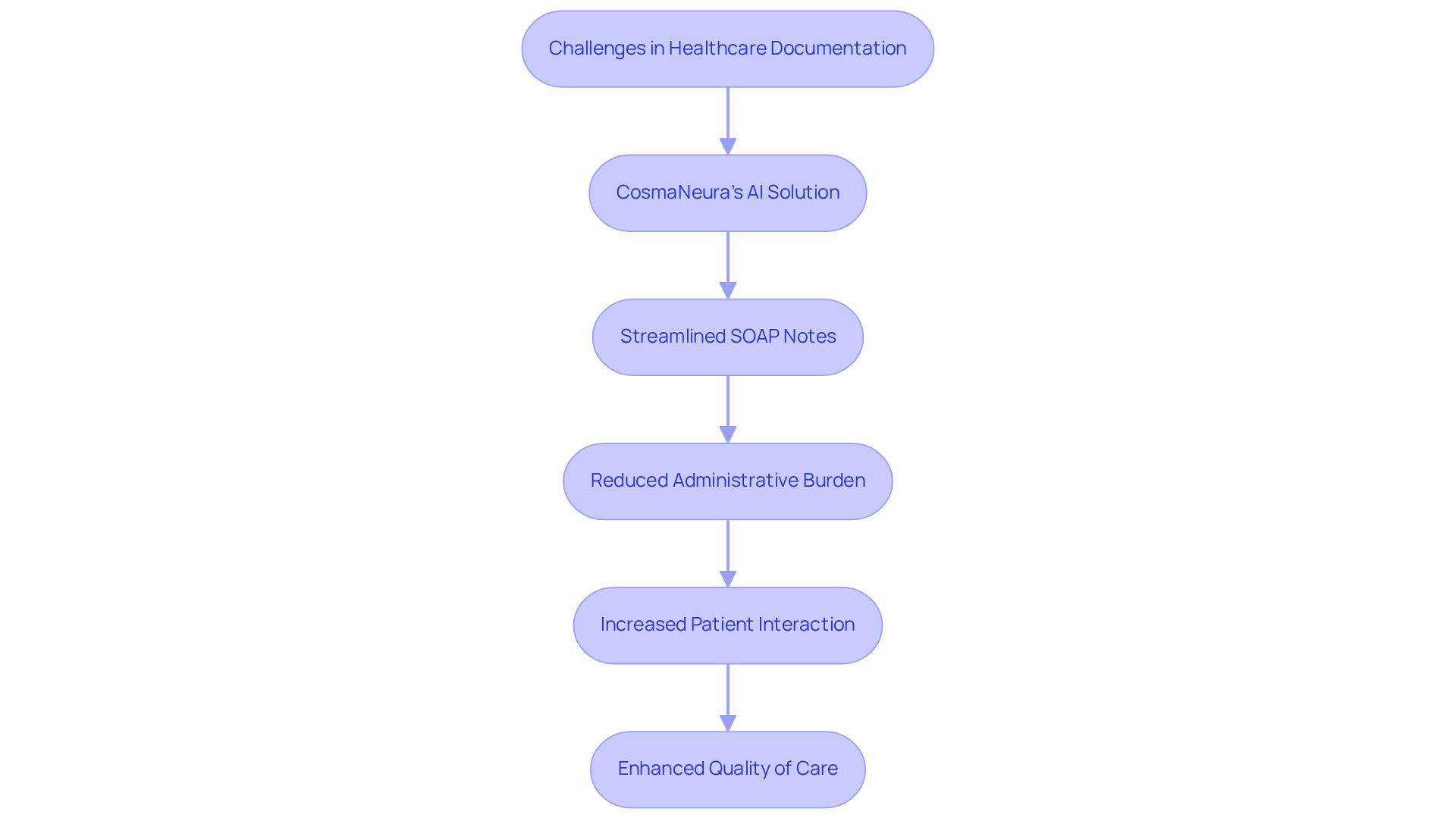
Healthcare providers often find themselves overwhelmed by a mountain of paperwork, which pulls them away from their true calling: delivering exceptional patient care. This constant juggling act can be emotionally draining. How can they balance the need for thorough documentation with the desire for meaningful patient interactions?
