Overview
The article highlights the emotional challenges healthcare providers face daily. With the pressures of administrative tasks, it’s easy to feel overwhelmed, which can impact patient care. How often do you find yourself wishing for a more streamlined way to document patient interactions?
This is where effective SOAP documentation comes into play. Structured SOAP notes—comprising subjective, objective, assessment, and plan components—are essential for capturing comprehensive patient information. By utilizing these notes, you can improve clinical decision-making and enhance treatment outcomes.
Consider the benefits of adopting structured SOAP notes:
- Improved communication with your team.
- Enhanced patient care through thorough documentation.
- Streamlined workflows that reduce administrative burdens.
By embracing this approach, you not only ease your workload but also foster a more nurturing environment for your patients. It’s about creating a space where you can focus on what truly matters—the well-being of those in your care.
Let’s take a step towards better patient care together. Explore how implementing structured SOAP notes can transform your practice and support your commitment to compassionate healthcare.
Introduction
In the intricate world of healthcare, effective documentation isn’t merely a bureaucratic task; it’s a vital part of delivering quality patient care. Healthcare providers often find themselves juggling the demands of administrative duties alongside the need for compassionate patient interactions. This dual pressure can make mastering SOAP documentation feel overwhelming.
How can we ease this burden? This article explores ten essential SOAP documentation examples designed to streamline the documentation process while enhancing the quality of care. By leveraging these examples, healthcare professionals can reduce their administrative load and ensure that every patient receives the attention they truly deserve.
Imagine a scenario where documentation feels less like a chore and more like a tool for better patient engagement. With the right strategies in place, it’s possible to transform the documentation experience into something that supports both providers and patients alike. Let’s dive into these examples and discover how they can make a meaningful difference in your practice.
CosmaNeura: AI-Powered SOAP Documentation for Efficient Patient Care
Healthcare providers often face overwhelming administrative tasks that can detract from their primary mission: caring for patients. Have you ever felt buried under paperwork, wishing you could spend more time with those who need your expertise?
CosmaNeura understands these emotional challenges. Our advanced AI technology transforms the management of SOAP documentation examples, significantly reducing the administrative burden on medical professionals. By automating data entry and ensuring accurate soap documentation examples, our platform enables you to prioritize client interactions over paperwork. This shift not only enhances operational efficiency but also improves the quality of care you provide, reflecting a deep commitment to compassionate medical service.
Consider this: 57% of physicians see the reduction of administrative burdens as the primary opportunity for AI. By integrating our solutions, you align perfectly with the evolving needs of primary care. As you regain valuable time, you can focus on what truly matters—improving outcomes and experiences for those receiving care.
Key Benefits of CosmaNeura:
- Less paperwork means more patient time.
- Accurate documentation enhances care quality.
- Streamlined processes improve operational efficiency.
Let’s work together to transform your practice. Imagine a world where you can dedicate your energy to healing rather than handling forms. Join us in this journey towards a more compassionate healthcare experience.
Understanding SOAP Notes: Key Components Every Provider Must Know
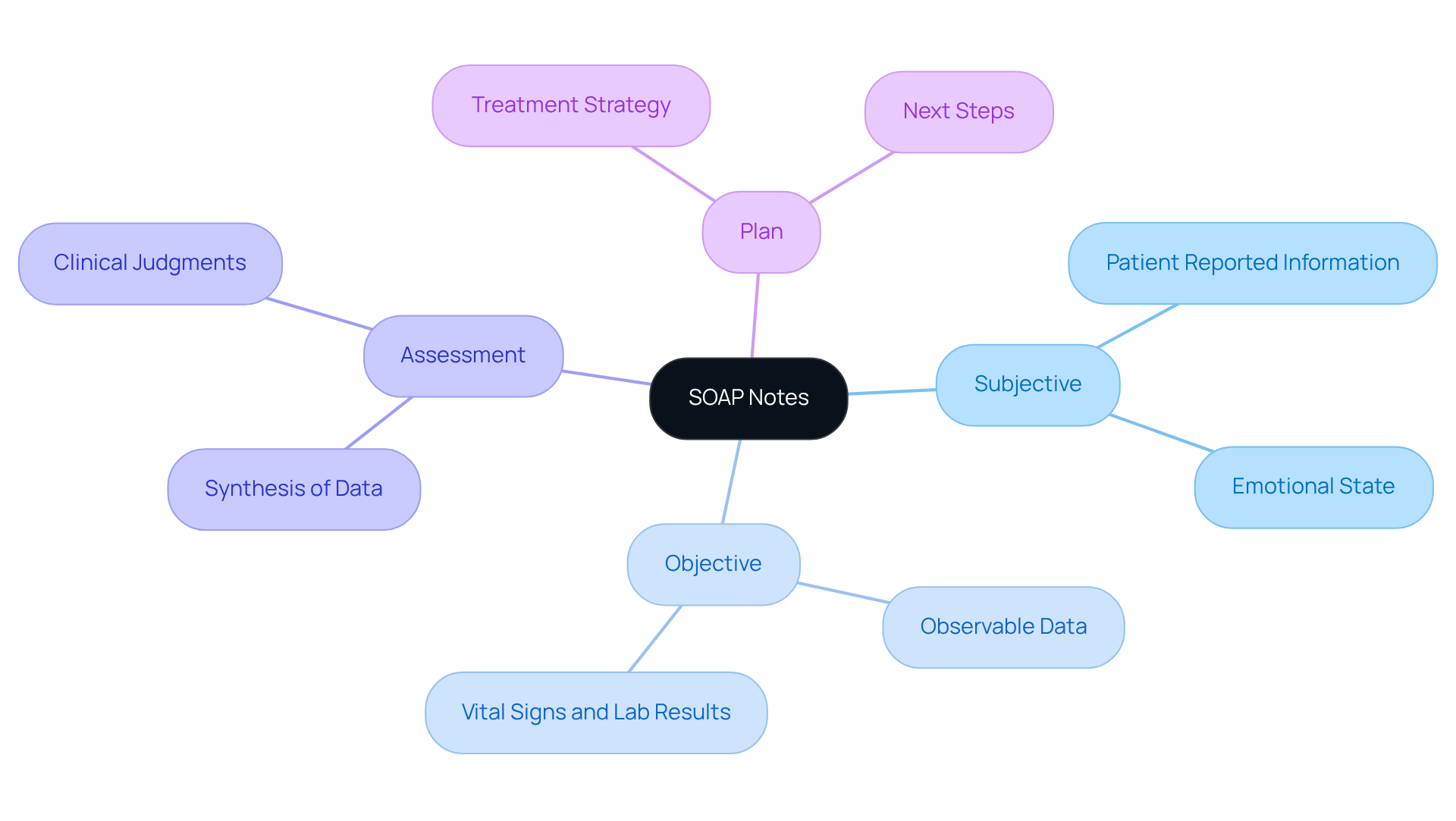
SOAP notes are structured into four essential components that not only facilitate effective clinical documentation but also support compassionate patient care:
- Subjective: This section captures the information reported by the patient, including their symptoms, concerns, and personal experiences. Understanding this perspective is crucial for recognizing the individual’s primary concern and emotional state.