In this article, we’ll explore ten essential SOAP note guidelines designed to streamline documentation processes. By embracing these guidelines, healthcare providers can enhance efficiency and ultimately improve the quality of care they offer. As the landscape of healthcare continues to evolve, it’s crucial for providers to adapt their practices to not only meet these guidelines but also to tackle the administrative burdens that can weigh them down.
Imagine a world where documentation doesn’t feel like a chore but rather a tool that supports patient care. By implementing these strategies, providers can reclaim precious time and focus on what truly matters—their patients. Let’s dive into these guidelines and discover how they can transform the way you approach documentation.
CosmaNeura: Streamline SOAP Notes with AI-Powered Documentation
Healthcare providers often face overwhelming administrative burdens that can detract from their primary focus: patient care. Have you ever felt the weight of paperwork pulling you away from what truly matters? CosmaNeura understands these challenges and offers a compassionate solution.
By utilizing advanced AI technology, CosmaNeura streamlines the generation of soap note guidelines for effective record-keeping. This allows you to create precise notes according to soap note guidelines in real-time during client interactions, significantly reducing the time spent on administrative tasks. Imagine regaining those precious moments to connect with your patients, enhancing both your efficiency and the quality of care you provide.
This innovation not only boosts clinical efficiency but also addresses the common resistance to change in healthcare, especially among physicians concerned about maintaining care quality. As healthcare costs continue to rise, CosmaNeura's AI solutions improve financial efficiency by simplifying record-keeping processes. This means you can focus more on delivering compassionate and effective care.