- Objective: Here, observable data collected during the examination is documented, such as vital signs, lab results, and physical findings. This factual information is vital for forming an accurate clinical picture and ensuring that no detail is overlooked.
- Assessment: This component synthesizes the subjective and objective data, allowing the provider to make informed clinical judgments. It includes the diagnosis and highlights areas needing further exploration or intervention, ensuring that every patient feels heard and cared for.
- Plan: The outline describes the suggested treatment strategy, detailing next steps such as additional tests, medications, referrals, or education for the individual. A well-organized strategy guarantees continuity of care and clarity for future medical providers, fostering trust and understanding.
Comprehending these elements is crucial for producing impactful records that not only aid clinical decision-making but also improve outcomes for individuals. Have you ever considered how comprehensive medical records can significantly lower the chance of sentinel events? Research shows that they enhance communication between medical professionals, ultimately benefiting patient safety. Moreover, effective methods in clinical record-keeping have been demonstrated to streamline workflows, enabling healthcare providers to focus more on care rather than administrative duties. By adhering to these structured components, healthcare professionals can foster better engagement and improve overall treatment efficacy.
Let’s embrace these practices together, ensuring that every patient receives the compassionate care they deserve.
Real-World SOAP Note Examples: Practical Applications for Healthcare Providers
Here are several real-world examples of SOAP notes that illustrate effective documentation in primary care:
-
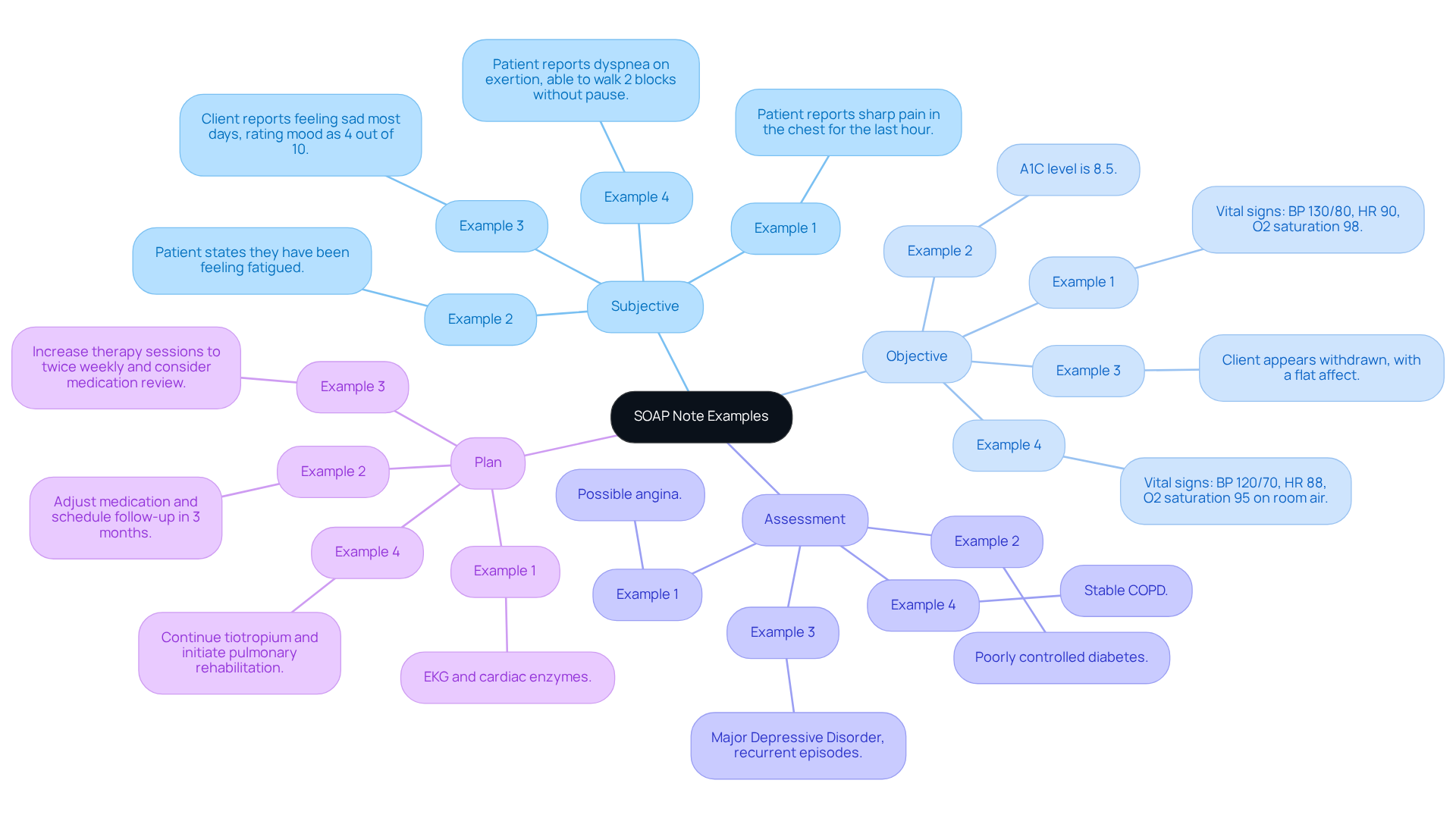
Example 1: An individual presents with chest pain.
- Subjective: Patient reports sharp pain in the chest for the last hour.
- Objective: Vital signs: BP 130/80, HR 90, O2 saturation 98%.
- Assessment: Possible angina.
- Plan: EKG and cardiac enzymes.
-
Example 2: A follow-up for diabetes management.
- Subjective: Patient states they have been feeling fatigued.
- Objective: A1C level is 8.5%.
- Assessment: Poorly controlled diabetes.
- Plan: Adjust medication and schedule follow-up in 3 months.
-
Example 3: An individual with recurrent depressive symptoms.
- Subjective: Client reports feeling sad most days, rating mood as 4 out of 10.
- Objective: Client appears withdrawn, with a flat affect.
- Assessment: Major Depressive Disorder, recurrent episodes.
- Plan: Increase therapy sessions to twice weekly and consider medication review.
-
Example 4: An individual experiencing shortness of breath.
- Subjective: Patient reports dyspnea on exertion, able to walk 2 blocks without pause.
- Objective: Vital signs: BP 120/70, HR 88, O2 saturation 95% on room air.
- Assessment: Stable COPD.