As the healthcare landscape evolves, incorporating AI in record-keeping is becoming essential. Studies suggest that clinicians could cut their record-keeping time by up to 50% by 2027. This shift not only enhances workflow efficiency but also aligns with ethical standards rooted in Catholic teachings, ultimately improving the overall quality of care.
Are you ready to embrace a solution that prioritizes both your time and your patients' well-being? Let’s work together to transform the way you manage records, allowing you to focus on what you do best—caring for your clients.
Understand the SOAP Note Structure: Subjective, Objective, Assessment, Plan
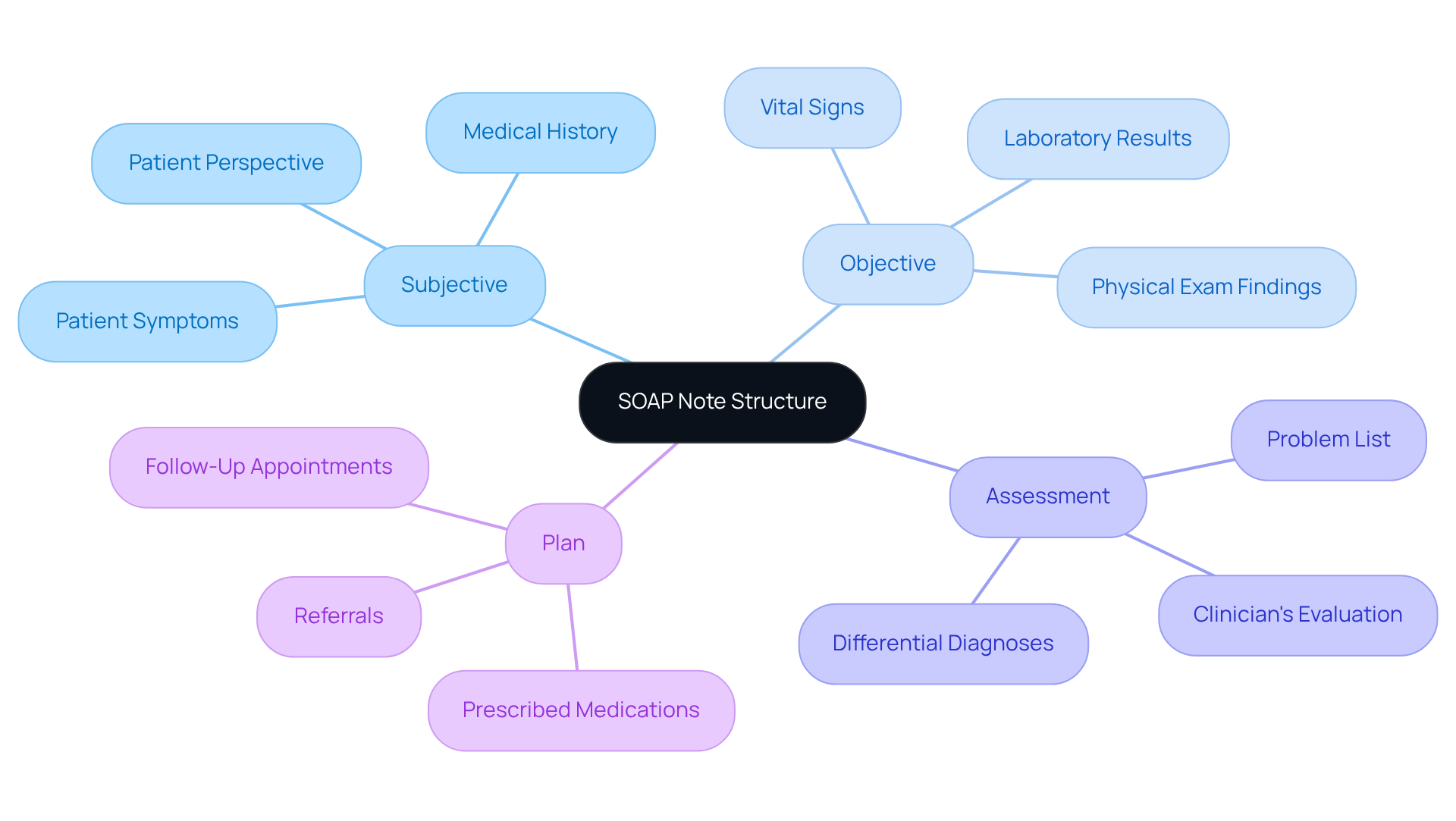
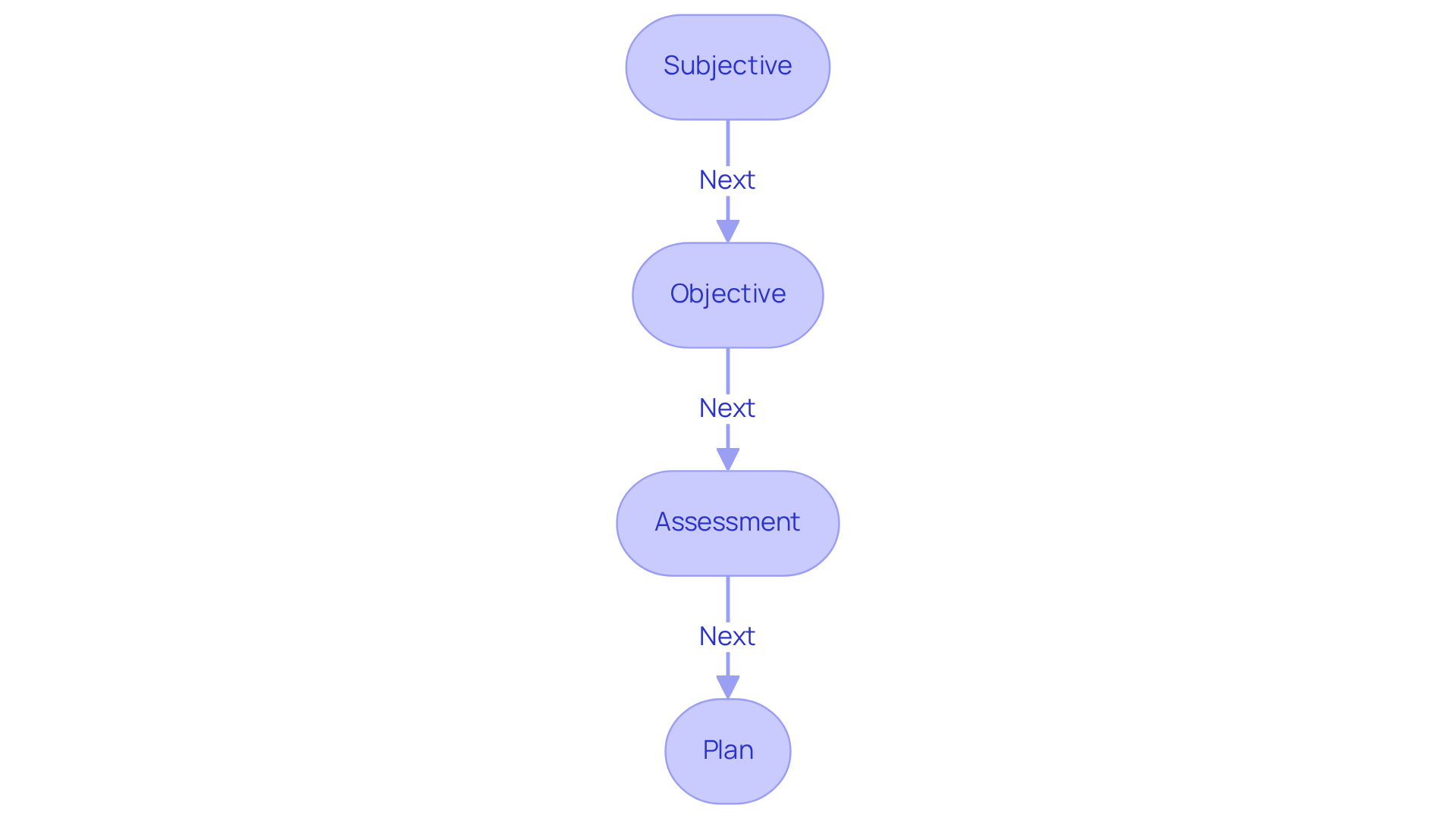
SOAP notes are structured into four essential components that facilitate effective patient documentation:
-
Subjective: This section captures the patient's reported symptoms and feelings, offering valuable insight into their condition from their perspective. It includes details such as the primary complaint and any relevant medical history, ensuring a comprehensive understanding of the individual's experience. Have you ever felt rushed during a consultation? By leveraging generative AI, physicians can analyze patient-reported data to identify patterns and trends that inform better care decisions, addressing the dissatisfaction stemming from hurried interactions.
-
Objective: In this part, healthcare providers document observable and measurable data, including vital signs, physical examination results, and laboratory findings. This objective information is crucial for forming an accurate clinical picture and aids in the assessment process. Imagine how much easier it would be if AI tools could automate the gathering and examination of this data. This would lessen the administrative load on healthcare providers, allowing them to focus more on meaningful interactions with individuals, especially in light of current labor shortages.
-
Assessment: This section combines the subjective and objective data to offer the clinician's evaluation of the individual's condition. It often includes a problem list and differential diagnoses, guiding further treatment decisions. By incorporating AI, physicians can enhance their diagnostic abilities, leading to more precise evaluations and better outcomes for individuals. This not only improves care but also alleviates some of the pressure linked to administrative tasks.
-
Plan: The strategy outlines the next steps in healthcare, detailing prescribed medications, referrals, additional testing, and follow-up appointments. This roadmap is vital for ensuring continuity of care and effective communication among healthcare providers. Generative AI can streamline this process by automating reminders and follow-ups, thus reducing some of the administrative tasks that contribute to physician burnout.
Understanding the SOAP note guidelines is crucial for healthcare providers, as it enhances record accuracy, improves patient safety, and fosters better communication within clinical teams. Training initiatives for healthcare workers are essential for the effective execution of structured documentation, helping to overcome obstacles like staff pushback and insufficient resources. The structured format developed by Larry Weed almost half a century ago acts not only as a recording tool but also as cognitive support for accessing information. Moreover, the format can be rearranged into APSO (Assessment, Plan, Subjective, Objective) to enhance efficiency in clinical documentation, particularly in the context of integrating AI.