- Plan: Continue tiotropium and initiate pulmonary rehabilitation.
These soap documentation examples emphasize the significance of organized records in effectively capturing clinical interactions. By employing this structured format, medical practitioners can ensure continuity of care and enhance communication among colleagues.
Why is effective documentation so crucial? It not only assists in clinical decision-making but also improves health outcomes by providing a clear record of the individual's health status and treatment strategy.
Consider this: When we take the time to document thoughtfully, we’re not just fulfilling a requirement; we’re nurturing the patient-provider relationship and paving the way for better care. Let's continue to support each other in this vital aspect of healthcare.
Best Practices for Writing Effective SOAP Notes in Healthcare
Writing effective SOAP notes can feel overwhelming at times, but with a few best practices, you can make this task more manageable and impactful for patient care.
-
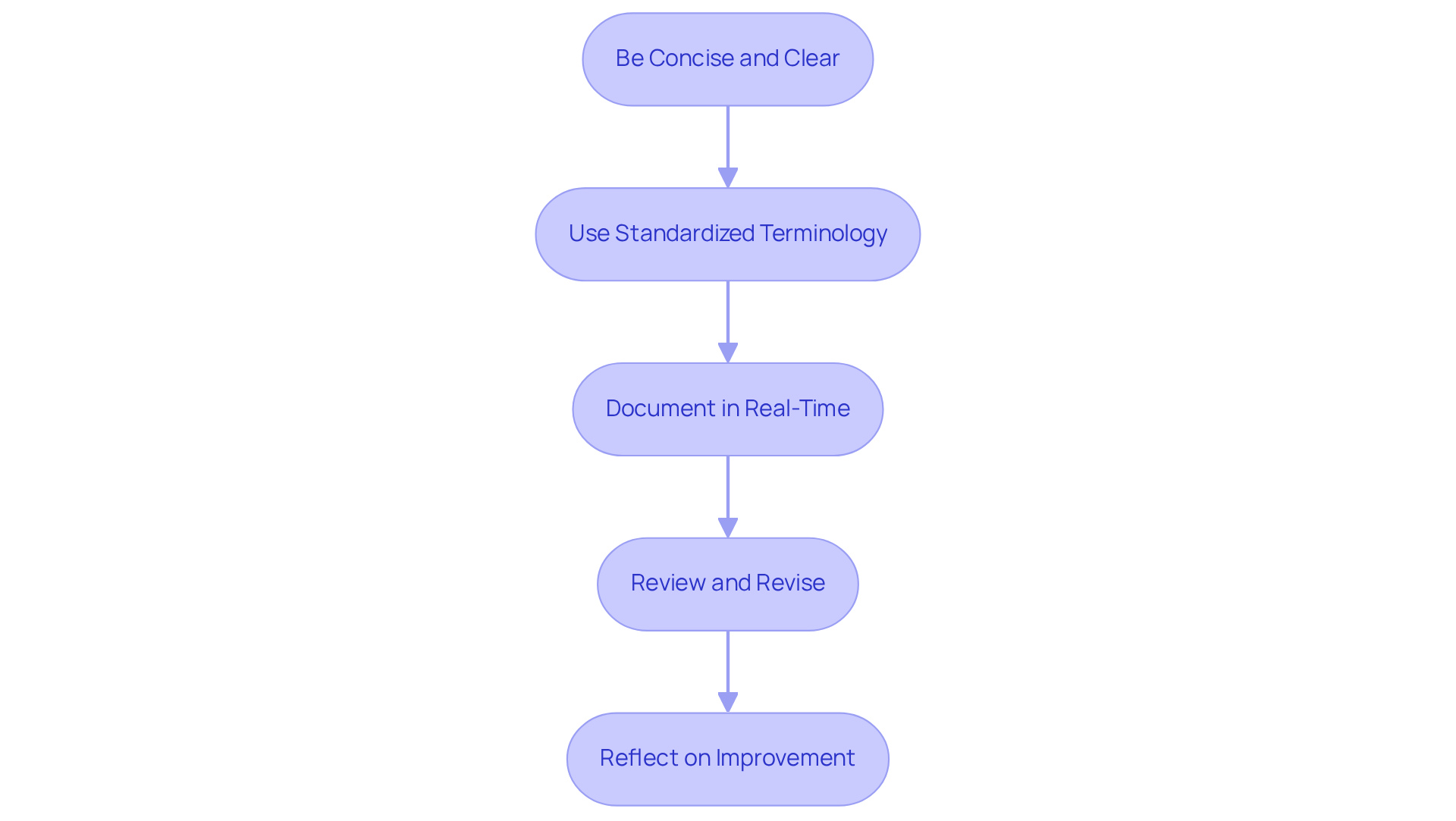
Be Concise and Clear: Use straightforward language to convey your thoughts. This clarity is essential, as even small errors can lead to significant implications for patient care. For instance, including significant negatives in your records can help ensure that no critical information is overlooked.
-
Use Standardized Terminology: Consistency in your terminology enhances clarity across documentation. This makes it easier for everyone on the healthcare team to interpret notes accurately. Avoiding non-standard abbreviations is crucial; it helps ensure that your assessments are clear and understandable.
-
Document in Real-Time: Writing notes during or immediately after your encounters can greatly enhance accuracy. As Vadim Kouznetsov, Founder and CEO of PatientNotes.AI, wisely states, "Timing is everything when it comes to SOAP notes. Ideally, you should write your notes right after meeting with a client while everything is still fresh in your mind." This practice helps capture essential details while they’re still vivid, reducing the risk of missing important information.
-
Review and Revise: Regularly assess your notes for completeness and clarity. A quick review can confirm the accuracy of names, medications, dosages, and observations, ensuring compliance and effective care. Remember, treatment plans should be revised at least every three months to meet compliance standards, highlighting the importance of detailed records.
By embracing these practices, you can significantly enhance the quality of your records, leading to better care outcomes and improved clinical decision-making. For example, in a case study of hypertension follow-up, precise records of a patient’s adherence to medication and lifestyle changes were vital for ongoing treatment planning.
So, take a moment to reflect: how can these practices improve your documentation and ultimately benefit your patients? Your commitment to clear and effective SOAP notes can make a world of difference.
Common Mistakes in SOAP Documentation: What to Avoid
Common errors found in soap documentation examples can significantly impact care and outcomes for individuals. Have you ever felt overwhelmed by the administrative tasks that seem to pile up? It’s a common challenge in healthcare, and it’s crucial to address these issues to ensure the best for our patients. Here are some key errors to avoid:
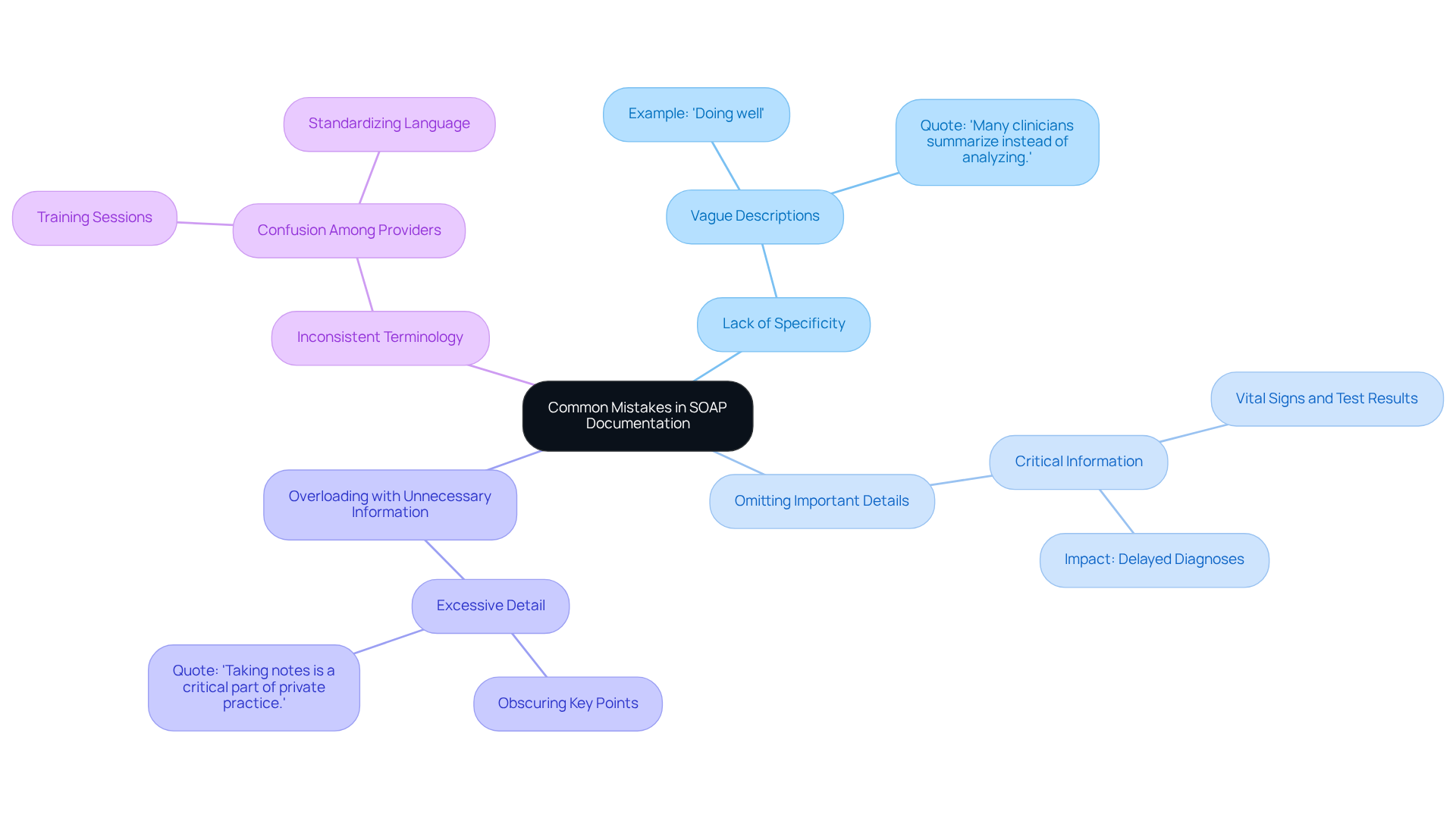
- Lack of Specificity: Vague descriptions can lead to misunderstandings and misinterpretations of a patient's condition. For instance, using broad expressions like 'doing well' doesn’t provide practical insights into the individual’s health status. As noted by HealthOrbit AI, 'Many clinicians summarize instead of analyzing,' which can diminish the quality of records.
- Omitting Important Details: Critical information, such as vital signs or specific test results, must be documented. Omissions can obscure underlying health issues, potentially delaying accurate diagnoses and treatment. Delays in recording patient interactions can lead to errors in SOAP documentation examples, which highlights the necessity for comprehensive records.
- Overloading with Unnecessary Information: Including excessive detail can obscure key points, making it difficult for other healthcare providers to extract essential information quickly. Clear and concise records are vital for effective communication. As Jess Barron, Editor-in-Chief at SimplePractice, states, "Taking notes is a critical part of private practice despite feeling like an additional task."
- Inconsistent Terminology: Using different terms for the same condition can confuse readers and hinder continuity of care. Standardizing language enhances clarity and ensures that all providers are on the same page. Regular training sessions can help familiarize staff with updated practices and guidelines, reducing inconsistencies.
Steering clear of these errors is essential for preserving high-quality soap documentation examples. Precise clinical documentation not only enhances effective communication among medical professionals but also plays a crucial role in ensuring safety and adherence to legal standards.
So, what can you do? Utilizing organized templates and participating in frequent training can greatly decrease the chances of record errors. This proactive approach ultimately leads to improved patient outcomes. Let’s work together to create a supportive environment where accurate documentation is a priority, ensuring that every patient receives the care they deserve.