Review SOAP Note Examples: Practical Applications for Healthcare Providers
Here are several practical examples of SOAP notes in action:
-
Example 1: Headache
- Subjective: The patient reports experiencing a severe headache for the past two days, rating it 8 out of 10.
- Objective: Vital signs are stable; no neurological deficits are observed.
- Assessment: Likely a tension headache.
- Plan: Recommend over-the-counter pain relief and schedule a follow-up in one week.
-
Example 2: Diabetes Management
- Subjective: The patient states they have been feeling fatigued and experiencing increased thirst.
- Objective: Blood glucose level is recorded at 250 mg/dL.
- Assessment: Poorly controlled diabetes.
- Plan: Adjust medication dosage and schedule a follow-up appointment in two weeks.
These examples illustrate how to effectively record patient interactions using soap note guidelines in a structured format. By utilizing soap note guidelines, healthcare providers can enhance record accuracy by 22% and reduce note completion time by 31%.
Imagine the relief of having more time to focus on patient care rather than paperwork. Integrating innovative AI solutions, like CosmaNeura's Agentic Platform, can significantly improve clinical documentation and streamline AI Medical Billing workflows. This not only provides a clear framework for treatment planning but also addresses the pressing issues of physician burnout and resistance to innovation.
The soap note guidelines established in the 1950s by Lawrence Weed continue to serve as a vital resource, promoting clarity and consistency in clinical records. By embracing these practices, we can improve care for individuals and tackle the administrative challenges that often hinder healthcare provision.
Are you ready to explore how these tools can transform your practice and enhance patient care?
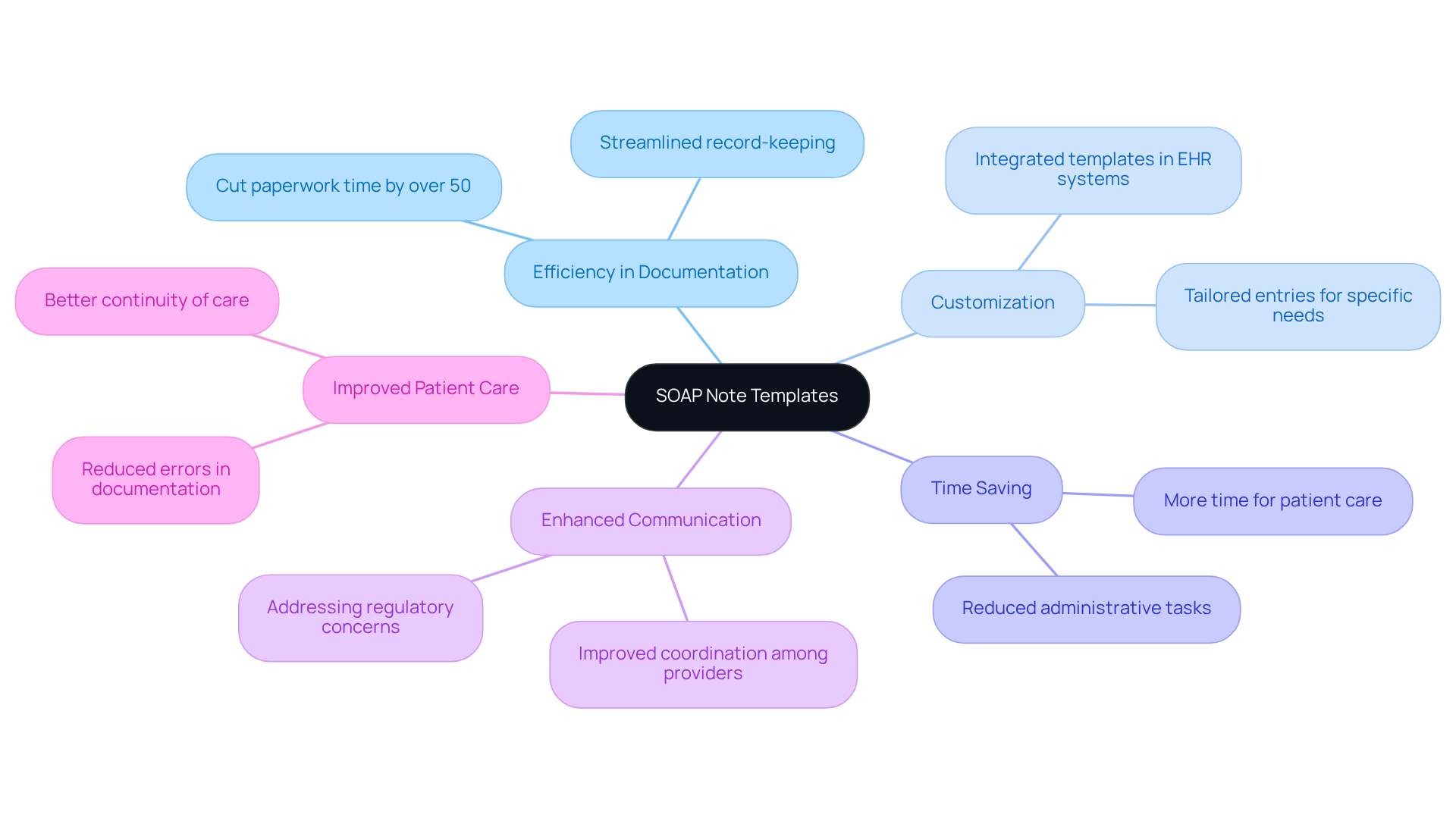
Utilize SOAP Note Templates: Enhance Efficiency in Documentation
Structured templates can truly transform the way healthcare providers manage their records. Have you ever felt overwhelmed by the sheer volume of paperwork? It’s a common struggle that can take precious time away from patient care. By offering an organized format, these templates ensure that all important information is recorded uniformly, allowing you to focus more on what really matters—your patients.