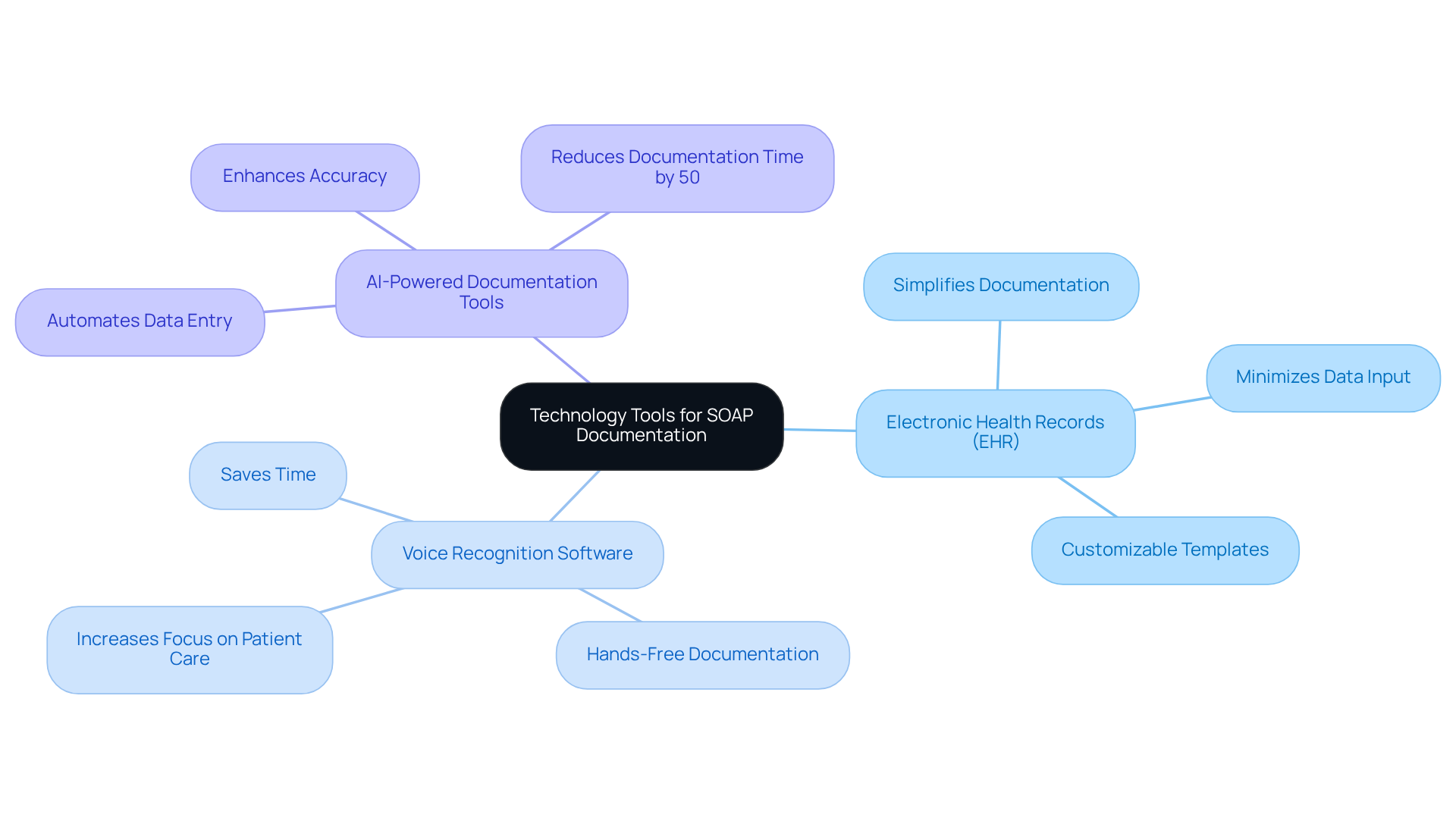
Technology Tools for Streamlining SOAP Documentation in Healthcare
In the fast-paced world of healthcare, many providers face overwhelming administrative burdens that can detract from the quality of patient care. Have you ever felt that the time spent on documentation takes away from the moments that truly matter with your patients? You're not alone. Fortunately, numerous technology tools are available to streamline SOAP documentation, significantly enhancing efficiency in healthcare settings:
- Electronic Health Records (EHR): EHR systems often come equipped with templates specifically designed for SOAP notes, simplifying the documentation process. By minimizing unnecessary data input and enabling customization according to medical specialties, EHRs enhance overall record-keeping efficiency.
- Voice Recognition Software: This technology allows providers to dictate notes, saving considerable time compared to traditional typing methods. For instance, users of Sunoh.ai report saving up to two hours each day, allowing them to focus more on providing care to individuals.
- AI-Powered Documentation Tools: Platforms like CosmaNeura automate data entry and ensure accuracy, further enhancing efficiency. SOAPNoteAI claims it can decrease daily record-keeping durations by as much as 50%, enabling medical professionals to concentrate more on client interactions instead of administrative duties.
By incorporating these advanced tools, medical service providers can significantly enhance their documentation processes. Imagine the relief of having more time to connect with your patients, leading to improved client care and a better work-life balance. Embrace these solutions and take a step towards a more fulfilling practice.
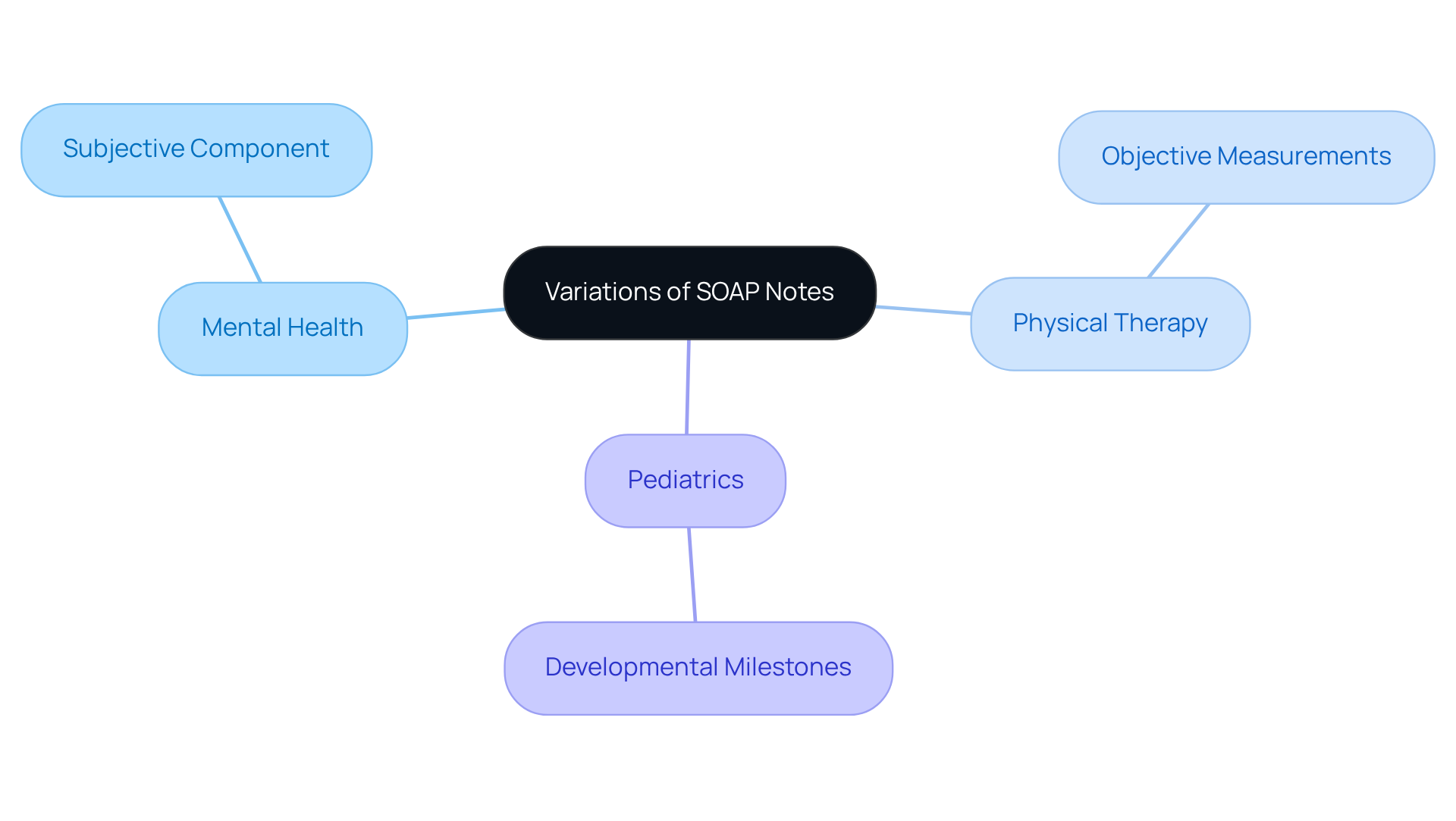
Variations of SOAP Notes: Tailoring Documentation for Different Healthcare Disciplines
SOAP notes aren’t just a standard template; they need to be customized to fit the unique needs of various healthcare disciplines. Have you ever felt overwhelmed by the administrative demands of your role? Let’s explore how tailoring SOAP notes can ease that burden and enhance patient care.