Imagine being able to customize entries to fit your specific needs, making data input quicker and more efficient. Many electronic health record (EHR) systems come equipped with integrated templates that follow soap note guidelines and automatically fill in client information. This feature has been shown to save providers significant time—research indicates that using standardized templates can cut paperwork time by over 50%! This means more time for you to concentrate on delivering quality care rather than getting bogged down by administrative tasks.
Moreover, these templates enhance communication and coordination among providers, addressing the challenges posed by fragmented healthcare systems. Regulatory concerns, like HIPAA, can create barriers to effective communication, but personalized templates can help bridge those gaps. By incorporating commonly used fields and specific clinical needs while following soap note guidelines, you can ensure that your records are both comprehensive and streamlined.
By adopting these practices, you can improve your workflow, reduce errors, and ultimately enhance the quality of patient care. Isn’t it time to take a step towards a more efficient and compassionate approach to healthcare? Let’s work together to make your administrative tasks easier, so you can focus on what you do best—caring for your patients.
Engage in SOAP Note Training: Improve Documentation Skills
Healthcare providers often face overwhelming administrative burdens that can impact their ability to deliver the best care. Have you ever felt that the paperwork takes away from your time with patients? Engaging in training programs that follow soap note guidelines can significantly enhance your skills and alleviate some of that stress.
Consider workshops, online courses, and peer review sessions. These opportunities provide invaluable feedback and insights into best practices. They focus on essential aspects like:
- Creating clear and concise records
- Avoiding common pitfalls
- Effectively utilizing technology to simplify the recording process
Research, including a study by Almasi et al., shows that structured training significantly improves record accuracy, with a p-value of <0.001. This improvement leads to better care outcomes for your patients. Moreover, using digital tools, such as standardized templates for clinical records, can enhance the structure and quality of your writing.
By implementing these best practices and emphasizing the importance of proofreading, you can ensure your records meet the highest standards. This not only benefits your practice but also enhances the care you provide to your patients. Remember, taking these steps can lead to a more fulfilling and effective practice. Why not explore these training options today?