- Mental Health: In this field, the subjective component is crucial. It captures the emotional and psychological states of patients, allowing for a deeper understanding of their experiences. This insight guides treatment strategies effectively.
- Physical Therapy: Here, objective measurements and functional assessments take center stage. Documenting specific metrics, like range of motion or strength levels, is vital for tracking progress and adjusting treatment plans.
- Pediatrics: Documentation often includes developmental milestones and parental observations. These elements are essential for assessing a child's growth and addressing any concerns early on.
Recognizing these differences empowers healthcare professionals to create more relevant and impactful records. Customized SOAP notes not only improve communication among providers but also lead to better outcomes for individuals. Did you know that organized records can significantly enhance the quality of notes? Studies show a mean quality score improvement from 64.35 to 77.2 (p < 0.001), highlighting the positive impact of tailored methods on record quality.
By understanding and implementing these specialized practices, you can ensure that your records truly support optimal care for your patients. Let’s work together to make your documentation process smoother and more effective.
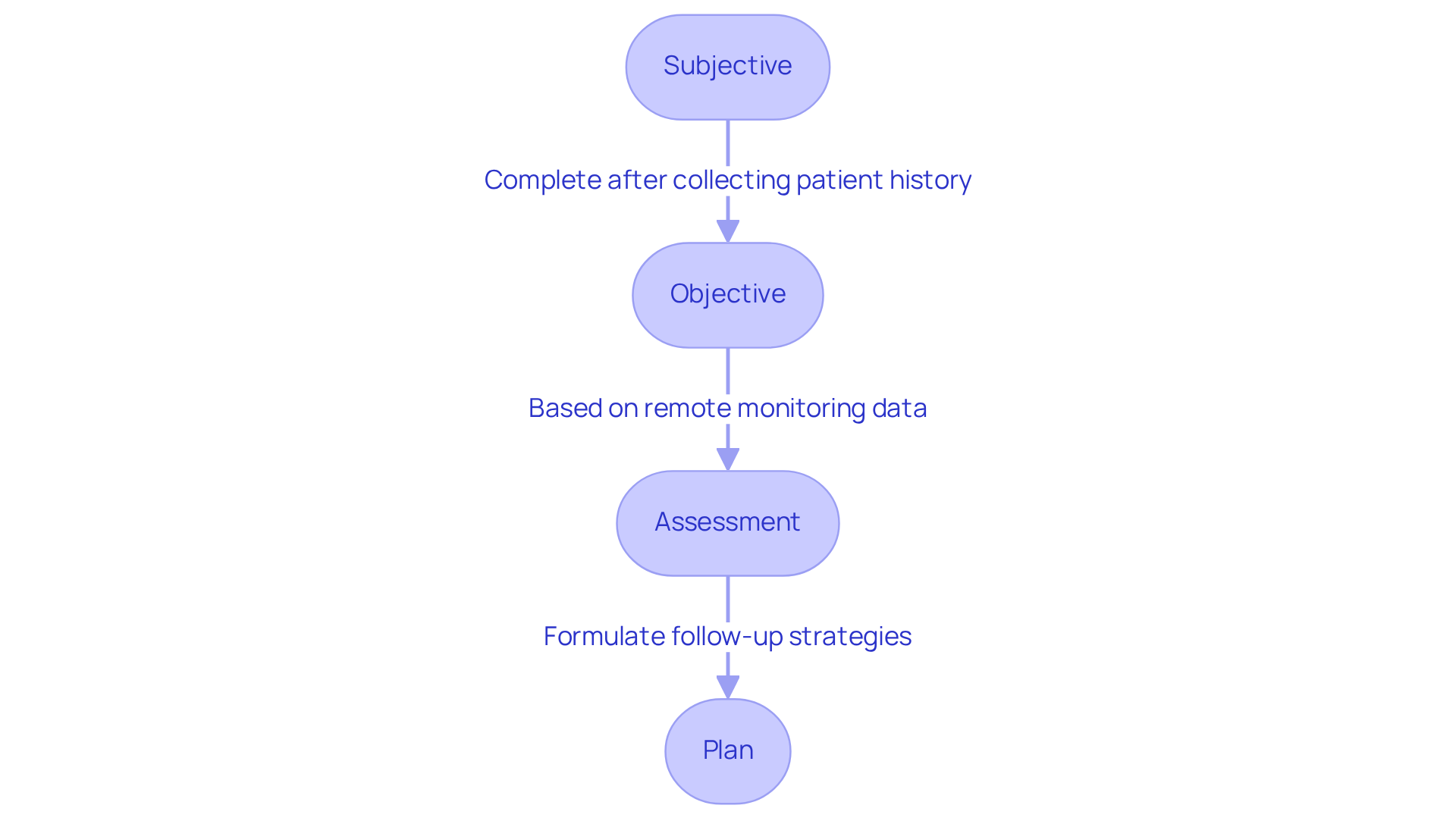
SOAP Notes in Telehealth: Adapting Documentation for Remote Care
In telehealth, it is essential to use soap documentation examples that adapt to the remote nature of care for maintaining effective documentation. Have you ever felt overwhelmed by the challenges of documenting patient care from a distance? You're not alone. Many healthcare providers face emotional hurdles as they navigate this new landscape. Let's explore how we can make this process smoother and more effective for everyone involved.
-
Subjective: Collecting comprehensive patient histories through virtual communication is crucial. This often means using direct quotes from patients to capture their concerns accurately, especially when physical examinations aren't possible. The Subjective section captures the client's history, symptoms, and concerns using direct quotes, ensuring that the patient's voice is truly heard.
-
Objective: Remote monitoring tools play a vital role in gathering vital signs and other measurable data. These tools enhance the accuracy of the Objective section by providing real-time health metrics, which are essential for informed clinical assessments. For instance, did you know that the average indirect waiting time for telehealth visits has decreased significantly? This highlights the efficiency of remote monitoring and its positive impact on patient care.
-
Assessment: Clinical judgments must be adjusted based on virtual interactions. This requires healthcare providers to be skilled at interpreting patient-reported symptoms and integrating them with data collected remotely. It's important to remember that legal and ethical factors are crucial; documentation must adhere to laws and regulations governing client records.
-
Plan: Clearly outlining follow-up steps and remote care strategies is critical. This involves detailing any required remote consultations, medication modifications, or lifestyle suggestions tailored to the individual's circumstances. By modifying clinical notes for virtual care, medical professionals can create effective soap documentation examples that remain relevant, ultimately improving patient support and outcomes.
As we adapt to this evolving landscape, let’s continue to support one another in providing the best care possible. How can we further enhance our documentation practices to better serve our patients?
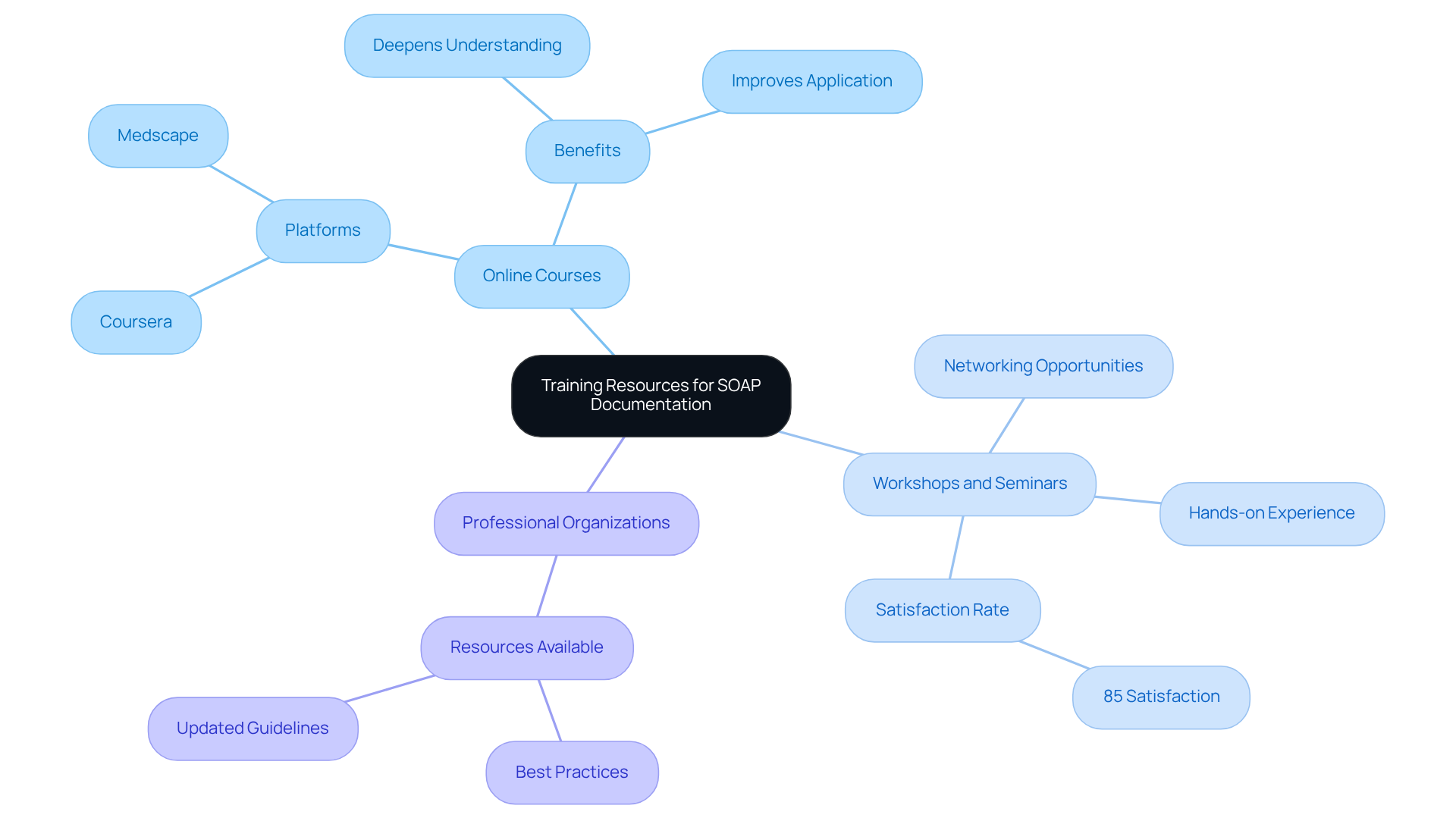
Training Resources for Mastering SOAP Documentation in Healthcare
To excel in SOAP documentation, healthcare providers often face emotional challenges that can feel overwhelming. The administrative burdens can detract from the core mission of patient care, leaving many feeling stressed and underprepared. But there’s hope! By leveraging a variety of training resources, providers can enhance their skills in SOAP documentation examples and improve their practice.
- Online Courses: Platforms like Coursera and Medscape offer specialized courses that focus on effective documentation techniques. These courses are designed to deepen understanding and application of SOAP documentation examples in clinical settings, making the process smoother and more intuitive.
- Workshops and Seminars: Participating in live workshops not only provides hands-on experience but also valuable networking opportunities. For instance, a recent series of workshops reported an impressive 85% satisfaction rate among attendees, showcasing the effectiveness of interactive learning. Research indicates that 85% to 98% of doctors noted improved quality, readability, and clinical precision of their records after training, underscoring the importance of these educational experiences.
- Professional Organizations: Joining relevant professional associations opens the door to a wealth of resources, including best practices and updated guidelines tailored to specific medical fields.
Investing in these training opportunities can lead to substantial enhancements in the quality of SOAP documentation examples. Did you know that medical professionals who engage in continuous education are 4.2 times more likely to maintain precise and thorough record-keeping methods? This ultimately improves patient care and safety. Moreover, the case study on 'Advanced EHR Skills Training at Kaiser Permanente' illustrates how focused training initiatives can significantly enhance record quality and physician satisfaction. This highlights the vital role of ongoing education in the healthcare sector.
So, why not take the next step? Embrace these training resources and empower yourself to provide the best care possible. Your commitment to continuous learning not only benefits you but also your patients, fostering a healthier future for all.