Identify Common SOAP Note Mistakes: Enhance Accuracy and Clarity
Recognizing the common challenges in adhering to soap note guidelines is crucial for enhancing precision and clarity in patient care. Have you ever felt overwhelmed by the administrative demands of your role? You're not alone. Many healthcare providers grapple with these issues, which can impact the quality of care they deliver. Here are some key pitfalls to avoid:
- Vague Language: Using non-specific terms can lead to misunderstandings among healthcare providers. For instance, phrases like 'the client seemed fine' lack the clarity needed for effective communication. Research shows that organized documentation can reduce medical mistakes by 40%. This highlights just how important clarity is in our records.
- Incomplete Information: Omitting relevant details can jeopardize patient care. Comprehensive records are vital for maintaining consistency in treatment strategies. As noted by the Social Work Portal Team, 'the soap note guidelines ensure the completeness of progress notes.'
- Overgeneralization: Avoid making broad statements without evidence. For example, saying 'the individual is anxious' without detailing specific symptoms can lessen the clinical value of your documentation. Including specific, measurable observations is essential for supporting clinical decisions.
- Neglecting Follow-Up: Not having a clear follow-up strategy can hinder the management of individuals. A well-defined follow-up plan is crucial for monitoring progress and ensuring that individuals receive the support they need. Consider using templates or digital tools to streamline this process, making thorough documentation easier.
By acknowledging these challenges, you can significantly enhance the precision and transparency of your documentation. This not only improves outcomes for individuals but also fosters better communication among care teams. Let's work together to create a supportive environment where clarity in documentation leads to better patient care.
Integrate SOAP Notes with EHR Systems: Improve Accessibility and Workflow
Healthcare providers often face overwhelming administrative burdens that can detract from their ability to deliver compassionate care. Have you ever felt that the time spent on paperwork takes away from the moments that truly matter with your patients? Incorporating clinical documentation with electronic health record (EHR) systems can be a game-changer in this regard.
This integration allows you to effortlessly access and modify client information, ensuring that all records are centralized and readily available. Imagine the relief of having patient information at your fingertips, streamlining your workflow and allowing you to focus more on what you love—caring for your patients. EHR systems can significantly reduce the time dedicated to record-keeping, which not only lowers the chances of mistakes but also enhances the quality of care you provide.
By embracing this technology, you can reclaim precious time and reduce stress in your daily routine. It’s not just about efficiency; it’s about creating a more nurturing environment for both you and your patients. Let’s explore how integrating EHR systems can transform your practice and improve patient outcomes. Together, we can make a difference.

Review and Update SOAP Note Practices: Stay Current with Best Practices
Healthcare providers often face overwhelming administrative burdens that can detract from their primary focus: patient care. Have you ever felt the weight of paperwork overshadowing your ability to connect with patients? It’s a common challenge, and it’s crucial to address it.
To navigate these complexities, it is essential to prioritize the regular review and enhancement of soap note guidelines. Participating in workshops and peer evaluations can significantly improve writing skills, ensuring that you meet legal and ethical standards. Did you know that a staggering 97% of organizations lack effective digital document processes? This highlights a pressing need for improvement in this area.
Moreover, without a solid document management strategy, 25% of documents may ultimately be lost. This statistic underscores the dangers of inadequate record-keeping practices. By committing to ongoing education and adapting to changes in record-keeping standards, you can enhance the quality of care you provide while minimizing risks associated with insufficient record maintenance.
As Julie Taitsman, Chief Medical Officer for the US Department of Health and Human Services, wisely states, "Effective record-keeping enhances safety and quality of care." By applying the soap note guidelines—such as utilizing structured templates and reducing jargon—you can foster clearer communication and better outcomes for your patients.
Furthermore, it’s important to recognize that 95% of ensuring suitable reimbursement is tied to effective record-keeping practices. This connection emphasizes the importance of a proactive strategy for improving clinical record practices.
Key Solutions:
- Engage in regular training and workshops.
- Implement structured templates for documentation.
- Develop a robust document management strategy.
Ultimately, a commitment to enhancing your record-keeping practices is vital for upholding high standards of patient care and ensuring compliance with regulations. Let’s work together to create a more efficient and compassionate healthcare environment.