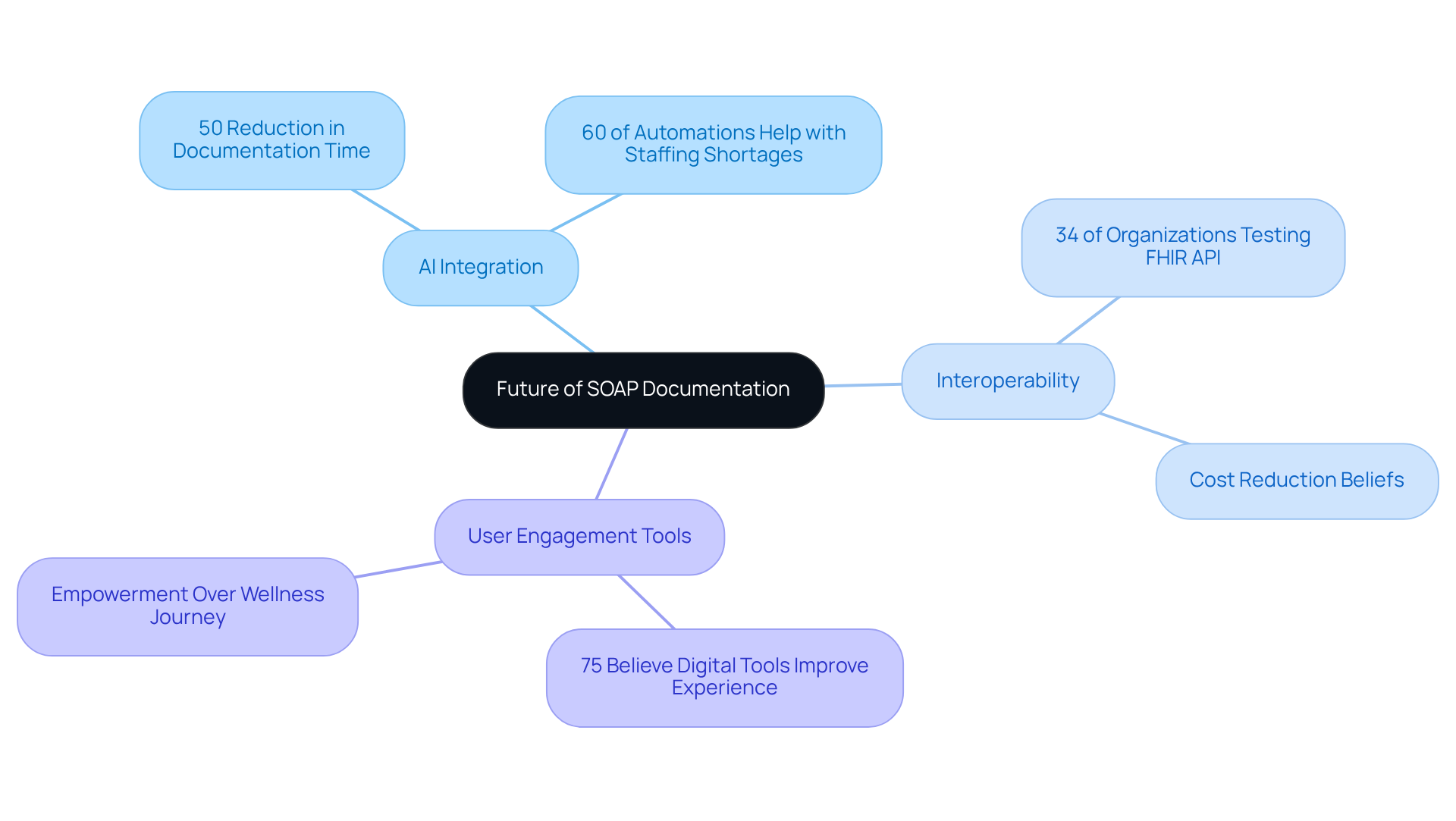
The Future of SOAP Documentation: Trends and Innovations in Healthcare
The future of SOAP documentation is on the brink of a significant transformation, driven by several key trends that can truly make a difference for healthcare providers:
-
AI Integration: Imagine a world where ongoing advancements in AI technology automate documentation processes, enhancing both accuracy and efficiency. By 2027, clinicians are expected to cut down their time spent on clinical documentation tasks by 50% thanks to generative AI. This shift allows them to focus more on what truly matters—patient care. Moreover, 60% of AI-enabled workflow automations are anticipated to help alleviate staffing shortages and clinician burnout, showcasing the profound advantages of AI in medical environments.
-
Interoperability is enhanced as systems are set to facilitate seamless sharing of SOAP documentation examples across various platforms and providers, significantly improving care coordination. Currently, 34% of U.S. medical organizations are testing or implementing the FHIR API, which supports this interoperability. Almost two-thirds of clinical, administrative, and IT leaders believe that AI can lower the overall cost of service delivery, underscoring the financial implications of enhanced interoperability.
-
User Engagement Tools: Innovations that actively involve individuals in the record-keeping process can lead to enhanced accuracy and satisfaction. With over 75% of individuals believing that digital tools improve their medical experience, incorporating user feedback into SOAP documentation examples will become increasingly important. As one expert noted, "AI is empowering individuals, providing them authority over their wellness journey," which aligns perfectly with the significance of user engagement in records.
Staying informed about these trends will empower healthcare providers to adapt their documentation practices effectively. By embracing these changes, they can ensure they remain at the forefront of patient care and operational efficiency. How can you leverage these trends to enhance your practice? Let's explore these opportunities together.
Conclusion
The essence of effective SOAP documentation is its power to ease the burden on healthcare providers while enhancing patient care. Have you ever felt overwhelmed by paperwork? By adopting structured SOAP notes, you can improve communication, ensure thorough record-keeping, and ultimately boost patient outcomes. With advanced technologies like AI and EHR systems, these benefits multiply, allowing you to focus more on meaningful patient interactions rather than getting lost in administrative tasks.
Throughout this article, we’ve shared key insights into the fundamental components of SOAP notes, practical examples of their application, and best practices for crafting effective documentation. We also highlighted common pitfalls to avoid, stressing the importance of specificity and clarity in clinical records. Tailoring SOAP notes to various healthcare disciplines and adapting documentation practices for telehealth settings is crucial in today’s evolving landscape.
As healthcare continues to change, embracing these documentation practices and leveraging innovative tools will be vital for enhancing patient care and operational efficiency. By committing to continuous learning and improvement in SOAP documentation, you can help create a more compassionate and effective healthcare environment. Remember, the journey toward better documentation isn’t just about compliance; it’s about nurturing the patient-provider relationship and ensuring that every individual receives the care and attention they truly deserve.
Key Solutions to Enhance SOAP Documentation:
- Streamline communication to improve patient interactions.
- Utilize technology to reduce administrative burdens.
- Tailor documentation to fit various healthcare settings.
Let’s work together to foster a healthcare environment where every patient feels valued and cared for.