Seek Peer Feedback on SOAP Notes: Foster Continuous Improvement
Engaging in peer feedback on soap note guidelines can truly transform the way healthcare providers collaborate. Have you ever felt overwhelmed by the administrative burdens that can distract from patient care? By sharing documentation with colleagues for review, you can gain valuable insights into your practices, helping to pinpoint areas for enhancement. This collaborative approach not only boosts individual skills but also fosters a stronger, more efficient team in delivering care.
Statistics show that effective communication and collaboration among healthcare teams significantly enhance the quality of care delivered. Teams that prioritize feedback often achieve better patient outcomes. As the saying goes, 'success is best when it's shared.' This highlights the collective effort needed to achieve better results.
Creating an environment where providers regularly examine one another's records promotes accountability and collective learning. This ultimately leads to improved record-keeping practices and a more unified healthcare delivery system in accordance with soap note guidelines. Remember, 'together we become strong because teamwork and collaboration enable us to achieve remarkable outcomes.' This underscores the importance of trust and mutual respect in effective teamwork.
Key Benefits of Peer Feedback:
- Enhances individual abilities
- Increases overall team efficiency
- Promotes responsibility and collective learning
Let’s embrace this culture of continuous improvement together. By supporting one another, we can navigate the challenges of healthcare more effectively and ensure that our patients receive the best care possible.

Understand Legal Implications of SOAP Notes: Protect Your Practice
SOAP records serve as vital legal documents that can protect healthcare providers during disputes or audits. Have you ever considered how precise and comprehensive records can showcase your adherence to legal and regulatory standards, including HIPAA regulations? As of May 2024, 28% of medical groups reported using ambient AI technology to transcribe speech or create records. This statistic highlights our growing reliance on technology for effective record-keeping.
It's essential for providers to recognize the legal implications of their records. Confidentiality and adherence to HIPAA regulations are paramount. Insufficient or incomplete clinical records can lead to serious allegations of negligence or malpractice. This reality underscores the risks associated with inadequate record-keeping. By maintaining high standards in clinical documentation and ensuring that records are securely stored in compliance with state and federal regulations, you can protect your practice and provide ethical care for your patients.
Well-organized documentation not only supports continuity of care by offering a clear, time-stamped record of interactions but also enhances safety and strengthens your accountability in clinical decision-making. Remember, the soap note guidelines are a foundational element of medical documentation, providing healthcare professionals with a structured method to capture, organize, and communicate patient information.
Key Solutions for Effective Record-Keeping:
- Utilize technology to streamline documentation processes.
- Regularly review and update clinical records to ensure completeness.
- Train staff on the importance of accurate record-keeping.
By taking these steps, you can foster a more efficient and compassionate healthcare environment.
Conclusion
Embracing effective SOAP note practices is essential for healthcare providers who want to enhance patient care while managing the weight of administrative tasks. Have you ever felt overwhelmed by paperwork? By prioritizing structured documentation, you can streamline your workflow, allowing you to focus more on your patients and less on the forms. Innovative tools, like CosmaNeura's AI-powered solutions, pave the way for a more efficient approach, transforming how records are maintained in healthcare settings.
In this article, we explored key aspects of SOAP notes, including:
- Their structure
- The importance of training
- Common pitfalls to avoid
- How they integrate with electronic health record (EHR) systems
By understanding and implementing these guidelines, you can improve the accuracy and clarity of your documentation. This not only enhances communication among clinical teams but also fosters better patient outcomes. Engaging in peer feedback and continuous training is vital, ensuring you stay current with best practices and legal requirements.
The importance of adopting these practices cannot be overstated. As healthcare evolves, so must our methods for documenting patient interactions. Embracing structured SOAP note guidelines protects your practice legally and promotes a culture of collaboration and accountability. It’s crucial for healthcare professionals to take proactive steps toward refining their documentation skills and utilizing available resources. This commitment ultimately leads to more compassionate and effective patient care.
So, what steps will you take today to enhance your documentation practices? Remember, every effort you make contributes to a more supportive environment for both you and your patients.




